Abstract
Background
Margin negative resection of rectal cancer with minimally invasive techniques remains technically challenging. Robotic surgery has potential advantages over traditional laparoscopy. We hypothesize that the difference in the rate of negative margin status will be < 6% between laparoscopic and robotic approach.
Methods
The National Cancer Database (2010–2014) was queried for adults with locally advanced rectal cancer who underwent neoadjuvant chemoradiation and curative resection to conduct an observational retrospective cohort study of a prospectively maintained database. Patients were grouped by either robotic (ROB) or laparoscopic (LAP) approach in an intent-to-treat analysis. Primary outcome was negative margin status, defined as a composite of circumferential resection margin and distal margin. Secondary outcomes included length of stay (LOS), readmission, 90-day mortality, and overall survival.
Results
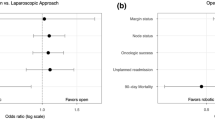
7616 patients with locally advanced rectal cancer who underwent minimally invasive resection were identified. 2472 (32%) underwent attempted robotic approach. The overall conversion rate was 13% and was increased in the laparoscopic group [LAP: 15% vs. ROB: 8%; OR 0.47; 95% CI (0.39, 0.57)]. Differences in margin negative resection rate were within the prespecified range of practical equivalence (LAP: 93% vs.: ROB 94%; 95% CI (0.69, 1.06); \(p_{\updelta}\) = 1). For secondary outcomes, there was no difference in 30-day readmission [LAP: 9% vs.: ROB 8%; 95% CI (0.84, 1.24)] and 90-day mortality [LAP: 1% vs.: ROB 1%; 95% CI (0.38, 1.24)]. While the median LOS was 5 days in both groups, the mean LOS was 0.6 (95% CI: 0.24, 0.89) days shorter in the robotic group.
Conclusion
This robust analysis supports either robotic or laparoscopic approach for resection of locally advanced rectal cancer from a margin perspective. Both have similar readmission and 5-year overall survival rates. Patients undergoing robotic surgery have a 0.6-day decrease in LOS and decreased conversion rate.




Similar content being viewed by others
References
Bonjer HJ, Deijen CL, Abis GA et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332
Fleshman J, Branda M, Sargent DJ et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15(7):767–774
Stevenson AR, Solomon MJ, Lumley JW et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363
Fleshman J, Branda ME, Sargent DJ et al (2019) Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer: follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg 269(4):589–595
Stevenson ARL, Solomon MJ, Brown CSB et al (2019) Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: the australasian laparoscopic cancer of the rectum randomized clinical trial. Ann Surg 269(4):596–602
Jayne D, Pigazzi A, Marshall H et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318(16):1569–1580
Nagtegaal ID, Quirke P (2008) What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol 26(2):303–312
Bilimoria KY, Stewart AK, Winchester DP et al (2008) The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol 15(3):683–690
Winchester DP, Stewart AK, Phillips JL et al (2010) The national cancer data base: past, present, and future. Ann Surg Oncol 17(1):4–7
Blume JD, D’Agostino McGowan L, Dupont WD et al (2018) Second-generation p-values: improved rigor, reproducibility, & transparency in statistical analyses. PLoS ONE 13(3):e0188299
Blume JD, Greevy RA, Welty VF et al (2019) An introduction to second-generation p-values. Am Stat 73(sup1):157–167
RC Team (2019) A language and environment for statistical computing. RC Team, Geneva
Quirke P, Steele R, Monson J et al (2009) Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR14 and NCIC-CTG CO16 randomised clinical trial. Lancet 373(9666):821–828
Kang SB, Park JW, Jeong SY et al (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11(7):637–645
Ahmed J, Nasir M, Flashman K et al (2016) Totally robotic rectal resection: an experience of the first 100 consecutive cases. Int J Colorectal Dis 31(4):869–876
Ali S, Taylor BM, Schlachta CM (2015) Evaluation of pilot experience with robotic-assisted proctectomy and coloanal anastomosis for rectal cancer. Can J Surg 58(3):188–192
Sammour T, Malakorn S, Bednarski BK et al (2018) Oncological outcomes after robotic proctectomy for rectal cancer: analysis of a prospective database. Ann Surg 267(3):521–526
Spanheimer PM, Armstrong JG, Fu S et al (2017) Robotic proctectomy for rectal cancer: analysis of 71 patients from a single institution. Int J Med Robot 13(4):e1841
Yamaguchi T, Kinugasa Y, Shiomi A et al (2016) Robotic-assisted vs conventional laparoscopic surgery for rectal cancer: short-term outcomes at a single center. Surg Today 46(8):957–962
Speicher PJ, Englum BR, Ganapathi AM et al (2015) Robotic low anterior resection for rectal cancer: a National perspective on short-term oncologic outcomes. Ann Surg 262(6):1040–1045
Sujatha-Bhaskar S, Jafari MD, Gahagan JV et al (2017) Defining the role of minimally invasive proctectomy for locally advanced rectal adenocarcinoma. Ann Surg 266(4):574–581
Silva-Velazco J, Dietz DW, Stocchi L et al (2017) Considering value in rectal cancer surgery: an analysis of costs and outcomes based on the open, laparoscopic, and robotic approach for proctectomy. Ann Surg 265(5):960–968
Moghadamyeghaneh Z, Phelan M, Smith BR et al (2015) Outcomes of open, laparoscopic, and robotic abdominoperineal resections in patients with rectal cancer. Dis Colon Rectum 58(12):1123–1129
Vasudevan V, Reusche R, Wallace H et al (2016) Clinical outcomes and cost-benefit analysis comparing laparoscopic and robotic colorectal surgeries. Surg Endosc 30(12):5490–5493
Acknowledgements
The authors thank Anne Zimmerman Hawkins for her proofreading.
Funding
Dr. Hawkins’ work on this manuscript was supported by the National Institute of Diabetes and Digestive and Kidney Disease of the National Institutes of Health under Award No. K23DK118192. The project described was supported by the National Center for Research Resources, Grant UL1 RR024975-01, and is now at the National Center for Advancing Translational Sciences, Grant 2 UL1 TR000445-06. Additional support was provided by CTSA Award No. UL1 TR002243 from the National Center for Advancing Translational Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Geiger is a paid consultant for INX medical, which has no relevance to this study. Drs. Hopkins, Ford, Muldoon, Beck, Stewart and Hawkins & Mr. Bethurum have no financial ties to disclose. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed, or the conclusions drawn from these data by the investigators. Drs. Hopkins, Geiger, Ford, Muldoon, Beck, Stewart and Hawkins & Mr. Bethurum have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hopkins, M.B., Geiger, T.M., Bethurum, A.J. et al. Comparing pathologic outcomes for robotic versus laparoscopic Surgery in rectal cancer resection: a propensity adjusted analysis of 7616 patients. Surg Endosc 34, 2613–2622 (2020). https://doi.org/10.1007/s00464-019-07032-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07032-1