Abstract
Background
Miscarriage is the most common adverse outcome in early pregnancy; however, high proportion of miscarriages are classified as unexplained. In addition, pregnant women attending early pregnancy assessment units might be more vulnerable.
Aims
The purpose of this study was to explore the risk factors that might be associated with miscarriage among women attending an early pregnancy assessment unit (EPAU).
Methods
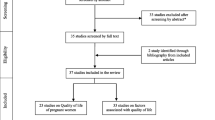
A prospective cohort study was undertaken. The study was conducted on women attending an EPAU at a large, tertiary hospital. A detailed lifestyle questionnaire was completed. In addition, data from validated psychometric scales were collected. Participants were followed up to determine pregnancy outcome. The relative risk was calculated to estimate the probability of having a miscarriage for all independent variables.
Results
A total sample of 293 women were included in this study. Well-established risk factors for miscarriage were found in this group including advanced maternal age and high-risk pregnancy (i.e. threatened miscarriage and recurrent miscarriage). In addition, lack of emotional wellbeing did contribute to an increased risk of miscarriage. Conversely, presenting with nausea or low-medium energy levels early in pregnancy were associated with a decreased risk of miscarriage. Finally, our results did not find any association between stressful life events, general health and lifestyle factors in this group.
Conclusions
Our findings indicated that maternal, psychological and obstetric factors may have an influence on miscarriage among women attending an EPAU. The insight of a relationship between emotional wellbeing and miscarriage opens a window for prevention in this area.
Similar content being viewed by others
References
Royal College of Physicians of Ireland (2010) Ultrasound diagnosis of early pregnancy miscarriage. RCPI, Republic of Ireland
Royal College of Physicians of Ireland (2017) The management of second trimester miscarriage. RCPI, Republic of Ireland
Macklon NS, Geraedts JPM, Fauser BCJM (2002) Conception to ongoing pregnancy: the ‘black box’ of early pregnancy loss. Hum Reprod Update 8(4):333–343
Zinaman MJ, Clegg ED, Brown CC, O’Connor J, Selevan SG (1996) Estimates of human fertility and pregnancy loss. Fertil Steril 65(3):503–509
Morris A, Meaney S, Spillane N, O'donoghue K (2015) 611: the postnatal morbidity associated with second-trimester miscarriage. Am J Obstet Gynecol 212(1):S303–S304 -65
Royal College of Obstetricians and Gynaecologists. The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage. No 17, Green-top Guideline. Royal College of Obstetricians and Gynaecologists; 2011
Zhang T, Sun Y, Chen Z, Li T (2018) Traditional and molecular chromosomal abnormality analysis of products of conception in spontaneous and recurrent miscarriage. BJOG 125(4):414–420
Zhou H, Liu YP, Liu L, Zhang M, Chen XZ, Qi YL (2016) Maternal pre-pregnancy risk factors for miscarriage from a prevention perspective: a cohort study in China. Eur J Obstet Gyn R B 206:57–63
Prior M, Bagness C, Brewin J, Coomarasamy A, Easthope L, Hepworth-Jones B, Hinshaw K, O'Toole E, Orford J, Regan L, Raine-Fenning N (2017) Priorities for research in miscarriage: a priority setting partnership between people affected by miscarriage and professionals following the James Lind Alliance methodology. BMJ Open 7(8):e016571
Maconochie N, Doyle P, Prior S, Simmons R (2007) Risk factors for first trimester miscarriage—results from a UK-population-based case–control study. BJOG 114(2):170–186
Feodor Nilsson S, Andersen PK, Strandberg-Larsen K, Nybo Andersen AM (2014) Risk factors for miscarriage from a prevention perspective: a nationwide follow-up study. BJOG 121(11):1375–1385
Hemming K (2014) Causation or association: running before we can walk? BJOG 121(11):1385
Turner MJ, Fattah C, O’Connor N, Farah N, Kennelly M, Stuart B (2010) Body mass index and spontaneous miscarriage. Eur J Obstet Gynecol Reprod Biol 151(2):168–170
Louis GMB, Sapra KJ, Schisterman EF, Lynch CD, Maisog JM, Grantz KL et al (2016) Lifestyle and pregnancy loss in a contemporary cohort of women recruited before conception: the LIFE study. Fertil Steril 106(1):180–188
Farren J, Mitchell-Jones N, Verbakel JY, Timmerman D, Jalmbrant M, Bourne T (2018) The psychological impact of early pregnancy loss. Hum Reprod Update 24:731–749
Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W (2009) Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Med 20(3):189–209
Mitchell J, Goodman J Comparative effects of antidepressant medications and untreated major depression on pregnancy outcomes: a systematic review. Arch Womens Ment Health 21(5):505–516
Arck PC, Rucke M, Rose M, Szekeres-Bartho J, Douglas AJ, Pritsch M et al (2008) Early risk factors for miscarriage: a prospective cohort study in pregnant women. Reprod BioMed Online 17(1):101–113
Milad MP, Klock SC, Moses S, Chatterton R (1998) Stress and anxiety do not result in pregnancy wastage. Hum Reprod 13(8):2296–2300
Nelson DB, Grisso JA, Joffe MM, Brensinger C, Shaw L, Datner E (2003) Does stress influence early pregnancy loss? Ann Epidemiol 13(4):223–229
Lynch CD, Sundaram R, Maisog JM, Sweeney AM, Buck Louis GM (2014) Preconception stress increases the risk of infertility: results from a couple-based prospective cohort study—the LIFE study. Hum Reprod 29(5):1067–1075
Lynch CD, Sundaram R, Buck Louis GM (2018) Biomarkers of preconception stress and the incidence of pregnancy loss. Hum Reprod 33:728–735
Bigrigg MA, Read MD (1991) Management of women referred to early pregnancy assessment unit: care and cost effectiveness. BMJ 302(6776):577–579
O'Keeffe LM, Kearney PM, Greene RA (2013) Surveillance during pregnancy: methods and response rates from a hospital based pilot study of the pregnancy risk assessment monitoring system in Ireland. BMC Pregnancy Childbirth 13:180
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396
Hays RD, Morales LS (2001) The RAND-36 measure of health-related quality of life. Ann Med 33(5):350–357
Steward AL, Sherbourne C, Hayes RD et al (1992) Summary and discussion of MOS measures. In: Stewart AL, Ware JE (eds) Measuring functioning and well-being: the medical outcome study approach. Duke University Press, Durham, NC, pp 345–371
Webster J, Linnane JW, Dibley LM, Hinson JK, Starrenburg SE, Roberts JA (2000) Measuring social support in pregnancy: can it be simple and meaningful? Birth 27(2):97–101
Scheier MF, Carver CS, Bridges MW (1994) Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. J Pers Soc Psychol 67(6):1063–1078
Tunde-Byass M, Cheung VY (2009) The value of the early pregnancy assessment clinic in the management of early pregnancy complications. J Obstet Gynaecol Can 31(9):841–844
Andersen AMN, Wohlfahrt J, Christens P, Olsen J, Melbye M (2000) Maternal age and fetal loss: population based register linkage study. BMJ 320(7251):1708–1712
Saraswat L, Bhattacharya S, Maheshwari A (2010) Maternal and perinatal outcome in women with threatened miscarriage in the first trimester: a systematic review. BJOG 117(3):245–257
Kenny LC, Lavender T, McNamee R, O’Neill SM, Mills T, Khashan AS (2013) Advanced maternal age and adverse pregnancy outcome: evidence from a large contemporary cohort. PLoS One 8(2):e56583
Hasan R, Baird DD, Herring AH, Olshan AF, Funk ML, Hartmann KE (2010) Patterns and predictors of vaginal bleeding in the first trimester of pregnancy. Ann Epidemiol 20(7):524–531
Bruckner TA, Mortensen LH, Catalano RA (2016) Spontaneous pregnancy loss in Denmark following economic downturns. Am J Epidemiol 183(8):701–708
Armstrong BG, Mcdonald AD, Sloan M (1992) Cigarette, alcohol, and coffee consumption and spontaneous-abortion. Am J Public Health 82(1):85–87
Wisborg K, Kesmodel U, Henriksen TB, Hedegaard M, Secher NJ (2003) A prospective study of maternal smoking and spontaneous abortion. Acta Obstet Gynecol Scand 82(10):936–941
Lee KA, Zaffke M (1999) Longitudinal changes in fatigue and energy during pregnancy and the postpartum period. J Obstet Gynecol Neonatal Nurs 28(2):183–191
Nakamura K, Sheps S, Arck PC (2008) Stress and reproductive failure: past notions, present insights and future directions. J Assist Reprod Genet 25(2–3):47–62
Qu F, Wu Y, Zhu YH, Barry J, Ding T, Baio G, Muscat R, Todd BK, Wang FF, Hardiman PJ (2017) The association between psychological stress and miscarriage: a systematic review and meta-analysis. Sci Rep 7(1):1731
National Health System (2018) Causes: miscarriage United Kingdown: National Health System; [Available from: https://www.nhs.uk/conditions/miscarriage/causes/. Accessed 7 Feb 2018
Meaney S, Corcoran P, Gallagher S, Lutomski JE, Spillane N, O'Donoghue K (2014) Perceived maternal stress and emotional wellbeing as risk factors for miscarriage. Arch Dis Child Fetal Neonatal Ed 99:A1–A180
Bailey S, Bailey C, Boivin J, Cheong Y, Reading I, Macklon N (2015) A feasibility study for a randomised controlled trial of the positive reappraisal coping intervention, a novel supportive technique for recurrent miscarriage. BMJ Open 5(4):e007322
Campillo IS, Meaney S, McNamara K, O'Donoghue K (2017) Psychological and support interventions to reduce levels of stress, anxiety or depression on women’s subsequent pregnancy with a history of miscarriage: an empty systematic review. BMJ Open 7(9):e017802
Acknowledgments
We are grateful to the women for participating in the study and giving of their time freely.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 42 kb)
Rights and permissions
About this article
Cite this article
San Lazaro Campillo, I., Meaney, S., Corcoran, P. et al. Risk factors for miscarriage among women attending an early pregnancy assessment unit (EPAU): a prospective cohort study. Ir J Med Sci 188, 903–912 (2019). https://doi.org/10.1007/s11845-018-1955-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1955-2