Abstract
Summary
Based on a population age 50+, significant excess costs relative to matched controls exist for patients with incident fractures that are similar in relative magnitude to other chronic diseases such as stroke or heart disease. Prevalent fractures also have significant excess costs that are similar in relative magnitude to asthma/chronic obstructive pulmonary disease.
Introduction
Cost of illness studies for osteoporosis that only include incident fractures may ignore the long-term cost of prevalent fractures and primary preventive care. We estimated the excess costs for patients with incident fractures, prevalent fractures, and nonfracture osteoporosis relative to matched controls.
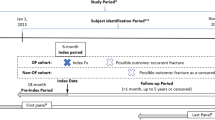
Methods
Men and women age 50+ were selected from administrative records in the province of Manitoba, Canada for the fiscal year 2007–2008. Three types of cases were identified: (1) patients with incident fractures in the current year (2007–2008), (2) patients with prevalent fractures in previous years (1995–2007), and (3) nonfracture osteoporosis patients identified by specific pharmacotherapy or low bone mineral density. Excess resource utilization and costs were estimated by subtracting control means from case means.
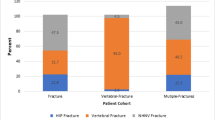
Results
Seventy-three percent of provincial population age 50+ (52 % of all men and 91 % of all women) were included (121,937 cases, 162,171 controls). There were 3,776 cases with incident fracture (1,273 men and 2,503 women), 43,406 cases with prevalent fractures (15,784 men and 27,622 women) and 74,755 nonfracture osteoporosis cases (7,705 men and 67,050 women). All incident fractures had significant excess costs. Incident hip fractures had the highest excess cost: men $44,963 (95 % CI: $38,498–51,428) and women $45,715 (95 % CI: $36,998–54,433). Prevalent fractures (other than miscellaneous or wrist fractures) also had significant excess costs. No significant excess costs existed for nonfracture osteoporosis.
Conclusion
Significant excess costs exist for patients with incident fractures and with prevalent hip, vertebral, humerus, multiple, and traumatic fractures. Ignoring prevalent fractures underestimate the true cost of osteoporosis.

Similar content being viewed by others
References
Leslie WD, Lix LM, Langsetmo L, Berger C, Goltzman D, Hanley DA, Adachi JD, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Construction of a FRAX(R) model for the assessment of fracture probability in Canada and implications for treatment. Osteoporos Int 22:817–827
Statistics Canada (2010) Estimates of population, by age group and sex for July 1, Canada, provinces and territories, annual. Table 051–0001
Becker DJ, Kilgore ML, Morrisey MA (2010) The societal burden of osteoporosis. Curr Rheumatol Rep 12:186–191
Akobundu E, Ju J, Blatt L, Mullins CD (2006) Cost-of-illness studies: a review of current methods. PharmacoEconomics 24:869–890
Strom O, Borgstrom F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, Abdon P, Ornstein E, Ceder L, Thorngren KG, Sernbo I, Jonsson B (2008) Long-term cost and effect on quality of life of osteoporosis-related fractures in Sweden. Acta Orthop 79:269–280
Leslie WD, Metge CJ, Azimaee M, Lix LM, Finlayson GS, Morin SN, Caetano P (2011) Direct costs of fractures in Canada and trends 1996–2006: a population-based cost-of-illness analysis. J Bone Miner Res 26(10):2419–2429
Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E (2001) Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int 12:271–278
Melton LJ III, Gabriel SE, Crowson CS, Tosteson AN, Johnell O, Kanis JA (2003) Cost-equivalence of different osteoporotic fractures. Osteoporos Int 14:383–388
Orsini LS, Rousculp MD, Long SR, Wang S (2005) Health care utilization and expenditures in the United States: a study of osteoporosis-related fractures. Osteoporos Int 16:359–371
Pike C, Birnbaum HG, Schiller M, Sharma H, Burge R, Edgell ET (2010) Direct and indirect costs of non-vertebral fracture patients with osteoporosis in the US. PharmacoEconomics 28:395–409
Rousculp MD, Long SR, Wang S, Schoenfeld MJ, Meadows ES (2007) Economic burden of osteoporosis-related fractures in Medicaid. Value Health 10:144–152
Goeree R, O’Reilly D, Hopkins R, Blackhouse G, Tarride JE, Xie F, Lim M (2010) General population versus disease-specific event rate and cost estimates: potential bias for economic appraisals. Expert Rev Pharmacoecon Outcomes Res 10:379–384
Knottnerus A, Tugwell P (2008) STROBE—a checklist to strengthen the reporting of observational studies in epidemiology. J Clin Epidemiol 61:323
Manitoba Centre for Health Policy (2010) University of Manitoba, Canada
WHO Collaborating Centre for Drug Statistics Methodology: Guidelines for ATC classification and DDD assignment (2010) Oslo, 2009
Kozyrskyj AL, Mustard CA (1998) Validation of an electronic, population-based prescription database. Ann Pharmacother 32:1152–1157
Poss JW, Hirdes JP, Fries BE, McKillop I, Chase M (2008) Validation of Resource Utilization Groups version III for Home Care (RUG-III/HC): evidence from a Canadian home care jurisdiction. Med Care 46:380–387
Ontario Ministry of Health and Long Term Care (2010) Long-Term Care Home Financial Policy. Ontario Ministry of Health and Long Term Care
Canadian Institute for Health Information (2010) Canadian MIS Database—hospital financial performance indicators, 1999–2000 to 2008–2009
Wiebe N, Vandermeer B, Platt RW, Klassen TP, Moher D, Barrowman NJ (2006) A systematic review identifies a lack of standardization in methods for handling missing variance data. J Clin Epidemiol 59:342–353
Briggs AH, Claxton K, Sculpher M (2006) Decision modelling for health economic evaluation. Oxford University Press, USA
Goeree R, O’Reilly D, Hux J, Lim M, Hopkins R, Tarride J, Blackhouse G, Xie F (2009) Total and excess costs of diabetes and related complications in Ontario. Can J Diabetes 33:35–45
Finlayson G, Ekuma O, Yogendran M, Burland E, Forget E (2010) The additional cost of chronic disease in Manitoba. Manitoba Centre for Health Policy, Winnipeg
Cochrane Handbook for Systematic Reviews of Interventions (2011) Version 5.1.0
StataCorp. Stata Statistical Software: Release 11 (2009)
Briggs AH, Mooney CZ, Wonderling DE (1999) Constructing confidence intervals for cost-effectiveness ratios: an evaluation of parametric and non-parametric techniques using Monte Carlo simulation. Stat Med 18:3245–3262
Willan AR, O’Brien BJ (1996) Confidence intervals for cost-effectiveness ratios: an application of Fieller’s theorem. Health Econ 5:297–305
Thompson SG, Barber JA (2000) How should cost data in pragmatic randomised trials be analysed? BMJ 320:1197–2000
Acknowledgments
The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Population Health Research Data Repository (HIPC file number 2009/2010–09). The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, or other data providers is intended or should be inferred.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Hopkins, R.B., Tarride, J.E., Leslie, W.D. et al. Estimating the excess costs for patients with incident fractures, prevalent fractures, and nonfracture osteoporosis. Osteoporos Int 24, 581–593 (2013). https://doi.org/10.1007/s00198-012-1997-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-1997-7