Abstract
Background
Microsurgical training is currently limited by high costs, lack of equipment and infrastructure, increasing concerns about patient safety and expectations, which have resulted in a perception of deficit in the training of new surgeons. Therefore, simulated models offer controlled and effective training, minimizing animal use.
Methods
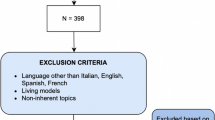
A simple and economical protocol was designed and applied in microsurgery training using exvivo models in 11 plastic surgery residents, lasting 40 h, during 13 sessions (3 h each), with a theoretical module and an explanatory video, supervised and given feedback by an expert. The initial assessment (IA) and a final assessment (FA) were recorded on video, subsequently evaluated by two blinded experts according to OSATS regulations, recording the tremor of participants using Apple Watch. A univariate and multivariate analysis were performed.
Results
All participants improved overall performance scores. In non-living models, IA = 19.6 points (CI: 16.2–23.1%) versus FA = 29.6 points (CI: 21.8–32%), and in ex vivo models, IA = 15.5 points (CI: 12.2–18%) versus FA = 23.9 points (CI: 19.3–28.5%), p = 0.005. Greater impact was identified in exercises that involve manipulation of fine elements, dexterity, precise movements, respect for the tissue, use of irrigation, saving sutures, and knotting techniques. No statistically significant improvement was found in tremor. No association was found with better performance for participants who engaged in extracurricular or meditation activities.
Conclusions
This curriculum allows for structured and sequential training in exvivo models, with a statistically significant improvement in global microsurgery performance scores among participants.
Level of evidence: Not ratable.







Similar content being viewed by others
Data Availability
The information supporting the data presented in graphs 2, 3 and 4 is from data collected during the study and not publicly available in order to protect participants privacy, but the data is available on request. Graph 1 and Figures 1, 2 and 3 are the product of the lab sessions and are publicly available in the figshare repository, as part of this record: https://figshare.com/s/a1ba1bdc7dc0c3cb1288.
References
Murray CJL, Vos T, Lozano R et al (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2197–2223. https://doi.org/10.1016/S0140-6736(12)61689-4
Chouari TAM, Lindsay K, Bradshaw E et al (2018) An enhanced fresh cadaveric model for reconstructive microsurgery training. Eur J Plast Surg 41(4):439–446. https://doi.org/10.1007/s00238-018-1414-3
Holler JT, Albright P, Challa S et al (2019) Barriers to performing soft tissue reconstruction procedures among orthopedic surgeons in low- and middle-income countries. Plast Reconstr Surg Glob Open 7(10):e2420. https://doi.org/10.1097/gox.0000000000002420
Reznick RK, MacRae H (2006) Teaching surgical skills — Changes in the wind. N Engl J Med 355(25):2664–9. https://doi.org/10.1056/NEJMra054785
Chikwe J, de Souza AC, Pepper JR (2004) No time to train the surgeons. BMJ 328(7437):418–419. https://doi.org/10.1136/bmj.328.7437.418
Kempenich JW, Willis RE, Rakosi R, Wiersch J, Schenarts PJ (2015) How do perceptions of autonomy differ in general surgery training between faculty, senior residents, hospital administrators, and the general public? A multi-institutional study. J Surg Educ 72(6):e193–e201. https://doi.org/10.1016/j.jsurg.2015.06.002
Almeland SK, Lindford A, Sundhagen HP et al (2020) The effect of microsurgical training on novice medical students’ basic surgical skills—a randomized controlled trial. Eur J Plast Surg 43(4):459–466. https://doi.org/10.1007/s00238-019-01615-w
Gul BU, Yanilmaz DK, Arslan D, Bayramicli M, Akbulut O (2019) Silicone-based simulation models for peripheral nerve microsurgery. J Plast Reconstr Aesthet Surg 72(3):477–483. https://doi.org/10.1016/j.bjps.2018.10.025
Ali S (2018) Basic microvascular anastomosis simulation hub microsurgery course: an innovative competency-based approach to microsurgical training for early year’s plastic surgery trainees. Ann Plast Surg 80(4):314–315. https://doi.org/10.1097/SAP.0000000000001390
Javid P, Aydın A, Mohanna PN, Dasgupta P, Ahmed K (2019) Current status of simulation and training models in microsurgery: a systematic review. Microsurgery 39(7):655–668. https://doi.org/10.1002/micr.30513
Odobescu A, Moubayed SP, Danino MA (2016) Thiel cadaveric nerve tissue: A model for microsurgical simulation. J Brachial Plex Peripher Nerve Inj 11(1):18–20. https://doi.org/10.1055/s-0036-1580626
Grober ED, Hamstra SJ, Wanzel KR et al (2004) The educational impact of bench model fidelity on the acquisition of technical skill: the use of clinically relevant outcome measures. Ann Surg 240(2):374–381. https://doi.org/10.1097/01.sla.0000133346.07434.30
Reichenberger M, Gazyakan E, Kohler S, Germann G, Engel H (2009) A new, custom-made device for flap protection in experimental rats. Microsurgery 29(6):504–506. https://doi.org/10.1002/micr.20654
Javid P, Aydın A, Mohanna PN, Dasgupta P, Ahmed K (2019) Current status of simulation and training models in microsurgery: a systematic review. Microsurgery 39(7):655–668. https://doi.org/10.1002/micr.30513
Vinagre G, Villa J, Amillo S (2017) Microsurgery training: does it improve surgical skills? J Hand Microsurg 09(01):047–048. https://doi.org/10.1055/s-0037-1599222
Ghanem A, Kearns M, Ballestín A et al (2020) International Microsurgery Simulation Society (IMSS) consensus statement on the minimum standards for a basic microsurgery course, requirements for a microsurgical anastomosis global rating scale and minimum thresholds for training. Injury 51(xxxx):S126-S130. https://doi.org/10.1016/j.injury.2020.02.004
Zambrano LC, Alarcon DF, Díaz KD, Rodriguez MA, Melendez GL, Ramirez MA (2023) Dye-perfused human placenta for simulation in a microsurgery laboratory for plastic surgeons. Arch Plast Surg Published online June 20, 2023. https://doi.org/10.1055/a-2113-4182
Reznick R, Regehr G, MacRae H, Martin J, McCulloch W (1997) Testing technical skill via an innovative “bench station” examination. Am J Surg 173(3):226–230. https://doi.org/10.1016/S0002-9610(97)89597-9
Martin JA, Regehr G, Reznick R et al (1997) Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 84(2):273–278. https://doi.org/10.1002/bjs.1800840237
Nugent E, Joyce C, Perez-Abadia G et al (2012) Factors influencing microsurgical skill acquisition during a dedicated training course. Microsurgery 32(8):649–656. https://doi.org/10.1002/micr.22047
Ezra DG, Aggarwal R, Michaelides M et al (2009) Skills acquisition and assessment after a microsurgical skills course for ophthalmology residents. Ophthalmology 116(2):257–262. https://doi.org/10.1016/j.ophtha.2008.09.038
Camacho FJ, Rojas MA, Cir RC, Original C (2016) Determinación de los niveles de competencia para entrenamiento básico en microcirugía. Rev Colombiana Cir 31(4):240–247. https://doi.org/10.30944/20117582.299
Fargen KM, Turner RD, Spiotta AM (2016) Factors that affect physiologic tremor and dexterity during surgery: a primer for neurosurgeons. World Neurosurg 86:384–389. https://doi.org/10.1016/j.wneu.2015.10.098
Hanrahan J, Sideris M, Pasha T et al (2018) Hands train the brain—what is the role of hand tremor and anxiety in undergraduate microsurgical skills? Acta Neurochir (Wien) 160(9):1673–1679. https://doi.org/10.1007/s00701-018-3609-6
Verrelli DI, Qian Y, Wood J, Wilson MK (2016) Measurement of tremor transmission during microsurgery. Int J Med Robot Comput Assist Surg 12(4):585–597. https://doi.org/10.1002/rcs.1717
Lemoyne R, Mastroianni T, Cozza M, Coroian C, Grundfest W (2010) Implementation of an iPhone for characterizing Parkinson’s disease tremor through a wireless accelerometer application. Annu Int Conf IEEE Eng Med Biol Soc. 2010:4954–8. https://doi.org/10.1109/IEMBS.2010.5627240
Vescio B, Quattrone A, Nisticò R, Crasà M, Quattrone A (2021) Wearable devices for assessment of tremor. Front Neurol 12. https://doi.org/10.3389/fneur.2021.680011
Araújo R, Tábuas-Pereira M, Almendra L et al (2016) Tremor frequency assessment by iPhone® applications: correlation with EMG analysis. J Parkinsons Dis 6(4):717–721. https://doi.org/10.3233/JPD-160936
Mustafa Erol Demirseren, Yasuyoshi Tosa YH (2003) Microsurgical training with surgical gauze: the first step. J Reconstr Microsurg 19(6):385–386. https://doi.org/10.1055/s-2003-42634
Kaufman T, Hurwitz DJ, Ballantyne DL (1984) The foliage leaf in microvascular surgery. Microsurgery 5(1):57–58. https://doi.org/10.1002/micr.1920050113
Crosby NL, Clapson JB, Buncke HJ, Newlin L (1995) Advanced non-animal microsurgical exercises. Microsurgery 16(9):655–658. https://doi.org/10.1002/micr.1920160913
Ilie VG, Ilie VI, Dobreanu C, Ghetu N, Luchian S (2009) Training of microsurgical skills on nonliving models. Microsurgery 28:571–577. https://doi.org/10.1002/micr
Creighton FX, Feng AL, Goyal N, Emerick K, Deschler D (2017) Chicken thigh microvascular training model improves resident surgical skills. Laryngoscope Investig Otolaryngol 2(6):471–474. https://doi.org/10.1002/lio2.94
Ribeiro De Oliveira MM, Ferrarez CE, Ramos TM et al (2018) Learning brain aneurysm microsurgical skills in a human placenta model: predictive validity. J Neurosurg 128(3):846–852. https://doi.org/10.3171/2016.10.JNS162083
Rodriguez JR, Yañez R, Cifuentes I, Varas J, Dagnino B (2016) Microsurgery workout: a novel simulation training curriculum based on nonliving models. Plast Reconstr Surg 138(4):739e–747e. https://doi.org/10.1097/PRS.0000000000002456
Lascar I, Totir D, Cinca A et al (2007) Training program and learning curve in experimental microsurgery during the residency in plastic surgery. Microsurgery 27(4):263–267. https://doi.org/10.1002/micr.20352
Kang BY, Jeon BJ, Lee KT, Mun GH (2017) Comprehensive analysis of chicken vessels as microvascular anastomosis training model. Arch Plast Surg 44(1):12–18. https://doi.org/10.5999/aps.2017.44.1.12
Magaldi M, Oliveira R De, Nicolato A et al (2015) Face, content, and construct validity of human placenta as a haptic training tool in neurointerventional surgery. Published online:1–3. https://doi.org/10.3171/2015.1.JNS141583
Krishnan KG, Dramm P, Schackert G (2004) Simple and viable in vitro perfusion model for training microvascular anastomoses. Microsurgery 24(4):335–338. https://doi.org/10.1002/micr.20031
Banda CH, Georgios P, Narushima M, Ishiura R, Fujita M, Goran J (2019) Challenges in global reconstructive microsurgery: the sub-Saharan african surgeons’ perspective. JPRAS Open 20:19–26. https://doi.org/10.1016/j.jpra.2019.01.009
Moustaki M, Masud D, Hachach-Haram N, Mohanna PN (2017) Effect of computer games and musical instruments on microsurgery. J Plast Reconstr Aesthet Surg 70(7):982–984. https://doi.org/10.1016/j.bjps.2017.02.014
Tannenbaum J, Bennett BT (2015) Russell and Burch’s 3Rs then and now: the need for clarity in definition and purpose. J Am Assoc Lab Anim Sci 54(2):120–132
De Maria F, Pinto V, Pinelli M et al (2023) Microsurgery courses vs continuous microsurgery laboratory training: an Italian experience. Eur J Plast Surg 46(6):1383–1388. https://doi.org/10.1007/s00238-023-02132-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Competing interests
None.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Universidad Industrial de Santander and Hospital Universitario de Santander (Act No 1, February 5, 2021) and Hospital Universitario de Santander (Act No 08, June 18, 2021).
Consent to participate
Written consent was obtained from the residents for participate and sharing their data and photos.
Consent to publish
Written consent was obtained from the residents for sharing their data and photos.
Additional information
Editor: Horacio F Mayer, MD, FACS.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zambrano-Jerez, L.C., Ramírez-Blanco, M.A., Alarcón-Ariza, D.F. et al. Novel and easy curriculum with simulated models for microsurgery for plastic surgery residents: reducing animal use. Eur J Plast Surg 47, 36 (2024). https://doi.org/10.1007/s00238-024-02177-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00238-024-02177-2