Abstract
Objective
This study aimed to investigate the biochemical effects of osteoarthritic infrapatellar fat pad (IPFP) on cartilage and the underlying mechanisms.
Methods
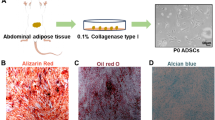
Human IPFP and articular cartilage were collected from end-stage osteoarthritis (OA) patients during total knee arthroplasty. IPFP-derived fat-conditioned medium (FCM) was used to stimulate human primary chondrocytes and cartilage explants. Functional effect of osteoarthritic IPFP was explored in human primary chondrocytes and articular cartilage in vitro and ex vivo. Activation of relative pathways and its effects on chondrocytes were assessed through immunoblotting and inhibition experiments, respectively. Neutralization test was performed to identify the main factors and their associated pathways responsible for the effects of IPFP.
Results
Osteoarthritic IPFP-derived FCM significantly induced extracellular matrix (ECM) degradation in both human primary chondrocytes and cartilage explants. Several pathways, such as NF-κB, mTORC1, p38MAPK, JNK, and ERK1/2 signaling, were significantly activated in human chondrocytes with osteoarthritic IPFP-derived FCM stimulation. Interestingly, inhibition of p38MAPK and ERK1/2 signaling pathway could alleviate the detrimental effects of FCM on chondrocytes, while inhibition of other signaling pathways had no similar results. In addition, IL-1β and TNF-α instead of IL-6 in osteoarthritic IPFP-derived FCM played key roles in cartilage degradation via activating p38MAPK rather than ERK1/2 signaling pathway.
Conclusion
Osteoarthritic IPFP induces the degradation and inflammation of cartilage via activation of p38MAPK and ERK1/2 pathways, in which IL-1β and TNF-α act as the key factors. Our study suggests that modulating the effects of IPFP on cartilage may be a promising strategy for knee OA intervention.






Similar content being viewed by others
References
Martel-Pelletier J, Barr AJ, Cicuttini FM, Conaghan PG, Cooper C, Goldring MB, et al. Osteoarthritis. Nat Rev Dis Primers. 2016;2:16072.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol (Hoboken, NJ). 2020;72:220–33.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393:1745–59.
Cao P, Li Y, Tang Y, Ding C, Hunter DJ. Pharmacotherapy for knee osteoarthritis: current and emerging therapies. Expert Opin Pharmacother. 2020;27:797–809.
Clockaerts S, Bastiaansen-Jenniskens YM, Feijt C, De Clerck L, Verhaar JA, Zuurmond AM, et al. Cytokine production by infrapatellar fat pad can be stimulated by interleukin 1beta and inhibited by peroxisome proliferator activated receptor alpha agonist. Ann Rheum Dis. 2012;71:1012–8.
Ushiyama T, Chano T, Inoue K, Matsusue Y. Cytokine production in the infrapatellar fat pad: another source of cytokines in knee synovial fluids. Ann Rheum Dis. 2003;62:108–12.
Pan F, Han W, Wang X, Liu Z, Jin X, Antony B, et al. A longitudinal study of the association between infrapatellar fat pad maximal area and changes in knee symptoms and structure in older adults. Ann Rheum Dis. 2015;74:1818–24.
Han W, Cai S, Liu Z, Jin X, Wang X, Antony B, et al. Infrapatellar fat pad in the knee: is local fat good or bad for knee osteoarthritis? Arthritis Res Ther. 2014;16:R145.
Teichtahl AJ, Wulidasari E, Brady SR, Wang Y, Wluka AE, Ding C, et al. A large infrapatellar fat pad protects against knee pain and lateral tibial cartilage volume loss. Arthritis Res Ther. 2015;17:318.
Cai J, Xu J, Wang K, Zheng S, He F, Huan S, et al. Association between infrapatellar fat pad volume and knee structural changes in patients with knee osteoarthritis. J Rheumatol. 2015;42:1878–84.
Han W, Aitken D, Zheng S, Wluka AE, Zhu Z, Blizzard L, et al. Association between quantitatively measured infrapatellar fat pad high signal-intensity alteration and magnetic resonance imaging-assessed progression of knee osteoarthritis. Arthritis Care Res (Hoboken). 2019;71:638–46.
Wang K, Ding C, Hannon MJ, Chen Z, Kwoh CK, Lynch J, et al. Signal intensity alteration within infrapatellar fat pad predicts knee replacement within 5 years: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2018;26:1345–50.
Han W, Aitken D, Zhu Z, Halliday A, Wang X, Antony B, et al. Signal intensity alteration in the infrapatellar fat pad at baseline for the prediction of knee symptoms and structure in older adults: a cohort study. Ann Rheum Dis. 2016;75:1783–8.
Han W, Aitken D, Zhu Z, Halliday A, Wang X, Antony B, et al. Hypointense signals in the infrapatellar fat pad assessed by magnetic resonance imaging are associated with knee symptoms and structure in older adults: a cohort study. Arthritis Res Ther. 2016;18:234.
Krasnokutsky S, Attur M, Palmer G, Samuels J, Abramson SB. Current concepts in the pathogenesis of osteoarthritis. Osteoarthritis Cartilage. 2008;16(Suppl 3):S1-3.
Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol. 2011;7:33–42.
Gross JB, Guillaume C, Gegout-Pottie P, Reboul P, Jouzeau JY, Mainard D, et al. The infrapatellar fat pad induces inflammatory and degradative effects in articular cells but not through leptin or adiponectin. Clin Exp Rheumatol. 2017;35:53–60.
Klein-Wieringa IR, Kloppenburg M, Bastiaansen-Jenniskens YM, Yusuf E, Kwekkeboom JC, El-Bannoudi H, et al. The infrapatellar fat pad of patients with osteoarthritis has an inflammatory phenotype. Ann Rheum Dis. 2011;70:851–7.
Rigoglou S, Papavassiliou AG. The NF-kappaB signalling pathway in osteoarthritis. Int J Biochem Cell Biol. 2013;45:2580–4.
Pal B, Endisha H, Zhang Y, Kapoor M. mTOR: a potential therapeutic target in osteoarthritis? Drugs R D. 2015;15:27–36.
Sondergaard BC, Schultz N, Madsen SH, Bay-Jensen AC, Kassem M, Karsdal MA. MAPKs are essential upstream signaling pathways in proteolytic cartilage degradation–divergence in pathways leading to aggrecanase and MMP-mediated articular cartilage degradation. Osteoarthritis Cartilage. 2010;18:279–88.
Chen WH, Lin CM, Huang CF, Hsu WC, Lee CH, Ou KL, et al. Functional recovery in osteoarthritic chondrocytes through hyaluronic acid and platelet-rich plasma-inhibited infrapatellar fat pad adipocytes. Am J Sports Med. 2016;44:2696–705.
Bastiaansen-Jenniskens YM, Clockaerts S, Feijt C, Zuurmond AM, Stojanovic-Susulic V, Bridts C, et al. Infrapatellar fat pad of patients with end-stage osteoarthritis inhibits catabolic mediators in cartilage. Ann Rheum Dis. 2012;71:288–94.
Hui W, Litherland GJ, Elias MS, Kitson GI, Cawston TE, Rowan AD, et al. Leptin produced by joint white adipose tissue induces cartilage degradation via upregulation and activation of matrix metalloproteinases. Ann Rheum Dis. 2012;71:455–62.
Chang J, Liao Z, Lu M, Meng T, Han W, Ding C. Systemic and local adipose tissue in knee osteoarthritis. Osteoarthritis Cartilage. 2018;26:864–71.
Fontanella CG, Macchi V, Carniel EL, Frigo A, Porzionato A, Picardi EEE, et al. Biomechanical behavior of Hoffa’s fat pad in healthy and osteoarthritic conditions: histological and mechanical investigations. Australas Phys Eng Sci Med. 2018;41:657–67.
Zhang H, Wang H, Zeng C, Yan B, Ouyang J, Liu X, et al. mTORC1 activation downregulates FGFR3 and PTH/PTHrP receptor in articular chondrocytes to initiate osteoarthritis. Osteoarthritis Cartilage. 2017;25:952–63.
Wang P, Mao Z, Pan Q, Lu R, Huang X, Shang X, et al. Histone deacetylase-4 and histone deacetylase-8 regulate interleukin-1beta-induced cartilage catabolic degradation through MAPK/JNK and ERK pathways. Int J Mol Med. 2018;41:2117–27.
Ge HX, Zou FM, Li Y, Liu AM, Tu M. JNK pathway in osteoarthritis: pathological and therapeutic aspects. J Recept Signal Transduct Res. 2017;37:431–6.
Fan Z, Bau B, Yang H, Aigner T. IL-1beta induction of IL-6 and LIF in normal articular human chondrocytes involves the ERK, p38 and NFkappaB signaling pathways. Cytokine. 2004;28:17–24.
Acknowledgements
We thank Prof. Lijun Lin for the help in sample collection. We also thank Wenquan Liang and Zhugui Chen for providing technical support. This work was supported by the National Natural Science Foundation of China (Grant No. 81773532, 81974342), China Postdoctoral Science Foundation (Grant No. 2021TQ0143), the Foundation of Hunan Educational Committee (Grant No. 20C1672), and Hunan Provincial Natural Science Foundation of China (Grant No. 2021JJ40518).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of Zhujiang Hospital of Southern Medical University (Guangzhou, China). This work does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Jason J. McDougall.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, Z., Tang, S., Nie, X. et al. Osteoarthritic infrapatellar fat pad aggravates cartilage degradation via activation of p38MAPK and ERK1/2 pathways. Inflamm. Res. 70, 1129–1139 (2021). https://doi.org/10.1007/s00011-021-01503-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-021-01503-9