Abstract
Objective
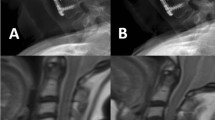
Determine the utility of ZTE as an adjunct to routine MR for assessing degenerative disease in the cervical spine.
Methods
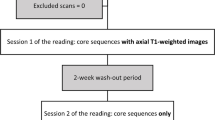
Retrospective study on 42 patients with cervical MR performed with ZTE from 1/1/2022 to 4/30/22. Fellowship trained radiologists evaluated each cervical disc level for neural foraminal (NF) narrowing, canal stenosis (CS), facet arthritis (FA), and presence of ossification of the posterior longitudinal ligament (OPLL). When NF narrowing and CS were present, the relative contributions of bone and soft disc were determined and a confidence level for doing so was assigned. Comparisons were made between assessments on routine MR without and with ZTE.
Results
With ZTE added, bone contribution as a cause of NF narrowing increased in 47% (n = 110) of neural foramina and decreased in 12% (n = 29) (p = < 0.001). Bone contribution as a cause of CS increased in 25% (n = 33) of disc levels and decreased in 10% (n = 13) (p = 0.013). Confidence increased in identifying the cause of NF narrowing (p = < 0.001)) and CS (p = 0.009) with ZTE. The cause of NF narrowing (p = 0.007) and CS (p = 0.041) changed more frequently after ZTE was added when initial confidence in making the determination was low. There was no change in detection of FA or presence of OPLL with ZTE.
Conclusion
Addition of ZTE to a routine cervical spine MR changes the assessment of the degree of bone involvement in degenerative cervical spine pathology.





Similar content being viewed by others
Data availability
Data is available by request.
References
Hurwitz EL, Randhawa K, Yu H, Côté P, Haldeman S. The global spine care initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J. 2018;27:796–801.
Donnally CJ, Patel PD, Canseco JA, Vaccaro AR, Kepler CK. Current management of cervical spondylotic myelopathy. Clin Spine Surg. 2022;35:E68-76.
Larson PEZ, Han M, Krug R, Jakary A, Nelson SJ, Vigneron DB, et al. Ultrashort echo time and zero echo time MRI at 7T. MAGMA. 2016;29:359–70.
Brown BM, Schwartz RH, Frank E, Blank NK. Preoperative evaluation of cervical radiculopathy and myelopathy by surface-coil MR imaging. AJR Am J Roentgenol. 1988;151:1205–12.
Aydıngöz Ü, Yıldız AE, Ergen FB. Zero echo time musculoskeletal MRI: technique, optimization, applications, and pitfalls. Radiographics. 2022;42:1398–414.
de Mello RAF, Ma Y-J, Ashir A, Jerban S, Hoenecke H, Carl M, et al. Three-dimensional zero echo time magnetic resonance imaging versus 3-dimensional computed tomography for glenoid bone assessment. Arthroscopy. 2020;36:2391–400.
Breighner RE, Endo Y, Konin GP, Gulotta LV, Koff MF, Potter HG. Technical developments: zero echo time imaging of the shoulder: enhanced osseous detail by using MR imaging. Radiology. 2018;286:960–6.
Breighner RE, Bogner EA, Lee SC, Koff MF, Potter HG. Evaluation of osseous morphology of the hip using zero echo time magnetic resonance imaging. Am J Sports Med. 2019;47:3460–8.
Li Y, Xiong Y, Hou B, Liu C, Wang J, Liu WV, et al. Comparison of zero echo time MRI with T1-weighted fast spin echo for the recognition of sacroiliac joint structural lesions using CT as the reference standard. Eur Radiol. 2022;32:3963–73.
Wolharn L, Guggenberger R, Higashigaito K, Sartoretti T, Winklhofer S, Chung CB, et al. Detailed bone assessment of the sacroiliac joint in a prospective imaging study: comparison between computed tomography, zero echo time, and black bone magnetic resonance imaging. Skeletal Radiol. 2022;51:2307–15.
Hou B, Liu C, Li Y, Xiong Y, Wang J, Zhang P, et al. Evaluation of the degenerative lumbar osseous morphology using zero echo time magnetic resonance imaging (ZTE-MRI). Eur Spine J. 2022;31:792–800.
Argentieri EC, Koff MF, Breighner RE, Endo Y, Shah PH, Sneag DB. Diagnostic Accuracy of Zero-Echo Time MRI for the Evaluation of Cervical Neural Foraminal Stenosis. Spine (Phila Pa 1976). 2018;43:928–33.
Ma Y-J, Chang EY. Ossification of the posterior longitudinal ligament on zero-TE MRI with “CT-like” contrast. AJR Am J Roentgenol. 2021;217:1242.
Khorami AK, Oliveira CB, Maher CG, Bindels PJE, Machado GC, Pinto RZ, et al. Recommendations for diagnosis and treatment of lumbosacral radicular pain: a systematic review of clinical practice guidelines. J Clin Med. 2021;10:2482.
Park HJ, Kim SS, Han CH, Lee SY, Chung EC, Kim MS, et al. The clinical correlation of a new practical MRI method for grading cervical neural foraminal stenosis based on oblique sagittal images. AJR Am J Roentgenol. 2014;203:412–7.
Kang Y, Lee JW, Koh YH, Hur S, Kim SJ, Chai JW, et al. New MRI grading system for the cervical canal stenosis. AJR Am J Roentgenol. 2011;197:W134-140.
Tobing SD, Aprianto P. Single level anterior cervical discectomy and fusion in multilevel herniated disc, a case report. Ann Med Surg. 2020;60:708.
Bender YY-N, Diederichs G, Walter TC, Wagner M, Liebig T, Rickert M, et al. Differentiation of osteophytes and disc herniations in spinal radiculopathy using susceptibility-weighted magnetic resonance imaging. Invest Radiol. 2017;52:75–80.
Beckworth WJ, Abramoff BA, Bailey IM, Yoon S, Umpierrez M, Kakarala A, et al. Acute cervical radiculopathy outcomes: soft disc herniations vs osteophytes. Pain Med. 2021;22:561–6.
Hilton B, Tempest-Mitchell J, Davies BM, Francis J, Mannion RJ, Trivedi R, et al. Cord compression defined by MRI is the driving factor behind the decision to operate in degenerative cervical myelopathy despite poor correlation with disease severity. PLoS ONE. 2019;14:e0226020.
Lee KH, Park HJ, Lee SY, Chung EC, Rho MH, Shin H, et al. Comparison of two MR grading systems for correlation between grade of cervical neural foraminal stenosis and clinical manifestations. Br J Radiol. 2016;89:20150971.
Eun SS, Lee H-Y, Lee S-H, Kim KH, Liu WC. MRI versus CT for the diagnosis of lumbar spinal stenosis. J Neuroradiol. 2012;39:104–9.
Tsuruda JS, Remley K. Effects of magnetic susceptibility artifacts and motion in evaluating the cervical neural foramina on 3DFT gradient-echo MR imaging. AJNR Am J Neuroradiol. 1991;12:237–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
N/A. Retrospective study. IRB approved.
Informed consent
N/A. Retrospective study. IRB approved.
Conflicts of interest
Authors 5 and 6: Employees of GE Healthcare.
Disclosures
Patrick Quarterman & Maggie Fung – Employed by GE Healthcare.
Grant support
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tran, C.V., Yang, H.R., Ahmad, Z.Y. et al. Utility of Zero-Echo time sequence as an adjunct for MR evaluation of degenerative disease in the cervical spine. Skeletal Radiol 53, 899–908 (2024). https://doi.org/10.1007/s00256-023-04507-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-023-04507-0