Abstract
The present study used triggered electromyographic (EMG) testing as a tool to determine the safety of pedicle screw placement. In this Institutional Review Board exempt review, data from 151 consecutive patients (100 robotic; 51 non-robotic) who had undergone instrumented spinal fusion surgery of the thoracic, lumbar, or sacral regions were analyzed. The sizes of implanted pedicle screws and EMG threshold data were compared between screws that were placed immediately before and after adoption of the robotic technique. The robotic group had significantly larger screws inserted that were wider (7 ± 0.7 vs 6.5 ± 0.3 mm; p < 0.001) and longer (47.8 ± 6.4 vs 45.7 ± 4.3 mm; p < 0.001). The robotic group also had significantly higher stimulation thresholds (34.0 ± 11.9 vs 30.2 ± 9.8 mA; p = 0.002) of the inserted screws. The robotic group stayed in the hospital postoperatively for fewer days (2.3 ± 1.2 vs 2.9 ± 2 days; p = 0.04), but had longer surgery times (174 ± 37.8 vs 146 ± 41.5 min; p < 0.001). This study demonstrated that the use of navigated, robot-assisted surgery allowed for placement of larger pedicle screws without compromising safety, as determined by pedicle screw stimulation thresholds. Future studies should investigate whether these effects become even stronger in a later cohort after surgeons have more experience with the robotic technique. It should also be evaluated whether the larger screw sizes allowed by the robotic technology actually translate into improved long-term clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pedicle screw fixation in spinal surgery is a widely accepted procedure to correct spinal alignment, provide stabilization following neural decompression, and allow fusion to occur [1,2,3,4,5,6]. Pedicle screw placement in the lumbar and lower thoracic areas provides spinal fixation while decreasing the risk of postoperative complications [2, 7]. However, the pedicle is surrounded by many sensitive biological entities such as the nerve roots, and these are usually not completely visualized during pedicle screw insertion. Pedicle screw misplacement may therefore lead to peripheral nerve injury in the lumbosacral spine [7, 8]. This occurs in approximately 4.2% of patients, and nerve injury may lead to serious postoperative motor and sensory deficits along with patient immobility, discomfort, and pain [7,8,9].
Computer-assisted navigation and surgical robotics are becoming increasingly common because they offer the abilities to direct and confirm pedicle screw placement with increased accuracy. These technologies also may decrease radiation exposure to the surgical staff, and decrease surgery and recovery time [10,11,12].
Triggered electromyograph(ic) (EMG) or pedicle stimulation is a technique that involves the electrical stimulation of a pedicle opening or screw to evoke muscle action potential and subsequent contractions of muscle fibers that can be recorded by carefully placed electrodes [13]. The number of milliamps required to evoke a muscle response can be measured as a threshold value, and this value will differ depending on the proximity of the stimulation source to the nerve root, as well as the conductivity of the intervening tissue. High stimulation thresholds indicate a safe screw placement due to increased resistance to current flow, whereas low stimulation thresholds are indicative of a pedicle screw breach, or proximity to an exiting or traversing nerve root [14,15,16]. Studies have shown that the use of EMG monitoring may increase the safety of pedicle screw placement by detecting pedicle wall breaches, and may thereby minimize the risk of patient injury [14, 17] (Fig. 1).
Although previous studies in the literature have investigated the accuracy of screws placed with the assistance of robots [18,19,20], studies exploring the safety of robotic-assisted screw placement are limited. To the authors’ knowledge, this is the first study to compare EMG stimulation threshold (STIM) data of patients who underwent spinal fusion surgery with robot-navigated assistance to that of patients who had spinal fusion surgery without the use of robotic technology. The purpose of this study is to retrospectively compare the sizes of inserted pedicle screws and STIM measurements between robotic versus non-robotic cohorts.
Materials and methods
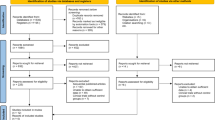
A retrospective institutional review board-exempt study was conducted of 151 consecutive patients who underwent instrumented spinal fusion surgery of the thoracic, lumbar, or sacral regions at a single facility. The first 100 patients who underwent surgery at this location with navigated, robotic assistance utilizing the ExcelsiusGPS® robot (Globus Medical, Inc., Audubon, PA, USA) were compared to the 51 patients who underwent free-hand/fluoroscopically guided surgery immediately prior to adoption of this robotic technique. All of the surgeries occurred between May 2017 and December 2018. The robotic technique was implemented in December 2017, and so all surgeries in the study after that point were performed with robotic assistance. All adult patients who had undergone spine surgery with posterior stabilization were included in the study to encompass the first 100 robotic patients and as far back as possible prior to robot adoption for which triggered EMG threshold values were able to be obtained. A midline open surgical technique was performed in all 51 non-robotic and in 69 of the 100 robotic surgeries, while the remaining surgeries used a Wiltse paraspinal minimally invasive approach [21]. Data were collected retrospectively from patient records without any identifying information. Patient demographics, intraoperative, and EMG threshold data were analyzed. STIM measurements were obtained by placing the stimulation probe on the shaft of the screw after the screw had been inserted. STIM measurements that were recorded intraoperatively as a range were entered in the final analysis as the lowest value in the range.
Navigated, robot-assisted pedicle screw positioning system
All screws in the robotic group were inserted utilizing the robot positioning system (Excelsius GPS®; Globus Medical, Inc. Audubon, PA, USA). This system uses real-time surgical navigation and robotic direction in conjunction with a dynamic reference base and positioning camera to guide pedicle screw placement. This system allows for preoperative planning, followed by robotic-assisted intraoperative implant placement with navigated instruments.
Statistical analysis
Data were analyzed using SPSS v20.0.0 software for Windows (IBM Corp., Armonk, New York). Demographic data such as age and body mass index (BMI) were reported as averages, while gender and diagnosis were reported as frequencies. Intraoperative data such as surgical time, radiation time, blood loss, and length of stay were reported as averages, while treatment type, surgical level and intraoperative complications were reported as frequencies. Parametric and nonparametric tests were used to assess differences between groups. Statistical significance level was set at 0.05.
Results
The most common indications for fusion surgery were degenerative spondylolisthesis and stenosis (64%) followed by iatrogenic instability (16%).
Demographic characteristics were similar between the robotic and non-robotic groups (Table 1). Fifty-four percent of patients in the robotic and 55% in the non-robotic group were female. The mean patient ages were 63 and 64 for the robotic and non-robotic groups, respectively. The mean patient BMIs were 31.2 and 29.7 kg/m2 for the robotic and non-robotic groups, respectively.
Operative data and differences between groups can be found in Table 2. No significant differences between groups were observed for fluoroscopy time or blood loss. Postoperative hospital stays for the robotic group were significantly shorter than for the non-robotic group (2.3 ± 1.2 vs 2.9 ± 1.9 days; p = 0.04), while the non-robotic group had significantly shorter operative times (174 ± 37.8 vs 146 ± 41.5 min; p < 0.001). The robotic group had a mean of 4.5 screws and 2.3 vertebrae per patient, whereas the non-robotic group had a mean of 4.7 screws and 2.4 vertebrae per patient.
There were 434 pedicle screws analyzed in the robotic group and 243 screws analyzed in the non-robotic group. The screw diameter and length were significantly greater in the robotic group compared to the non-robotic group (p < 0.001). Of the pedicle screws with STIM data available (619 screws), STIM threshold values for the robotic group were significantly higher than for the non-robotic group (n = 432; 34.0 ± 11.9 mA, and n = 187; 30.2 ± 9.8 mA, respectively; p = 0.002).
No complications occurred that were attributable to robotic technique. There were no implant failures and no revision or removal of implants within 1 year after the surgical dates for any patients. Within 1.5 years of the surgical dates, 1 patient in the non-robotic group suffered bilateral S1 pedicle screw fractures with pseudoarthrosis and required revision fusion surgery. No robotic surgery patients required hardware revision within 1.5 years of follow-up.
Discussion
The present study compared pedicle screw sizes and placement safety using threshold stimulation measurements in patients who had surgery with or without robotic technology. Based on STIM values, it appears that robotic guidance allows for safe placement of pedicle screws as demonstrated by average STIM threshold. This held true even though, on average, 0.5 mm larger screws, which have the greatest risk of pedicle breach, were placed in the robotic group.
It is a common strategy to utilize pedicle screw fixation to stabilize the thoracic and lumbar spine in the instrumented correction of spinal pathologies [2, 22, 23]. Mispositioned pedicle screws may lead to a number of potentially life-threatening complications such as neurovascular damage, dural tearing, pain, and excessive bleeding, among others [24]. The free-hand technique with fluoroscopic guidance is currently the most utilized method of pedicle screw implantation. However, there are numerous disadvantages to this approach such as increased intraoperative radiation exposure and the potential of violation of facet joint during screw insertion (with less accurate screw positions) compared to robot-assisted surgery [24, 25].
Intraoperative validation of pedicle screw position is an extremely useful strategy for verifying screw position. One technique to check screw position is triggered EMG testing. Numerous studies have investigated the reliability of triggered EMG testing for identifying potential mispositioned screws, reporting a specificity of 0.94 [26]. Using triggered EMG testing provides the surgeon with real-time monitoring of potential hazards. Electrical stimulation near a nerve causes a subsequent muscle action potential from the myotomes innervated by the nerve roots close to the stimulated instrument [13]. Therefore, a positive response at a relatively low threshold is indicative of pedicle wall breach, and is considered a warning sign of poor implant position and potential neurologic injury [14, 15].
In recent years, robotic guidance systems have been developed as a means to decrease pedicle screw mispositioning. This is accomplished through the robot’s ability to use real-time image guidance and navigational capabilities [10, 20, 27,28,29]. Many studies claim that robotic guidance during surgery allows for improved screw placement with up to 99% screw placement accuracy, while others have reported equal or less accurate placement when comparing other methods of screw insertion with robotic technology [18,19,20, 30, 31]. These inconsistencies necessitate the need for studies such as this one to investigate the safety of using robotic technology in spinal surgery.
Results of the present study suggest that the use of robotic technology increases operative time by about 30 min. However, it should be noted that this study focused on the initial 100 consecutive patients after adoption of robotic technology. There is likely a learning curve associated with incorporating robotic technology, and operative times typically decrease with more experience and newer-generation software. For example, there was a significant difference (p < 0.01) in the average operative time in the robotic group between the first 14 cases of minimally invasive, one-level transforaminal fusion (TLIF) (177 min) and the last 14 cases (131 min). Additionally, by adopting the robotic technology, the surgeon could do more MIS surgeries so that a remarkable number of minimally invasive surgeries (one-third of the cohort) were performed in the robotic group, and that could have influenced the change in operative times. Patients who underwent surgery with the use of robotic technology had fewer postoperative days in the hospital compared to the non-robotic group. This finding is likely mostly due to the presence of minimally invasive cases in the robotic group, as minimally invasive approaches have been associated with shorter-length hospital stays [32]. While there was no significant difference in the length of hospital stays between robotic and non-robotic open cases (p = 0.18), the MIS robotic patients had significantly shorter lengths of stay compared to the open non-robotic cases (2.3 vs 2.9 days, respectively; p = 0.04).
This is the first study to use triggered EMG thresholds to compare pedicle screw placement in spinal surgery between robotic and non-robotic surgical patients. These thresholds can be seen as a surrogate marker of the safety of the implanted screw position. Based on the operative findings (Table 2), screw diameter and length were significantly greater in the robotic group. The use of larger screws is advantageous because it allows for increased stability [33, 34]. However, larger screw size can translate to increased risk of screw misplacement because there is less room for error [35]. Additionally, screws with wider diameters also have less electrical resistance, and this also could potentially lower the STIM threshold. Despite this, the robotic group still had significantly higher STIM values compared to the non-robotic group (p = 0.002), suggesting that surgeons may be able to use larger pedicle screws without compromising safety by utilizing robotic technology.
There are inconsistencies in the literature with regard to a STIM safety threshold [36, 37]. However, it does appear that most authors hover around 8 mA as a threshold to denote what is considered safe for the patient, with anything below 8 mA being potentially harmful, especially with the lumbar pedicle screws in which the test has a higher sensitivity and specificity [13, 37, 38]. Screw placement was acceptable and considered safe in both cohorts based on the average STIM thresholds (34 and 30 mA). However, since there were significantly higher STIM scores in the robotic group even though the screws were significantly larger, these results suggest that robotic assistance allows for larger screws to be placed without compromising patient safety.
These results should be interpreted within the confines of study limitations. The generalizability of these results is limited, as the current study is a retrospective review of data from a single surgeon at a single facility. These data suggest that the robotic technique may limit future problems and the need for additional surgery, since one patient in the non-robotic group required revision surgery within 1.5 years after the primary surgery, while no robotic surgery patients required revision within the same time frame. Future studies are needed, however, to determine conclusively if the larger pedicle screw sizes made possible with robotic technology actually translate into improved long-term clinical outcomes. The high STIM thresholds in this study suggest that the robotic technique allows for insertion of large screws without compromising safety.
Conclusion
The results of the present study indicate that the use of robotic navigation and guidance during spinal surgery allows larger pedicle screws to be inserted without compromising safety, as determined by the surrogate marker of STIM threshold values.
References
Perna F, Borghi R, Pilla F, Stefanini N, Mazzotti A, Chehrassan M (2016) Pedicle screw insertion techniques: an update and review of the literature. Musculoskelet Surg 100(3):165–169
Gaines RW Jr (2000) The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am 82(10):1458–1476
Kotani Y, Abumi K, Ito M, Sudo H, Abe Y, Minami A (2012) Mid-term clinical results of minimally invasive decompression and posterolateral fusion with percutaneous pedicle screws versus conventional approach for degenerative spondylolisthesis with spinal stenosis. Eur Spine J 21(6):1171–1177
Zhou Y, Zhang C, Wang J, Chu TW, Li CQ, Zhang ZF, Zheng WJ (2008) Endoscopic transforaminal lumbar decompression, interbody fusion and pedicle screw fixation-a report of 42 cases. Chin J Traumatol 11(4):225–231
Kaiser MG, Eck JC, Groff MW, Watters WC 3rd, Dailey AT, Resnick DK, Choudhri TF, Sharan A, Wang JC, Mummaneni PV et al (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 1: introduction and methodology. J Neurosurg Spine 21(1):2–6
Zhao Y, Yang S, Ding W (2019) Unilateral versus bilateral pedicle screw fixation in lumbar fusion: a systematic review of overlapping meta-analyses. PLoS ONE 14(12):e0226848
Hicks JM, Singla A, Shen FH, Arlet V (2010) Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 35(11):E465-470
Du JY, Wu JS, Wen ZQ, Lin XJ (2016) Treatment strategies for early neurological deficits related to malpositioned pedicle screws in the lumbosacral canal: a pilot study. Bone Joint Res 5(2):46–51
Rahyussalim AJ, Saleh I, Armin MF, Kurniawati T, Safri AY (2016) Pedicle screw position changing policy for nerve injury problems during screw insertion on thoracolumbar compression fractures. Int J Surg Case Rep 28:155–160
Stull JD, Mangan JJ, Vaccaro AR, Schroeder GD (2019) Robotic guidance in minimally invasive spine surgery: a review of recent literature and commentary on a developing technology. Curr Rev Musculoskelet Med 12(2):245–251
Bertelsen A, Melo J, Sanchez E, Borro D (2013) A review of surgical robots for spinal interventions. Int J Med Robot 9(4):407–422
Galetta MS, Leider JD, Divi SN, Goyal DKC, Schroeder GD (2019) Robotics in spinal surgery. Ann Transl Med 7(Suppl 5):S165
Lee CH, Kim HW, Kim HR, Lee CY, Kim JH, Sala F (2015) Can triggered electromyography thresholds assure accurate pedicle screw placements? A systematic review and meta-analysis of diagnostic test accuracy. Clin Neurophysiol 126(10):2019–2025
Calancie B, Donohue ML, Moquin RR (2014) Neuromonitoring with pulse-train stimulation for implantation of thoracic pedicle screws: a blinded and randomized clinical study. Part 2. The role of feedback. J Neurosurg Spine 20(6):692–704
Samdani AF, Tantorski M, Cahill PJ, Ranade A, Koch S, Clements DH, Betz RR, Asghar J (2011) Triggered electromyography for placement of thoracic pedicle screws: is it reliable? Eur Spine J 20(6):869–874
Gonzalez AA, Jeyanandarajan D, Hansen C, Zada G, Hsieh PC (2009) Intraoperative neurophysiological monitoring during spine surgery: a review. Neurosurg Focus 27(4):E6
Wood MJ, McMillen J (2014) The surgical learning curve and accuracy of minimally invasive lumbar pedicle screw placement using CT based computer-assisted navigation plus continuous electromyography monitoring - a retrospective review of 627 screws in 150 patients. Int J Spine Surg 8:27
Fan Y, Du JP, Liu JJ, Zhang JN, Qiao HH, Liu SC, Hao DJ (2018) Accuracy of pedicle screw placement comparing robot-assisted technology and the free-hand with fluoroscopy-guided method in spine surgery: an updated meta-analysis. Medicine (Baltimore) 97(22):e10970
Laudato PA, Pierzchala K, Schizas C (2018) Pedicle screw insertion accuracy using O-arm, robotic guidance, or freehand technique: a comparative study. Spine (Phila Pa 1976) 43(6):E373–E378
Ringel F, Stuer C, Reinke A, Preuss A, Behr M, Auer F, Stoffel M, Meyer B (2012) Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine (Phila Pa 1976) 37(8):E496-501
Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE (1968) The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 50(5):919–926
Kosmopoulos V, Schizas C (2007) Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 32(3):E111-120
Tukkapuram VR, Kuniyoshi A, Ito M (2019) A review of the historical evolution, biomechanical advantage, clinical applications, and safe insertion techniques of cervical pedicle screw fixation. Spine Surg Relat Res 3(2):126–135
Aoude AA, Fortin M, Figueiredo R, Jarzem P, Ouellet J, Weber MH (2015) Methods to determine pedicle screw placement accuracy in spine surgery: a systematic review. Eur Spine J 24(5):990–1004
Gao S, Lv Z, Fang H (2018) Robot-assisted and conventional freehand pedicle screw placement: a systematic review and meta-analysis of randomized controlled trials. Eur Spine J 27(4):921–930
Mikula AL, Williams SK, Anderson PA (2016) The use of intraoperative triggered electromyography to detect misplaced pedicle screws: a systematic review and meta-analysis. J Neurosurg Spine 24(4):624–638
Benech CA, Perez R, Benech F, Greeley SL, Crawford N, Ledonio C (2020) Navigated robotic assistance results in improved screw accuracy and positive clinical outcomes: an evaluation of the first 54 cases. J Robot Surg 14(3):431–437
Wallace DJ, Vardiman AB, Booher GA, Crawford NR, Riggleman JR, Greeley SL, Ledonio CG (2020) Navigated robotic assistance improves pedicle screw accuracy in minimally invasive surgery of the lumbosacral spine: 600 pedicle screws in a single institution. Int J Med Robot 16(1):e2054
Joseph JR, Smith BW, Liu X, Park P (2017) Current applications of robotics in spine surgery: a systematic review of the literature. Neurosurg Focus 42(5):E2
van Dijk JD, van den Ende RP, Stramigioli S, Kochling M, Hoss N (2015) Clinical pedicle screw accuracy and deviation from planning in robot-guided spine surgery: robot-guided pedicle screw accuracy. Spine (Phila Pa 1976) 40(17):E986-991
Devito DP, Kaplan L, Dietl R, Pfeiffer M, Horne D, Silberstein B, Hardenbrook M, Kiriyanthan G, Barzilay Y, Bruskin A et al (2010) Clinical acceptance and accuracy assessment of spinal implants guided with SpineAssist surgical robot: retrospective study. Spine (Phila Pa 1976) 35(24):2109–2115
Uribe JS, Beckman J, Mummaneni PV, Okonkwo D, Nunley P, Wang MY, Mundis GM Jr, Park P, Eastlack R, Anand N et al (2017) Does MIS surgery allow for shorter constructs in the surgical treatment of adult spinal deformity? Neurosurgery 80(3):489–497
Karami KJ, Buckenmeyer LE, Kiapour AM, Kelkar PS, Goel VK, Demetropoulos CK, Soo TM (2015) Biomechanical evaluation of the pedicle screw insertion depth effect on screw stability under cyclic loading and subsequent pullout. J Spinal Disord Tech 28(3):E133-139
Saraf SK, Singh RP, Singh V, Varma A (2013) Pullout strength of misplaced pedicle screws in the thoracic and lumbar vertebrae—a cadaveric study. Indian J Orthop 47(3):238–243
Gonzalvo A, Fitt G, Liew S, de la Harpe D, Vrodos N, McDonald M, Rogers MA, Wilde PH (2015) Correlation between pedicle size and the rate of pedicle screw misplacement in the treatment of thoracic fractures: can we predict how difficult the task will be? Br J Neurosurg 29(4):508–512
Kaliya-Perumal AK, Charng JR, Niu CC, Tsai TT, Lai PL, Chen LH, Chen WJ (2017) Intraoperative electromyographic monitoring to optimize safe lumbar pedicle screw placement—a retrospective analysis. BMC Musculoskelet Disord 18(1):229
Raynor BL, Lenke LG, Bridwell KH, Taylor BA, Padberg AM (2007) Correlation between low triggered electromyographic thresholds and lumbar pedicle screw malposition: analysis of 4857 screws. Spine (Phila Pa 1976) 32(24):2673–2678
Wilson B, Curtis E, Hirshman B, Oygar A, Chen K, Gabel BC, Vaida F, Allison DW, Ciacci JD (2017) Lateral mass screw stimulation thresholds in posterior cervical instrumentation surgery: a predictor of medial deviation. J Neurosurg Spine 26(3):346–352
Funding
No grants/external fund was received in support of this study.
Author information
Authors and Affiliations
Contributions
CK provided the clinical data, generated concept and designed the study DMB helped with data analysis and editing the manuscript NT drafted the manuscript, did the analysis BB supervised and directed the study, helped with editing
Corresponding author
Ethics declarations
Conflict of interest
CWK: has research support from Globus Medical Inc., BB and NT: employee with stock options from Globus Medical Inc.
Ethical approval
Western Institutional Review Board’s (WIRB’s) IRB Affairs Department reviewed the study under the Common Rule and applicable guidance. The study is exempt because Information, is recorded by the investigator in such a manner that the identity of the human subjects cannot readily be ascertained directly or through identifiers linked to the subjects, the investigator does not contact the subjects, and the investigator will not re-identify subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kanaly, C.W., Backes, D.M., Toossi, N. et al. Robotic-assisted spine surgery allows for increased pedicle screw sizes while still improving safety as indicated by elevated triggered electromyographic thresholds. J Robotic Surg 17, 1007–1012 (2023). https://doi.org/10.1007/s11701-022-01493-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-022-01493-8