Abstract
Objectives
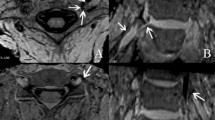
To evaluate a dynamic half-Fourier acquired single turbo spin echo (HASTE) sequence following anterior cervical discectomy and fusion (ACDF) at the junctional level for adjacent segment degeneration comparing dynamic listhesis to radiographs and assessing dynamic cord contact and deformity during flexion-extension
Methods
Patients with ACDF referred for cervical spine MRI underwent a kinematic flexion-extension sagittal 2D HASTE sequence in addition to routine sequences. Images were independently reviewed by three radiologists for static/dynamic listhesis, and compared to flexion-extension radiographs. Blinded assessment of the HASTE sequence was performed for cord contact/deformity between neutral, flexion, and extension, to evaluate concordance between readers and inter-modality agreement. Inter-reader agreement for dynamic listhesis and impingement grade and inter-modality agreement for dynamic listhesis on MRI and radiographs was assessed using the kappa coefficient and percentage concordance.
Results
A total of 28 patients, mean age 60.2 years, were included. Mean HASTE acquisition time was 42 s. 14.3% demonstrated high grade dynamic stenosis (> grade 4) at the adjacent segment. There was substantial agreement for dynamic cord impingement with 70.2% concordance (kappa = 0.62). Concordance across readers for dynamic listhesis using HASTE was 81.0% (68/84) (kappa = 0.16) compared with 71.4% (60/84) (kappa = 0.40) for radiographs. Inter-modality agreement between flexion-extension radiographs and MRI assessment for dynamic listhesis across the readers was moderate (kappa = 0.41; 95% confidence interval: 0.16 to 0.67).
Conclusions
A sagittal flexion-extension HASTE cine sequence provides substantial agreement between readers for dynamic cord deformity and moderate agreement between radiographs and MRI for dynamic listhesis.
Clinical relevance statement
Degeneration of the adjacent segment with instability and myelopathy is one of the most common causes of pain and neurological deterioration requiring re-operation following cervical fusion surgery.
Key Points
• A real-time kinematic 2D sagittal HASTE flexion-extension sequence can be used to assess for dynamic listhesis, cervical cord, contact and deformity.
• The additional kinematic cine sequence was well tolerated and the mean acquisition time for the 2D HASTE sequence was 42 s (range 31–44 s).
• A sagittal flexion-extension HASTE cine sequence provides substantial agreement between readers for dynamic cord deformity and moderate agreement between radiographs and MRI for dynamic listhesis.




Similar content being viewed by others
Abbreviations
- ACDF:
-
Anterior cervical discectomy and fusion
- ASD:
-
Adjacent segment degeneration
- HASTE:
-
Half-Fourier acquired single turbo spin echo
References
Alkosha HMA, El Adalany MA, Elsobky H, Zidan AS, Sabry A, Awad BI (2022) Flexion/extension cervical magnetic resonance imaging: a potentially useful tool for decision-making in patients with symptomatic degenerative cervical spine. World Neurosurg. https://doi.org/10.1016/j.wneu.2022.05.097
Nayak KS, Lim Y, Campbell-Washburn AE, Steeden J (2022) Real-time magnetic resonance imaging. J Magn Reson Imaging 55:81–99
Walter WR, Alizai H, Bruno M, Portugal S, Burke CJ (2021) Real-time dynamic 3-T MRI assessment of spine kinematics: a feasibility study utilizing three different fast pulse sequences. Acta Radiol 62:58–66
Duerinckx AJ, Yu WD, El-Saden S, Kim D, Wang JC, Sandhu HS (1999) MR imaging of cervical spine motion with HASTE. Magn Reson Imaging 17:371–381
Burke CJ, Samim M, Alizai H et al (2021) Clinical feasibility of 2D dynamic sagittal HASTE flexion-extension imaging of the cervical spine for the assessment of spondylolisthesis and cervical cord impingement. Eur J Radiol 134:109447
Galbraith JG, Butler JS, Dolan AM, O'Byrne JM (2012) Operative outcomes for cervical myelopathy and radiculopathy. Adv Orthop 2012:919153
Wang JC, McDonough PW, Endow KK, Delamarter RB (2000) Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 25:41–45
Saifi C, Fein AW, Cazzulino A et al (2018) Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J 18:1022–1029
Guo X, Zhou J, Tian Y, Kang L, Xue Y (2021) Biomechanical effect of different plate-to-disc distance on surgical and adjacent segment in anterior cervical discectomy and fusion - a finite element analysis. BMC Musculoskelet Disord 22:340
Matsumoto M, Okada E, Ichihara D et al (2010) Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 35:36–43
Chung JY, Kim SK, Jung ST, Lee KB (2014) Clinical adjacent-segment pathology after anterior cervical discectomy and fusion: results after a minimum of 10-year follow-up. Spine J 14:2290–2298
Wang F, Hou HT, Wang P, Zhang JT, Shen Y (2017) Symptomatic adjacent segment disease after single-lever anterior cervical discectomy and fusion: incidence and risk factors. Medicine (Baltimore) 96:e8663
Lee JC, Lee SH, Peters C, Riew KD (2015) Adjacent segment pathology requiring reoperation after anterior cervical arthrodesis: the influence of smoking, sex, and number of operated levels. Spine (Phila Pa 1976) 40:E571–E577
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81:519–528
Kaye ID, David Kaye I, Hilibrand AS (2017) Adjacent level disease-background and update based on disc replacement data. Curr Rev Musculoskelet Med 10:147–152
Chung YW, Kim SK, Park YJ (2021) Differences in the prevalence of clinical adjacent segment pathology among continents after anterior cervical fusion: meta-analysis of randomized controlled trials. J Clin Med 10:4125
Carrier CS, Bono CM, Lebl DR (2013) Evidence-based analysis of adjacent segment degeneration and disease after ACDF: a systematic review. Spine J 13:1370–1378
Burkhardt BW, Brielmaier M, Schwerdtfeger K, Sharif S, Oertel JM (2016) Smith-Robinson procedure with an autologous iliac crest graft and caspar plating: report of 65 patients with an average follow-up of 22 years. World Neurosurg 90:244–250
Burkhardt BW, Brielmaier M, Schwerdtfeger K, Oertel JM (2018) Clinical outcome following anterior cervical discectomy and fusion with and without anterior cervical plating for the treatment of cervical disc herniation-a 25-year follow-up study. Neurosurg Rev 41:473–482
Muhle C, Metzner J, Weinert D et al (1998) Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. AJNR Am J Neuroradiol 19:1763–1771
Muhle C, Weinert D, Falliner A et al (1998) Dynamic changes of the spinal canal in patients with cervical spondylosis at flexion and extension using magnetic resonance imaging. Invest Radiol 33:444–449
Zeitoun D, El Hajj F, Sariali E, Catonné Y, Pascal-Moussellard H (2015) Evaluation of spinal cord compression and hyperintense intramedullary lesions on T2-weighted sequences in patients with cervical spondylotic myelopathy using flexion-extension MRI protocol. Spine J 15:668–674
Fleck SK, Langner S, Rosenstengel C et al (2017) 3-Tesla kinematic MRI of the cervical spine for evaluation of adjacent level disease after monosegmental anterior cervical discectomy and arthroplasty: results of 2-year follow-up. Spine (Phila Pa 1976) 42:224–231
Gerigk L, Bostel T, Hegewald A et al (2012) Dynamic magnetic resonance imaging of the cervical spine with high-resolution 3-dimensional T2-imaging. Clin Neuroradiol 22:93–99
Bartlett RJ, Hill CA, Rigby AS, Chandrasekaran S, Narayanamurthy H (2012) MRI of the cervical spine with neck extension: is it useful? British J Radio 85:1044–1051
Bartlett RJ, Rigby AS, Joseph J, Raman A, Kunnacherry A, Hill CA (2013) Extension MRI is clinically useful in cervical myelopathy. Neuroradiology 55:1081–1088
Nigro L, Donnarumma P, Tarantino R, Rullo M, Santoro A, Delfini R (2017) Static and dynamic cervical MRI: two useful exams in cervical myelopathy. J Spine Surg 3:212–216
Chiavassa H, Sans N, Galy-Fourcade D et al (2000) HASTE sequence and cine-MRI evaluation of the cervical spinal canal: evaluation in 11 healthy subjects. J Radiol 81:611–617
Dalbayrak S, Yaman O, Firidin MN, Yilmaz T, Yilmaz M (2015) The contribution of cervical dynamic magnetic resonance imaging to the surgical treatment of cervical spondylotic myelopathy. Turk Neurosurg 25:36–42
Guppy KH, Hawk M, Chakrabarti I, Banerjee A (2009) The use of flexion-extension magnetic resonance imaging for evaluating signal intensity changes of the cervical spinal cord. J Neurosurg Spine 10:366–373
Michelini G, Corridore A, Torlone S et al (2018) Dynamic MRI in the evaluation of the spine: state of the art. Acta Biomed 89:89–101
Lao L, Daubs MD, Scott TP, Phan KH, Wang JC (2014) Missed cervical disc bulges diagnosed with kinematic magnetic resonance imaging. Eur Spine J 23:1725–1729
Paholpak P, Tamai K, Shoell K, Sessumpun K, Buser Z, Wang JC (2018) Can multi-positional magnetic resonance imaging be used to evaluate angular parameters in cervical spine? A comparison of multi-positional MRI to dynamic plain radiograph. Eur Spine J 27:1021–1027
Hennig J, Nauerth A, Friedburg H (1986) RARE imaging: a fast imaging method for clinical MR. Magn Reson Med 3:823–833
Stehling MK, Nitz W, Holzknecht N (1995) Fast and ultra-fast magnetic resonance tomography. Basic principles, pulse sequences and special properties. Radiologe 35:879–893
Aerts P, Van Hoe L, Bosmans H, Oyen R, Marchal G, Baert AL (1996) Breath-hold MR urography using the HASTE technique. AJR Am J Roentgenol 166:543–545
Xu N, Wang S, Yuan H, Liu X, Liu Z (2017) Does dynamic supine magnetic resonance imaging improve the diagnostic accuracy of cervical spondylotic myelopathy? A review of the current evidence. World Neurosurg 100:474–479
Fraser JF, Härtl R (2007) Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine 6:298–303
Charalampidis A, Hejrati N, Ramakonar H, Kalsi PS, Massicotte EM, Fehlings MG (2022) Clinical outcomes and revision rates following four-level anterior cervical discectomy and fusion. Sci Rep 12:5339
Tarantino U, Fanucci E, Iundusi R et al (2013) Lumbar spine MRI in upright position for diagnosing acute and chronic low back pain: statistical analysis of morphological changes. J Orthop Traumatol 14:15–22
Sundseth J, Jacobsen EA, Kolstad F, Nygaard OP, Zwart JA, Hol PK (2013) Magnetic resonance imaging evaluation after implantation of a titanium cervical disc prosthesis: a comparison of 1.5 and 3 Tesla magnet strength. Eur Spine J 22:2296–2302
Chen CJ, Hsu HL, Niu CC et al (2003) Cervical degenerative disease at flexion-extension MR imaging: prediction criteria. Radiology 227:136–142
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Christopher Burke.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
None of the study subjects or cohorts have been previously reported.
Methodology
-
retrospective
-
cross sectional study
-
performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 130 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Burke, C.J., Samim, M., Babb, J.S. et al. Utility of a 2D kinematic HASTE sequence in magnetic resonance imaging assessment of adjacent segment degeneration following anterior cervical discectomy and fusion. Eur Radiol 34, 1113–1122 (2024). https://doi.org/10.1007/s00330-023-10133-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10133-0