Abstract
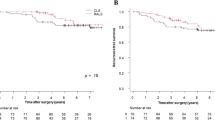
Robotic-assisted surgery (RAS) is becoming increasingly common for the surgical treatment of rectal cancer. However, the use and implementation of robotic surgery remains controversial. This study aimed to compare the short-term outcomes of robotic surgery, focusing on pathological results and disease-free survival (DFS), in our cohort with initial robotic experience by multiple surgeon implementation. This retrospective study enrolled 571 patients diagnosed with rectal cancer, who were treated with chemoradiotherapy and surgery between January 2015 and December 2021. Surgical outcomes after RAS and laparoscopic surgery (LS) were compared using a propensity score-matching (PSM) analysis. After matching, 200 patients (100 in each group) were included. The median operative time was significantly longer in the RAS group than in the LS group (p < 0.001). The conversion and morbidity rates were similar between the groups. A significantly higher rate of complete mesorectal excision (92% vs. 72%; p = 0.001) and number of lymph nodes harvested (p = 0.009) was observed in the RAS group. There were no statistically significant differences between the groups regarding circumferential and distal resection margin involvement. The 3-year overall and disease-free survival rate was similar between the two groups (p = 0.849 and p = 0.582, respectively). Two patients in the LS group developed local recurrence and 27 patients (15.4%) developed metastatic disease. Multivariate analysis showed that tumor stage III was the only factor associated with disease-free survival (HR, 9.34; (95% CI 1.13–77.1), p = 0.038). RAS and LS showed similar outcomes in terms of perioperative, anatomopathological, and disease-free survival, after multiple surgeon implementations.


Similar content being viewed by others
References
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J et al (2017) Effect of Robotic-Assisted vs Conventional Laparoscopic Surgery on Risk of Conversion to Open Laparotomy Among Patients Undergoing Resection for Rectal Cancer: The ROLARR Randomized Clinical Trial. JAMA 318(16):1569–1580
Safiejko K, Tarkowski R, Koselak M, Juchimiuk M, Tarasik A, Pruc M et al (2021) Robotic-Assisted vs. Standard Laparoscopic Surgery for Rectal Cancer Resection: A Systematic Review and Meta-Analysis of 19,731 Patients. Cancers (Basel) 14(1):180
Tang B, Lei X, Ai J, Huang Z, Shi J, Li T (2021) Comparison of robotic and laparoscopic rectal cancer surgery: a meta-analysis of randomized controlled trials. World J Surg Oncol 19(1):38
Phan K, Kahlaee HR, Kim SH, Toh JWT (2019) Laparoscopic vs robotic rectal cancer surgery and the effect on conversion rates: a meta-analysis of randomized controlled trials and propensity-score-matched studies. Tech Coloproctol 23(3):221–230
AlAsari S, Min BS (2012) Robotic Colorectal Surgery: A Systematic Review. ISRN Surgery 13(2012):1–12
Halabi M, Kamal J, Reguig F, Zenilman ME, Moussa H (2023) Implementation of robotic surgery in Dubai: a focus on outcomes. J Robotic Surg 17(1):169–176
Hol JC, Dogan K, Blanken-Peeters CFJM, van Eekeren RRJP, de Roos MAJ, Sietses C et al (2021) Implementation of robot-assisted total mesorectal excision by multiple surgeons in a large teaching hospital: Morbidity, long-term oncological and functional outcome. Int J Med Robot Comp Assist Surg 17(3):e2227
Povolotskaya N, Woolas R, Brinkmann D (2015) Implementation of a Robotic Surgical Program in Gynaecological Oncology and Comparison with Prior Laparoscopic Series. Int J Surg Oncol 15(2015):e814315
Randell R, Honey S, Alvarado N, Greenhalgh J, Hindmarsh J, Pearman A et al (2019) Factors supporting and constraining the implementation of robot-assisted surgery: a realist interview study. BMJ Open 9(6):e028635
Montroy J, Elzayat E, Morash C, Blew B, Lavallée LT, Cagiannos I et al (2017) Long-term patient outcomes from the first year of a robotic surgery program using multi-surgeon implementation. CUAJ 12(2):38–43
Lawrie L, Gillies K, Duncan E, Davies L, Beard D, Campbell MK (2022) Barriers and enablers to the effective implementation of robotic assisted surgery. PLoS ONE 17(8):e0273696
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH (2002) Cooperative Clinical Investigators of the Dutch Colorectal Cancer Group. Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J. Clin. Oncol 20(7):1729–1734
Quirke P (2003) Training and quality assurance for rectal cancer: 20 years of data is enough. Lancet Oncol 4(11):695–702
D’Annibale A, Pernazza G, Monsellato I, Pende V, Lucandri G, Mazzocchi P et al (2013) Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc 27(6):1887–1895
Gachabayov M, Kim SH, Jimenez-Rodriguez R, Kuo LJ, Cianchi F, Tulina I et al (2020) Impact of robotic learning curve on histopathology in rectal cancer: A pooled analysis. Surg Oncol 1(34):121–125
Trastulli S, Farinella E, Cirocchi R, Cavaliere D, Avenia N, Sciannameo F et al (2012) Robotic resection compared with laparoscopic rectal resection for cancer: systematic review and meta-analysis of short-term outcome. Colorectal Dis 14(4):e134-156
Kethman WC, Harris AH, Morris AM, Shelton A, Kirilcuk N, Kin C (2020) Oncologic and perioperative outcomes of laparoscopic, open, and robotic approaches for rectal cancer resection: a multicenter, propensity score-weighted cohort study. Dis Colon Rectum 63(1):46–52
Lam J, Tam MS, Retting RL, McLemore EC (2021) Robotic Versus Laparoscopic Surgery for Rectal Cancer: A Comprehensive Review of Oncological Outcomes. Perm J 25(21):050
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the Adoption of Robotic Surgery for Common Surgical Procedures. JAMA Netw Open 3(1):e1918911
Yamanashi T, Miura H, Tanaka T, Watanabe A, Goto T, Yokoi K et al (2022) Comparison of short-term outcomes of robotic-assisted and conventional laparoscopic surgery for rectal cancer: A propensity score-matched analysis. Asia J Endosc Surg. https://doi.org/10.1111/ases.13075
Park SY, Lee SM, Park JS, Kim HJ, Choi GS (2021) Robot Surgery Shows Similar Long-term Oncologic Outcomes as Laparoscopic Surgery for Mid/Lower Rectal Cancer but Is Beneficial to ypT3/4 After Preoperative Chemoradiation. Dis Colon Rectum 64(7):812–821
Fiorillo C, Quero G, Menghi R, Cina C, Laterza V, De Sio D et al (2021) Robotic rectal resection: oncologic outcomes. Updates Surg 73(3):1081–1091
Aliyev V, Tokmak H, Goksel S, Meric S, Acar S, Kaya H et al (2020) The long-term oncological outcomes of the 140 robotic sphincter-saving total mesorectal excision for rectal cancer: a single surgeon experience. J Robot Surg 14(4):655–661
Sueda T, Tei M, Nishida K, Yoshikawa Y, Matsumura T, Koga C et al (2022) Short-term outcomes of robotic-assisted versus conventional laparoscopic-assisted surgery for rectal cancer: a propensity score-matched analysis. J Robotic Surg 16(2):323–331
Prete FP, Pezzolla A, Prete F, Testini M, Marzaioli R, Patriti A et al (2018) Robotic Versus Laparoscopic Minimally Invasive Surgery for Rectal Cancer: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann Surg 267(6):1034–1046
Planellas P, Cornejo L, Pigem A, Gómez-Romeu N, Julià-Bergkvist D, Ortega N et al (2022) Challenges and Learning Curves in Adopting TaTME and Robotic Surgery for Rectal Cancer: A Cusum Analysis. Cancers 14(20):5089
Jiménez-Rodríguez RM, Rubio-Dorado-Manzanares M, Díaz-Pavón JM, Reyes-Díaz ML, Vazquez-Monchul JM, Garcia-Cabrera AM et al (2016) Learning curve in robotic rectal cancer surgery: current state of affairs. Int J Colorectal Dis 31(12):1807–1815
Jiménez-Rodríguez RM, Díaz-Pavón JM, La Portilla De, De Juan F, Prendes-Sillero E, Dussort HC, Padillo J (2013) Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int J Colorectal Dis 28(6):815–821
Wang Y, Liu Y, Han G, Yi B, Zhu S (2020) The severity of postoperative complications after robotic versus laparoscopic surgery for rectal cancer: A systematic review, meta-analysis and meta-regression. PLoS ONE 15(10):e0239909
Ohtani H, Maeda K, Nomura S, Shinto O, Mizuyama Y, Nakagawa H et al (2018) Meta-analysis of Robot-assisted Versus Laparoscopic Surgery for Rectal Cancer. In Vivo 32(3):611–623
Reyes R, Kindler C, Smedh K, Tiselius C (2022). A comparative study of the pathological outcomes of robot-assisted versus open surgery for rectal cancer. Annals of coloproctology. https://doi.org/10.3393/ac.2022.00332.0047
Burghgraef TA, Sikkenk DJ, Crolla RMPH, Fahim M, Melenhorst J, Moumni ME, Schelling GV, Smits AB, Stassen LP S, Verheijen PM, Consten ECJ (2023). Assessing the learning curve of robot-assisted total mesorectal excision: a multicenter study considering procedural safety, pathological safety, and efficiency. Int J Colorectal Dis 38(1):9
Martínez-Pérez A, Carra MC, Brunetti F, de’Angelis N, (2017) Pathologic Outcomes of Laparoscopic vs Open Mesorectal Excision for Rectal Cancer: A Systematic Review and Meta-analysis. JAMA Surg 152(4):e165665
Park CH, Bae SU, Jeong WK, Baek SK (2021) Early and late clinico-pathologic outcomes of minimally invasive total mesorectal excision for rectal cancer: A propensity score-matched comparison of robotic and laparoscopic approaches. Rob Comp Surg. https://doi.org/10.1002/rcs.2324
Park JS, Lee SM, Choi GS, Park SY, Kim HJ, Song SH et al (2023) Comparison of Laparoscopic Versus Robot-Assisted Surgery for Rectal Cancers: The COLRAR Randomized Controlled Trial. Ann Surg 278(1):31–38
Allemann P, Duvoisin C, Di Mare L, Hübner M, Demartines N, Hahnloser D (2016) Robotic-Assisted Surgery Improves the Quality of Total Mesorectal Excision for Rectal Cancer Compared to Laparoscopy: Results of a Case-Controlled Analysis. World J Surg 40(4):1010–1016
de Jesus JP, Valadão M, de Castro Araujo RO, Cesar D, Linhares E, Iglesias AC (2016) The circumferential resection margins status: A comparison of robotic, laparoscopic and open total mesorectal excision for mid and low rectal cancer. Eur J Surg Oncol (EJSO) 42(6):808–812
Kim MJ, Park SC, Park JW, Chang HJ, Kim DY, Nam BH et al (2018) Robot-assisted Versus Laparoscopic Surgery for Rectal Cancer: A Phase II Open Label Prospective Randomized Controlled Trial. Ann Surg 267(2):243–251
Seow W, Dudi-Venkata NN, Bedrikovetski S, Kroon HM, Sammour T (2023) Outcomes of open vs laparoscopic vs robotic vs transanal total mesorectal excision (TME) for rectal cancer: a network meta-analysis. Tech Coloproctol 27(5):345–360
Khajeh E, Aminizadeh E, Dooghaie Moghadam A, Nikbakhsh R, Goncalves G, Carvalho C et al (2023) Outcomes of Robot-Assisted Surgery in Rectal Cancer Compared with Open and Laparoscopic Surgery. Cancers (Basel) 15(3):839
Lei X, Yang L, Huang Z, Shi H, Zhou Z, Tang C et al (2021) No beneficial effect on survival but a decrease in postoperative complications in patients with rectal cancer undergoing robotic surgery: a retrospective cohort study. BMC Surg 28(21):355
Delitto D, George TJ, Loftus TJ, Qiu P, Chang GJ, Allegra CJ et al (2017) Prognostic Value of Clinical vs Pathologic Stage in Rectal Cancer Patients Receiving Neoadjuvant Therapy. J Natl Cancer Inst 110(5):460–466
Acknowledgements
We thank Anastasia Glagolieva, who collaborated to facilitate this project.
Funding
Dr. Ernesto Barzola, MsC. Lidia Cornejo, Dr. Núria Gòmez, Dr. Anna Pigem, Dr. David Julià, Dr.Nuria Ortega, Dr. Olga Delisau, Dr. Kelly-Ann Bobb, Dr.Ramon Farrès, and Dr.Pere Planellas have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Contributions
EB: study conception and design, literature review, acquisition of data, analysis and interpretation of data, drafting of the manuscript, and critical revision and final approval of the manuscript. PP: study conception and design, literature review, acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision, and final approval of the manuscript. LC: analysis and interpretation of data, critical revision, and final approval of the manuscript. NG: analysis and interpretation of data, critical revision, and final approval of the manuscript. AP: analysis and interpretation of data, critical revision, and final approval of the manuscript. OD: analysis and interpretation of data, critical revision, and final approval of the manuscript. NO: analysis and interpretation of data, critical revision, and final approval of the manuscript. K-AB: analysis and interpretation of data, critical revision, and final approval of the manuscript. RF: study conception and design, literature review, analysis and interpretation of data, critical revision, and final approval of the manuscript. All authors agree to be held accountable for all aspects of this work.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Ernesto Barzola, MsC. Lidia Cornejo, Dr. Núria Gómez, Dr. Anna Pigem, Dr. David Julià, Dr.Nuria Ortega, Dr. Olga Delisau, Dr. Kelly-Ann Bobb, Dr.Ramon Farrés, and Dr.Pere Planellas have no conflicts of interest regarding the publication of this article.
Ethical approval
This study was approved by the hospital’s ethics committee and conducted in accordance with the 1964 Helsinki Declaration and its later amendments. (N °2022.164).
Informed consent
All patients provided written informed consent to collect data and authorize the analysis of the results.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barzola, E., Cornejo, L., Gómez, N. et al. Comparative analysis of short-term outcomes and oncological results between robotic-assisted and laparoscopic surgery for rectal cancer by multiple surgeon implementation: a propensity score-matched analysis. J Robotic Surg 17, 3013–3023 (2023). https://doi.org/10.1007/s11701-023-01736-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-023-01736-2