Abstract
Background
Despite recent approvals of lifesaving treatments for chronic lymphocytic leukemia (CLL), real-world data on the tolerability of the Bruton tyrosine kinase inhibitor ibrutinib for CLL treatment are lacking, especially in Black patients.
Objective
To expand upon a previously reported retrospective chart review of ibrutinib-treated patients with CLL to increase the number of sites and the enrollment period in first-line (1L) and relapsed/refractory (R/R) settings with a subanalysis based on ethnicity.
Patients and Methods
Adults with CLL who initiated ibrutinib treatment from five centers were followed for ≥ 6 months.
Results
We identified 482 patients with CLL [405 White (153 1L, 252 R/R), 37 Black (17 1L, 20 R/R), 40 other/unidentified]. At baseline, 58.5% of all patients (68.8% of Black patients) had hypertension. At a median follow-up of 28.2 months, 31.1% of patients overall discontinued ibrutinib, 16.2% due to adverse events (12.2% 1L, 18.8% R/R). Overall, 46.0% of patients experienced ≥ 1 dose hold (40.2% 1L, 49.8% R/R), and 28.8% of patients experienced ≥ 1 dose reduction (24.9% 1L, 31.4% R/R). Among Black patients, ibrutinib was discontinued in 24.3% of patients (17.6% 1L, 30.0% R/R), 8.1% due to disease progression and 5.4% due to adverse events; 40.5% of patients experienced ≥ 1 dose hold (35.3% 1L, 45.0% R/R), and 32.4% of patients experienced ≥ 1 dose reduction (23.5% 1L, 40.0% R/R).
Conclusions
Toxicity and disease progression were the most common reasons for ibrutinib discontinuations in the overall population and among Black patients, respectively. Encouraging research participation of underrepresented patient groups will help clinicians better understand treatment outcomes.
Plain Language Summary
Ibrutinib, a Bruton tyrosine kinase inhibitor, is an approved oral targeted therapy for the treatment of chronic lymphocytic leukemia (CLL). Patients treated with ibrutinib can experience side effects (referred to as adverse events) and may need to reduce the drug dose (referred to as dose reductions) or stop treatment (referred to as discontinuations) for a variety of reasons. A previous study showed that patients who were treated with ibrutinib experienced frequent dose reductions and discontinuations. This study described dose reductions and discontinuations in a larger patient population treated with ibrutinib and also described outcomes in Black patients. Patients with CLL treated with ibrutinib were identified from five medical centers and were followed for a minimum of 6 months. Patients experienced frequent dose reductions and discontinuations in routine clinical practice. The most common cause of discontinuations was adverse events in the overall patient population and disease progression in the Black patient population. Black patients treated with ibrutinib had similar rates of dose reductions and discontinuations as the overall patient population. Rates of dose reductions and discontinuations for patients with CLL treated with ibrutinib were higher in this real-world study than in clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Toxicity remains the most common reason for ibrutinib discontinuation among patients with CLL who were treated with ibrutinib during routine clinical practice. |
Black patients with CLL treated with ibrutinib had similar rates of dose reductions and discontinuations as the overall cohort. |
1 Introduction
Chronic lymphocytic leukemia (CLL) is a commonly diagnosed chronic leukemia. Over 20,000 new cases are diagnosed annually in the USA, with ~ 91% of new cases occurring among White patients and ~ 7% among Black patients [1, 2]. Black patients with CLL typically present at a younger age and have worse survival outcomes than White patients [3]. The etiology for the racial disparities is not clear [2, 3].
Approval of the covalent Bruton tyrosine kinase inhibitors (BTKis) ibrutinib and acalabrutinib changed the CLL treatment landscape over the past decade. In young and elderly patients in first-line (1L), relapsed/refractory (R/R), and high-risk disease settings, BTKis demonstrated superior progression-free survival and improved tolerability compared with chemoimmunotherapy (CIT) [4]. However, outcomes that include baseline racial characteristics have not been described in detail within published clinical trials. Black race is an independent prognostic variable for worse overall survival (OS) for patients with CLL [3, 5]. Data demonstrating outcomes with BTKis are limited because of limited participation of minorities in the pivotal trials [6]. In fact, the landmark trial data that led to the US Food and Drug Administration approval of drugs for CLL between 2011 and 2021 show that, out of 1849 participants, only 20 were Black (1.1%) [6]. SEER database analyses from 2009–2019 identified 57,783 CLL cases, of which 7.3% were Black patients [3].
BTKis are administered daily, either as monotherapy or with monoclonal antibodies in a combination therapy approach [4, 7,8,9,10], and are given continuously until disease progression or intolerance. Early treatment discontinuation is associated with worse survival outcomes [11]. Understanding issues affecting tolerability of BTKis may help identify treatment modifications and potentially allow patients to continue treatment. Importantly, underrepresentation of marginalized patients in clinical trials make the results difficult to extrapolate to all relevant populations. Although most patients with CLL in the USA are treated in community practice settings [12, 13], real-world data published on treatment outcomes are mostly obtained from major academic centers or registrational trials [12, 13]. Studies of real-world populations are critical to confirm benefits of new therapeutic agents outside the strictly controlled clinical trial setting. In addition to lack of real-world data, follow-up is generally limited to 1–2 years [14, 15]. Discontinuations due to adverse events (AEs) were reported at 4–9% in phase 3 clinical trials of ibrutinib in CLL [8, 16], but subsequent real-world studies [17,18,19] reported higher rates of discontinuation (14–29%). Similarly, rates of ibrutinib dose reduction due to AEs was 9% in clinical trials [20], but these were higher (11–31%) in real-world studies [14, 15, 21].
In addition to differing dose reduction and discontinuation rates, data on the effectiveness and safety of therapies in underrepresented communities with CLL are lacking [22, 23]. Black patients with CLL tend to present at diagnosis with more risk factors and experience poorer survival outcomes compared with White patients [23]. Given these discrepancies, additional real-world evidence (RWE) that considers racial disparities in the tolerability of ibrutinib in the treatment of CLL is necessary.
In 2020, we completed a pilot retrospective chart review study to add to the published literature on the real-world use of ibrutinib among 180 patients with CLL in community and academic settings [24]. The primary objective of that study was to describe ibrutinib dose reductions, discontinuations, and holds (defined as a gap in ibrutinib use of fewer than 90 days) among patients with CLL in the context of routine clinical practice, and to determine the reasons for those decisions.
Since treatment patterns may differ by practice and experience with the drug, we expanded the study to include one additional community site and one additional academic site, and we increased data collection from two of the community-based networks in the original study. This expansion enabled us to perform a descriptive analysis on a subgroup of Black patients with CLL treated with ibrutinib.
2 Methods
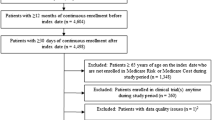
The initial retrospective chart review study design, patient inclusion criteria, and statistical methodology were previously reported [24]. In the original study, 180 patients with CLL treated with ibrutinib at two community networks and one academic practice were followed for a minimum of 6 months, and their data were abstracted from electronic medical records. The expansion study included one additional community site and one additional academic site. Adult patients with a confirmed diagnosis of CLL were included in the study if they initiated ibrutinib between March 2014 and February 2020. The 6-month follow-up period for data collection was extended until August 2020. Patients who died before the end of the 6-month period were included in the study.
3 Results
3.1 Overall Patient Population
As of August 2020, a total of 482 patients with a diagnosis of CLL were identified and enrolled in the study; 189 patients received ibrutinib as 1L therapy and 293 patients received ibrutinib as therapy for R/R CLL (Table 1). Eighty-four percent of the patients were White (n = 405) and 7.7% were Black (n = 37).
For 1L patients, the median age was 71.0 years, and 58.7% of patients were male. Atrial fibrillation was present at baseline in 13.2% of patients, and 61.9% had hypertension. Nineteen percent of patients had del(17p), 14.3% had del(11q), and 39.7% had del(13q). For R/R ibrutinib patients, the median age was 69.0 years and 64.2% of patients were male. At baseline, 9.6% of R/R patients had atrial fibrillation and 56.0% had hypertension; 10.6% of patients had del(17p), 17.1% had del(11q), and 29.7% had del(13q). Genetic mutation testing was documented in ~ 60% of the overall patient population.
The median follow-up time was 28.2 months (26.1 months 1L, 29.9 months R/R), with patients receiving ibrutinib for a median of 19.5 months (21.2 months 1L, 16.7 months R/R). Ibrutinib discontinuation, dose reduction, and dose hold data are summarized in Fig. 1. In the overall population, 31.1% of patients discontinued ibrutinib during the study period (22.2% 1L, 36.9% R/R; Table 2). The median time to discontinuation was 8.4 months (9.3 months 1L, 8.4 months R/R). Overall, 16.2% of patients discontinued due to AEs (n = 23, 12.2% 1L; n = 55, 18.8% R/R) and 6.4% due to progression/refractory disease (n = 3, 1.6% 1L; n = 28, 9.6% R/R). There were no discontinuations for financial reasons. Among the patients who discontinued due to an AE, the most common AEs were atrial fibrillation (n = 6, 26.1% 1L; n = 10, 18.2% R/R), fatigue (n = 3, 13.0% 1L; n = 8, 14.5% R/R), and rash (n = 1, 4.3% 1L; n = 8, 14.5% R/R) (Supplementary Table 1). The median time to discontinuation due to disease progression was 29.3 months (43.5 months 1L, 28.8 months R/R), the median time to discontinuation due to AEs was 6.1 months (4.03 months 1L, 7.2 months R/R), and the median time to next treatment after discontinuation due to disease progression was 35 days (74 days 1L, 28 days R/R).
During the study period, 28.8% of patients experienced at least one dose reduction (n = 47, 24.9% 1L; n = 92, 31.4% R/R). The median time to first dose reduction was 4.8 months (8.2 months 1L, 3.6 months R/R). In the overall population, the most common reasons for first dose reduction were AEs (n = 38, 20.1% 1L; n = 76, 25.9% R/R), drug-drug interactions (n = 4, 2.1% 1L; n = 4, 1.4% R/R), and other (n = 3, 1.6% 1L; n = 10, 3.4% R/R). Among patients who had a dose reduction associated with an AE, the most common AEs were fatigue (n = 6, 15.8% 1L; n = 18, 23.7% R/R), diarrhea (n = 6, 15.8% 1L; n = 10, 13.2% R/R), and thrombocytopenia (n = 5, 13.2% 1L; n = 8, 10.5% R/R) (Supplementary Table 1).
Almost half (46.0%) of patients experienced at least one dose hold (40.2% 1L, 49.8% R/R). The median time to first hold was 51.5 months in 1L and 17.4 months in R/R ibrutinib patients. The median duration of dose holds was 10.5 days in 1L and 15.0 days in R/R ibrutinib patients. The most common reasons for dose holds were AEs (n = 57, 30.2% 1L; n = 98, 33.4% R/R) and procedures (n = 17, 9.0% 1L; n = 38, 13.0% R/R) (Fig. 1). Among patients who had a dose held because of an AE, the most common of these AEs were rash (n = 8, 14.0% 1L; n = 14, 14.3% R/R), neutropenia (n = 4, 7.0% 1L; n = 12, 12.2% R/R), and fatigue (n = 3, 5.3% 1L; n = 9, 9.2% R/R) (Supplementary Table 1).
3.2 Black Patients
In this study there were 37 patients with CLL identified as Black (17 1L, 20 R/R). Median age was 71.0 years in the overall Black population (65.0 years, 1L; 73.0 years, R/R). Among these patients, 8.1% had del(17p); 35% of patients did not have evidence of diagnostic testing. Other important prognostic markers included 29.7% of patients with del(11q) (test not documented in 32.4% of patients), and 27.0% of patients with del(13q) (test not documented in 37.8% of patients). Comorbid conditions at baseline included hypertension and atrial fibrillation in 68.8% and 2.7% of patients, respectively.
During the study period, 24.3% of Black patients discontinued ibrutinib (17.6% 1L, 30.0% R/R) and 32.4% experienced at least one dose reduction (23.5% 1L, 40.0% R/R). The median time to discontinuation was 16.6 months (19.5 months 1L, 11.8 months R/R), and the median time to next treatment after discontinuation due to disease progression was 50.5 days (R/R patients only), compared with a median time to discontinuation of 10.9 months (7.6 months 1L, 11.7 months R/R) in White patients. Among this subgroup, 5.4% of Black patients discontinued ibrutinib due to AEs (5.9% 1L, 5.0% R/R) and 8.1% due to progression/refractory disease (5.9% 1L, 10.0%, R/R). Among White patients (n = 405), 18.5% discontinued ibrutinib due to AEs (13.7% 1L, 21.4% R/R) and 6.7% due to progression/refractory disease (0.7% 1L, 10.3% R/ R) (Table 2).
The median time to first dose reduction was 6.5 months (14.2 months 1L, 5.3 months R/R). The most common reason for first dose reduction was AEs (17.6% 1L, 25.0% R/R). Drug–drug interactions led to dose reduction in 10% of patients in the R/R group and no patients in the 1L group. The AE most often associated with dose reductions in the R/R group was dizziness (10% of patients). In the 1L group, AEs leading to dose reduction were muscle spasms, fatigue, and rash (n = 1 each). During the study period, 40.5% of Black patients experienced one or more dose holds (35.3% 1L, 45.0% R/R).
4 Discussion
The results of the expanded study are consistent with the initial collection data [24] and other published RWE studies on ibrutinib therapy for CLL [25,26,27,28]. The proportion of Black patients with CLL in this study is similar to that reported in SEER databases and matches the demographic diversity of the population affected by the disease [2, 3]. The rate of baseline del(17p) mutation in 1L patients in this study is higher than the rate reported in another frontline study [10], while the rate of del(17p) mutation in R/R patients in this study is lower than in previously reported RWE studies. Higher baseline rates of del(17p) mutation may reflect that, despite several guidelines recommending testing before therapy initiation—including International Workshop on Chronic Lymphocytic Leukemia (iwCLL) guidelines, prognostic marker testing is not commonly performed [27, 28].
In our analysis of 482 patients, there were fewer patients with del(17p) mutations (13.9% versus 18.3%) and atrial fibrillation events (11.0% versus 14.4%) compared with the initial analysis of 180 patients. Higher incidence of atrial fibrillation may better reflect real-world prevalence, as clinical trials for ibrutinib exclude patients on warfarin, which is usually taken by patients with atrial fibrillation. The proportion of patients with hypertension (58.5% versus 52.0%) was higher in this expanded analysis [24].
In the overall population, 16.2% of patients discontinued ibrutinib due to AEs (12.2% 1L, 18.8% R/R). Given an overall rate for ibrutinib discontinuations of ~ 30%, discontinuations due to AEs account for almost half of drug discontinuations in the study. Rates of discontinuation due to disease progression were low (~ 6%). The proportion of patients experiencing dose reductions (28.8%) was similar to the previous report [24]. Compared with the rates in the trials leading to the approval of BTKis, the rates of discontinuations and dose modifications seen in real-world practice are higher. This may be related to a lack of formal guidelines surrounding AE management [21], or to clinical trial populations not being representative of the real-world population, for which AEs may occur at higher rates. Ensuring representative inclusion of patients with comorbidities and patients from underrepresented groups in clinical trials could enhance the generalizability of outcomes and optimize the medical management of drug-related AEs. Additionally, given the high rates of AE-based discontinuations in RWE studies [21], physicians should counsel patients, particularly those with comorbidities, on potential AEs before initiation of therapy.
The current expanded study builds on evidence that a subset of patients treated with ibrutinib experienced premature discontinuations, dose reductions, and dose holds due to tolerability issues. For patients on a treat-to-progression regimen, treatment interruptions may have impacted overall disease outcomes. A recent study by Collins et al. assessed impact of adherence to ibrutinib on clinical outcomes using proportion of days covered (PDC) as a measurement of adherence and found that patients with PDC > 95% during the first 6 months of treatment experienced fewer events of disease progression, but discontinued ibrutinib sooner and more often due to AEs compared with patients with PDC ≤ 95% [29]. The authors hypothesized that high PDC while the patient was on therapy led to more AEs, which could be indicative of tolerability issues with the dosage [29]. However, PDC only addresses adherence when a patient has an active prescription and does not account for any time after the patient discontinues therapy [29].
To our knowledge, our study is the first to report real-world data on ibrutinib use, rate of discontinuations or dose holds, and reasons for discontinuation in a subgroup of Black patients with CLL in the era of commercial access to novel targeted agents. This addresses an important evidence gap, as most CLL clinical trials over-enroll White patients relative to cancer incidence and mortality among that population, with minimal published data available for minority racial and ethnic populations [6, 22]. On average, White patients comprise 76–82% of patients in cancer clinical trials, while Black patients comprise 3–4% [6, 22]. Although the sample was limited, these data mirror what could be expected in the community, as the proportion of Black patients in our report reflects what would be expected in the real world. These data may improve our understanding of racial differences in outcomes among patients treated with ibrutinib.
The demographic and clinical characteristics of the Black patients were consistent with the rest of the dataset and with prior reports of the prevalence of CLL in the Black community [2]. A larger proportion of Black patients had hypertension at baseline (68.8% versus 58.5%) compared with the overall patient population, and a smaller proportion of Black patients had atrial fibrillation (2.7% versus 11.0%). Black patients receiving 1L therapy were slightly younger (median, 65.0 versus 71.0 years) compared with the overall cohort. Fewer Black patients discontinued treatment compared with the overall cohort (24.3% versus 31.1%), but a slightly higher proportion experienced a dose reduction (32.4% versus 28.8%). The most common reason for discontinuation among Black patients was disease progression (n = 3, 8.1%), which was slightly higher than the overall cohort (n = 31, 6.4%). Black patients experienced longer median time to next treatment compared with the overall cohort (50.5 days versus 35.0 days, although only two Black patients initiated a new treatment). As median time to next treatment in the overall population was 35 days, providers should be ready to provide next treatment shortly after discontinuation. “Financial toxicity” also may contribute to disparate rates of discontinuation for underrepresented patient populations [3]. In this study, wherein no discontinuations occurred for financial reasons, Black patients had similar outcomes as the overall cohort. Because clinical trial data are lacking, the information we obtain from real-world studies, including this study, may help us better understand whether access to treatment with BTKis becomes an equalizer in racial disparities.
Low genomic and molecular testing rates in the Black subgroup and low community testing rates in general [12] are a concern because current iwCLL guidelines recommend diagnostic testing for genetic abnormalities to guide treatment decisions [30]. Given that CIT is ineffective for patients with del(17p) and TP53 mutations, there is a risk that patients who are not tested for these mutations (such as ~ 40% of patients overall and ~ 35% of Black patients in this study) could be harmed by exposure to drugs that are less efficacious and more toxic than other options [31]. Future interventions to improve equitable care should focus on improving rates of genetic testing among Black patients to ensure higher-quality therapy.
This study had several limitations. The study utilized medical records that are created for patient care rather than research; therefore, the records may contain errors or missing information. Given its retrospective nature, there may also be variability in how reasons for reductions and discontinuations of ibrutinib are captured across practices. The study captured only the number of discontinuations and AEs associated with discontinuation, not all AEs that patients experienced. We therefore cannot determine if baseline comorbidities, such as hypertension, led to increased risk of atrial fibrillation in patients who received ibrutinib. Patients initiating therapy more recently in the study had limited follow-up time; therefore, true duration of therapy, rates of dose reduction, and discontinuations may be underestimated for those patients. Because of the small sample size of Black patients, no statistical comparison was conducted between the subgroup and overall cohort. Despite these limitations, this study of patients treated with ibrutinib is the first to present real-world ibrutinib data in Black patients.
5 Conclusion
In our expanded retrospective study, we demonstrate high rates of dose reductions, holds, and discontinuations in real-world settings compared with rates reported in clinical trials. AEs were the most common cause of dose reductions and discontinuations among patients receiving ibrutinib treatment.
Although Black race has been associated with worse OS [3], most data emerged when the mainstay of therapy was CIT. With an increasing number of novel agents available for the treatment of CLL, similar real-world studies with larger numbers of Black patients are needed to identify areas of unmet need and obtain clinical data on safety and tolerability in underserved populations. Further research is needed to understand if the worse outcomes in Black patients with CLL are due to lack of access to novel drugs such as BTKis or due to difficulty in managing AEs.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. https://doi.org/10.3322/caac.21590.
Shenoy PJ, Malik N, Sinha R, Nooka A, Nastoupil LJ, Smith M, et al. Racial differences in the presentation and outcomes of chronic lymphocytic leukemia and variants in the United States. Clin Lymphoma Myeloma Leuk. 2011;11(6):498–506. https://doi.org/10.1016/j.clml.2011.07.002.
Kittai AS, Huang Y, Bhat SA, Paskett ED, Rogers KA, Barrientos J, et al. Racial and socioeconomic disparities in CLL/SLL: analysis of SEER data from 2006–2019. Blood Adv. 2023;7(11):2575–9. https://doi.org/10.1182/bloodadvances.2022008643.
Ghia P, Pluta A, Wach M, Lysak D, Kozak T, Simkovic M, et al. ASCEND: Phase III, randomized trial of acalabrutinib versus idelalisib plus rituximab or bendamustine plus rituximab in relapsed or refractory chronic lymphocytic leukemia. J Clin Oncol. 2020;38(25):2849–61. https://doi.org/10.1200/JCO.19.03355.
Vardell V, Ermann DA, Shah H, Fitzgerald L, Hu B, Stephens DM. Influence of racial and ethnic identity on overall survival in patients with chronic lymphocytic lymphoma [abstract 7508]. J Clin Oncol. 2022;40(16):7508. https://doi.org/10.1200/JCO.2022.40.16_suppl.7508.
Casey M, Odhiambo L, Aggarwal N, Shoukier M, Garner J, Islam KM, et al. Are pivotal clinical trials for drugs approved for leukemias and multiple myeloma representative of the population at risk? J Clin Oncol. 2022;40(32):3719–29. https://doi.org/10.1200/jco.22.00504.
Sharman JP, Egyed M, Jurczak W, Skarbnik A, Pagel JM, Flinn IW, et al. Efficacy and safety in a 4-year follow-up of the ELEVATE-TN study comparing acalabrutinib with or without obinutuzumab versus obinutuzumab plus chlorambucil in treatment-naïve chronic lymphocytic leukemia. Leukemia. 2022;36(4):1171–5. https://doi.org/10.1038/s41375-021-01485-x.
Byrd JC, Brown JR, O’Brien S, Barrientos JC, Kay NE, Reddy NM, et al. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371(3):213–23. https://doi.org/10.1056/NEJMoa1400376.
Shanafelt TD, Wang XV, Hanson CA, Paietta EM, O’Brien S, Barrientos JC, et al. Long-term outcomes for ibrutinib-rituximab and chemoimmunotherapy in CLL: updated results of the E1912 trial. Blood. 2022;140(2):112–20. https://doi.org/10.1182/blood.2021014960.
Shanafelt TD, Wang XV, Kay NE, Hanson CA, O’Brien S, Barrientos J, et al. Ibrutinib-rituximab or chemoimmunotherapy for chronic lymphocytic leukemia. N Engl J Med. 2019;381(5):432–43. https://doi.org/10.1056/NEJMoa1817073.
Jain P, Thompson PA, Keating M, Estrov Z, Ferrajoli A, Jain N, et al. Long-term outcomes for patients with chronic lymphocytic leukemia who discontinue ibrutinib. Cancer. 2017;123(12):2268–73. https://doi.org/10.1002/cncr.30596.
Mato AR, Barrientos JC, Ghosh N, Pagel JM, Brander DM, Gutierrez M, et al. Prognostic testing and treatment patterns in chronic lymphocytic leukemia in the era of novel targeted therapies: results from the informCLL registry. Clin Lymphoma Myeloma Leuk. 2020;20(3):174-83.e3. https://doi.org/10.1016/j.clml.2019.10.009.
Mato A, Nabhan C, Lamanna N, Kay NE, Grinblatt DL, Flowers CR, et al. The connect CLL registry: final analysis of 1494 patients with chronic lymphocytic leukemia across 199 US sites. Blood Adv. 2020;4(7):1407–18. https://doi.org/10.1182/bloodadvances.2019001145.
Frei CR, Le H, McHugh D, Elesinmogun C, Galley S, Franklin K, et al. Treatment patterns and outcomes of 1205 patients on novel agents in the US Veterans Health Administration (VHA) System: results from the largest retrospective EMR and chart review study in the real-world setting [abstract]. Blood. 2019;134(Suppl 1):795. https://doi.org/10.1182/blood-2019-122434.
Hardy-Abeloos C, Pinotti R, Gabrilove J. Ibrutinib dose modifications in the management of CLL. J Hematol Oncol. 2020;13(1):66. https://doi.org/10.1186/s13045-020-00870-w.
Burger JA, Tedeschi A, Barr PM, Robak T, Owen C, Ghia P, et al. Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med. 2015;373(25):2425–37. https://doi.org/10.1056/NEJMoa1509388.
Sharman JP, Black-Shinn JL, Clark J, Bitman B. Understanding ibrutinib treatment discontinuation patterns for chronic lymphocytic leukemia [abstract]. Blood. 2017;130(suppl 1):4060.
Hampel PJ, Ding W, Call TG, Rabe KG, Kenderian SS, Witzig TE, et al. Rapid disease progression following discontinuation of ibrutinib in patients with chronic lymphocytic leukemia treated in routine clinical practice. Leuk Lymphoma. 2019;60(11):2712–9. https://doi.org/10.1080/10428194.2019.1602268.
Parikh SA, Achenbach SJ, Call TG, Rabe KG, Ding W, Leis JF, et al. The impact of dose modification and temporary interruption of ibrutinib on outcomes of chronic lymphocytic leukemia patients in routine clinical practice. Cancer Med. 2020;9(10):3390–9. https://doi.org/10.1002/cam4.2998.
Imbruvica [package insert]. Sunnyvale, CA, Horsham, PA: Pharmacyclics, Janssen Biotech, Inc.; 2022.
Dimou M, Iliakis T, Pardalis V, Bitsani C, Vassilakopoulos TP, Angelopoulou M, et al. Safety and efficacy analysis of long-term follow up real-world data with ibrutinib monotherapy in 58 patients with CLL treated in a single-center in Greece. Leuk Lymphoma. 2019;60(12):2939–45. https://doi.org/10.1080/10428194.2019.1620944.
Loree JM, Anand S, Dasari A, Unger JM, Gothwal A, Ellis LM, et al. Disparity of race reporting and representation in clinical trials leading to cancer drug approvals from 2008 to 2018. JAMA Oncol. 2019;5(10): e191870. https://doi.org/10.1001/jamaoncol.2019.1870.
Falchi L, Keating MJ, Wang X, Coombs CC, Lanasa MC, Strom S, et al. Clinical characteristics, response to therapy, and survival of African American patients diagnosed with chronic lymphocytic leukemia: joint experience of the MD Anderson Cancer Center and Duke University Medical Center. Cancer. 2013;119(17):3177–85. https://doi.org/10.1002/cncr.28030.
Hou JZ, Ryan K, Du S, Fang B, Marks S, Page R, et al. Real-world ibrutinib dose reductions, holds and discontinuations in chronic lymphocytic leukemia. Future Oncol. 2021;17(35):4959–69. https://doi.org/10.2217/fon-2021-0964.
Mato A, Nabhan C, Kay NE, Lamanna N, Kipps TJ, Grinblatt DL, et al. Prognostic testing patterns and outcomes of chronic lymphocytic leukemia patients stratified by fluorescence in situ hybridization/cytogenetics: a real-world clinical experience in the Connect CLL Registry. Clin Lymphoma Myeloma Leuk. 2018;18(2):114-24.e2. https://doi.org/10.1016/j.clml.2017.11.010.
Akhtar OS, Attwood K, Lund I, Hare R, Hernandez-Ilizaliturri FJ, Torka P. Dose reductions in ibrutinib therapy are not associated with inferior outcomes in patients with chronic lymphocytic leukemia (CLL). Leuk Lymphoma. 2019;60(7):1650–5. https://doi.org/10.1080/10428194.2018.1554862.
Mato AR, Nabhan C, Barr PM, Ujjani CS, Hill BT, Lamanna N, et al. Outcomes of CLL patients treated with sequential kinase inhibitor therapy: a real world experience. Blood. 2016;128(18):2199–205. https://doi.org/10.1182/blood-2016-05-716977.
Mato AR, Hill BT, Lamanna N, Barr PM, Ujjani CS, Brander DM, et al. Optimal sequencing of ibrutinib, idelalisib, and venetoclax in chronic lymphocytic leukemia: results from a multicenter study of 683 patients. Ann Oncol. 2017;28(5):1050–6. https://doi.org/10.1093/annonc/mdx031.
Collins J, Stump SE, Heiling H, Muir M, Deal A, Proco D, et al. Impact of adherence to ibrutinib on clinical outcomes in real-world patients with chronic lymphocytic leukemia. Leuk Lymphoma. 2022;63(8):1823–30. https://doi.org/10.1080/10428194.2022.2045597.
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018;131(25):2745–60. https://doi.org/10.1182/blood-2017-09-806398.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma version 2.2022: National Comprehensive Cancer Network; 2021 [updated 18 January 2022. Available from: https://www.nccn.org/professionals/physician_gls/default.aspx.
Acknowledgements
The authors wish to acknowledge the patients who participated in the study; EMOL for data harvesting; Nancy Rizkalla, PharmD, Martin Gozar, PharmD, and the CARTI Research coordinators for their data collection efforts; Tyler Knight and Reema Patel from Labcorp for support with analytics and database; and the OPEN Health team for medical writing support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by AstraZeneca. Medical writing and editorial support was provided by Claire Jarvis, PhD, and Maria Ali, PhD, of Peloton Advantage, LLC (Parsippany, NJ, USA), an OPEN Health company, and funded by AstraZeneca.
Competing interests
Jacqueline C. Barrientos has received research support from Oncternal, VelosBio, AstraZeneca, and Pharmacyclics/AbbVie and has served on advisory boards for BeiGene, Pharmacyclics/AbbVie, TG Therapeutics, and MEI Pharma. Ayed O. Ayed has served on an advisory board for AstraZeneca. Agnes Cha has received a research grant (paid to institution) from AstraZeneca. Senxi Du, Bruno Fang, Ryan Hall, Stanley M. Marks, Eileen Peng, Sharon B. Winters, and Percy L. Yeung have no disclosures to report. Joanna M. Rhodes has received research support from Oncternal, VelosBio, Pharmacyclics/AbbVie, and LOXO Oncology and has served as a consultant for BeiGene, Pharmacyclics/AbbVie, TG Therapeutics, MorphoSys, Verastem, ADC Therapeutics, Genentech, SeaGen, GenMab, Janssen, Epizyme, and AstraZeneca. Kellie Ryan is an employee of AstraZeneca. Jing-Zhou Hou has received a research grant (paid to institution) from AstraZeneca.
Ethics Approval
The study protocol was exempt from ethical review by the Western Institutional Review Board (WA, USA) prior to starting data collection. This observational study was performed in accordance with ethical principles that are consistent with the Declaration of Helsinki, the International Conference on Harmonisation’s Guidelines for Good Clinical Practice, the Guidelines for Good Pharmacoepidemiology Practices and applicable legislation on noninterventional studies and/or observational studies.
Consent to Participate
Not applicable.
Consent to Publish
Not applicable.
Availability of Data and Material
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure. Data for studies directly listed on Vivli can be requested through Vivli at www.vivli.org. Data for studies not listed on Vivli could be requested through Vivli at https://vivli.org/members/enquiries-about-studies-not-listed-on-the-vivli-platform/. AstraZeneca Vivli member page is also available outlining further details: https://vivli.org/ourmember/astrazeneca/.
Code Availability
Not applicable.
Author Contributions
SMM and KR designed the study. JCB, AC, BF, RH, SMM, and JMR served as study investigators. AC, SD, RH, SMM, JMR, SBW, and PLY collected and assembled the data. JCB, SMM, and KR analyzed the data. JCB, AOA, SMM, EP, and KR interpreted the data. SMM, KR, and PLY prepared the manuscript. All authors reviewed and revised the manuscript. All authors provided final approval of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Barrientos, J.C., Ayed, A.O., Cha, A. et al. Results from a Real-World Multicenter Analysis of 482 Patients with Chronic Lymphocytic Leukemia Treated with Ibrutinib: A Look at Racial Differences. Targ Oncol 18, 727–734 (2023). https://doi.org/10.1007/s11523-023-00988-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-023-00988-0