Abstract
Background
Loss of terminal differentiation markers and gain of stem cell-like properties are a major hallmark of cancer malignant progression. Identification of novel biomarkers representing tumor developmental progeny and predictive of patients’ prognosis would greatly benefit clinical cancer management.
Methods
Human embryonic stem cells were induced to differentiate into hepatocytes along hepatic lineages. Transcriptomic data from different liver developmental stages were analyzed combining with the RNA-seq data from The Cancer Genome Atlas (TCGA) project. Kaplan–Meier survival analysis and Cox regression analyses were used to analyze the clinical significance in HCC patients.
Results
A shifted expression pattern of claudin (CLDN) family genes were identified to be closely associated with liver development and tumor progression. Claudins with hepatic features were found to be significantly down-regulated and predicted better prognosis in HCC patients. Conversely, another set of claudins with embryonic stem cell features were found to be significantly up-regulated and predicted worse prognosis in HCC patients. A claudin signature score system was further established by combining the two sets of claudin genes. The newly established claudins signature could robustly predict HCC patients’ prognosis in the training, testing, and independent validation cohorts.
Conclusions
In the present study, we developed a novel embryonic developmental claudins signature to monitor the extent of tumor dedifferentiation in HCC from an in vitro hepatocyte differentiation model. The claudins signature might present a great potential in predicting prognostic significance in HCC as cell surface biomarkers, and provide novel therapeutic targets for precision oncology further in the clinic.




Similar content being viewed by others
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- RNA-seq:
-
RNA sequencing
- TCGA:
-
The cancer genome atlas
- ICGC:
-
International Cancer Genome Consortium
- hESCs:
-
Human embryonic stem cells
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under curve
- HCS:
-
Hepatic claudins signature
- ECS:
-
Embryonic claudins signature
- CSS:
-
Claudins signature scores
- PPI:
-
Protein–protein interaction
- HR:
-
Hazard ratio
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87–108. https://doi.org/10.3322/caac.21262
El-Serag HB. Hepatocellular carcinoma. N Engl J Med 2011;365:1118–1127. https://doi.org/10.1056/NEJMra1001683
Bass AJ, Watanabe H, Mermel CH, Yu S, Perner S, Verhaak RG, et al. SOX2 is an amplified lineage-survival oncogene in lung and esophageal squamous cell carcinomas. Nat Genet 2009;41:1238–1242. https://doi.org/10.1038/ng.465
Yimlamai D, Christodoulou C, Galli GG, Yanger K, Pepe-Mooney B, Gurung B, et al. Hippo pathway activity influences liver cell fate. Cell 2014;157:1324–1338. https://doi.org/10.1016/j.cell.2014.03.060
Sell S. Alpha-fetoprotein, stem cells and cancer: how study of the production of alpha-fetoprotein during chemical hepatocarcinogenesis led to reaffirmation of the stem cell theory of cancer. Tumour Biol 2008;29:161–180. https://doi.org/10.1159/000143402
Ramaswamy S, Tamayo P, Rifkin R, Mukherjee S, Yeang CH, Angelo M, et al. Multiclass cancer diagnosis using tumor gene expression signatures. Proc Natl Acad Sci USA 2001;98:15149–15154. https://doi.org/10.1073/pnas.211566398
Gunzel D, Fromm M. Claudins and other tight junction proteins. Compr Physiol 2012;2:1819–1852. https://doi.org/10.1002/cphy.c110045
Lal-Nag M, Morin PJ. The claudins. Genome Biol 2009;10:235. https://doi.org/10.1186/gb-2009-10-8-235
Gonzalez-Mariscal L, Betanzos A, Nava P, Jaramillo BE. Tight junction proteins. Prog Biophys Mol Biol 2003;81:1–44. https://doi.org/10.1016/S0079-6107(02)00037-8
Kwon M. Emerging roles of claudins in human cancer. Int J Mol Sci 2013;14:18148–18180. https://doi.org/10.3390/ijms140918148
Lin G, Xie Y, Ouyang Q, Qian X, Xie P, Zhou X, et al. HLA-matching potential of an established human embryonic stem cell bank in China. Cell Stem Cell 2009;5:461–465. https://doi.org/10.1016/j.stem.2009.10.009
Xie P, Sun Y, Ouyang Q, Hu L, Tan Y, Zhou X, et al. Physiological oxygen prevents frequent silencing of the DLK1-DIO3 cluster during human embryonic stem cells culture. Stem Cells 2014;32:391–401. https://doi.org/10.1002/stem.1558
Gramignoli R, Tahan V, Dorko K, Venkataramanan R, Fox IJ, Ellis EC, et al. Rapid and sensitive assessment of human hepatocyte functions. Cell Transplant 2014;23:1545–1556. https://doi.org/10.3727/096368914X680064
Zabulica M, Srinivasan RC, Vosough M, Hammarstedt C, Wu T, Gramignoli R, et al. Guide to the assessment of mature liver gene expression in stem cell-derived hepatocytes. Stem Cells Dev 2019;28:907–919. https://doi.org/10.1089/scd.2019.0064
Fujimoto A, Furuta M, Totoki Y, Tsunoda T, Kato M, Shiraishi Y, et al. Whole-genome mutational landscape and characterization of noncoding and structural mutations in liver cancer. Nat Genet 2016;48:500–509. https://doi.org/10.1038/ng.3547
Zhou Y, Zhou B, Pache L, Chang M, Khodabakhshi AH, Tanaseichuk O, et al. Metascape provides a biologist-oriented resource for the analysis of systems-level datasets. Nat Commun 2019;10:1523. https://doi.org/10.1038/s41467-019-09234-6
Su JS, Tsai TF, Chang HM, Chao KM, Su TS, Tsai SF. Distant HNF1 site as a master control for the human class I alcohol dehydrogenase gene expression. J Biol Chem 2006;281:19809–19821
Sgodda M, Aurich H, Kleist S, Aurich I, König S, Dollinger MM, et al. Hepatocyte differentiation of mesenchymal stem cells from rat peritoneal adipose tissue in vitro and in vivo. Exp Cell Res 2007;313:2875–2886
Zhang K, Zhang L, Liu W, Ma X, Cen J, Sun Z, et al. In vitro expansion of primary human hepatocytes with efficient liver repopulation capacity. Cell Stem Cell 2018;23:806–819.e4. https://doi.org/10.1016/j.stem.2018.10.018
Leonce J, Brockton N, Robinson S, Venkatesan S, Bannister P, Raman V, et al. Glucose production in the human placenta. Placenta 2006;27(Suppl A):S103–S108
Money TT, King RG, Wong MH, Stevenson JL, Kalionis B, Erwich JJ, et al. Expression and cellular localization of chloride intracellular channel 3 in human placenta and fetal membranes. Placenta 2007;28:429–436
Venook AP, Papandreou C, Furuse J, de Guevara LL. The incidence and epidemiology of hepatocellular carcinoma: a global and regional perspective. Oncologist 2010;15:5–13. https://doi.org/10.1634/theoncologist.2010-S4-05
Lee K, Lee KB, Jung HY, Yi NJ, Lee KW, Suh KS, et al. The correlation between poor prognosis and increased yes-associated protein 1 expression in keratin 19 expressing hepatocellular carcinomas and cholangiocarcinomas. BMC Cancer 2017;17:441. https://doi.org/10.1186/s12885-017-3431-1
Reinhard K, Rengstl B, Oehm P, Michel K, Billmeier A, Hayduk N, et al. An RNA vaccine drives expansion and efficacy of claudin-CAR-T cells against solid tumors. Science 2020. https://doi.org/10.1126/science.aay5967
Zhou B, Flodby P, Luo J, Castillo DR, Liu Y, Yu FX, et al. Claudin-18-mediated YAP activity regulates lung stem and progenitor cell homeostasis and tumorigenesis. J Clin Invest 2018;128:970–984. https://doi.org/10.1172/JCI90429
Wang SB, Xu T, Peng S, Singh D, Ghiassi-Nejad M, Adelman RA, et al. Disease-associated mutations of claudin-19 disrupt retinal neurogenesis and visual function. Commun Biol 2019;2:113. https://doi.org/10.1038/s42003-019-0355-0
Du W, Xu X, Niu Q, Zhang X, Wei Y, Wang Z, et al. Spi-B-mediated silencing of claudin-2 promotes early dissemination of lung cancer cells from primary tumors. Cancer Res 2017;77:4809–4822. https://doi.org/10.1158/0008-5472.CAN-17-0020
Cheng B, Rong A, Zhou Q, Li W. CLDN8 promotes colorectal cancer cell proliferation, migration, and invasion by activating MAPK/ERK signaling. Cancer Manag Res 2019;11:3741–3751. https://doi.org/10.2147/CMAR.S189558
Li CP, Cai MY, Jiang LJ, Mai SJ, Chen JW, Wang FW, et al. CLDN14 is epigenetically silenced by EZH2-mediated H3K27ME3 and is a novel prognostic biomarker in hepatocellular carcinoma. Carcinogenesis 2016;37:557–566. https://doi.org/10.1093/carcin/bgw036
Fan J, Zhu M, Wang Y, Li Z, Zhang J, Wang L, et al. Genome-wide analysis of expression quantitative trait loci identified potential lung cancer susceptibility variants among Asian populations. Carcinogenesis 2019;40:263–268. https://doi.org/10.1093/carcin/bgy165
Acknowledgements
We thank Prof. Lu and Prof. Lin’s group from the Institute of Reproductive and Stem Cell Engineering, School of Basic Medical Science, Central South University, Changsha, China, for kindly establish the in vitro hepatocyte differentiation model for us.
Funding
This work was supported by National Natural Science Foundation of China (81702400); Guangdong Province Universities and Colleges Pear River Scholar Funded Scheme (2018). The funders had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
ML and N-FM initiated and designed the project; F-EK, Y-QT, Y-FG, J-QM, YZ performed statistical analyses; F-EK, Y-QT, M-ML, WC, W-JZ, H-LL performed bioinformatic analyses; S-SL and LH provided the HCC clinical samples and the relevant clinical information; N-FM, and X-YG provided valuable comments; F-EK and ML wrote the manuscript, and all authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in this work.
Ethical approval
The study was approved by the Research Ethics Committees of Affiliated Cancer Hospital & Institute of Guangzhou Medical University. The experiments regarding the establishment of human embryonic stem cells and induced in vitro differentiation were approved and guided by the ethical committee of CITIC-Xiangya Reproductive & Genetic Hospital. The blastocysts, which were donated for the study after obtaining written informed consents from the patients undergoing assisted reproductive technology treatment, came from various clinical useless embryos, including poor quality embryos, abnormal embryos after pre-implantation genetic diagnosis (PGD), zygotes with the abnormal pronuclear number and partheno-activated embryos [11].
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12072_2020_10035_MOESM1_ESM.tif
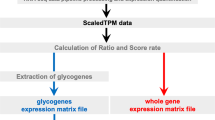
Supplementary file1 Supplementary Fig. S1 Flowchart of selecting claudins signature genes in predicting HCC prognosis (TIF 6588 kb)
12072_2020_10035_MOESM2_ESM.tif
Supplementary file2 Supplementary Fig. S2 Protein interaction of the claudins signatures genes and relevant enrichment analysis. (a) PPI network of claudins signatures genes and the 100 closest interaction genes were formed by using STRING database in Cytoscape 3.6.1. (b) Gene ontology and enrichment analysis also revealed the signaling pathways and function categories significantly associated with claudins signatures related genes, which included pathways or biological processes closely related to embryonic development (TIF 13711 kb)
12072_2020_10035_MOESM3_ESM.tif
Supplementary file3 Supplementary Fig. S3 Forest map (Logistic analysis) of claudins signatures and common clinical character in multiple HCC clinical cohorts. (a) Forest map (Logistic analysis) of hepatic and embryonic claudins signatures and other clinical characteristics in the training cohort (TCGA-LIHC Cohort I, n=189). (b) Similar analysis was presented in the testing cohort (TCGA-LIHC Cohort II, n=182) (c) and validated in an independent validation cohort (LIRI-JP Cohort, n=232). HR less than 1 was considered as low risk and HR more than 1 was considered as high risk. P value less than 0.05 was considered statistically significant. (TIF 10632 kb)
12072_2020_10035_MOESM4_ESM.tif
Supplementary file4 Supplementary Fig. S4 Kaplan-Meier survival analysis of overall survival and disease-free survival in HCC patients treated with sorafenib from the TCGA-LIHC database. (a) The sub-group of patients treated with sorafenib form the TCGA-LIHC database were extracted, and Kaplan-Meier survival analysis was performed according to the “Embryonic claudins signature” (ECS) score (b) “Hepatic claudins signature” (HCS) score, and (c) “Claudins signature score” (CSS) (TIF 946 kb)
12072_2020_10035_MOESM5_ESM.tif
Supplementary file5 Supplementary Fig. S5 Kaplan-Meier survival analysis of overall survival in HCC patients with or without HCV infection from the TCGA-LIHC database (TIF 4125 kb)
Rights and permissions
About this article
Cite this article
Kong, FE., Tang, YQ., Gong, YF. et al. Identification of prognostic claudins signature in hepatocellular carcinoma from a hepatocyte differentiation model. Hepatol Int 14, 521–533 (2020). https://doi.org/10.1007/s12072-020-10035-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-020-10035-z