Abstract
Purpose of Review
Increasing evidence on the significance of nutrition in reproduction is emerging from both animal and human studies, suggesting an association between nutrition and male fertility. Here, we have highlighted the impact of the various food groups on reproductive hormones and on spermatogenesis, and the effects of classical and latest dietary patterns such as Mediterranean diet, Western diet, intermittent fasting, ketogenic diet, and vegan/vegetarian diet on male fertility.
Recent Findings
Nutrients are the precursors of molecules involved in various body’s reactions; therefore, their balance is essential to ensure the correct regulation of different systems including the endocrine system. Hormones are strongly influenced by the nutritional status of the individual, and their alteration can lead to dysfunctions or diseases like infertility. In addition, nutrients affect sperm production and spermatogenesis, controlling sexual development, and maintaining secondary sexual characteristics and behaviors.
Summary
The consumption of fruit, vegetables, fish, processed meats, dairy products, sugars, alcohol, and caffeine importantly impact on male fertility. Among dietary patterns, the Mediterranean diet and the Western diet are most strongly associated with the quality of semen. Nutrients, dietary patterns, and hormonal levels have an impact on male infertility. Therefore, understanding how these factors interact with each other is important for strategies to improve male fertility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nutritional status is directly related to eating habits, and adequate nutrition is fundamental for health. In recent years, unhealthy eating patterns, characterized by greater consumption of saturated fats, trans fatty acids, simple sugars and high sodium content, and lower consumption of foods rich in antioxidants, such as fruits and vegetables [1], have spread. Unhealthy eating patterns and a sedentary lifestyle contribute to the increased incidence of overweight and obesity, which are risk factors for many chronic diseases, such as cancer, diabetes, and cardiovascular disease and male infertility [2].
Physiologically gonadotropin-releasing hormone (GnRH) causes the pituitary gland in the brain to make and secrete the hormones luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones target the testis; in particular, LH acts on the Leydig cells, while FSH acts on the Sertoli cells. The Leydig cells are the primary source of testosterone (Te) and androgens which have a crucial role in fertility, including sperm production and spermatogenesis, controlling sexual development, and maintaining secondary sexual characteristics and behaviors [3,4,5].
In obesity, the increased adipose tissue determines an increase in adipocyte aromatase activity and a consequent increase in the circulating levels of 17 beta-estradiol (E2). The increase in E2, in turn, acts with a negative feedback mechanism on the hypothalamic-pituitary axis, with consequent inhibition of GnRH, LH, and FSH (Fig. 1) [6]. BMI was negatively correlated with inhibin B levels and with FSH. Increasing BMI in males is associated with decreased levels of serum Te, sex hormone binding globulin (SHBG), and inhibin B and increased free androgen index and E2 levels. Such reduced pituitary FSH stimulation could adversely affect Sertoli cell function, inhibin B, and sperm production, as well as Leydig cell testosterone production. A hypothesized mechanism for these changes involves the aromatase enzyme, capable of converting steroid precursors into estrogens. Increased amounts of adipose tissue would lead to increased conversion of Te to estrogen reported associated with obesity. On the contrary, there was no significant association of testicular volume with BMI but the lower concentrations of inhibin B in obese males seems to indicate decreased tubule function resulting in decreased tubular volume [2, 7].
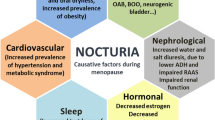
Gonadotropin-releasing hormone (GnRH) is secreted from the hypothalamus by GnRH-expressing neurons. The anterior portion of the pituitary gland produces luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and the gonads produce estrogen (E2) and testosterone (Te). The increase in E2, in turn, acts with a negative feedback mechanism, on the hypothalamic-pituitary axis, with consequent inhibition of the release of GnRH and pituitary gonadotropins. These hormones target the testis; in particular, LH acts on the Leydig cells inducing the synthesis of steroid hormones, while FSH acts on the Sertoli cells, stimulating spermatogenesis. The increase of estrogens was related to intake of food pattern like red meat, dairy product, alcohol, SSB, sugars, and soy
In addition to these factors, an unbalanced diet leads to a low-grade systemic inflammatory state that can impact on spermatogenesis [8]. In this regard, men who are overweight and suffer from metabolic syndrome may be at higher risk of infertility due to abnormal hormonal regulation and radical oxygen species (ROS) production. Thus, an alteration of sexual hormones, obesity incidence, and inflammatory state can have a direct effect on Leydig cell dysfunction and poor semen parameters as the sperm concentration, motility, vitality, and morphology [9].
Since the eighties, the excessive or insufficient intake of some substances, as trans fatty acids and zinc respectively, has been considered a determining factor for sperm function, fertility, and the functionality of the reproductive system [10, 11].
Recently, several studies highlighted how diets rich in fish, shellfish and seafood, poultry, cereals, vegetables and fruit, and dairy products (low fat content) are positively correlated with semen quality [12, 13]. Conversely, diets rich in processed meats, soy, potatoes, full-fat dairy products, coffee, alcohol, sugary drinks, and sweets seem to worsen semen quality [12, 14] (Fig. 2).
The father’s nutritional status during the periconceptional period is particularly important for the efficient fetal development and the growth of the progeny [15, 16]. In addition to age and environmental exposures, food may also be a risk factor for de novo mutations in fathers with possibly transgenerational consequences. All these events are adaptive and may change during life conferring, or not, predisposition to chronic disease and cancer [15, 16].
The aim of this review is to summarize the available findings on food and dietary patterns and their impact on male fertility.
Methods
We conducted a narrative review of the literature to evaluate the relationship between food groups, dietary patterns, and male fertility. We searched the Medline (PubMed) database between 2010 and January 2023 using the following search terms: male fertility OR fertility OR male infertility OR reproduction OR semen quality OR sperm OR asthenozoospermia OR teratozoospermia OR sperm DNA damage OR oligozoospermia OR oligoasthenozoospermia OR oligoasthenoteratozoospermia AND nutrition OR nutrient OR diet OR food OR vitamins OR antioxidants OR cereals OR meat OR fatty acids OR poultry OR vegetables OR fruit OR nuts OR fish OR shellfish OR sweets OR sugars OR sugar-sweetened beverages OR legumes OR milk OR cheese OR dairy products OR eggs OR caffeine OR alcohol OR ethanol OR sugar OR consumption OR soy OR estrogens OR Mediterranean diet OR Western diet OR Vegetarian diet OR Vegan diet OR Ketogenic diet OR Intermittent fasting.
Additional studies were identified from the study reference lists. We included case–control, cross-sectional and observational prospective and retrospective studies, review articles, meta-analysis, RCTs, and animal studies.
Food Groups and Their Influence on Fertility
Dairy Products and Meats
Saturated fatty acids (SFAs) and trans fatty acids (TFAs) are present in most foods of animal origin including meat, dairy products, and hydrogenated vegetable oils and have a role in the increasing incidence of obesity, coronary heart disease, diabetes, cancer, and also infertility [17]. In this regard, several studies have identified a negative correlation between a diet rich in trans fatty acids and sperm concentration, ejaculate volume, motility, better morphology [18,19,20], and high Te level [21].
The impact of SFAs in the deterioration of seminal quality could be attributed to their ability to induce a low-grade state of inflammation and the increased concentration of cholesterol in the membrane of spermatozoa, damaging their structure and compromising the quality of the gamete. Furthermore, the mitochondria, following the increase and accumulation of substrates, may not be able to oxidize all the lipids that accumulate in them, thus triggering the process that leads to an excess of radical oxygen species (ROS) production by sperm [22], and an adverse impact on motility and DNA integrity (Table 1) [23]. On the contrary, the polyunsaturated fatty acids (PUFAs), particularly the omega 3 PUFAs, have a positive effect on seminal pH, semen volume, sperm motility, sperm concentration, and vitality [24].
Regarding meat consumption, the intake of total meat, unprocessed meat, and raw vegetables may reduce the risk of asthenozoospermia, while a higher consumption of processed meat (about 2 or more servings/day) may increase the risk [25••]. Poultry intake was linked to a higher fertilization rate; conversely, processed meat consumption was associated with a lower fertilization rate in couples undergoing assisted reproduction [26]. Likewise, in the study of Braga et al., red meat consumption was inversely related to implantation and pregnancy rate in couples undergoing intracytoplasmic sperm injection (ICSI) [27].
To note, the greatest amount of meat consumed in the western countries derives from intensive farming and contains high concentrations of xenoestrogens and in some cases steroids, which, being endowed with estrogen-like actions, can become responsible for a decrease in male fertility impacting on semen quality and reproductive hormone levels [23, 25••, 26]. Among xenoestrogens, polychlorinated biphenyls (PCBs) were detected in the seminal plasma of infertile men and the concentration of phthalate esters (PEs) was significantly higher in infertile men compared with controls. In particular, in infertile men, the xenoestrogen concentrations were inversely proportional to the total motile sperm counts [28].
Analyzing the dietary habits of patients affected by oligoasthenoteratozoospermia (OAT) was found that the intake of dairy fat was positively associated with the risk of OAT [30]. Conversely, the use of low-fat milk was associated with a lower risk of asthenozoospermia (Table 1) [31]. In addition, some studies evaluated the relationship between the intake of dairy products and male fertility, and observed that the intake of dairy products was inversely related to sperm morphology and progressive motility, but positively correlated with FSH levels (Table 1) [29].
Other important evidence comes from the recent work of He et al., in which it was shown that lactoferrin and milk attenuate the dysfunctions of spermatogenesis, improving disordered autophagy, apoptosis, and oxidative stress, in the male mice reproductive system [32].
As for meat, cow’s milk has also been suggested as a possible source of xenoestrogens that could affect human health, even if the amounts of estrogens in cow’s milk are usually too low to affect humans [33]. The presence of environmental contaminants in dairy products, such as pesticides and chlorinated pollutants [34], have been associated with lower sperm quality [28, 35] and elevated FSH levels and no alteration of other sexual hormones [36]. The data was interesting and is in contrast with the physiological effect of FSH on spermatogenesis in which the administration of FSH to normogonadotropic patients with male factor infertility induced a marked increase in sperm count, a slight increase in sperm motility [37]. The potential effects of fermented milk products on male reproductive health were investigated in animal models [38] identifying a protective effect of fermented goat’s milk on genomic stability, oxidative stress, and inflammation in rat testis during anemia recovery. In particular, the study of Hammami et al. on mice showed how kefir consumption recovers impaired spermatogenesis due to a high-fat diet and restores testicular barrier proteins [39].
Fruits, Vegetables, and Legumes
Fruit and vegetables are the main sources of antioxidant substances in nature. In a healthy and balanced diet, the intake of these foods corresponds to 3 portions of fruit and 2 portion of vegetables per day [40].
Fruits and vegetables have a low-calorie content and provide water, simple sugars (fructose), vitamins, minerals (potassium and magnesium), fibers, and phytochemicals. Phytochemicals (organic acids, polyphenols, and oligosaccharides) are organic compounds of vegetable origin without nutritional properties, with antioxidant action against free radicals and polyunsaturated fatty acids and contribute to the development of intestinal bacterial flora [40]. Antioxidant power of vitamins has been associated with the ability of sperm to produce ROS [41••]. Several studies have confirmed the negative effects of ROS accumulation on seminal quality, chromatin integrity, and on the rate of abortion and malformations in offspring [8, 42]. Interestingly, some human studies have shown that antioxidant supplementation can reduce the oxidative stress in spermatozoa [43, 44].
In this regard, some studies have highlighted the protective role of some fruit juices and extracts on male fertility. In particular, the antioxidant activity of vitamins and phytochemicals, contained in pineapple, tomato, strawberry, elderberry, pomegranate, cherry laurel, grape, raspberry, and white mulberry, can have a protective role in testicular damage rodent models. Altogether, the main effects would be to restore serum Te levels, reduce testicular oxidative imbalance, improve the morphological condition of the seminiferous tubules, and thus improve seminal quality including concentration, motility, and morphology [45,46,47,48,49].
Moreover, resveratrol, a natural non-flavonoid polyphenol widely present in grapes, peanuts, berries, and red wine, has a positive effect on sperm motility at low concentrations, whereas at higher concentrations, it has a detrimental effect on sperm motility and has a protective role against sperm DNA damage caused by oxidative stress [50].
Some human studies have shown the protective effect of the consumption of dried fruit, in particular walnuts, date palm, hazelnut, and chestnut on male fertility [12, 51, 52]. The consumption of walnuts daily added to a Western-style diet improved effects on sperm vitality, motility, and morphology and had an impact on sperm DNA methylation (Table 1) [53], testicular antioxidant function, and semen quality. The consumption of chestnut polysaccharides has an impact on restoring spermatogenesis [54]. In fact, the presence of omega-3 alpha-linolenic acid (ALA) is crucial for some cellular functions such as phagocytosis of residual bodies by Sertoli cells, morphology, and fluidity of the sperm membrane [55].
Beyond vitamins, folates, mainly present in green leafy vegetables, protect the DNA from damage, by reducing the concentration of homocysteine through its re-methylation into methionine. In fact, homocysteine, functioning as a strong oxidative stress factor, can increase the reactive oxygen species which in turn can compromise the concentration of spermatozoa and their mobility. Furthermore, folates play a central role in spermatogenesis with a significant increase in total normal sperm count and a minor increase of abnormal spermatozoa in double-blind, randomized, placebo-controlled trial sub-fertile and fertile men (Table 1) [56].
The supplementation of folate, zinc, and antioxidants (vitamin C, vitamin E, and beta-carotene) in men with adequate nutrition is associated with lower frequencies of sperm with aneuploidy [57].
Furthermore, fruits, vegetables, legumes, and whole grains are the main source of fiber. It was highlighted that the consumption of fibers reduces plasma estrogen levels, due to their direct link with non-conjugated estrogens of food origin, limiting their intestinal absorption [58].
Among legumes, soy, in contrast to the other legumes, may have deleterious effects on spermatogenesis, even if the results are not concordant across the studies. This negative influence may be due to the presence of phytoestrogens [59, 60]; in fact, the intake of soy foods and sources of isoflavones is inversely related to the concentration of sperm [58] and free Te levels [61, 62]. Some studies have shown a deleterious impact of soy consumption on neonatal exposure male rats or humans on reproductive defects [63,64,65,66] and decreased weight or size of testicles [67]. Instead, other studies have not shown effects of soy on the concentration of gonadotropins and sex hormones, or on seminal quality [61, 68] while other identified lower levels of FSH [67] and Te [69] (Table 1).
Fish and Shellfish
Fish consumption is associated with a higher number of total spermatozoa and a higher percentage of morphologically normal spermatozoa (Table 1) [70]. Specifically, dark meat, such as salmon and tuna, is associated with an increase in the total number of spermatozoa while the consumption of fish with light flesh, such as cod and halibut, correlates with a greater expression of typical forms of sperm [20].
The potential benefits deriving from fish and shellfish can be related to their content in omega-3 fatty acids or PUFAs, such as docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA). Omega-3 essential fatty acids are important components of sperm cell membranes [71, 72], and omega-3 supplementation in a double-blind, placebo-controlled, randomized study conducted in subjects affected by idiopathic oligoasthenoteratospermia resulted in an improved the sperm cell total count, and both SOD-like and catalase-like activity [73].
Despite the beneficial effect linked to PUFAs, fish can compromise fertility because of toxic molecules. A Swedish study reported that organochlorines, pollutants present especially in mollusks and seafood, are associated to the alteration of seminal parameters such as total motility and chromatin integrity [74]. Heavy metals as mercury (Hg), found in high concentrations in the adipose tissue of marine fauna, affect spermatogenesis [75]. Furthermore, a recent study showed that the consumption of canned fish was inversely related to sperm immobility, while a high consumption of fresh fish increased the percentage of immotile sperm in Iranian infertile men [76]. However, the authors should be considered that in Iranian habits, fresh fish is eaten fried and therefore seems to have a negative effect on seminal quality.
Taking all these considerations, further investigations are needed to confirm the relation between fish and male infertility.
Sugars and Sugar-Sweetened Beverages
Glucose metabolism is essential for spermatogenesis. Glucose enters the spermatozoa by facilitated diffusion, through the expression of glucose transporters (GLUT) on the cell membrane. However, an excessive intake of glucose due to diets rich in sugars, sweets, potatoes, and foods with a high glycemic index influence semen quality [77] because hyperglycemia affects sperm motility and sperm maturation [78]. Sugar-sweetened beverage (SSBs) intake was inversely correlated with low semen quality in terms of total sperm count, semen volume, and motility (Table 1) [79]. The consumption of SSBs is also associated with a lower serum inhibin-B/FSH ratio [80] and higher E2 level that are correlated with low sperm production and quality (Table 1) [81•]. Hatch et al. observed that SSBs, particularly sodas and energy drinks, were associated with lower fecundability in a North American preconception cohort [82].
Moreover, the consumption of sweets and sugary drinks is associated with a higher incidence of obesity, type 2 diabetes mellitus, and metabolic syndrome, all conditions in which insulin resistance occurs, which leads to an increase in oxidative stress [78].
Caffeine and Alcohol
Among the various eating habits, the increasingly frequent intake of coffee has been associated with altered spermatogenesis [83], and with increased blood Te levels that leads to a decrease in circulating gonadotropins (Table 1) [84]. However, the association between caffeine and fertility rates is not defined [85]. Recently, Ricci et al. have shown that a moderate caffeine intake by women and men in the year prior to the assisted reproductive technology (ART) procedure was not associated with negative outcomes [86].
The relationship between caffeine and fertility remains unclear. In fact, if on the one hand it seems to correlate with a decrease in the total number of spermatozoa [84, 87] and with an increased number of atypia and sperm DNA damage (Table 1) [87], on the other hand, it seems to improve the energy metabolism of Sertoli cells [88] and sperm motility [89, 90, 91•, 92]. Akomolafe et al. showed that caffeine reversed the alteration of fertility parameters in a rat model through the modulation of the steroidogenic enzymes, improving sperm quality and attenuating the oxidative damage in testicular and epididymal tissues [92]. In rodents, caffeine exposure has shown an effect on the weight and size of reproductive organs [93], on the testicular microarchitecture, and on the germ cell proliferation [94].
It has also been highlighted that the risk of dyspermia is directly proportional to the number of cups of coffee consumed daily [83, 84, 95]. In contrast, a study conducted on the Danish population found only a reduction in the total number of spermatozoa in relation to excessive caffeine intake [87].
Several animal and human studies have focused on the impact of ethanol (EtOH) consumption on reproductive hormonal regulation, semen quality, gene transcription, genetics, and epigenetics regulation [96, 97]. Moderate alcohol consumption does not seem to have a major effect on the seminal fluid parameters [98]; on the contrary, its abuse has a negative effect on the entire male reproductive system, through various pathogenic mechanisms. In fact, EtOH and its metabolites, by influencing the hypothalamic pituitary axis, induce a suppression of gonadotropin production, causing a decrease in Te levels and an altered relationship between free Te and free E2 [96]. Moreover, alcohol has a direct negative impact on spermatogenesis (Table 1) [96] as it contributes significantly to the increase of oxidative stress and the formation of ROS [99, 100]. Alcohol may also alter the secretion of the accessory glands, resulting in a decreased seminal quality [101] in terms of volume, concentration, morphology, motility, epigenetic regulation, expression of genes, and protein involved in sperm functions, DNA integrity, and chromatin condensation [102]. These alterations can occur both in the chronic alcoholic and in the occasional drinker, causing a reduction in seminal volume, a reduction in the total number of spermatozoa, and an increase in atypia (Table 1) [97, 103].
Only a few studies showed how moderate alcohol consumption is related to male fertility. Ricci’s human study associated moderate alcohol consumption to an improvement of seminal quality in terms of volume and concentration [98]. Instead, the sub-chronic ingestion of alcohol negatively affects sperm morphology, capacitation parameters, and IVF dynamics on mice. Interestingly, two animal studies have focused on understanding the role of alcohol in the relationship between gut and male fertility. In particular, the work of Li et al. showed that chronic alcohol consumption induces intestinal dysbiosis, which leads to testicular inflammation and impaired sperm quality [104]. In the same way, Aderara et al. sustained that the exacerbating effects of ethanol on ulcerative colitis-induced testicular dysfunction are related to increased oxidative stress and inflammation [105].
Rao et al. conducted a systematic review and a dose-response meta-analysis to evaluate the association between caffeine and alcohol consumption and in vitro fertilization (IVF) and ICSI outcome. The authors reported that men’s weekly alcohol consumption greater than 84 g was associated with decreased live birth rate after IVF/ICSI treatment [106]. In contrast, Karmon et al. reported that the intake of alcohol was directly associated with live birth after assisted reproductive technologies, but not with semen parameters [107]. Instead, caffeine intake seems to be negatively associated with ICSI [107].
An Overview of Dietary Patterns
Mediterranean and Western Diet
Over the last few years, nutritional epidemiology has shown that an adequate caloric intake, the reduced consumption of red meat in favor of white meat, the increased intake of fruit and vegetables, and the replacement of saturated fats with mono fats and polyunsaturated fats benefit parameters of human health, including fertility [108,109,110]. A greater compliance to the Mediterranean Diet (MedDiet) is associated with better semen quality parameters as sperm concentration, total sperm count, total, and progressive motility [111, 112] but not with semen volume [13], in normal subjects, and among men of subfertile couples attempting fertility [113].
Montano et al. studied healthy young men living in highly polluted areas of Italy in a randomized trial, and reported that a lifestyle intervention based on MedDiet and physical activity resulted in an increase of sperm concentration, total and progressive motility, increased percentage of spermatozoa with normal morphology, and a decrease of round cell concentration [114••].
Additionally, other studies have investigated the impact of the MedDiet on male infertility by comparing it to other types of diets including Western diet. The Western diet is characterized by high intakes of pre-packaged foods, refined grains, red meat, processed meat, high-sugar drinks, candy and sweets, and fried foods [115]. In vitro and in vivo studies in rodents have elucidated the consequences of chronic intake of high-fat foods on male fertility. The high-fat diet (HFD) can cause high expression of heat shock protein 60 (HSP60) in spermatozoa triggering apoptosis [116], altered DNA methyltransferase enzymes and global methylation in gonads and testes [117, 118], decreased sperm quality by disrupting energy metabolism in Sertoli cells [119], and aberrations in the testicular proteome [120].
Cutillas-Tolin et al., in their study, showed that the Mediterranean pattern is positively associated with total sperm count. Instead, the Western pattern is positively related to the percentage of morphologically normal sperm and inversely related to sperm concentration among overweight or obese men but not among lean men [121]. The effects of the Mediterranean and Western diet on testicular function showed adverse consequences of high-saturated fatty acids and cholesterol diets on testicular function, supporting benefits of a Mediterranean diet and virgin olive oil to improve male fertility [122].
Yörüsün et al. confirmed that SSB, red meat, and organ meat consumption negatively correlate with sperm parameters. On the other hand, the consumption of fish, egg, and nuts is positively correlated with sperm parameters [123]. Men with higher adherence to a “prudent” or “health-conscious” pattern, a diet rich in fruit, vegetables, whole grains, legumes, nuts, fish, and low-fat dairy products, bearing close resemblance to the Mediterranean pattern, were associated with higher sperm concentration, progressive motility [124], and total sperm [125, 126] and had an inverse association with the odds of infertility [127]. Furthermore, health conscious dietary pattern, which comprises high intakes of fruit, vegetables, fish and other seafood, whole grains and legumes and low intakes of fatty sauces, meat products, refined grains, sugar, and confectionary, was associated with lower sperm DNA damage among subfertile men of couples undergoing IVF/ICSI in the Netherlands [128]. Recently, Muffone et al. conducted a systematic review with meta-analysis to understand whether high MedDiet adherence could be a contributing factor to positive fertility outcomes in infertile men and women. According to this work, the current evidence of high adherence to MedDiet and fertility markers is insufficient to support their clinical application, even though it indicates sperm improvement and a possibility of better pregnancy outcomes [129].
Vegetarian and Vegan Diet
Individuals who follow a vegetarian diet abstain from the consumption of animal meat for cultural, environmental, economic, health, political, or religious reasons. There are different variations of the vegetarian diet such as ovo vegetarians who consume eggs but no dairy products, and lacto-ovo vegetarians who include both milk and eggs in their diet [130]. Conversely, vegans consume only plant products. Generally, most vegetarians replace meat products with soy in their diet to ensure protein intake. A vegetarian diet rich in soy foods has been recognized as healthy for decades, due to the positive effects on metabolic parameters and cardiovascular risk [131] but actually following the identification of isoflavones in soy foods, which exert estrogen-like effects, have been shown to have a negative role on fertility [132,133,134,135,136]. Orzylowska showed that there is a reduction in sperm concentration and motility but no alterations in sperm morphology and sperm chromatin integrity in vegetarians [136]. While in vegans an inefficient sperm hyperactivation was highlighted [136], as well as higher sperm DNA methylation levels in metabolism-related genes [137] and alterated spermatozoa fatty acids composition [138], results obtained in Kljajic’s study supported the favorable effect of a vegan diet on semen parameters as total sperm count, percentage of progressive motility, DNA integrity, and oxidation–reduction potential [139]. Of note, evaluations on the effects of vegetarian diets on male fertility should be integrated, taking into consideration the eventual exposure to pesticides [140], mycotoxins [141], and the eventual shortage of zinc and vitamin B12 [142].
Intermittent Fasting Diet
Intermittent fasting is an increasingly popular strategy for weight loss, but concerns have been raised regarding the effects of fasting on the reproductive health of women and men. Intermittent fasting reduced Te levels and the reductions did not appear to be related to the duration of intervention [143].
Sex hormone binding globulin (SHBG) is the major serum carrier of sex hormones. The reduction of Te lead to intermittent fasting does not impact on SHBG levels [144, 145] probably because the Te became bound to other carriers such as albumin. Low Te levels can negatively affect metabolic health, muscle mass synthesis, and libido in males [143]. However, the reduction of Te impacts on the reduction of fat mass but not to fat-free mass [144, 145]. There is no data in the literature on the impact of intermittent fasting on seminal fluid.
Ketogenic Diet
Ketogenic diet is characterized by a metabolic switch that determines the development of ketosis, as fat is used as a primary source of energy, instead of carbohydrates. The oxidation of the fatty acids determines the production of ketone bodies that are used as fuel by many tissues, including the central nervous system, skeletal muscle, and the heart. It has been developed as an adjuvant therapy in refractory epilepsy in children, and nowadays, it is recommended in severe obesity. Ketogenic diet has also been proposed as an adjuvant therapy for other pathologies, as headache and COVID-19 [146,147,148]. There are few studies advocating the effects of a ketogenic diet on improving fertility, and most have focused on female fertility [62, 149].
In vitro study has demonstrated that ketone bodies are being utilized as an energy source for sperm movement. In an animal study, the ketogenic diet restored the sperm motility, the percentage of sperm with a normal morphology, and spermatogenic cell maturation in HFC-fed mice, even though there was no greater enhancement in Te levels [149]. Omowumi et al. investigated the effects of ketogenic diet in monosodium glutamate (MSG)–induced rat testicular toxicity [150]. MSG is a flavor enhancing food additive found and is a major component of many proteins such as milk, meat, fish, and some vegetables. MSG treatment can cause an alteration of redox status, a reduction of testicular glycogen, a decreasing of NO level, and alteration of lipid profiling. This study showed that ketogenic diet improved the rat bio-chemical parameters as well as the testicular functional indices included testicular: alkaline phosphatase (ALP), acid phosphatase (ACP), cholesterol, protein, glycogen, and testicular lipid profile [150].
In addition, a ketogenic diet with curcumin supplementation could ameliorate Te levels, poor spermatogenesis, sperm parameters as motility and morphology, and reverse oxidative stress; inhibit inflammation; and inhibit apoptosis in the testes of low-carbohydrate-diet-fed mice [151].
Conclusion
Several scientific studies highlighted that unbalanced diet could affect male fertility. Processed meats, dairy products, canned fish, sweets and sugary beverages, soy, and the abuse of alcohol and caffeine have a negative impact on semen quality. Instead, the consumption of fish, fruit, dried fruit, vegetables, legumes, cereals, and low-fat milk benefit male fertility. Among dietary patterns, the Mediterranean diet is positively associated with semen quality, while the Western diet negatively affects spermatogenesis. In the vegetarian diet, results are not clear, but the wide use of soy correlates with deleterious effects on spermatogenesis, probably because of its content of phytoestrogens. Some preliminary results suggest that the ketogenic diet may have a positive impact on spermatogenesis and increase the Te levels in men.
Despite the increasing amount of literature regarding the relationship between male fertility and diet, the current evidence of nutrition and fertility markers is insufficient to support their clinical application. Future research should also consider the need for randomized controlled trials.
Nevertheless, the work-up of the infertile patients should take into consideration also the nutritional aspect, to adjuvate medical therapies and personalize the medical approach. Thus, there is a need for more standardized integration of nutrition counseling into treatment delivery for infertility.
More research is warranted to further elucidate the complex mechanisms between diet and fertility outcomes, and the implications for public health and clinical practice.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kamangar F, Karimi P. The state of nutritional epidemiology: why we are still unsure of what we should eat? Arch Iran Med. 2013;16(8):483–6.
Aggerholm AS, et al. Is overweight a risk factor for reduced semen quality and altered serum sex hormone profile? Fertil Steril. 2008;90(3):619–26.
Smith LB, Walker WH. The regulation of spermatogenesis by androgens. Semin Cell Dev Biol. 2014;30:2–13.
Rosato E, et al. Revisiting the physiological role of androgens in women. Expert Rev Endocrinol Metab. 2022;17(6):547–61.
Sciarra F, et al. Disruption of Circadian rhythms: a crucial factor in the etiology of infertility. Int J Mol Sci. 2020;21(11):3943.
Venkatesh VS, et al. The role of the androgen receptor in the pathogenesis of obesity and its utility as a target for obesity treatments. Obes Rev. 2022;23(6):e13429.
Belloc S, et al. High body mass index has a deleterious effect on semen parameters except morphology: results from a large cohort study. Fertil Steril. 2014;102(5):1268–73.
Aitken RJ. Oxidative stress and the etiology of male infertility. J Assist Reprod Genet. 2016;33(12):1691–2.
Björndahl L, Kirkman Brown J. The sixth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen: ensuring quality and standardization in basic examination of human ejaculates. Fertil Steril. 2022;117(2):246–251.
Hanis T, et al. Effects of dietary trans-fatty acids on reproductive performance of Wistar rats. Br J Nutr. 1989;61(3):519–29.
Imoedemhe DA, et al. The effect of caffeine on the ability of spermatozoa to fertilize mature human oocytes. J Assist Reprod Genet. 1992;9(2):155–60.
Salas-Huetos A, Bulló M, Salas-Salvadó J. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies. Hum Reprod Update. 2017;23(4):371–89.
Ricci E, et al. Mediterranean diet and the risk of poor semen quality: cross-sectional analysis of men referring to an Italian Fertility Clinic. Andrology. 2019;7(2):156–62.
Torres-Arce E, et al. Dietary Antioxidants in the Treatment of Male Infertility: Counteracting Oxidative Stress. Biology (Basel). 2021;10(3).
Bakos HW, et al. The effect of paternal diet-induced obesity on sperm function and fertilization in a mouse model. Int J Androl. 2011;34(5 Pt 1):402–10.
Dimofski P, et al. Consequences of paternal nutrition on offspring health and disease. Nutrients. 2021;13(8).
Pipoyan D, et al. The effect of trans fatty acids on human health: regulation and consumption patterns. Foods. 2021;10(10).
Attaman JA, et al. Dietary fat and semen quality among men attending a fertility clinic. Hum Reprod. 2012;27(5):1466–74.
Jensen TK, et al. High dietary intake of saturated fat is associated with reduced semen quality among 701 young Danish men from the general population. Am J Clin Nutr. 2013;97(2):411–8.
Afeiche MC, et al. Processed meat intake is unfavorably and fish intake favorably associated with semen quality indicators among men attending a fertility clinic. J Nutr. 2014;144(7):1091–8.
Veaute C, et al. Effects of isomeric fatty acids on reproductive parameters in mice. Am J Reprod Immunol. 2007;58(6):487–96.
Ye L, et al. Impacts of immunometabolism on male reproduction. Front Immunol. 2021;12:658432.
Cocuzza M, et al. Clinical relevance of oxidative stress and sperm chromatin damage in male infertility: an evidence based analysis. Int Braz J Urol. 2007;33(5):603–21.
Esmaeili V, et al. Saturated, omega-6 and omega-3 dietary fatty acid effects on the characteristics of fresh, frozen-thawed semen and blood parameters in rams. Andrologia. 2014;46(1):42–9.
•• Liu YS, et al. Associations between meat and vegetable intake, cooking methods, and asthenozoospermia: a hospital-based case-control study in China. Nutrients. 2022;14(9). This article examines a case control study of patients with asthenozoospermia and healthy controls. The associations between meat, unprocessed meat, vegetable, and cooking methods are investigated. Results indicate a correlation between these foods and asthenozoospermia.
Xia W, et al. Men’s meat intake and treatment outcomes among couples undergoing assisted reproduction. Fertil Steril. 2015;104(4):972–9.
Braga DP, et al. Food intake and social habits in male patients and its relationship to intracytoplasmic sperm injection outcomes. Fertil Steril. 2012;97(1):53–9.
Rozati R, et al. Role of environmental estrogens in the deterioration of male factor fertility. Fertil Steril. 2002;78(6):1187–94.
Afeiche M, et al. Dairy food intake in relation to semen quality and reproductive hormone levels among physically active young men. Hum Reprod. 2013;28(8):2265–75.
Wang XB, et al. Dairy product consumption and oligo-astheno-teratozoospermia risk: a hospital-based case-control study in China. Front Nutr. 2021;8:742375.
Eslamian G, et al. Intake of food groups and idiopathic asthenozoospermia: a case-control study. Hum Reprod. 2012;27(11):3328–36.
He H, et al. Lactoferrin alleviates spermatogenesis dysfunction caused by bisphenol A and cadmium via ameliorating disordered autophagy, apoptosis and oxidative stress. Int J Biol Macromol. 2022;222(Pt A):1048–62.
Snoj T, Majdič G. Mechanisms in endocrinology: estrogens in consumer milk: is there a risk to human reproductive health? Eur J Endocrinol. 2018;179(6):R275-r286.
Schaum J, et al. A national survey of persistent, bioaccumulative, and toxic (PBT) pollutants in the United States milk supply. J Expo Anal Environ Epidemiol. 2003;13(3):177–86.
Meeker JD, Hauser R. Exposure to polychlorinated biphenyls (PCBs) and male reproduction. Syst Biol Reprod Med. 2010;56(2):122–31.
Aguilar-Garduño C, et al. Changes in male hormone profile after occupational organophosphate exposure. A longitudinal study. Toxicology. 2013;307:55–65.
Paradisi R, et al. Effects of high doses of recombinant human follicle-stimulating hormone in the treatment of male factor infertility: results of a pilot study. Fertil Steril. 2006;86(3):728–31.
Akram M, et al. Dietary intake of probiotic fermented milk benefits the gut and reproductive health in mice fed with an obesogenic diet. Food Funct. 2022;13(2):737–52.
Hammami I, et al. Kefir milk consumption decreases sperm alterations due to the high-fat diet in adult male rats. Andrologia. 2022;54(7):1631–42.
Ricci E, et al. Dietary habits and semen parameters: a systematic narrative review. Andrology. 2018;6(1):104–16.
•• Madej D, et al. Influence of fruit and vegetable consumption on antioxidant status and semen quality: a cross-sectional study in adult men. Front Nutr. 2021;8:753843.This article examines a cross-sectional study in adult men. The influence of fruit and vegetable consumption on semen quality by reducing oxidative stress was investigated. The results indicate a positive influence of high consumption of fruit and vegetables in sperm quality parameters.
Tremellen K. Oxidative stress and male infertility—a clinical perspective. Hum Reprod Update. 2008;14(3):243–58.
Gharagozloo P, Aitken RJ. The role of sperm oxidative stress in male infertility and the significance of oral antioxidant therapy. Hum Reprod. 2011;26(7):1628–40.
Showell MG, et al. Antioxidants for male subfertility. Cochrane Database Syst Rev. 2014;12:Cd007411.
Yamamoto Y, et al. The effects of tomato juice on male infertility. Asia Pac J Clin Nutr. 2017;26(1):65–71.
Erukainure OL, et al. Strawberry fruit (Fragaria x ananassa Romina) juice attenuates oxidative imbalance with concomitant modulation of metabolic indices linked to male infertility in testicular oxidative injury. Andrologia. 2021;53(9):e14175.
Moghaddam MH, et al. Elderberry diet restores spermatogenesis in the transient scrotal hyperthermia-induced mice. Reprod Sci. 2022;29(12):3373–86.
Beigi Boroujeni M, et al. Effects of pomegranate peel extract on histopathology, testosterone levels and sperm of testicular torsion-detorsion induced in adult Wistar rats. J Complement Integr Med. 2017;14(4).
Amini N, et al. Protective effects of the fruit extract of raspberry (Rubus fruticosus L.) on pituitary-gonadal axis and testicular histopathology in streptozotocin induced diabetic male rats. Avicenna J Phytomed. 2021;11(2):199–209.
Mongioì LM, et al. The role of resveratrol in human male fertility. Molecules. 2021;26(9).
Robbins WA, et al. Walnuts improve semen quality in men consuming a Western-style diet: randomized control dietary intervention trial. Biol Reprod. 2012;87(4):101.
Shehzad M, et al. Therapeutic potential of date palm against human infertility: a review. Metabolites. 2021;11(6).
Salas-Huetos A, et al. Sperm DNA methylation changes after short-term nut supplementation in healthy men consuming a Western-style diet. Andrology. 2021;9(1):260–8.
Sun ZY, et al. Correction: chestnut polysaccharides restore impaired spermatogenesis by adjusting gut microbiota and the intestinal structure. Food Funct. 2022;13(5):3077.
Oresti GM, et al. Differentiation-related changes in lipid classes with long-chain and very long-chain polyenoic fatty acids in rat spermatogenic cells. J Lipid Res. 2010;51(10):2909–21.
Wong WY, et al. Effects of folic acid and zinc sulfate on male factor subfertility: a double-blind, randomized, placebo-controlled trial. Fertil Steril. 2002;77(3):491–8.
Young SS, et al. The association of folate, zinc and antioxidant intake with sperm aneuploidy in healthy non-smoking men. Hum Reprod. 2008;23(5):1014–22.
Goldin BR, et al. Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women. N Engl J Med. 1982;307(25):1542–7.
Santti R, et al. Phytoestrogens: potential endocrine disruptors in males. Toxicol Ind Health. 1998;14(1–2):223–37.
Jargin SV. Soy and phytoestrogens: possible side effects. Ger Med Sci. 2014;12:Doc18.
D’Adamo CR, Sahin A. Soy foods and supplementation: a review of commonly perceived health benefits and risks. Altern Ther Health Med. 2014;20(Suppl 1):39–51.
Hamilton-Reeves JM, et al. Clinical studies show no effects of soy protein or isoflavones on reproductive hormones in men: results of a meta-analysis. Fertil Steril. 2010;94(3):997–1007.
Fielden MR, et al. Effect of human dietary exposure levels of genistein during gestation and lactation on long-term reproductive development and sperm quality in mice. Food Chem Toxicol. 2003;41(4):447–54.
Kang KS, Che JH, Lee YS. Lack of adverse effects in the F1 offspring maternally exposed to genistein at human intake dose level. Food Chem Toxicol. 2002;40(1):43–51.
Kang J, et al. Non-isoflavone phytochemicals in soy and their health effects. J Agric Food Chem. 2010;58(14):8119–33.
Nagao T, et al. Reproductive effects in male and female rats of neonatal exposure to genistein. Reprod Toxicol. 2001;15(4):399–411.
Atanassova N, et al. Comparative effects of neonatal exposure of male rats to potent and weak (environmental) estrogens on spermatogenesis at puberty and the relationship to adult testis size and fertility: evidence for stimulatory effects of low estrogen levels. Endocrinology. 2000;141(10):3898–907.
Beaton LK, et al. Soy protein isolates of varying isoflavone content do not adversely affect semen quality in healthy young men. Fertil Steril. 2010;94(5):1717–22.
Wisniewski AB, et al. Perinatal exposure to genistein alters reproductive development and aggressive behavior in male mice. Physiol Behav. 2005;84(2):327–34.
Salas-Huetos A, et al. Women’s and men’s intake of omega-3 fatty acids and their food sources and assisted reproductive technology outcomes. Am J Obstet Gynecol. 2022;227(2):246.e1-246.e11.
Lenzi A, et al. Fatty acid composition of spermatozoa and immature germ cells. Mol Hum Reprod. 2000;6(3):226–31.
Lenzi A, et al. Polyunsaturated fatty acids of germ cell membranes, glutathione and blutathione-dependent enzyme-PHGPx: from basic to clinic. Contraception. 2002;65(4):301–4.
Safarinejad MR. Effect of omega-3 polyunsaturated fatty acid supplementation on semen profile and enzymatic anti-oxidant capacity of seminal plasma in infertile men with idiopathic oligoasthenoteratospermia: a double-blind, placebo-controlled, randomised study. Andrologia. 2011;43(1):38–47.
Axmon A, Rylander L, Rignell-Hydbom A. Reproductive toxicity of seafood contaminants: prospective comparisons of Swedish east and west coast fishermen’s families. Environ Health. 2008;7:20.
Mocevic E, et al. Environmental mercury exposure, semen quality and reproductive hormones in Greenlandic Inuit and European men: a cross-sectional study. Asian J Androl. 2013;15(1):97–104.
Ghiasvand R, et al. The association between animal flesh foods consumption and semen parameters among infertile Iranian men: a cross-sectional study. Nutr J. 2020;19(1):113.
Miki K. Energy metabolism and sperm function. Soc Reprod Fertil Suppl. 2007;65:309–25.
Ding GL, et al. The effects of diabetes on male fertility and epigenetic regulation during spermatogenesis. Asian J Androl. 2015;17(6):948–53.
Meldgaard M, et al. Consumption of sugar-sweetened or artificially sweetened beverages and semen quality in young men: a cross-sectional study. Int J Environ Res Public Health. 2022;19(2).
Nassan FL, et al. Association between intake of soft drinks and testicular function in young men. Hum Reprod. 2021;36(12):3036–48.
• Kiwitt-Cárdenas J, et al. Sugar-sweetened beverage intake in relation to reproductive parameters in young men. Rev Int Androl. 2022;20(Suppl 1):S39–s47. This article examines a cross-sectional study in men evaluating SSB consumption, reproductive hormones, and seminal analysis. The results indicate an association with SSB intake and sperm morphology and estradiol levels.
Hatch EE, et al. Intake of sugar-sweetened beverages and fecundability in a North American preconception cohort. Epidemiology. 2018;29(3):369–78.
Jurewicz J, et al. Lifestyle and semen quality: role of modifiable risk factors. Syst Biol Reprod Med. 2014;60(1):43–51.
Ricci E, et al. Coffee and caffeine intake and male infertility: a systematic review. Nutr J. 2017;16(1):37.
Wesselink AK, et al. Caffeine and caffeinated beverage consumption and fecundability in a preconception cohort. Reprod Toxicol. 2016;62:39–45.
Ricci E, et al. Maternal and paternal caffeine intake and ART outcomes in couples referring to an Italian fertility clinic: a prospective cohort. Nutrients. 2018;10(8).
Jensen TK, et al. Caffeine intake and semen quality in a population of 2,554 young Danish men. Am J Epidemiol. 2010;171(8):883–91.
Dias TR, et al. Dose-dependent effects of caffeine in human Sertoli cells metabolism and oxidative profile: relevance for male fertility. Toxicology. 2015;328:12–20.
Nabavi N, Todehdehghan F, Shiravi A. Effect of caffeine on motility and vitality of sperm and in vitro fertilization of outbreed mouse in T6 and M16 media. Iran J Reprod Med. 2013;11(9):741–6.
Yang H, et al. Lifestyles associated with human semen quality: results from MARHCS cohort study in Chongqing, China. Medicine (Baltimore). 2015;94(28):e1166.
• Banihani SA, Khaled HJ. Caffeine increased progressive motility of human spermatozoa in normozoospermic and asthenozoospermic semen samples and enhanced activity of seminal creatine kinase. Andrologia. 2021;53(6):e14052. This article examinated the effect of caffeine on motility of human spermatozoa in normozoospermic and asthenozoospermic semen samples. The results indicate a correlation between progressive motility of human spermatozoa with higher concentration of caffeine.
Akomolafe SF, et al. Caffeine improves sperm quality, modulates steroidogenic enzyme activities, restore testosterone levels and prevent oxidative damage in testicular and epididymal tissues of scopolamine-induced rat model of amnesia. J Pharm Pharmacol. 2019;71(10):1565–75.
Kwak Y, Choi H, Roh J. The effects of caffeine on the long bones and testes in immature and young adult rats. Toxicol Res. 2017;33(2):157–64.
Bae J, et al. Dose- and time-related effects of caffeine on the testis in immature male rats. Exp Anim. 2017;66(1):29–39.
Parazzini F, et al. Risk factors for unexplained dyspermia in infertile men: a case-control study. Arch Androl. 1993;31(2):105–13.
Muthusami KR, Chinnaswamy P. Effect of chronic alcoholism on male fertility hormones and semen quality. Fertil Steril. 2005;84(4):919–24.
Silva JV, et al. Study on the short-term effects of increased alcohol and cigarette consumption in healthy young men’s seminal quality. Sci Rep. 2017;7:45457.
Ricci E, et al. Alcohol intake and semen variables: cross-sectional analysis of a prospective cohort study of men referring to an Italian fertility clinic. Andrology. 2018;6(5):690–6.
Lavranos G, et al. Investigating ROS sources in male infertility: a common end for numerous pathways. Reprod Toxicol. 2012;34(3):298–307.
Dobrakowski M, et al. Oxidative stress and motility impairment in the semen of fertile males. Andrologia. 2017;49(10).
Mendes LO, et al. Mast cells and ethanol consumption: interactions in the prostate, epididymis and testis of UChB rats. Am J Reprod Immunol. 2011;66(3):170–8.
Finelli R, Mottola F, Agarwal A. Impact of alcohol consumption on male fertility potential: a narrative review. Int J Environ Res Public Health. 2021;19(1).
La Vignera S, et al. Does alcohol have any effect on male reproductive function? A review of literature. Asian J Androl. 2013;15(2):221–5.
Li H, et al. Chronic alcohol-induced dysbiosis of the gut microbiota and gut metabolites impairs sperm quality in mice. Front Microbiol. 2022;13:1042923.
Adedara IA, et al. Interactive effects of ethanol on ulcerative colitis and its associated testicular dysfunction in pubertal BALB/c mice. Alcohol. 2017;64:65–75.
Rao W, et al. The association between caffeine and alcohol consumption and IVF/ICSI outcomes: a systematic review and dose-response meta-analysis. Acta Obstet Gynecol Scand. 2022;101(12):1351–63.
Karmon AE, et al. Male caffeine and alcohol intake in relation to semen parameters and in vitro fertilization outcomes among fertility patients. Andrology. 2017;5(2):354–61.
Gaskins AJ, Chavarro JE. Diet and fertility: a review. Am J Obstet Gynecol. 2018;218(4):379–89.
Panth N, et al. The influence of diet on fertility and the implications for public health nutrition in the United States. Front Public Health. 2018;6:211.
Nassan FL, Chavarro JE, Tanrikut C. Diet and men’s fertility: does diet affect sperm quality? Fertil Steril. 2018;110(4):570–7.
Salas-Huetos A, et al. Adherence to the Mediterranean diet is positively associated with sperm motility: a cross-sectional analysis. Sci Rep. 2019;9(1):3389.
Caruso P, et al. Effects of Mediterranean diet on semen parameters in healthy young adults: a randomized controlled trial. Minerva Endocrinol. 2020;45(4):280–7.
Karayiannis D, et al. Association between adherence to the Mediterranean diet and semen quality parameters in male partners of couples attempting fertility. Hum Reprod. 2017;32(1):215–22.
•• Montano L, et al. Effects of a lifestyle change intervention on semen quality in healthy young men living in highly polluted areas in Italy: the FASt randomized controlled trial. Eur Urol Focus. 2022;8(1):351–359. The study is a randomized controlled trial conducted in healthy young men. The effects of lifestyle were investigated. The results showed that an intervention based on Mediterranean diet and regular physical activity can determine an improvement of semen quality.
Statovci D, et al. The impact of Western diet and nutrients on the microbiota and immune response at mucosal interfaces. Front Immunol. 2017;8:838.
Cheng L, et al. Abnormal lipid metabolism induced apoptosis of spermatogenic cells by increasing testicular HSP60 protein expression. Andrologia. 2020;52(11): e13781.
Soubry A, et al. Opposing epigenetic signatures in human sperm by intake of fast food versus healthy food. Front Endocrinol (Lausanne). 2021;12: 625204.
Sukur G, Uysal F, Cinar O. High-fat diet induced obesity alters Dnmt1 and Dnmt3a levels and global DNA methylation in mouse ovary and testis. Histochem Cell Biol. 2023;159(4):339–52.
Luo D, et al. High fat diet impairs spermatogenesis by regulating glucose and lipid metabolism in Sertoli cells. Life Sci. 2020;257: 118028.
Jarvis S, et al. High fat diet causes distinct aberrations in the testicular proteome. Int J Obes (Lond). 2020;44(9):1958–69.
Cutillas-Tolín A, et al. Mediterranean and western dietary patterns are related to markers of testicular function among healthy men. Hum Reprod. 2015;30(12):2945–55.
Domínguez-Vías G, et al. Influence of a virgin olive oil versus butter plus cholesterol-enriched diet on testicular enzymatic activities in adult male rats. Int J Mol Sci. 2017;18(8).
Yörüsün T, et al. Nutritional factors related to male fertility: Turkish sample. Afr J Reprod Health. 2020;24(2):85–95.
Gaskins AJ, et al. Dietary patterns and semen quality in young men. Hum Reprod. 2012;27(10):2899–907.
Skoracka K, et al. Diet and nutritional factors in male (in)fertility-underestimated factors. J Clin Med. 2020;9(5).
Cao LL, et al. The effect of healthy dietary patterns on male semen quality: a systematic review and meta-analysis. Asian J Androl. 2022;24(5):549–57.
Haeri F, et al. The relationship between major dietary patterns and fertility status in iranian men: a case-control study. Sci Rep. 2021;11(1):18861.
Vujkovic M, et al. Associations between dietary patterns and semen quality in men undergoing IVF/ICSI treatment. Hum Reprod. 2009;24(6):1304–12.
Muffone A, de Oliveira Lübke PDP, Rabito EI. Mediterranean diet and infertility: a systematic review with meta-analysis of cohort studies. Nutr Rev. 2023;81(7):775–89.
Appleby PN, Key TJ. The long-term health of vegetarians and vegans. Proc Nutr Soc. 2016;75(3):287–93.
Orlich MJ, et al. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med. 2013;173(13):1230–8.
Caceres S, et al. Effects of soya milk on reproductive hormones during puberty in male Wistar rats. Reprod Domest Anim. 2019;54(6):855–63.
Luo Q, et al. Soy isoflavones improve the spermatogenic defects in diet-induced obesity rats through Nrf2/HO-1 pathway. Molecules. 2019;24(16).
Jeminiwa BO, et al. Regulation of the neuroendocrine axis in male rats by soy-based diets is independent of age and due specifically to isoflavone action. Biol Reprod. 2020;103(4):892–906.
Povey AC, et al. Phytoestrogen intake and other dietary risk factors for low motile sperm count and poor sperm morphology. Andrology. 2020;8(6):1805–14.
Orzylowska EM, et al. Food intake diet and sperm characteristics in a blue zone: a Loma Linda Study. Eur J Obstet Gynecol Reprod Biol. 2016;203:112–5.
Franzago M, et al. Sperm DNA methylation at metabolism-related genes in vegan subjects. Front Endocrinol (Lausanne). 2021;12: 633943.
Chamorro R, et al. Diet, plasma, erythrocytes, and spermatozoa fatty acid composition changes in young vegan men. Lipids. 2020;55(6):639–48.
Kljajic M, et al. Impact of the vegan diet on sperm quality and sperm oxidative stress values: a preliminary study. J Hum Reprod Sci. 2021;14(4):365–71.
Chiu YH, et al. Fruit and vegetable intake and their pesticide residues in relation to semen quality among men from a fertility clinic. Hum Reprod. 2015;30(6):1342–51.
Chiminelli I, et al. Emerging mycotoxins and reproductive effects in animals: A short review. J Appl Toxicol. 2022;42(12):1901–9.
Sinclair S. Male infertility: nutritional and environmental considerations. Altern Med Rev. 2000;5(1):28–38.
Cienfuegos S, et al. Effect of intermittent fasting on reproductive hormone levels in females and males: a review of human trials. Nutrients. 2022;14(11).
Moro T, et al. Time-restricted eating effects on performance, immune function, and body composition in elite cyclists: a randomized controlled trial. J Int Soc Sports Nutr. 2020;17(1):65.
Moro T, et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J Transl Med. 2016;14(1):290.
Di Lorenzo C, et al. Applications of ketogenic diets in patients with headache: clinical recommendations. Nutrients. 2021;13(7).
Gangitano E, et al. Ketogenic diet as a preventive and supportive care for COVID-19 patients. Nutrients. 2021;13(3).
Gangitano E, et al. Ketogenic diet for obese COVID-19 patients: is respiratory disease a contraindication? A narrative review of the literature on ketogenic diet and respiratory function. Front Nutr. 2021;8: 771047.
Liu CY, et al. Is a ketogenic diet superior to a high-fat, high-cholesterol diet regarding testicular function and spermatogenesis? Front Nutr. 2022;9: 805794.
Kayode OT, et al. Monosodium glutamate (MSG)-induced male reproductive dysfunction: a mini review. Toxics. 2020;8(1).
Tsao CW, et al. Curcumin remedies testicular function and spermatogenesis in male mice with low-carbohydrate-diet-induced metabolic dysfunction. Int J Mol Sci. 2022;23(17).
Mendiola J, et al. Food intake and its relationship with semen quality: a case-control study. Fertil Steril. 2009;91(3):812–8.
Türk G, et al. Effects of pomegranate juice consumption on sperm quality, spermatogenic cell density, antioxidant activity and testosterone level in male rats. Clin Nutr. 2008;27(2):289–96.
Kara H, et al. Hazelnut consumption improves testicular antioxidant function and semen quality in young and old male rats. Food Chem. 2019;294:1–8.
Chavarro JE, et al. Soy food and isoflavone intake in relation to semen quality parameters among men from an infertility clinic. Hum Reprod. 2008;23(11):2584–90.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
G. P., M. A. V.: conception and design; F. S., G. P.: data collection and interpretation; G. P., F. S., E. G.: wrote the manuscript; M. A. V.: provided suggestions and revised the manuscript for final submission. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there are no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pecora, G., Sciarra, F., Gangitano, E. et al. How Food Choices Impact on Male Fertility. Curr Nutr Rep 12, 864–876 (2023). https://doi.org/10.1007/s13668-023-00503-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-023-00503-x