Abstract
Purpose
Overweight and obesity are important risk factors for diabetes, cardiovascular diseases, and premature death in modern society. Recently, numerous natural and synthetic compounds have been tested in diet-induced obese animal models, to counteract obesity. Melatonin is a circadian hormone, produced by pineal gland and extra-pineal sources, involved in processes which have in common a rhythmic expression. In teleost, it can control energy balance by activating or inhibiting appetite-related peptides. The study aims at testing effects of melatonin administration to control-fed and overfed zebrafish, in terms of expression levels of orexigenic (Ghrelin, orexin, NPY) and anorexigenic (leptin, POMC) genes expression and morphometry of visceral and subcutaneous fat depots.
Methods
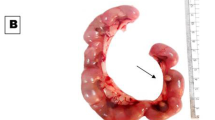
Adult male zebrafish (n = 56) were divided into four dietary groups: control, overfed, control + melatonin, overfed + melatonin. The treatment lasted 5 weeks and BMI levels of every fish were measured each week. After this period fishes were sacrificed; morphological and morphometric studies have been carried out on histological sections of adipose tissue and adipocytes. Moreover, whole zebrafish brain and intestine were used for qRT-PCR.
Results
Our results demonstrate that melatonin supplementation may have an effect in mobilizing fat stores, in increasing basal metabolism and thus in preventing further excess fat accumulation. Melatonin stimulates the anorexigenic and inhibit the orexigenic signals.
Conclusions
It seems that adequate melatonin treatment exerts anti-obesity protective effects, also in a diet-induced obesity zebrafish model, that might be the result of the restoration of many factors: the final endpoint reached is weight loss and stabilization of weight gain.






Similar content being viewed by others
References
D.W. Haslam, W.P. James, Obesity. Lancet 366(9492), 1197–1209 (2005). https://doi.org/10.1016/S0140-6736(05)67483-1
M. Cecchini, F. Sassi, Tackling obesity requires efficient government policies. Isr. J. Health Policy Res. 1(1), 18 (2012). https://doi.org/10.1186/2045-4015-1-18
T. Magrone, E. Jirillo, Childhood obesity: immune response and nutritional approaches. Front. Immunol. 6, 76 (2015). https://doi.org/10.3389/fimmu.2015.00076
N.M. Iyengar, C.A. Hudis, A.J. Dannenberg, Obesity and inflammation: new insights into breast cancer development and progression. Am. Soc. Clin. Oncol. Educ. Book (2013). https://doi.org/10.1200/EdBook_AM.2013.33.46
J.R. Speakman, Functional analysis of seven genes linked to body mass index and adiposity by genome-wide association studies: a review. Hum. Hered. 75(2-4), 57–79 (2013). https://doi.org/10.1159/000353585
B. de Luxán-Delgado, B. Caballero, Y. Potes, A. Rubio-González, I. Rodríguez, J. Gutiérrez-Rodríguez, J.J. Solano, A. Coto-Montes, Melatonin administration decreases adipogenesis in the liver of ob/ob mice through autophagy modulation. J. Pineal Res. 56(2), 126–133 (2014). https://doi.org/10.1111/jpi.12104
R.J. Reiter, D.X. Tan, L. Fuentes-Broto, Melatonin: a multitasking molecule. Prog. Brain. Res. 181, 127–151 (2010). https://doi.org/10.1016/S0079-6123(08)81008-4
J. Cipolla-Neto, F.G. Amaral, S.C. Afeche, D.X. Tan, R.J. Reiter, Melatonin, energy metabolism, and obesity: a review. J. Pineal Res. 56(4), 371–381 (2014). https://doi.org/10.1111/jpi.12137
D. Zephy, J. Ahmad, Type 2 diabetes mellitus: role of melatonin and oxidative stress. Diabetes Metab. Syndr. 9(2), 127–131 (2015). https://doi.org/10.1016/j.dsx.2014.09.018
D. Gnocchi, G. Bruscalup, Circadian rhythms and hormonal homeostasis: pathophysiological implications. Biology 6(1) (2017). https://doi.org/10.3390/biology6010010.
S.R. Pandi-Perumal, V. Srinivasan, G.J. Maestroni, D.P. Cardinali, B. Poeggeler, R. Hardeland, Melatonin: Nature’s most versatile biological signal? Febs. J. 273(13), 2813–2838 (2006). https://doi.org/10.1111/j.1742-4658.2006.05322.x
R.J. Reiter, D.X. Tan, A. Korkmaz, S. Ma, Obesity and metabolic syndrome: association with chronodisruption, sleep deprivation, and melatonin suppression. Ann. Med. 44(6), 564–577 (2012). https://doi.org/10.3109/07853890.2011.586365
M.B. Arnao, J. Hernandez-Ruiz, Functions of melatonin in plants: a review. J. Pineal Res. 59(2), 133–150 (2015). https://doi.org/10.1111/jpi.12253
G.A. Bubenik, Gastrointestinal melatonin: localization, function, and clinical relevance. Dig. Dis. Sci. 47(10), 2336–2348 (2002)
O. Lepage, E.T. Larson, I. Mayer, S. Winberg, Tryptophan affects both gastrointestinal melatonin production and interrenal activity in stressed and nonstressed rainbow trout. J. Pineal Res. 38(4), 264–271 (2005). https://doi.org/10.1111/j.1600-079X.2004.00201.x
C.C. Piccinetti, B. Migliarini, I. Olivotto, M.P. Simoniello, E. Giorgini, O. Carnevali, Melatonin and peripheral circuitries: insights on appetite and metabolism in Danio rerio. Zebrafish 10(3), 275–282 (2013). https://doi.org/10.1089/zeb.2012.0844
M.L. Pinillos, N. De Pedro, A.L. Alonso-Gomez, M. Alonso-Bedate, M.J. Delgado, Food intake inhibition by melatonin in goldfish (Carassius auratus). Physiol. Behav. 72(5), 629–634 (2001)
J. Falcon, L. Besseau, S. Sauzet, G. Boeuf, Melatonin effects on the hypothalamo-pituitary axis in fish. Trends Endocrinol. Metab. 18(2), 81–88 (2007). https://doi.org/10.1016/j.tem.2007.01.002
N. De Pedro, R.M. Martinez-Alvarez, M.J. Delgado, Melatonin reduces body weight in goldfish (Carassius auratus): effects on metabolic resources and some feeding regulators. J. Pineal Res. 45(1), 32–39 (2008). https://doi.org/10.1111/j.1600-079X.2007.00553.x
C.C. Piccinetti, B. Migliarini, I. Olivotto, G. Coletti, A. Amici, O. Carnevali, Appetite regulation: the central role of melatonin in Danio rerio. Horm. Behav. 58(5), 780–785 (2010). https://doi.org/10.1016/j.yhbeh.2010.07.013
D.X. Tan, L.C. Manchester, L. Fuentes-Broto, S.D. Paredes, R.J. Reiter, Significance and application of melatonin in the regulation of brown adipose tissue metabolism: relation to human obesity. Obes. Rev. 12(3), 167–188 (2011). https://doi.org/10.1111/j.1467-789X.2010.00756.x
P.J. Lardone, S.N. Alvarez-Sanchez, J.M. Guerrero, A. Carrillo-Vico, Melatonin and glucose metabolism: clinical relevance. Curr. Pharm. Des. 20(30), 4841–4853 (2014)
R. Hardeland, D.P. Cardinali, V. Srinivasan, D.W. Spence, G.M. Brown, S.R. Pandi-Perumal, Melatonin--a pleiotropic, orchestrating regulator molecule. Prog. Neurobiol. 93(3), 350–384 (2011). https://doi.org/10.1016/j.pneurobio.2010.12.004
I. Vinogradova, V. Anisimov, Melatonin prevents the development of the metabolic syndrome in male rats exposed to different light/dark regimens. Biogerontology 14(4), 401–409 (2013). https://doi.org/10.1007/s10522-013-9437-4
J.P. Chaput, Sleep patterns, diet quality and energy balance. Physiol. Behav. 134, 86–91 (2014). https://doi.org/10.1016/j.physbeh.2013.09.006
A.W. McHill, A.J. Phillips, C.A. Czeisler, L. Keating, K. Yee, L.K. Barger, M. Garaulet, F.A. Scheer, E.B. Klerman, Later circadian timing of food intake is associated with increased body fat. Am. J. Clin. Nutr. 106(5), 1213–1219 (2017). https://doi.org/10.3945/ajcn.117.161588
A. Seth, D.L. Stemple, I. Barroso, The emerging use of zebrafish to model metabolic disease. Dis. Models & Mech. 6(5), 1080–1088 (2013). https://doi.org/10.1242/dmm.011346
T. Oka, Y. Nishimura, L. Zang, M. Hirano, Y. Shimada, Z. Wang, N. Umemoto, J. Kuroyanagi, N. Nishimura, T. Tanaka, Diet-induced obesity in zebrafish shares common pathophysiological pathways with mammalian obesity. BMC Physiol. 10, 21 (2010). https://doi.org/10.1186/1472-6793-10-21
G. Montalbano, M. Mania, M.C. Guerrera, F. Abbate, R. Laurà, M. Navarra, J.A. Vega, E. Ciriaco, A. Germanà, Morphological differences in adipose tissue and changes in BDNF/Trkb expression in brain and gut of a diet induced obese zebrafish model. Ann. Anat. 204, 36–44 (2015). https://doi.org/10.1016/j.aanat.2015.11.003
S.K. McMenamin, J.E. Minchin, T.N. Gordon, J.F. Rawls, D.M. Parichy, Dwarfism and increased adiposity in the gh1 mutant zebrafish vizzini. Endocrinology 154(4), 1476–1487 (2013). https://doi.org/10.1210/en.2012-1734
J.E.N. Minchin, J.F. Rawls, A classification system for zebrafish adipose tissues. Dis. Model Mech. 10(6), 797–809 (2017). https://doi.org/10.1242/dmm.025759
M.B. Levanti, M.C. Guerrera, M.G. Calavia, E. Ciriaco, G. Montalbano, J. Cobo, A. Germana, J.A. Vega, Acid-sensing ion channel 2 (ASIC2) in the intestine of adult zebrafish. Neurosci. Lett. 494(1), 24–28 (2011). https://doi.org/10.1016/j.neulet.2011.02.046
F. Abbate, M.C. Guerrera, G. Montalbano, M.B. Levanti, G.P. Germanà, M. Navarra, R. Laurà, J.A. Vega, E. Ciriaco, A. Germanà, Expression and anatomical distribution of TrkB in the encephalon of the adult zebrafish (Danio rerio). Neurosci. Lett. 563, 66–69 (2014). https://doi.org/10.1016/j.neulet.2014.01.031
M.L. Bonet, P. Oliver, A. Palou, Pharmacological and nutritional agents promoting browning of white adipose tissue. Biochim. Biophys. Acta 1831(5), 969–985 (2013). https://doi.org/10.1016/j.bbalip.2012.12.002
H. Zhu, Q. Jin, Y. Li, Q. Ma, J. Wang, D. Li, H. Zhou, Y. Chen, Melatonin protected cardiac microvascular endothelial cells against oxidative stress injury via suppression of IP3R-[Ca(2+)]c/VDAC-[Ca(2+)]m axis by activation of MAPK/ERK signaling pathway. Cell Stress Chaperon-. 23(1), 101–113 (2018). https://doi.org/10.1007/s12192-017-0827-4
S. Roman, A. Agil, M. Peran, E. Alvaro-Galue, F.J. Ruiz-Ojeda, G. Fernandez-Vazquez, J.A. Marchal, Brown adipose tissue and novel therapeutic approaches to treat metabolic disorders. Transl. Res. 165(4), 464–479 (2015). https://doi.org/10.1016/j.trsl.2014.11.002
G. Favero, A. Stacchiotti, S. Castrezzati, F. Bonomini, M. Albanese, R. Rezzani, L.F. Rodella, Melatonin reduces obesity and restores adipokine patterns and metabolism in obese (ob/ob) mice. Nutr. Res. 35(10), 891–900 (2015). https://doi.org/10.1016/j.nutres.2015.07.001
R.J. Reiter, Pineal melatonin: cell biology of its synthesis and of its physiological interactions. Endocr. Rev. 12(2), 151–180 (1991). https://doi.org/10.1210/edrv-12-2-151
H. Gurer-Orhan, S. Suzen, Melatonin, its metabolites and its synthetic analogs as multi-faceted compounds: antioxidant, prooxidant and inhibitor of bioactivation reactions. Curr. Med. Chem. 22(4), 490–499 (2015)
M. Gallagher, W.D. Brown, Composition of San Francisco bay brine shrimp (Artemia salina). J. Agric. Food Chem. 23(4), 630–632 (1975). https://doi.org/10.1021/jf60200a008
R.Y. Xu, Y.P. Wan, Q.Y. Tang, J. Wu, W. Cai, The effects of high fat on central appetite genes in Wistar rats: a microarray analysis. Clin. Chim. Acta 397(1-2), 96–100 (2008). https://doi.org/10.1016/j.cca.2008.07.027
V. Srinivasan, Y. Ohta, J. Espino, J.A. Pariente, A.B. Rodriguez, M. Mohamed, R. Zakaria, Metabolic syndrome, its pathophysiology and the role of melatonin. Recent Pat. Endocr. Metab. Immun. Drug Discov. 7(1), 11–25 (2013)
N. De Pedro, R.M. Martínez-Alvarez, M.J. Delgado, Melatonin reduces body weight in goldfish (Carassius auratus): effects on metabolic resources and some feeding regulators. J. Pineal Res. 45(1), 32–39 (2008). https://doi.org/10.1111/j.1600-079X.2007.00553.x
B. Perry, Y. Wang, Appetite regulation and weight control: the role of gut hormones. Nutr. Diabetes 2, e26 (2012). https://doi.org/10.1038/nutd.2011.21
B. Prunet-Marcassus, M. Desbazeille, A. Bros, K. Louche, P. Delagrange, P. Renard, L. Casteilla, L. Penicaud, Melatonin reduces body weight gain in Sprague Dawley rats with diet-induced obesity. Endocrinology 144(12), 5347–5352 (2003). https://doi.org/10.1210/en.2003-0693
F. Nduhirabandi, E.F. du Toit, A. Lochner, Melatonin and the metabolic syndrome: a tool for effective therapy in obesity-associated abnormalities? Acta Physiol. 205(2), 209–223 (2012). https://doi.org/10.1111/j.1748-1716.2012.02410.x
E. Lima-Cabello, M.E. Diaz-Casado, J.A. Guerrero, B.B. Otalora, G. Escames, L.C. Lopez, R.J. Reiter, D. Acuna-Castroviejo, A review of the melatonin functions in zebrafish physiology. J. Pineal Res. 57(1), 1–9 (2014). https://doi.org/10.1111/jpi.12149
F. Nduhirabandi, B. Huisamen, H. Strijdom, D. Blackhurst, A. Lochner, Short-term melatonin consumption protects the heart of obese rats independent of body weight change and visceral adiposity. J. Pineal Res. 57(3), 317–332 (2014). https://doi.org/10.1111/jpi.12171
K. Szewczyk-Golec, P. Rajewski, M. Gackowski, C. Mila-Kierzenkowska, R. Wesołowski, P. Sutkowy, M. Pawłowska, A. Woźniak, Melatonin supplementation lowers oxidative stress and regulates adipokines in obese patients on a calorie-restricted diet. Oxid. Med. Cell Longev. 2017, 8494107 (2017). https://doi.org/10.1155/2017/8494107
C.C. Piccinetti, L.A. Ricci, N. Tokle, G. Radaelli, F. Pascoli, L. Cossignani, F. Palermo, G. Mosconi, V. Nozzi, F. Raccanello, I. Olivotto, Malnutrition may affect common sole (Solea solea L.) growth, pigmentation and stress response: molecular, biochemical and histological implications. Comparative biochemistry and physiology. Part A Mol. Integr. Physiol. 161(4), 361–371 (2012). https://doi.org/10.1016/j.cbpa.2011.12.009
F. García-García, E. Juárez-Aguilar, J. Santiago-García, D.P. Cardinali, Ghrelin and its interactions with growth hormone, leptin and orexins: implications for the sleep-wake cycle and metabolism. Sleep. Med. Rev. 18(1), 89–97 (2014). https://doi.org/10.1016/j.smrv.2013.04.003
H. Mangge, K. Summers, G. Almer, R. Prassl, D. Weghuber, W. Schnedl, D. Fuchs, Antioxidant food supplements and obesity-related inflammation. Curr. Med. Chem. 20(18), 2330–2337 (2013)
C.E. Perez-Leighton, C.J. Billington, C.M. Kotz, Orexin modulation of adipose tissue. Biochim. Biophys. Acta 1842(3), 440–445 (2014). https://doi.org/10.1016/j.bbadis.2013.06.007
C. Kotz, J. Nixon, T. Butterick, C. Perez-Leighton, J. Teske, C. Billington, Brain orexin promotes obesity resistance. Ann. N. Y. Acad. Sci. 1264, 72–86 (2012). https://doi.org/10.1111/j.1749-6632.2012.06585.x
C.M. Novak, C.M. Kotz, J.A. Levine, Central orexin sensitivity, physical activity, and obesity in diet-induced obese and diet-resistant rats. Am. J. Physiol. Endocrinol. Metab. 290(2), E396–403 (2006). https://doi.org/10.1152/ajpendo.00293.2005
R.D. Cone, The Central Melanocortin System and Energy Homeostasis. Trends Endocrinol. Metab. 10(6), 211–216 (1999)
J.M. Cerda-Reverter, M.J. Agulleiro, R.G. R, E. Sanchez, R. Ceinos, J. Rotllant, Fish melanocortin system. Eur. J. Pharmacol. 660(1), 53–60 (2011). https://doi.org/10.1016/j.ejphar.2010.10.108
I. Gantz, T.M. Fong, The melanocortin system. Am. J. Physiol. Endocrinol. Metab. 284(3), E468–474 (2003). https://doi.org/10.1152/ajpendo.00434.2002
E. Valassi, M. Scacchi, F. Cavagnini, Neuroendocrine control of food intake. Nutr., Metab., Cardiovasc. Dis. 18(2), 158–168 (2008). https://doi.org/10.1016/j.numecd.2007.06.004
A. Agil, M. El-Hammadi, A. Jimenez-Aranda, M. Tassi, W. Abdo, G. Fernandez-Vazquez, R.J. Reiter, Melatonin reduces hepatic mitochondrial dysfunction in diabetic obese rats. J. Pineal Res. 59(1), 70–79 (2015). https://doi.org/10.1111/jpi.12241
Author contributions
Conceived and designed the experiments: M.G., M.M., G.A. Performed the experiment: M.G., M.M., G.M.C. Collection and assembly of data: M.G., M.M., G.A. Data analysis and interpretation: M.G., M.M., G.A., G.M.C., L.M., V.J.A., A.F., N.M., L.R. Manuscript writing: M.G., M.M. Final approval of manuscript: all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
These authors contributed equally: Montalbano G. and Mania M.
Rights and permissions
About this article
Cite this article
Montalbano, G., Mania, M., Abbate, F. et al. Melatonin treatment suppresses appetite genes and improves adipose tissue plasticity in diet-induced obese zebrafish. Endocrine 62, 381–393 (2018). https://doi.org/10.1007/s12020-018-1653-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1653-x