Abstract
Inflammation is the core contributor in the pathogenesis of various acute and chronic illness including appendicitis, bronchitis, arthritis, cancer and neurological diseases. NSAIDs, commonly used medications for inflammatory diseases, on prolonged use cause GI bleeding, ulcers and many more issues. Plant-based therapeutic agents including essential oils in combination with low-dose synthetic drugs have been shown to produce synergistic effects and reduce complications of synthetic drugs. This study was designed to evaluate the anti-inflammatory, analgesic and anti-pyretic properties of Eucalyptus globulus essential oil alone and in combination with flurbiprofen. GC–MS analysis was performed to screen chemical composition of oil. In vitro anti-inflammatory assay (membrane stabilization assay) and in vivo inflammatory acute (carrageenan and histamine-induced paw oedema) and chronic (cotton pellet-induced granuloma and Complete Freund’s adjuvant-induced arthritis) models were performed to check anti-inflammatory properties. Acetic acid-induced algesia and yeast-induced pyrexia models were performed to check analgesic and anti-pyretic properties. qRT-PCR was performed to study the effect of treatments on the expression of inflammatory biomarkers. GC–MS analysis of E. globulus essential oil showed the presence of eucalyptol along with other active biomolecules. 500 + 10 mg/kg of oil-drug combination showed significantly (p < 0.05) better in vitro membrane stabilization effects as compared with groups treated with 500 mg/kg of E. globulus oil and 10 mg/kg of Flurbiprofen alone. 500 + 10 mg/kg of oil-drug combination showed significantly (p < 0.05) better anti-inflammatory, analgesic and antipyretic effects as compared to 500 mg/kg of E. globulus oil alone in all in vivo models. When comparison was done between 500 + 10 mg/kg of oil-drug combination-treated and 10 mg/kg Flurbiprofen-treated group, the former group showed significantly (p < 0.05) better anti-inflammatory and anti-pyretic effects, but there were non-significant differences in the analgesic model. Animal group treated with 10 mg/kg of Flurbiprofen showed significantly (p < 0.05) better anti-inflammatory and analgesic effects than group treated with 500 mg/kg of oil alone while, there were non-significant differences in anti-pyretic effects. qRT-PCR analysis showed significant (p < 0.05) down-regulation in the expression of IL-4 and TNF-α in serum samples of animals treated with 500 + 10 mg/kg of oil-drug combination as compared to the diseased control (arthritic) group. Overall, the current research demonstrates that Eucalyptus globulus essential oil in combination with flurbiprofen showed better anti-inflammatory, analgesic and anti-pyretic effects than oil and flurbiprofen alone which is attributed to the down-regulation of pro-inflammatory biomarkers (IL-4 and TNF-α). Further studies are required to formulate a stable dosage form and to check the anti-inflammatory efficacy in different inflammatory disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory process involves series of complex cellular and molecular interactions, that can be triggered by variety of factors including infections, toxins, auto-immune reactions and damaged cells (Nathan 2002). It is a multi-step process in which various components of vascular tissue, blood vessels, circulating blood cells, and cell mediators take part. The net outcome of which is increased vascular permeability, recruitment of inflammatory and immune cells and release of plethora of inflammatory mediators (Fujiwara and Kobayashi 2005). Depending upon duration and severity of inflammatory reaction, it can be beneficial to the body or vice versa (Andleeb et al. 2022). Chronic inflammation-associated diseases are one of the most common causes of deaths worldwide. It is identified as a core issue in the pathogenesis of diseases like gastritis, chronic obstructive pulmonary disease, inflammatory bowel disease, diabetes, obesity and different types of cancers etc. (Furman et al. 2019; Ploeger et al. 2009).
Non-Steroidal Anti-inflammatory Drugs (NSAIDs) block the production of various inflammatory mediators by inhibiting cyclooxygenases (COX-1 and -2). In chronic illness like arthritis, NSAIDs are prescribed for long duration. The prolonged use of these cause gastric bleeding and perforations, cardiovascular abnormalities including thrombus formation and acute renal failure (Marcum and Hanlon 2010). Plant-based drugs are known to mitigate the side effects of synthetic drugs when used in combination. A study conducted by Tanzeem el al. reported the gastroprotective effects of clove oil against flurbiprofen when used in combination (Tanzeem et al. 2019). Moreover, improvement in therapeutic efficacy of synthetic drugs is observed when given in combination with plant extracts. A study by Yehya et al. showed sensitization of gemcitabine resistant cells towards gemcitabine when used in combination with a standardised extract of Orthosiphon stamineus (C5EOSEW5050ESA) (Yehya et al. 2023). An in vitro antimicrobial study conducted by Rosato et al. showed synergistic actions of Diclofenac sodium salt when used in combination with essential oils obtained from Mentha piperita, Pelargonium graveolens and Melaleuca alternifolia (Rosato et al. 2021). Essential oils obtained from various plant species are known to have anti-oxidant and anti-inflammatory effects. Reduction in the levels of reactive oxygen and reactive nitrogen species, elevation in the levels of anti-oxidant enzymes, inhibition of COX-2 enzyme, reduction in the levels of various pro-inflammatory cytokines including TFN-α, IL-6 and IL-1β and maintenance of balance between Th1 and Th2 cells population are among the few mechanisms responsible for anti-inflammatory attributes of essential oils (de Lavor et al. 2018; Zuo et al. 2020).
Eucalyptus is a large Genera comprising of almost 700 species. Various plant parts including bark and leaves of Eucalyptus species have been used as traditional remedies for the treatment of different human ailments since medieval times (Chandorkar et al. 2021). Eucalyptus globulus Labill. of family Myrtaceae is one of the most widely used medicinal plants globally due to its wide spectrum of pharmacological attributes (Shala and Gururani 2021). It is now widely cultivated throughout the world. Essential oil obtained from E. globulus have been shown to have anti-oxidant, analgesic, anti-inflammatory, antibacterial, antiviral, bronchodilator and CNS stimulant properties (Asif et al. 2020b; Chandorkar et al. 2021). E. globulus essential oil and its active component, eucalyptol (1,8–cineole) is the main ingredient of many marketed medicinal products. Soledum™ (100 mg of 1,8–cineole), a herbal product of E. globulus essential oil is used for the treatment of acute and chronic bronchitis, sinusitis, and other respiratory infections (Chandorkar et al. 2021). Vicks VapoRub™ containing 1,8-cineole (eucalyptol 1.33% w/w) as one of the active components is used to relieve nasal congestion (Asif et al. 2020b). Literature review at https://clinicaltrials.gov showed that multiple clinical trials are registered to explore the beneficial effects of E. globulus essential oil in muscle soreness, hypertension, migraine, COVID-19, tick bites, gingivitis and dental plague. This data highlights the high human acceptability and medicinal potential of E. globulus essential oil. Numerous pre-clinical studies have reported the anti-inflammatory and analgesic effects of E. globulus essential oil in in vitro and in vivo models (Chandorkar et al. 2021; Ho et al. 2020; Lin et al. 2018; Shao et al. 2020; Silva et al. 2003). However, to best of our knowledge there is no scientific study available which has reported the anti-inflammatory, analgesic and anti-pyretic effects of E. globulus essential oil in combination with Flurbiprofen (FB). Therefore, the current study was designed to explore the anti-inflammatory attributes of E. globulus essential oil alone and in combination with Flurbiprofen using series of in vivo models along with its possible molecular mechanisms.
Materials and methods
Collection of essential oils
Eucalyptus globulus oil was procured from local supplier (Go Natural), Lahore, Pakistan.
GC–MS analysis
GC–MS analysis of Eucalyptus globulus essential oil (E.G) was performed following reported protocols. The oil constituents were identified by comparing MS data with NIST mass spectral library and published mass spectra (Andleeb et al. 2022).
Animals
Albino Wistar rats (male and female) of weight 180–200 g and mice (male and female) of weight 20–30 g were obtained from the animal house of Department of Pharmacology, the Islamia University of Bahawalpur. The animals were kept in the laboratory under standard conditions of humidity (50%), temperature (set at 25 ± 5 ℃) and 12 h light/dark cycles. All animals were given standard pellet diet and free access to tap water. One week acclimatization of animals was done prior to pharmacological activities. All the experimental procedures were approved by Pharmacy Ethics Committee (PAEC/22/86).
Anti-inflammatory studies
In vitro membrane stabilization assay (heat-induced haemolysis)
Human blood was collected in heparinized tubes followed by centrifugation at 3000 rpm for 5 min and then washed with equal volumes of 0.9% NaCl. Blood suspension (v/v) was prepared with isotonic buffer solution (pH: 7.4). Then, 0.05 ml of this suspension was mixed with 0.05 ml of different concentrations of E. globulus oil (E.G: 125, 250, 500 mg/ml), flurbiprofen (FB, 10 mg/ml) and E. globulus oil and flurbiprofen combination (E.G + FB: 125 + 10, 250 + 10, 500 + 10 mg/ml) respectively. In all these mixtures, 2.95 ml of buffer solution was added and incubated for 20 min in shaking water bath set at 54 0C, followed by centrifugation at 2500 rpm for 3 min. Later, supernatant was collected and absorbance was measured by UV spectrophotometer at 540 nm. Percentage of inhibition was calculated following reported formula (Gunathilake et al. 2018).
In vivo anti-inflammatory studies
For all in vivo models animals were treated orally with E.G (125, 250, 500 mg/kg), FB (10 mg/kg) and E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/kg) respectively.
Carrageenan and Histamine-induced paw oedema models
After one hour of pre-treatment with E.G (125, 250, 500 mg/kg), FB (10 mg/kg) and E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/kg), 0.1 ml of 1% w/v freshly prepared carrageenan and histamine solutions were injected subcutaneously into sub-plantar surface of left hind paw of each rat separately. Measurement of paw volumes was done at 0, 1, 2, 3, 4, 5 and 6 h. with the help of digital Vernier calliper. Anti-inflammatory effects are presented as percentage inhibition of paw oedema, calculated using reported formula (Shabbir et al. 2018).
Acetic acid-induced pain model
Acetic acid-induced writhing test was performed in mice following reported protocols. In brief, 10 ml/kg of 0.6% acetic acid was injected i.p in the abdominal area of mice and abdominal writhes were noted for 25 min starting 5 min after the administration of acetic acid. Animals were treated following the same scheme as mentioned in the above section and percent inhibition of writhing was calculated using reported formula (Naghizadeh et al. 2016).
Brewer's yeast-induced pyrexia model
In brief, digital thermometer was inserted 2 cm-deep into the rectum of each rat to record the initial rectal temperature (RT). Rats with starting RT between 37 and 37.5 ℃ were selected. Brewer’s yeast suspension (20 mg/kg) was subcutaneously injected at the back of the neck to induce pyrexia. Animals having rectal temperature difference of 1 ℃ or above were given different treatments to test the anti-pyretic effects. Animals were treated following the same scheme as mentioned in the above section and rectal temperatures were noted at 1, 2, 3 and 4 h. (Kong et al. 2014).
Cotton pellet-induced granuloma model
In brief, rats were anaesthetised using mixture of ketamine and xylazine. Sterile cotton pellets (20 mg) were implanted subcutaneously in both shaved axilla regions of rats by creating small incisions. Treatments were given in the same manners as mentioned above for the consecutive 10 days. At day 11, animals were dissected and cotton pellets were removed, cleaned of extraneous tissue, weighed, and dried at 60 °C to a constant weight. Increase in the dry weight of pellets was calculated and percent inhibition of granuloma formation was calculated using reported formula (Sokeng et al. 2020).
Complete Freund’s Adjuvant-induced arthritic model
In brief, 0.1 ml of Complete Freund’s Adjuvant (CFA) was injected in sub-plantar region of left hind paw of each rat to induce arthritis. Rats were divided into eight groups as descried above and treatment was given for 21 days. Paw volumes were measured by digital Vernier calliper at day 3, 5,9,13 and 21 (Zhu et al. 2020). Anti-inflammatory effects are reported as percentage of inhibition of paw oedema which was calculated using reported formula (Nagarkar and Jagtap 2017).
Molecular Mechanistic studies
RT-PCR technique was employed to analyse effects of different treatments on the expressions of different inflammatory biomarkers following well-reported method (Andleeb et al. 2022). Expression of two major genes including TNF-α, and IL-4 was checked. Primer sequences of these genes are mentioned in Table 1. Data is presented as relative fold change values (n = 3) (De Cicco et al. 2020; Saleem et al. 2021).
Statistical analysis
Data is presented as Mean ± Standard Error of Mean (SEM). Statistical analysis was performed using ONE WAY and TWO WAY ANOVA models. p values less than 0.05 were considered statistically significant.
Results
GC–MS analysis of Eucalyptus globulus essential oil
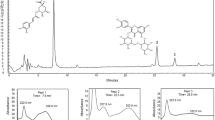
GC–MS analysis of Eucalyptus globulus oil showed the presence of eucalyptol, limonene, cymene, mycrene, pinene, phellandrene and cyclohexene (Table 2 and Fig. 1).
Anti-inflammatory studies
In vitro membrane stabilization assay (heat-induced haemolysis)
Maximum membrane stabilization effects observed in groups treated with E.G (125, 250, 500 mg/ml), FB (10 mg/ml), E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/ml) were 53.51 ± 4.31, 65.24 ± 1.22, 68.77 ± 1.08, 69.71 ± 3.07, 70.97 ± 3.48, 75.02 ± 2.05, 80.18 ± 1.18% respectively. Better protective effects were observed in E.G + FB at the concentration of 500 + 10 mg/ml than other treatment groups. Flurbiprofen (10 mg/ml) and E.G 500 mg/ml treated samples showed almost same effects with no statistical difference (p > 0.05) (Table 3 and Fig. 2).
Effect of different treatments on in vitro membrane stabilization. Values shown are mean ± SEM of percentage inhibition of RBC’s haemolysis (n = 3). Where E.G = Eucalyptus globulus oil, FB = Flurbiprofen, # = non-significant, * = p < 0.05, ** = p < 0.01, *** = p < 0.001 respectively. Black colour sign indicates the comparison of 125 vs 125 + 10 mg/ml and, 125 vs 250 mg/ml. Green colour sign indicates the comparison of 250 vs 250 + 10 mg/ml and, 250 vs 500 mg/ml. Blue colour sign indicates the comparison of 500 vs 500 + 10 mg/ml. Red colour sign indicates the comparison of FB with 500, 125 + 10, 250 + 10 and, 500 + 10 mg/ml
In vivo anti-inflammatory studies
Carrageenan-induced paw oedema model
Maximum anti-inflammatory effects observed in groups treated with E.G (125, 250, 500 mg/kg), FB (10 mg/kg), E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/kg) were 40.96 ± 1.00, 57.18 ± 4.03, 60.12 ± 3.89, 71.38 ± 8.10, 60.22 ± 13.61, 68.10 ± 7.94, 83.22 ± 11.09% respectively. During the first 2 h of study, no statistical differences in terms of percent inhibition of paw oedema was observed in E.G, FB and E.G + FB treatment groups when compared with each other. At 3rd hr. E.G + FB treated group showed significantly better anti-inflammatory (p <0.05) activity in terms of percentage inhibition of paw oedema when compared with E.G 500 mg/kg treated group. From 4th hr onward, E.G + FB combination-treated groups showed significantly (p < 0.05) better anti-inflammatory effects than E.G alone treatment groups. No statistical difference in terms of percentage inhibition of paw oedema was observed in E.G (500 mg/kg) and flurbiprofen (10 mg/kg) treatment groups during first 4 h of study. At 6th hr flurbiprofen treated group showed significantly (p < 0.01) better anti-inflammatory effects when compared with E.G 500 mg/kg treated group (Table 4 and Fig. 3).
Effect of different treatments on carrageenan-induced paw oedema. Values shown are mean ± SEM of percentage inhibition of paw oedema (n =6). Where E.G = Eucalyptus globulus oil, FB = Flurbiprofen. # = non-significant, * = p < 0.05, ** = p < 0.01, *** = p < 0.001 respectively. Black colour sign indicates the comparison of 125 vs 125 + 10 mg/kg, 125 vs 250 mg/kg. Green colour sign indicates the comparison of 250 vs 250 + 10 mg/kg, 250 vs 500 mg/kg. Blue colour sign indicates the comparison of 500 vs 500 + 10 mg/kg. Red colour sign indicates the comparison of drug with 500, 125 + 10, 250 + 10 and 500 + 10 mg/kg
Histamine-induced paw oedema model
Maximum anti-inflammatory effects observed in groups treated with E.G (125, 250, 500 mg/kg), FB (10 mg/kg), E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/kg) were 49.64 ± 3.82, 56.81 ± 2.30, 60.30 ± 6.54, 68.01 ± 5.61, 69.14 ± 1.07, 77.22 ± 1.57, 85.93 ± 2.68% respectively. E.G + FB (500 + 10 mg/kg) treated group showed significantly (p < 0.05) better anti-inflammatory effects in terms of percentage inhibition of paw oedema than other treatment groups during the study. Flurbiprofen (FB 10 mg/kg) and E.G (500 mg/kg) treated groups showed almost same effects with no statistical differences (p > 0.05) from 1st to 5th hr. At 6th h. flurbiprofen treated group showed significantly (p < 0.01) better anti-inflammatory effects when compared with E.G (500 mg/kg) treated group (Fig. 4 and Table 5).
Effect of different treatments on histamine-induced oedema. Values shown are mean ± SEM of percentage inhibition (n = 6). Where E.G = Eucalyptus globulus oil, FB = Flurbiprofen. # = non-significant, * = p < 0.05, ** = p < 0.01, *** = p < 0.001 respectively. Black colour sign indicates the comparison of 125 vs 125 + 10 mg/kg, 125 vs 250 mg/kg. Green colour sign indicates the comparison of 250 vs 250 + 10 mg/kg, 250 vs 500 mg/kg. Blue colour sign indicates the comparison of 500 vs 500 + 10 mg/kg. Red colour sign indicates the comparison of drug with 500, 125 + 10, 250 + 10, 500 + 10 mg/kg
Acetic acid-induced pain model
Maximum analgesic effects observed in groups treated with E.G (125, 250, 500 mg/kg), FB (10 mg/kg), E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/kg) were 33.09 ± 4.81, 39.43 ± 3.63, 45.07 ± 3.63, 60.47 ± 2.65, 56.94 ± 3.58, 63.19 ± 4.74, 65.97 ± 4.74% respectively. E.G + FB combination-treated groups showed significantly (p < 0.05) better analgesic effects than E.G alone treatment groups and comparable effects with flurbiprofen. Flurbiprofen (10 mg/kg) showed significantly (p < 0.05) better analgesic effects than E.G (500 mg/kg) treated group (Fig. 5 and Table 6).
Effect of different treatments on acetic acid-induced algesia. Values shown are mean ± SEM (n = 6). Where E.G = Eucalyptus globulus oil, FB = Flurbiprofen, # = non-significant, * = p < 0.05, ** = p < 0.01, *** = p < 0.001 respectively. Black colour sign indicates the comparison of 125 vs 125 + 10 mg/kg and, 125 vs 250 mg/kg. Green colour sign indicates the comparison of 250 vs 250 + 10 mg/kg and, 250 vs 500 mg/kg. Blue colour sign indicates the comparison of 500 vs 500 + 10 mg/kg. Red colour sign indicates the comparison of drug with 500, 125 + 10, 250 + 10, and 500 + 10 mg/kg
Yeast-induced pyrexia model
Maximum antipyretics effects observed in groups treated with E.G (125, 250, 500 mg/kg), FB (10 mg/kg), E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/kg) were 101.00 ± 0.34, 99.37 ± 1.35, 99.15 ± 1.04, 99.10 ± 0.54, 98.57 ± 0.42, 97.50 ± 0.60, 96.85 ± 0.520F respectively. No statistical differences between E.G (500 mg/kg) and E.G + FB (500 + 10 mg/kg) treatment groups were observed at 1st hr. From 2nd hr onwards E.G + FB (500 + 10 mg/kg) treated group showed significant (p < 0.05) antipyretic effects as compared with rest of the groups. Flurbiprofen (10 mg/kg) and E.G (500 mg/kg) treated groups showed almost same anti-pyretic effects (p > 0.05) (Table 7 and Fig. 6).
Effect of E.G, FB, E.G + FB treatments on yeast-induced pyrexia. Values shown are mean ± SEM (n = 6). Where E.G = Eucalyptus globulus essential oil, FB = Flurbiprofen, # = non-significant, * = p < 0.05, ** = p < 0.01, *** = p < 0.001 respectively. Black colour sign indicates the comparison of 125 vs 125 + 10 mg/kg and, 125 vs 250 mg/kg. Green colour sign indicates the comparison of 250 vs 250 + 10 mg/kg and, 250 vs 500 mg/kg. Blue colour sign indicates the comparison of 500 vs 500 + 10 mg/kg. Red colour sign indicates the comparison of drug with 500, 125 + 10, 250 + 10, and 500 + 10 mg/kg
Cotton pellet-induced granuloma model
Maximum anti-granulomatous effects in animals treated with E.G (125, 250, 500 mg/kg), FB (10 mg/kg), E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/kg) were 44.54 ± 1.44, 51.26 ± 1.44, 57.98 ± 7.23, 65.54 ± 4.87, 66.94 ± 8.65, 71.99 ± 5.71, 76.47 ± 5.25% respectively. E.G + FB combination treated groups showed significantly (p < 0.05) better anti-granulomatous effects than E.G-treated groups and comparable effects with FB-treated group. Flurbiprofen (10 mg/kg) and E.G (500 mg/kg) treatment groups showed almost same anti-granulomatous effects when compared with each other (p > 0.05) (Table 8 and Fig. 7).
Effect of different treatments on cotton pellet-induced granuloma. Values shown are mean ± SEM of percentage inhibition of granuloma (n = 6). Where E.G = Eucalyptus globulus oil, FB = Flurbiprofen, # = non-significant, * = p < 0.05, ** = p < 0.01, *** = p < 0.001 respectively. Black colour sign indicates the comparison of 125 vs 125 + 10 mg/kg and, 125 vs 250 mg/kg. Green colour sign indicates the comparison of 250 vs 250 + 10 mg/kg and, 250 vs 500 mg/kg. Blue colour sign indicates the comparison of 500 vs 500 + 10 mg/kg. Red colour sign indicates the comparison of drug with 500, 125 + 10, 250 + 10, and 500 + 10 mg/kg
CFA-induced arthritic model
Maximum anti-arthritic effects as reported in terms of percent inhibition of inflammation observed in groups treated with E.G (125, 250, 500 mg/kg), FB (10 mg/kg), E.G + FB (125 + 10, 250 + 10, 500 + 10 mg/kg) were 39.69 ± 2.25, 40.53 ± 1.65, 46.06 ± 5.26, 57.62 ± 18.58, 50.39 ± 5.05, 61.23 ± 2.14, 78.95 ± 2.36% respectively. No statistical differences in terms of percent inhibition of paw oedema were observed in E.G (500 mg/kg) and E.G + FB (500 + 10 mg/kg) treatment groups from day 1 to 5. At day 9, 13 and 21, E.G + FB (500 + 10 mg/kg) combination treated group showed significant (p < 0.05) anti-inflammatory effects than E.G 500 mg/kg treated group. Flurbiprofen (10 mg/kg) and E.G (500 mg/kg) treated groups showed same anti-inflammatory effects from day 1st to 13th. At day 21, flurbiprofen (10 mg/kg) treated group showed significant (p < 0.05) anti-inflammatory effects than E.G 500 mg/kg group (Table 9 and Fig. 8).
Effect of different treatments on CFA-induced arthritis. Values shown are mean ± SEM of percentage inhibition (n = 6). Where E.G = Eucalyptus globulus oil, FB = Flurbiprofen, # = non-significant, * = p < 0.05, ** = p < 0.01, *** = p < 0.001 respectively. Black colour sign indicates the comparison of 125 vs 125 + 10 mg/kg and, 125 vs 250 mg/kg. Green colour sign indicates the comparison of 250 vs 250 + 10 mg/kg and, 250 vs 500 mg/kg. Blue colour sign indicates the comparison of 500 vs 500 + 10 mg/kg. Red colour sign indicates the comparison of drug with 500, 125 + 10, 250 + 10, and 500 + 10 mg/kg
Relative fold change values of TNF-α and IL-4 in different treatment groups are presented in Fig. 9. Relative fold change values of TNF- α were 0.96 ± 0.05, 0.82 ± 0.00 and 0.80 ± 0.05 in the diseased control, E.G (500 mg/kg) and E.G + FB (500 + 10 mg/kg) treated group respectively. Relative fold change values of IL-4 in E.G (500 mg/kg), E.G + FB (500 + 10 mg/kg) and diseased control were calculated to be 0.33 ± 0.00, 0.25 ± 0.00 and 0.96 ± 0.03 respectively.
Effect of Eucalyptus globulus oil and Flurbiprofen treatments alone and in combination on the expression of TNF-α and IL-4. Values shown are mean ± SEM of three independent experiments (n = 3). Where # = non-significant, * = p < 0.05, ** = p < 0.01, *** = p < 0.001 respectively. Red and green colours indicate comparison of 500 mg/kg and 500 + 10 mg/kg treatments with the diseased control group respectively
Discussion
Chemo-herbal combinations have shown remarkable effects in the management of various types of cancers. These combinations are known to enhance the efficacy, reduce the side effects and increase the sensitivity of cancer cells towards the standard drugs (Hu et al. 2016; Yehya et al. 2023). Eucalyptus globulus essential oil has been in clinical use since long. Soledum™ (100 mg of 1,8–cineole), a herbal product of E. globulus essential oil is clinically used for the treatment of acute and chronic bronchitis, sinusitis, and other respiratory infections (Chandorkar et al. 2021). Vicks VapoRub™ containing 1,8-cineole (eucalyptol 1.33% w/w) as one of the active components is clinically used to relieve nasal congestion (Asif et al. 2020b). Based on the concept of mitigation of adverse effects of synthetic drugs via combination with natural products, the current study was designed to evaluate the anti-inflammatory, analgesic and anti-pyretic properties of Eucalyptus globulus essential oil in combination with flurbiprofen. Moreover, same doses of E. globulus essential oil and flurbiprofen were tested alone to establish synergism.
Rupture of lysosomal membranes leading to the release of degrading enzymes is among the variety of events which take place during inflammation. These leaked enzymes cause injury to neighbouring cells. Heat-induced haemolysis of human RBC’s is one of the most commonly employed in vitro methods to test the efficacy of drugs to prevent lysosomal membrane rupture. This membrane is considered analogous to the lysosomal membrane and its stabilization suggests that test drug may also stabilise lysosomal membranes (Boukhatem et al. 2020). Eucalyptol rich essential oil of Lavender has been shown to prevent hypotonicity-induced lysis of RBC’s membrane. In the current study, combination of Eucalyptus globulus oil and flurbiprofen (500 + 10 mg/ml) showed maximum protection against heat-induced haemolysis. Eucalyptol is suggested to play a major role in this protection as reported by Boukhatem and colleagues (Boukhatem et al. 2020).
Carrageenan-induced inflammation is a two phase process as reported by various scientists. The early phase involves release of serotonin, histamine and other mediators followed by the release and subsequent degrading actions of lysosomes, prostaglandins and proteases on tissue cells (Cronstein et al. 1999; Mworia et al. 2021; Pillinger et al. 1998). Histamine released during an acute inflammatory phase increases vascular permeability, draws neutrophils at the site of inflammation where exudate forms, and works in conjunction with prostaglandins to promote oedema. This inflammatory phase lasts only for a brief period (de Morais Oliveira-Tintino et al. 2018). 1,8- Cineole has been shown to inhibit carrageenan-induced oedema by blocking the increase in capillary permeability (Takaki et al. 2008). Moreover, it is known to suppress mast cells degranulation (Nakamura et al. 2020). Flurbiprofen is known to inhibit carrageenan-induced paw oedema through COX inhibition (Sugimoto et al. 2016). Combination treatment of E. globulus oil and flurbiprofen (500 + 10 mg/kg) showed significantly better results in both acute model of inflammation as compared with other treatments. This could be due to multi-targeted actions of bioactive molecules of Eucalyptus globulus oil and flurbiprofen.
Acetic acid serves as a stimulus for acute nociception in an inflammatory pain model. Acetic acid damages tissues and releases chemicals that cause pain. It also activates peripheral nociceptors on sensory nerve fibres (Naghizadeh et al. 2016). Flurbiprofen is known to rapidly decrease PGE2 levels in paw exudate and inflammatory pain in the acetic acid-induced pain model (Sugimoto et al. 2016). Eucalyptus globulus oil has established peripheral effects which reduces the writhes (Silva et al. 2003). Limonene, the second most bioactive molecule detected in E. globulus oil has been proved to have anti-nociceptive effects (Adriana Estrella et al. 2021). In the current study, combination treatment showed significantly better analgesic effects which are suggested to be due to reduced levels as well as actions of PGE2 on peripheral nerves.
Fever is a complex physiologic response which may be caused by infection or aseptic stimuli. When prostaglandins (PGE2) accumulates in the hypothalamus pre-optic region, it causes elevation in body temperature (Mworia et al. 2019). In the current study, combination treatment (500 + 10 mg/kg) showed significantly better anti-pyretic activity than other treatment groups. This may be due to the flurbiprofen which inhibit prostaglandin E2 synthesis via COX inhibition in hypothalamus region (Mworia et al. 2019).
Cotton pellet-induced granuloma represents three stages of inflammation. The transudative phase in vascular permeability increases, capillary fluids develop and fill the pellets. The exudative phase which occurs between 3 and 72 h involves proteins migration around granuloma. The third phase (proliferative phase), which is characterised by an increase in the dry weight of the pellet, as a result of recruitment of fibroblasts, neutrophils, and macrophages (Sokeng et al. 2020). 1,8-Cineole is known to inhibit granuloma formation (Martins et al. 2017). Moreover, essential oil of Citrus aurantium L. containing limonene has been shown to be effective regarding the transudate and granuloma formation amount (Khodabakhsh et al. 2015). NSAIDs also have anti-proliferative effects which decrease granuloma formation (de Morais Oliveira-Tintino et al. 2018). In the current study, combination treatment (500 + 10 mg/kg) inhibited granuloma formation. This could be due to multi-targeted actions of bioactive molecules of Eucalyptus globulus oil and flurbiprofen.
Features of Complete Freund's adjuvant (CFA)-induced arthritis pathologically match with rheumatoid arthritis (RA) (Andleeb et al. 2022). CFA injection can trigger release of number of inflammatory cytokines including, IL-1, IL-6, and COX-2 (Zhang et al. 2020). IL-1, IL-6, and TNF-alpha are among the few pro-inflammatory mediators which are elevated in RA (Andleeb et al. 2022; Asif et al. 2020a). The increased production of free radicals by activated neutrophils and macrophages is a key factor in the pathogenesis of RA (Mahdi et al. 2018). Moreover, IL-4 has been revealed to have both pro- and anti-inflammatory effects. On one side it decreases monocyte and macrophage functions and induces a Th2 type response. On the other side it causes recruitment of inflammatory cells by increasing the expression of cell adhesion molecules (VCAM-1) on the endothelial surface and increases eosinophils, macrophages and B cells chemo-attraction (Ratthé et al. 2009). In the current study, combination treatment (500 + 10 mg/kg) showed significantly better anti-arthritic effects as compared with other treatment groups. These effects may be due to cytokines inhibitory effects of eucalyptol (Silva et al. 2003) and flurbiprofen which blocks COX-2 expression at the site of inflammation. Overall, this causes possible decrease in number of inflammatory cells and cytokines release at the site of inflammation.
Conclusion
The current research demonstrates that eucalyptol rich Eucalyptus globulus essential oil in combination with flurbiprofen has potent anti-inflammatory, analgesic and anti-pyretic effects. Down-regulation of expression and actions of pro-inflammatory cytokines (e.g., TNF-α and IL-4) with subsequent inhibition of cellular events controlled by these mediators is proposed to be the major pathway. Further studies to formulate a stable dosage form of this combination and exploration of its effects in various chronic inflammatory disorders is undergoing in our research laboratory.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Adriana Estrella G-R, María Eva G-T, Alberto H-L, María Guadalupe V-D, Azucena C-V, Sandra O-S, Noé A-V, Francisco Javier L-M (2021) Limonene from Agastache mexicana essential oil produces antinociceptive effects, gastrointestinal protection and improves experimental ulcerative colitis. J Ethnopharmacol 280:114462. https://doi.org/10.1016/j.jep.2021.114462
Andleeb F, Asif M, Yaseen HS (2022) Exploration of molecular mechanisms responsible for anti-inflammatory and anti-angiogenic attributes of methanolic extract of Viola betonicifolia. Inflammopharmacology 30:1459–1474
Asif M, Mahrukh Saadullah M, Yaseen HS, Saleem M, Yousaf HM, Khan IU, Yaseen M, Shams MU (2020a) Evaluation of in vivo anti-inflammatory and anti-angiogenic attributes of methanolic extract of Launaea spinosa. Inflammopharmacology 28:993–1008. https://doi.org/10.1007/s10787-020-00687-6
Asif M, Saleem M, Saadullah M, Yaseen HS, Al Zarzour R (2020b) COVID-19 and therapy with essential oils having antiviral, anti-inflammatory, and immunomodulatory properties. Inflammopharmacology 28:1153–1161. https://doi.org/10.1007/s10787-020-00744-0
Boukhatem MN, Sudha T, Darwish NHE, Chader H, Belkadi A, Rajabi M, Houche A, Benkebailli F, Oudjida F, Mousa SA (2020) A new eucalyptol-rich lavender (Lavandula stoechas L.) essential oil: emerging potential for therapy against inflammation and cancer. Molecules. https://doi.org/10.3390/molecules25163671
Chandorkar N, Tambe S, Amin P, Madankar C (2021) A systematic and comprehensive review on current understanding of the pharmacological actions, molecular mechanisms, and clinical implications of the genus Eucalyptus. Phytomedicine Plus 1:100089. https://doi.org/10.1016/j.phyplu.2021.100089
Cronstein BN, Montesinos MC, Weissmann G (1999) Salicylates and sulfasalazine, but not glucocorticoids, inhibit leukocyte accumulation by an adenosine-dependent mechanism that is independent of inhibition of prostaglandin synthesis and p105 of NFkappaB. Proc Natl Acad Sci U S A 96:6377–6381. https://doi.org/10.1073/pnas.96.11.6377
De Cicco P, Maisto M, Tenore GC, Ianaro A (2020) Olive leaf extract, from Olea Europaea L., reduces palmitate-induced inflammation via regulation of murine macrophages polarization. Nutrients 12:3663
Fujiwara N, Kobayashi K (2005) Macrophages in inflammation. Curr Drug Targets-Inflamm Allergy 4:281–286
Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM (2019) Chronic inflammation in the etiology of disease across the life span. Nat Med 25:1822–1832. https://doi.org/10.1038/s41591-019-0675-0
Gunathilake K, Ranaweera K, Rupasinghe HV (2018) In vitro anti-inflammatory properties of selected green leafy vegetables. Biomedicines 6:107
Ho C-L, Li L-H, Weng Y-C, Hua K-F, Ju T-C (2020) Eucalyptus essential oils inhibit the lipopolysaccharide-induced inflammatory response in RAW2647 macrophages through reducing MAPK and NF-κB pathways. BMC Complement Med Ther 20:200. https://doi.org/10.1186/s12906-020-02999-0
Hu XQ, Sun Y, Lau E, Zhao M, Su SB (2016) Advances in synergistic combinations of chinese herbal medicine for the treatment of cancer. Curr Cancer Drug Targets 16:346–356. https://doi.org/10.2174/1568009616666151207105851
Khodabakhsh P, Shafaroodi H, Asgarpanah J (2015) Analgesic and anti-inflammatory activities of Citrus aurantium L. blossoms essential oil (neroli): involvement of the nitric oxide/cyclic-guanosine monophosphate pathway. J Nat Med 69:324–331. https://doi.org/10.1007/s11418-015-0896-6
Kong X, Wan H, Su X, Zhang C, Yang Y, Li X, Yao L, Lin N (2014) Rheum palmatum L. and Coptis chinensis Franch., exert antipyretic effect on yeast-induced pyrexia rats involving regulation of TRPV1 and TRPM8 expression. J Ethnopharmacol 153:160–168
de Lavor ÉM, Fernandes AWC, de Andrade Teles RB, Leal AEBP, de Oliveira Júnior RG, Gamae Silva M, de Oliveira AP, Silva JC, de Moura Fontes Araújo MT, Coutinho HDM, de Menezes IRA, Picot L, da Silva Almeida JRG (2018) essential oils and their major compounds in the treatment of chronic inflammation: a review of antioxidant potential in preclinical studies and molecular mechanisms. Oxidative Med Cell Longev 2018:6468593. https://doi.org/10.1155/2018/6468593
Lin TC, Wang SH, Huang CC, Lai YC, Song TY, Tsai MS (2018) Anti-fatigue, antioxidation, and anti-inflammatory effects of eucalyptus oil aromatherapy in swimming-exercised rats. Chin J Physiol 61:257–265. https://doi.org/10.4077/cjp.2018.bag572
Mahdi HJ, Khan NAK, Asmawi MZB, Mahmud R, Vikneswaran A, Murugaiyah L (2018) In vivo anti-arthritic and anti-nociceptive effects of ethanol extract of Moringa oleifera leaves on complete Freund’s adjuvant (CFA)-induced arthritis in rats. Integr Med Res 7:85–94
Marcum ZA, Hanlon JT (2010) Recognizing the risks of chronic nonsteroidal anti-inflammatory drug use in older adults. Ann Longterm Care 18:24–27
Martins AOBPB, Rodrigues LB, Cesário FRAS, de Oliveira MRC, Tintino CDM, Castro FFE, Alcântara IS, Fernandes MNM, de Albuquerque TR, da Silva MSA, de Sousa Araújo AA, Júniur LJQ, da Costa JGM, de Menezes IRA, Wanderley AG (2017) Anti-edematogenic and anti-inflammatory activity of the essential oil from Croton rhamnifolioides leaves and its major constituent 1,8-cineole (eucalyptol). Biomed Pharmacother 96:384–395. https://doi.org/10.1016/j.biopha.2017.10.005
de Morais Oliveira-Tintino CD, Pessoa RT, Fernandes MNM, Alcântara IS, da Silva BAF, de Oliveira MRC, Martins AOBPB, da Silva MdS, Tintino SR, Rodrigues FFG (2018) Anti-inflammatory and anti-edematogenic action of the Croton campestris A. St.-Hil (Euphorbiaceae) essential oil and the compound β-caryophyllene in in vivo models. Phytomedicine 41:82–95
Mworia JK, Kibiti CM, Ngugi MP, Ngeranwa JN (2019) Antipyretic potential of dichloromethane leaf extract of Eucalyptus globulus (Labill) and Senna didymobotrya (Fresenius) in rats models. Heliyon 5:e02924
Mworia JK, Kibiti CM, Ngeranwa JJ, Ngugi MP (2021) Anti-inflammatory potential of dichloromethane leaf extracts of Eucalyptus globulus (Labill) and Senna didymobotrya (Fresenius) in mice. Afr Health Sci 21:397–409
Nagarkar B, Jagtap S (2017) Effect of new polyherbal formulations DF1911, DF2112 and DF2813 on CFA induced inflammation in rat model. BMC Complement Altern Med 17:1–12
Naghizadeh B, Mansouri MT, Ghorbanzadeh B (2016) Ellagic acid enhances the antinociceptive action of carbamazepine in the acetic acid writhing test with mice. Pharm Biol 54:157–161
Nakamura T, Yoshida N, Yamanoi Y, Honryo A, Tomita H, Kuwabara H, Kojima Y (2020) eucalyptus oil reduces allergic reactions and suppresses mast cell degranulation by downregulating IgE-FcεRI signalling. Sci Rep 10:1–15
Nathan C (2002) Points of control in inflammation. Nature 420:846–852
Pillinger MH, Capodici C, Rosenthal P, Kheterpal N, Hanft S, Philips MR, Weissmann G (1998) Modes of action of aspirin-like drugs: salicylates inhibit erk activation and integrin-dependent neutrophil adhesion. Proc Natl Acad Sci U S A 95:14540–14545. https://doi.org/10.1073/pnas.95.24.14540
Ploeger HE, Takken T, De Greef M, Timmons BW (2009) The effects of acute and chronic exercise on inflammatory markers in children and adults with a chronic inflammatory disease: a systematic review. Exerc Immunol Rev 15:6–41
Ratthé C, Ennaciri J, Garcês Gonçalves DM, Chiasson S, Girard D (2009) Interleukin (IL)-4 induces leukocyte infiltration in vivo by an indirect mechanism. Mediat Inflamma 2009:193970. https://doi.org/10.1155/2009/193970
Rosato A, Altini E, Sblano S, Salvagno L, Maggi F, de Michele G, Carocci A, Clodoveo ML, Corbo F, Fracchiolla G (2021) Synergistic activity of new diclofenac and essential oils combinations against different candida spp. Antibiotics (Basel). https://doi.org/10.3390/antibiotics10060688
Saleem M, Iftikhar A, Asif M, Hussain K, Shah PA, Saleem A, Akhtar MF, Tanzeem M, Yaseen HS (2021) Asphodelus tenuifolius extracts arrested inflammation and arthritis through modulation of TNF-α, NF-κB, ILs, and COX-2 activities in in vivo models. Inflammopharmacology 29:483–497
Shabbir A, Batool SA, Basheer MI, Shahzad M, Sultana K, Tareen RB, Iqbal J (2018) Ziziphora clinopodioides ameliorated rheumatoid arthritis and inflammatory paw edema in different models of acute and chronic inflammation. Biomed Pharmacother 97:1710–1721
Shala AY, Gururani MA (2021) Phytochemical properties and diverse beneficial roles of eucalyptus globulus labill.: a review. Horticulturae 7:450
Shao J, Yin Z, Wang Y, Yang Y, Tang Q, Zhang M, Jiao J, Liu C, Yang M, Zhen L, Hassouna A, White WL, Lu J (2020) Effects of different doses of eucalyptus oil from eucalyptus globulus labill on respiratory tract immunity and immune function in healthy rats. Front Pharmacol. https://doi.org/10.3389/fphar.2020.01287
Silva J, Abebe W, Sousa S, Duarte V, Machado M, Matos F (2003) Analgesic and anti-inflammatory effects of essential oils of Eucalyptus. J Ethnopharmacol 89:277–283
Sokeng SD, Talla E, Sakava P, Fokam Tagne MA, Henoumont C, Sophie L, Mbafor JT, Tchuenguem Fohouo F-N (2020) Anti-inflammatory and analgesic effect of arachic acid ethyl ester isolated from propolis. BioMed Res Int 2020:1–8
Sugimoto M, Toda Y, Hori M, Mitani A, Ichihara T, Sekine S, Kaku S, Otsuka N, Matsumoto H (2016) Topical anti-inflammatory and analgesic effects of multiple applications of S(+)-flurbiprofen plaster (SFPP) in a rat adjuvant-induced arthritis model. Drug Dev Res 77:206–211. https://doi.org/10.1002/ddr.21314
Takaki I, Bersani-Amado L, Vendruscolo A, Sartoretto S, Diniz S, Bersani-Amado C, Cuman R (2008) Anti-inflammatory and antinociceptive effects of Rosmarinus officinalis L. essential oil in experimental animal models. J Med Food 11:741–746
Tanzeem MU, Asghar S, Khalid SH, Asif M, Ullah MS, Khan IU, Khalid I, Faran SA, Rehman A, Gohar UF, Hussain T (2019) Clove oil based co-surfactant free microemulsion of flurbiprofen: Improved solubility with ameliorated drug-induced gastritis. Pak J Pharm Sci 32:2787–2793
Yehya AHS, Asif M, Abdul Majid AMS, Oon CE (2023) Polymolecular botanical drug of Orthosiphon stamineus extract (C5OSEW5050ESA) as a complementary therapy to overcome gemcitabine resistance in pancreatic cancer cells. J Tradit Complement Med 13:39–50. https://doi.org/10.1016/j.jtcme.2022.10.002
Zhang L, Liang X, Ou Z, Ye M, Shi Y, Chen Y, Zhao J, Zheng D, Xiang H (2020) Screening of chemical composition, anti-arthritis, antitumor and antioxidant capacities of essential oils from four Zingiberaceae herbs. Ind Crop Prod 149:112342
Zhu L, Zhang Z, Xia N, Zhang W, Wei Y, Huang J, Ren Z, Meng F, Yang L (2020) Anti-arthritic activity of ferulic acid in complete Freund’s adjuvant (CFA)-induced arthritis in rats: JAK2 inhibition. Inflammopharmacology 28:463–473
Zuo X, Gu Y, Wang C, Zhang J, Zhang J, Wang G, Wang F (2020) A systematic review of the anti-inflammatory and immunomodulatory properties of 16 essential oils of herbs. Evid-Based Complement Altern Med 2020:8878927. https://doi.org/10.1155/2020/8878927
Acknowledgements
We would like to thank Faculty of Pharmacy, the Islamia University of Bahawalpur, Punjab, Pakistan for providing the research facilities to carry out this project.
Funding
Portion of this project was supported by Higher Education Commission of Pakistan research grant (20–15527/NRPU/R&D/HEC/2021 2021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors do not declare conflict of interest in the current work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arooj, B., Asghar, S., Saleem, M. et al. Anti-inflammatory mechanisms of eucalyptol rich Eucalyptus globulus essential oil alone and in combination with flurbiprofen. Inflammopharmacol 31, 1849–1862 (2023). https://doi.org/10.1007/s10787-023-01237-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-023-01237-6