Abstract
Summary
Our study demonstrates a strong increase in utilization of inpatient health care and clear excess costs in older people in the first year after pelvic fracture, the latter even after adjustment for several confounders. Excess costs were particularly high in the first few months and mainly attributable to inpatient treatment.
Introduction
We aimed to estimate health care utilization and excess costs in patients aged minimum 60 years up to 1 year after pelvic fracture compared to a population without pelvic fracture.
Methods
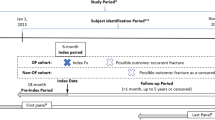
In this retrospective population-based observational study, we used routine data from a large statutory health insurance (SHI) in Germany. Patients with a first pelvic fracture between 2008 and 2010 (n=5685, 82% female, mean age 80±9 years) were frequency matched with controls (n=193,159) by sex, age at index date, and index month. We estimated health care utilization and mean total direct costs (SHI perspective) with 95% confidence intervals (CIs) using BCA bootstrap procedures for 52 weeks before and after the index date. We calculated cost ratios (CRs) in 4-week intervals after the index date by fitting mixed two-part models including adjustment for possible confounders and repeated measurement. All analyses were further stratified for men/women, in-/outpatient-treated, and major/minor pelvic fractures.
Results
Health care utilization and mean costs in the year after the index date were higher for cases than for controls, with inpatient treatment being particularly pronounced. CRs (95% CIs) decreased from 10.7 (10.2–11.1) within the first 4 weeks to 1.3 (1.2–1.4) within week 49–52. Excess costs were higher for inpatient than for outpatient-treated persons (CRs of 13.4 (12.9–13.9) and 2.3 (2.0–2.6) in week 1–4). In the first few months, high excess costs were detected for both persons with major and minor pelvic fracture.
Conclusion
Pelvic fractures come along with high excess costs and should be considered when planning and allocating health care resources.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low-energy pelvic fractures, which are mainly a result of simple falls among older people [1,2,3,4], are assumed to affect a growing number of individuals. In line, an increase of the incidence of pelvic fracture has already been reported [4,5,6,7,8]. In Germany, the incidence of pelvic fractures among older people was estimated to be even higher when compared to other countries [9]. For the same study population, excess mortality was found in the first 8 months after pelvic fracture even after adjustment for age, sex, insurance region, level of care, comorbidity, health care cost, and type of pelvic fracture [10]. Due to the worldwide demographic change and an aging population, pelvic fractures will gain increasing relevance for the society in general and for the German health care system in particular [11]. In addition to developing and monitoring prevention programs, it is necessary to describe health care utilization and determine the burden of pelvic fractures in monetary terms. This knowledge is, for example, needed for planning and allocating health care resources. It is well known that hip fractures are the most expensive fractures on a per-patient basis [12,13,14,15]. In comparison, there is only little evidence regarding the financial burden of pelvic fractures, although there are hints that pelvic fractures contribute to high costs as well [13, 14, 16]. Up to now, we have not identified any study that evaluated fracture severity, i.e., major or minor pelvic fractures. The aim of this study was to estimate health care utilization and excess costs in patients aged 60 years or older after a pelvic fracture compared to people without a pelvic fracture in Germany, based on data from a large statutory health insurance company (SHI). In sex-stratified analyses, particular attention was paid to the treatment setting and severity of fracture.
Material and methods
Study Design, data source, and population
The study is a retrospective population-based observational study. Routine data on health care provision was provided by a large SHI in Germany, the AOK NordWest. Overall, the AOK NordWest covers around 2.8 million people in two regions—Schleswig-Holstein (700,000 people) and Westfalen-Lippe (2.1 million people)—of whom about 29% are 60 years or older. We included all people aged 60 years or older who were continuously insured for at least 1 year between January 1, 2007, and December 31, 2011 (4,511,645 person-years at risk). The selection process is presented in detail elsewhere [9].
Ascertainment of cases with pelvic fracture events and controls without pelvic fracture
All insured persons with a first pelvic fracture between 2008 and 2010 were identified. In brief, pelvic fractures along with the exact week of occurrence were identified in inpatient and outpatient data according to the 10th revision of the International Classification of Diseases (ICD-10). A fracture event was defined by the following ICD-10 codes and classified into a major or minor pelvic fracture according to clinicians’ decision: S32.1 (fracture of sacrum, major), S32.2 (fracture of coccyx, minor), S32.3 (fracture of ilium, major), S32.4 (fracture of acetabulum, major), S32.5 (fracture of pubis, minor), S32.81 (fracture of ischium, minor), S32.83 (fracture of pelvis unspecified, minor), and S32.89 (multiple and other fractures of pelvis, major). Only persons with a first fracture defined by an event-free period of at least 1 year prior to the event were included. For further analyses, we distinguished between persons with exclusively outpatient-treated and at some point inpatient-treated pelvic fracture within 1 year after the event. First pelvic fractures were considered inpatient-treated fractures, when insured persons had at least one hospital admission with a diagnosis of a pelvic fracture during the whole study period in line with a previous study conducted by the authors [9]. A pelvic fracture was classified as a major pelvic fracture if at least one major ICD-10 code occurred during the index week. To ensure complete cost data, we excluded persons who were not insured at least one complete year after the first fracture, with the only exception of death during this time (exclusion 4.4% of all persons with a fracture between 2008 and 2010) [9]. Persons with a first pelvic fracture in 2008–2010 (“case”) and controls without pelvic fractures during the whole study period were frequency matched by sex, age (in integer years, one class for age ≥100 years), and index month. The index date was the date of the first pelvic fracture for cases and was randomly selected in the insurance period of the controls. The requirement of continuously insured time periods for the controls was the same as for cases. In the end, the sample comprised 5685 cases with and 193,159 controls without a pelvic fracture, equivalent to a mean matching rate of 1 to 34. No further selection of the controls was done. This implies more precise estimates in controls and simplifies subgroup analyses. The overall power is limited by the number of cases.
Assessment of health care utilization and costs
Health care utilization considering place and type of service, namely, inpatient care, outpatient care, outpatient drug prescriptions, rehabilitation, and received sickness benefit, was assessed. Direct net costs from the perspective of the SHI were assessed in total and separately for inpatient care, outpatient care, prescribed outpatient medication, and rehabilitation. Co-payments from the patients are not included. All costs were assessed in euro (€). Additionally, sickness benefit was considered as transfer payment and stratified for cases and controls. Since our base year was 2011, all costs were adjusted to 2011 using the general consumer price index. Mean total costs included (a) inpatient costs: total costs of treatment of each hospitalization excluding costs for outpatient hospital services; (b) outpatient costs: costs of outpatient consultations, which are expressed as fees for all outpatient services, including extra-budgetary services and costs of dialysis treatment; (c) medication costs: costs of each outpatient medication; (d) total costs of rehabilitation; and (e) total costs of sickness benefit. Outpatient costs were available only quarterly (as in Germany most outpatient services are reimbursed once in a quarter) and equally distributed over the weeks of the quarter.
Assessment of further variables
The following variables were included as possible confounders and are already described in full detail elsewhere [10]: age in 5-year age groups, sex, index year, insurance region as an approximation for the residence of the insured person, level of care according to the German legislation on social care insurance [17], comorbidity assessed by using the enhanced Charlson comorbidity algorithm for ICD-10 codes [18,19,20,21,22,23], health care cost consisting of inpatient and outpatient care, medications, rehabilitation, and sickness benefit accumulated in the year before the index week, death, and observation/survival time. For people who died during the observation period, the corresponding week of death was recorded. Additionally, observation time was considered, which equals survival time in weeks since the index week. Our selection of confounders was based on literature evidence [14, 24, 25] and clinical experience.
Statistical analyses
Patient characteristics in the index week were described by frequency tables, means ± standard deviations. Analyses were stratified by cases (all, inpatient-/outpatient-treated fractures, minor/major fractures) with controls as reference. The frequency matching ensured an adequate overall adjustment regarding age and gender. Frequency matching was not stratified for the different subgroups (e.g., for inpatient and outpatient cases) to avoid different control populations. However, in the fully adjusted models, adjustment was performed for confounders including sex and age. Prevalence of health care utilization as well as mean values for health care utilization for cases and controls were estimated along with 95% BCA bootstrap confidence intervals [26] to compare cases and controls 52 weeks before and after the index date. Mean total costs were calculated cumulatively for a total of 52 weeks before the index date. Health care costs 52 weeks before the index date were categorized in approximate quintile classes (€ 0–499, 500–999, 1000–1999, 2000–4999, 5000+) to get more robust results from the adjusted models (described below). After the index date, costs were on the one hand cumulated for 52 weeks and on the other hand proportionally divided in 13 time intervals of 4 weeks, in order to investigate the development of costs for cases and controls more closely. In each time interval, only data of surviving patients were included. There are alternative methods to describe excess costs (please see also Comparison to previous studies). One way is to calculate cost differences by subtracting the mean cost of controls from the mean cost of cases, as done in this manuscript for instance, to provide an estimate along with a 95% BCA bootstrap confidence interval for the absolute mean difference of annual total costs between cases and controls. Since the relation between costs for cases and controls is easier to understand and in order to facilitate interpretation of the data and improve legibility, excess costs were expressed as cost ratios and not as differences (subtracted costs). Cost outcomes were investigated by fitting uncorrelated mixed multiple two-part models [27] as follows: Firstly, in small but non-negligible (about 9%) percentages, there were zero values of costs for patients without a pelvic fracture in the follow-up intervals of 4 weeks and also for some cases in the time course after the pelvic fracture. In the first part of the model, the probability of “health care utilization” was used as a binary outcome, and relative risks (RRs) were estimated for independent variables (per unit change). Instead of a log-binomial model, a Poisson model with robust variance estimation was used to get stable results [28]. In the second part, a gamma model with log-link was fitted on the subpopulation with positive costs estimating CRs for unit changes of independent variables [29]. Both parts of the model were assumed to be approximately independent because of low percentages of zero costs. However, a valid estimation of correlations between all random effects in a correlated two-part model cannot be expected taking into account the efforts to get stable results in the first part of the model. A joint model was derived by multiplication of the RR and CR to get a joint CR corresponding to the overall means for the unit change of each independent variable. Variances and confidence intervals of the CRs in the joint model were calculated using log transformation. Independent variables were case (all or inpatient/outpatient or major/minor cases) versus control, time, and interaction time * case/control. Furthermore, adjusted models were fitted comprising the above named prespecified possible confounders including an interaction term for health care costs in the year before * case/control. Furthermore, high costs because of death were adjusted by including the confounder death and survival time. Adjustment for repeated measurement was performed by covariance patterns [30]. All analyses were performed separately for men and women. For the statistical analyses the software package SAS was used (SAS for X64_10PRO, Release 9.4, SAS Institute Inc. Cary, NC, USA).
Results
Characteristics of the study population
The study cohort comprised 5685 persons (n=4689 (82.5%) women) with a first pelvic fracture between 2008 and 2010, as well as 193,159 persons (n=154,960 (80.2%) women) without a pelvic fracture. The mean age (± standard deviation) was 80.3±8.7 (81.0±8.4 in women and 76.9±9.3 in men) for cases and 79.1 ± 8.4 years (79.8 ± 8.2 years in women and 76.2 ± 8.7 years in men) for controls. Further characteristics for cases and controls are summarized in Table 1. Overall, of 5685 persons with pelvic fracture, 4214 (74.1%) were at some point inpatient treated (for pelvic fracture within 1 year after the event), and 3646 (64.1%) had a major pelvic fracture. About 82.7% of major pelvic fractures were at some point inpatient treated. Yet, more than half of the minor pelvic fractures (58.8%) were at some point inpatient treated, too. Table 2 shows selected characteristics in more detail.
Health care utilization 1 year before the index date and in the year after
Table 3 shows health care utilization 52 weeks before and after the index date for the whole sample and stratified for men and women. Hospitalization, outpatient care, and prescriptions were frequently used, whereas rehabilitation and payment of sickness benefit for cases and controls did not contribute much to the overall health care utilization. In the year before the index date, health care use was higher in cases than in controls, particularly hospitalization. In the year after the index date, occurrence of inpatient care rose to almost 90% for cases, while it stayed almost the same for controls. No large difference was seen for outpatient care compared to the year before, although prevalence for cases was slightly lower than in the year before (but still > 98%). The number of outpatient drug prescriptions increased for cases and did not alter much for controls. Although a slight increase in occurrence of rehabilitation and payment of sickness benefit could be observed, the overall impact was still small. Comparing all components for cases, the largest change was seen in inpatient treatment. For controls, the development of health care utilization in the year after the index date was without striking deviations. There was only a small difference between cases and controls for men and women. However, the number of prescribed outpatient drugs was slightly higher for women—again higher for female cases than female controls—and increased in the year after the index date for the female cases. Table 4 reports health care utilization for at some point inpatient and exclusively outpatient-treated persons as well as patients with major and minor pelvic fractures. In the year before the index date, almost similar results were observed. Health care utilization in the year after the index date was clearly higher in inpatients compared to outpatients, in particular hospitalization. Inpatient care increased to over 90% for major pelvic fractures and about 80% for minor pelvic fractures.
Mean costs 1 year before the index date and in the year after
Mean total costs for the whole sample and stratified for men and women are also shown in Table 3. The observed overall pattern was similar to that described for health care utilization. Previous-year costs were higher in cases. While the mean total costs for the cases were nearly doubled compared to the previous year, the mean total costs for controls almost stayed the same. The absolute mean difference of total costs between cases and controls (95% CIs) in the year after the index date was €7317 (6992–7691). Thus, a disproportionate increase in the cost of cases compared to controls was observed, mainly driven by costs for inpatient care. Unadjusted absolute mean differences of different costs and subgroups can be calculated from the estimates in Tables 3 and 4.
In the year before and after the index date, the costs in total and all cost components were generally higher for men than for women in cases and controls. An exception were costs for outpatient drug prescriptions and rehabilitation which were higher for female cases.
Table 4 also displays mean total costs for at some point inpatient and exclusively outpatient-treated persons as well as patients with major and minor pelvic fractures. In contrast to the year after the index date, mean total costs and their cost components did not differ considerably for inpatient-treated and outpatient-treated persons in the year before. However, costs for inpatients were already a bit higher than for outpatients. In the year after the index date, costs for inpatient-treated cases were twice as high as for outpatient-treated cases, again driven by costs for hospitalization. Mean costs for outpatient care and outpatient drug prescriptions were slightly lower for inpatients than for outpatients.
In the year before the index date, the mean total costs for persons with major and minor fractures were almost the same. In total and for some components costs were slightly higher for persons with minor fracture. In the year after the index date, the mean total costs for major fractures exceeded the costs for minor fractures. The largest increase in costs was attributable to inpatient care, where costs almost doubled for minor pelvic fractures and were about 2.5 times higher for major pelvic fractures compared to the year before.
Excess costs after pelvic fracture (two-part models and cost ratios)
Table 5 shows the fully adjusted CRs (95% CI) for the 4-week periods up to 52 weeks for the total sample and for at some point inpatient-treated and exclusively outpatient-treated persons. Overall, significant excess costs were observed until 52 weeks after the index date. CRs decreased during the 52 weeks from 10.7 (10.2–11.1) in week 1–4 to 1.3 (1.2–1.4) in week 49–52. Excess costs in men and women were quite similar.
Moreover, fully adjusted CRs were elevated until week 52 for inpatient-treated persons and until week 44 for outpatient-treated persons. For inpatient-treated persons, the fully adjusted CR was 13.4 (12.9–13.9) in week 1–4. Outpatient-treated persons showed a fully adjusted CR of 2.3 (2.0–2.6) in week 1–4 weeks after pelvic fracture.
Table 5 also contains fully adjusted CRs (95% CI) for the 4-week periods up to 52 weeks for persons with major and minor pelvic fractures. CRs express excess costs for persons with major and minor pelvic fractures when compared with persons without a pelvic fracture. Fully adjusted CRs for persons with major pelvic fracture were 11.9 (11.4-12.4) in the first 4 weeks and 1.2 (1.1-1.4) in week 49-52 after the index date. Excess costs (CRs) for minor pelvic fractures were high (but not comparable) in the beginning, too: From 8.5 (7.9–9.1) in the fully adjusted model in week 1–4, they lowered to 1.3 (1.1–1.5) in week 49–52.
Discussion
Main findings
By using longitudinal SHI data from a large population-based sample, we were able to assess health care utilization and costs in great detail and provide accurate estimates. Our results are broadly in line with our expectations: It was found that in the year after the index date, health care utilization of persons with pelvic fracture increased compared to the year before, with utilization of inpatient treatment being particularly noticeable. Accordingly, our study showed high costs with a disproportionate increase in the year after pelvic fracture, especially for inpatient care. However, it has to be taken into account that already in the year before the index date, health care use and costs were higher in cases than in controls. This leads to the conclusion that cases were sicker than the controls. Excess costs (adjusted for confounders) were observed in the complete year after a pelvic fracture—which was somewhat surprising—with a fairly similar pattern in men and women. Excess costs were particularly high in the first 4 weeks after pelvic fracture and lowered substantially in later weeks. Already in weeks 5–8, they were only about half as high as in the first period, with the only exception of excess costs for outpatient-treated persons (which were rather low in comparison). Excess costs were highest for inpatient-treated persons. In the first few months, high excess costs were detected for persons with major and persons with minor pelvic fracture (when compared with persons without a pelvic fracture), although excess costs for minor fractures occurred to a lesser extent.
Comparison to previous studies
The comparison with existing studies is limited due to differences in study design, study period, study population, and methods used for cost analysis. Since most studies are carried out in the USA, a comparison with German data is considerably limited due to the different health care and insurance systems. Overall, we identified no study which analyzed excess cost in time intervals of 4 weeks in the year after the index date. However, there were three studies that examined direct medical costs in older people after a pelvic fracture based on administrative data using different approaches [13, 14, 16]. Ohsfeldt et al. [13] provided estimates of fracture-related direct medical costs and data on health care utilization in a managed care setting for patients with a mean age of 70 years with a primary diagnosis for a fragility non-vertebral fracture, including pelvic fracture, during the first year following the event. They analyzed cost per fracture for the first month separately. Results were stratified for outpatient, inpatient, long-term care, and other. However, by using this approach, no excess/incremental costs were reported. Kilgore et al. [16] conducted a retrospective, person-level, and pre-/post-fracture analysis among a sample of Medicare beneficiaries aged 65 years or older and presented incremental and attributable payments in the 6 months after the fracture event for various closed fractures, among other pelvic fractures. In their study, costs for drug prescription and institutional care are missing. Pike et al. [14] described resource use, as well as direct and indirect costs for Medicare patients at age 65 or older in the first year after a fracture. Osteoporotic fracture cases, including patients with pelvic fracture, were matched randomly on age, sex, geographic region, and race to controls with osteoporosis and no fractures. Cost differences between patients and controls were calculated as excess costs. It has to be kept in mind that this study only included patients with diagnosed osteoporosis, which might lead to a selection bias, since relevant patient groups, e.g., undiagnosed patients or patients with osteopenia, are not analyzed. In line with our findings, these three studies confirm high costs in the year after the fracture. Ohsfeldt et al. [13] reported that the costs for pelvic fractures were particularly high in the first month after fracture. Eighty-eight percent of annual costs occurred during this period, which may be due to the approach used, among other reasons. In our study, 30% of the costs of cases and 9% of the costs of controls were incurred within the first month. Pike et al. found high excess costs for Medicare patients within the first year after pelvic fracture/other non-vertebral fractures and therefore examined the economic burden of various fractures over a 2-year period, but only in a privately insured population aged 18–64 years [15]. Comparable to our study, most pelvic fractures were treated in an inpatient care setting, so most costs occurred for inpatient care as well [13, 14]. In our study, 74% of pelvic fracture patients were at some point inpatient treated. Mean inpatient care costs for these patients were €9907, which is approximately 78% of total costs for this patient group. Similar to our results, Ohsfeldt et al. [13] reported that 70% of patients with a pelvic fracture required a hospital stay, causing 86% of fracture-related direct medical costs. Since pelvic fractures come along with high costs, the comparison of major or minor pelvic fracture is of particular interest. It seems possible that the procedures for diagnosis and treatment of major and minor pelvic fractures are rather similar. This argument could explain why we found excess costs for both. To our knowledge, no other study provides findings stratified for major and minor fractures. Our study is therefore an expansion of existing research. However, future research should be conducted.
Implications
As we have already shown, incidence rates of pelvic fracture in Germany are considerably high [9]. The already high health care utilization and excess costs among older people with pelvic fractures—which might further increase due to the demographic change—need to be recognized in the future for planning and allocating health care resources, especially for inpatient treatment. The planning and allocation of resources should not be done in isolation but should take into account all diseases with high excess costs (e.g., chronic diseases like diabetes). The data can also be used for cost effectiveness analysis in the context of prevention.
Limitations and strengths
Several limitations need to be considered: First, we used only specific ICD-10 coding for pelvic fracture and the underlying causes of injury were not recorded. Thus, the level of associated trauma was missing, and we could not distinguish between low-energy and high-energy fractures. However, we assume that the vast majority of pelvic fractures are caused by low-energy trauma resulting from simple falls. Second, clinical parameters could not be described, which could limit the presentation of the study population and interpretation of the results. However, we were able to adjust for comorbidity in a reasonable way, and thus at least consider the coexistence of diseases in terms of cost. Third, we made use of the general consumer price index. However, in many countries, the inflation in health sector outstrips that in general goods. Fourth, due to data limitations, the costs of care services that are covered by the SHI (which also includes payments of the care insurance) could not be included in our analysis, although they are considered a relevant cost component. Fortunately, we were able to perform a descriptive analysis in a subpopulation with complete care costs. It appeared that mean costs of care services, which were higher for cases than for controls, were the second largest component of mean total costs (after costs for inpatient care) 52 weeks after the index date. Initially, the costs of care services for cases did not differ substantially from controls after the index date, but they increased over time to a relatively constant level. This could be explained by the facts that during the frequent inpatient stays at the beginning, fewer costs of care services are incurred and that some persons only need additional care services after the pelvic fracture, so that the costs do not start to count until later in time. Overall, results have to be interpreted with caution, since the subpopulation was selected, the sample size was small—even more limited in subgroups—and large variances were observed. In future research, it would be interesting to examine these findings with more recent and comprehensive data. Fifth, we could only use SHI data up to 2011, which might raise questions regarding the timeliness of the results. However, since no major administrative changes have taken place in Germany in recent years with regard to health care utilization or reimbursement considering pelvic fractures, the study provides relevant insights on health care utilization and costs after pelvic fracture. Sixth, bias from mortality was induced in different directions, which cannot be adjusted by a simple confounding term in the model. There might be further interactions between time and confounders (time specific confounding), as well. We decided not to fit models including interactions between time and confounders, because we expected serious runtime and convergence problems.
Our study has several strengths: First, we were able to analyze longitudinal SHI data from a large population-based sample and take into account a number of possible confounders. Second, since personalized individual data was available 1 year before and 1 year after the event, it was possible to track all insured persons over a long observation period. Finally, we conducted an exact assessment of fracture events, especially regarding treatment setting and fracture severity, and were thus able to gain new insights into the occurrence of health care utilization and costs.
Conclusions
Our study demonstrates a strong increase in utilization of inpatient health care and clear excess costs in older people in the first year after pelvic fracture, the latter even after adjustment for several confounders. Excess costs were particularly high in the first month and again mainly attributable to inpatient treatment. Subgroup analyses regarding treatment setting and severity of fracture reveal substantial differences and provide specific insights for appropriate planning and allocation of health care resources.
Availability of data and material
Data are subject to the legal data protection laws and only available in an aggregated form upon formal request. The contact person is Dr. Burkhard Haastert, responsible Biostatistican of the project group, mediStatistica, 58809 Neuenrade, and associate researcher at the Institute for Health Services Research and Health Economics, Faculty of Medicine, Heinrich-Heine-University Düsseldorf, Germany, who needs to be contacted at haastert@medistatistica.de.
Code availability
Not applicable
References
Balogh Z, King KL, Mackay P, McDougall D, Mackenzie S, Evans JA, Lyons T, Deane SA (2007) The epidemiology of pelvic ring fractures: a population-based study. J Trauma 63:1066–1073. https://doi.org/10.1097/TA.0b013e3181589fa4
Kelsey JL, Prill MM, Keegan THM, Quesenberry CP Jr, Sidney S (2005) Risk factors for pelvis fracture in older persons. Am J Epidemiol 162:879–886. https://doi.org/10.1093/aje/kwi295
Court-Brown CM, Clement ND, Duckworth AD, Biant LC, McQueen MM (2017) The changing epidemiology of fall-related fractures in adults. Injury 48:819–824. https://doi.org/10.1016/j.injury.2017.02.021
Boufous S, Finch C, Lord S, Close J (2005) The increasing burden of pelvic fractures in older people, New South Wales, Australia. Injury 36:1323–1329. https://doi.org/10.1016/j.injury.2005.02.008
Nanninga GL, de Leur K, Panneman MJM et al (2014) Increasing rates of pelvic fractures among older adults: the Netherlands, 1986-2011. Age Ageing 43:648–653. https://doi.org/10.1093/ageing/aft212
King AB, Tosteson ANA, Wong JB, Solomon DH, Burge RT, Dawson-Hughes B (2009) Interstate variation in the burden of fragility fractures. J Bone Miner Res 24:681–692. https://doi.org/10.1359/jbmr.081226
Islam S, Liu Q, Chines A, Helzner E (2009) Trend in incidence of osteoporosis-related fractures among 40- to 69-year-old women: analysis of a large insurance claims database, 2000-2005. Menopause 16:77–83. https://doi.org/10.1097/gme.0b013e31817b816e
Parkkari J, Kannus P, Niemi S, Pasanen M, JÄrvinen M, Lüthje P, Vuori I (1996) Secular trends in osteoporotic pelvic fractures in Finland: number and incidence of fractures in 1970-1991 and prediction for the future. Calcif Tissue Int 59:79–83. https://doi.org/10.1007/s002239900090
Andrich S, Haastert B, Neuhaus E, Neidert K, Arend W, Ohmann C, Grebe J, Vogt A, Jungbluth P, Rösler G, Windolf J, Icks A (2015) Epidemiology of pelvic fractures in Germany: considerably high incidence rates among older people. PLoS One 10:e0139078. https://doi.org/10.1371/journal.pone.0139078
Andrich S, Haastert B, Neuhaus E, Neidert K, Arend W, Ohmann C, Grebe J, Vogt A, Jungbluth P, Thelen S, Windolf J, Icks A (2017) Excess mortality after pelvic fractures among older people. J Bone Miner Res 32:1789–1801. https://doi.org/10.1002/jbmr.3116
World Health Organization Global Health and Aging. https://www.who.int/ageing/publications/global_health.pdf?ua=1. Accessed 31 Jan 2020
Orsini LS, Rousculp MD, Long SR, Wang S (2005) Health care utilization and expenditures in the United States: a study of osteoporosis-related fractures. Osteoporos Int 16:359–371. https://doi.org/10.1007/s00198-004-1694-2
Ohsfeldt RL, Borisov NN, Sheer RL (2006) Fragility fracture-related direct medical costs in the first year following a nonvertebral fracture in a managed care setting. Osteoporos Int 17:252–258. https://doi.org/10.1007/s00198-005-1993-2
Pike C, Birnbaum HG, Schiller M, Sharma H, Burge R, Edgell ET (2010) Direct and indirect costs of non-vertebral fracture patients with osteoporosis in the US. Pharmacoeconomics 28:395–409. https://doi.org/10.2165/11531040-000000000-00000
Pike C, Birnbaum HG, Schiller M, Swallow E, Burge RT, Edgell ET (2011) Economic burden of privately insured non-vertebral fracture patients with osteoporosis over a 2-year period in the US. Osteoporos Int 22:47–56. https://doi.org/10.1007/s00198-010-1267-5
Kilgore ML, Morrisey MA, Becker DJ, Gary LC, Curtis JR, Saag KG, Yun H, Matthews R, Smith W, Taylor A, Arora T, Delzell E (2009) Health care expenditures associated with skeletal fractures among Medicare beneficiaries, 1999-2005. J Bone Miner Res 24:2050–2055. https://doi.org/10.1359/jbmr.090523
Bundesministerium für Justiz und Verbraucherschutz Sozialgesetzbuch (SGB) - Elftes Buch (XI) - Soziale Pflegeversicherung (Artikel 1 des Gesetzes vom 26. Mai 1994, BGBI, I S. 1014) § 15 Stufen der Pflegebedürftigkeit. https://www.gesetze-im-internet.de/sgb_11/__15.html. Accessed 31 Jan 2020
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA (2004) New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol 57:1288–1294. https://doi.org/10.1016/j.jclinepi.2004.03.012
Toson B, Harvey LA, Close JCT (2015) The ICD-10 Charlson comorbidity index predicted mortality but not resource utilization following hip fracture. J Clin Epidemiol 68:44–51. https://doi.org/10.1016/j.jclinepi.2014.09.017
Klabunde CN, Potosky AL, Legler JM, Warren JL (2000) Development of a comorbidity index using physician claims data. J Clin Epidemiol 53:1258–1267. https://doi.org/10.1016/S0895-4356(00)00256-0
Reyes C, Estrada P, Nogués X, Orozco P, Cooper C, Díez-Pérez A, Formiga F, Mácias JG, Prieto-Alhambra D (2014) The impact of common co-morbidities (as measured using the Charlson index) on hip fracture risk in elderly men: a population-based cohort study. Osteoporos Int 25:1751–1758. https://doi.org/10.1007/s00198-014-2682-9
Lix LM, Quail J, Teare G, Acan B (2011) Performance of comorbidity measures for predicting outcomes in population-based osteoporosis cohorts. Osteoporos Int 22:2633–2643. https://doi.org/10.1007/s00198-010-1516-7
Leslie WD, Metge CJ, Azimaee M, Lix LM, Finlayson GS, Morin SN, Caetano P (2011) Direct costs of fractures in Canada and trends 1996-2006: a population-based cost-of-illness analysis. J Bone Miner Res 26:2419–2429. https://doi.org/10.1002/jbmr.457
Hopkins RB, Tarride JE, Leslie WD, Metge C, Lix LM, Morin S, Finlayson G, Azimaee M, Pullenayegum E, Goeree R, Adachi JD, Papaioannou A, Thabane L (2013) Estimating the excess costs for patients with incident fractures, prevalent fractures, and nonfracture osteoporosis. Osteoporos Int 24:581–593. https://doi.org/10.1007/s00198-012-1997-7
Efron B, Tibshirani R (1993) An introduction to the bootstrap. Chapman and Hall, New York
Smith VA, Maciejewski ML, Olsen MK (2018) Modeling semicontinuous longitudinal expenditures: a practical guide. Health Serv Res 53:3125–3147. https://doi.org/10.1111/1475-6773.12815
Zou G (2004) A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–706. https://doi.org/10.1093/aje/kwh090
Barber J, Thompson S (2004) Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy 9:197–204. https://doi.org/10.1258/1355819042250249
Brown H, Prescott R (2006) Applied mixed models in medicine. In: Statistics in practice, 2nd edn. Wiley, Chichester
Acknowledgements
We would like to thank Falk Hoffmann for his helpful recommendations during data analysis and Ute Linnenkamp for her constructive comments on this manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. The project was supported by a grant of the German Federal Ministry of Education and Research (BMBF; 01GY1136).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the ethics committee of the Faculty of Medicine, Heinrich-Heine-University Düsseldorf (approval reference 3839). The survey and utilization of secondary health administration data was conducted retrospectively and in compliance with the applicable standards and legal rules on data protection. All procedures performed were in accordance with the Declaration of Helsinki and comparable ethical standards (e.g., Good Epidemiologic Practice (GEP) and Good Practice of Secondary Data Analysis (GPS)). The data were analyzed anonymously; informed patient consent is not required.
Consent to participate
Not applicable
Consent for publication
Not applicable
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Andrich, S., Haastert, B., Neuhaus, E. et al. Health care utilization and excess costs after pelvic fractures among older people in Germany. Osteoporos Int 32, 2061–2072 (2021). https://doi.org/10.1007/s00198-021-05935-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-05935-1