Abstract
Nucleic acid therapeutics is a growing field aiming to treat human conditions that has gained special attention due to the successful development of mRNA vaccines against SARS-CoV-2. Another type of nucleic acid therapeutics is antisense oligonucleotides, versatile tools that can be used in multiple ways to target pre-mRNA and mRNA. While some years ago these molecules were just considered a useful research tool and a curiosity in the clinical market, this has rapidly changed. These molecules are promising strategies for personalized treatments for rare genetic diseases and they are in development for very common disorders too. In this chapter, we provide a brief description of the different mechanisms of action of these RNA therapeutic molecules, with clear examples at preclinical and clinical stages.
You have full access to this open access chapter, Download protocol PDF
Similar content being viewed by others
Key words
1 Introduction
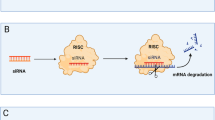
Nucleic acid therapeutics is still a growing field. With the irruption of the mRNA vaccines against SARS-CoV-2 special attention has been given to this type of therapies but other types of nucleic acid therapeutics, coined antisense oligonucleotides (AONs), have been studied for many years. Although only a dozen therapeutic oligonucleotides have been formally approved for clinical use, there are many new such drugs in the pipeline for a plethora of (mainly rare) diseases. These AON molecules interact with different nucleic acids (mRNA , non-coding RNA, and DNA) thanks to sequence specific Watson–Crick base pairing. Their mechanism of action, that may be designed to bind specific targets, makes these drugs easy to design, less likely to cause side effects and, therefore, potential candidates to lead the next wave of precision medicine. In this chapter, we describe the most frequently used AON-based therapeutic strategies, their mechanisms of action (Fig. 1), and the results of several clinical trials, with special emphasis in eye and muscle diseases.
Schematic representation of the multiple mechanisms of action of antisense oligonucleotide (AON) molecules. AONs can act at pre- and mRNA levels of the synthesis of a functional protein (left panel). They can be used to modulate splicing (upper right panel) or to degrade (pre-)mRNA (lower right panel). Splice-modulating AONs bind to pre-mRNA and promote the insertion or skipping of regular exons. In addition, they can redirect splicing when mutations in a gene lead to splicing defects (such as pseudoexon insertions). This splicing modulation causes the degradation of the transcript and a consequent reduction of protein levels. Alternatively, transcript degradation can also be achieved by using AONs binding to the pre-mRNA to disrupt the open reading frame and degrade transcripts via nonsense-mediated decay (NMD). Gapmers, in contrast, can bind to both pre-mRNA and mRNA and activate RNase-H1 RNA degradation. (Created with BioRender.com)
2 Mechanisms of Action
2.1 Splicing Modulation
The majority of existing therapeutic AONs are designed to alter the splicing pattern of specific pre-mRNAs [1]. This can be used to treat disorders caused by splicing alterations, which with the current widespread availability of better and cheaper sequencing options are being identified more easily and can be specifically targeted [2].
2.1.1 Exon Exclusion (Shortened Proteins)
In many genes, deleting an exon would result in the production of a non-functional protein, as their structure and function would be compromised. However, there are some cases in which internally “trimmed” proteins could be partially functional due to the existence of less-vital structures within a large protein. Mutations in the DMD gene disrupt the open reading frame (ORF) and the expression of the dystrophin protein, leading to Duchene muscular dystrophy (DMD). In contrast, in the much milder Becker muscular dystrophy mutations in the same gene that maintain the ORF produce an internally deleted but functional protein. This real-life example was rapidly seized as an opportunity to achieve the same effect using therapeutic AONs, and several of the recently approved AON molecules target different DMD exons [3,4,5,6,7,8,9]. Because there are many different DMD mutations, the skipping specific exons would be therapeutic for different subsets of patients.
This concept has also been employed in the development of new AONs to skip in-frame exons carrying single-nucleotide changes generating premature stop codons in large genes. Mutations in USH2A cause either Usher syndrome (deafness combined with blindness) or isolated blindness in the form of retinitis pigmentosa. Exon 13 of USH2A is prone to carry truncating variants and by deleting it, a protein with residual function is potentially produced [10, 11]. This is also the case of a stop codon introduced by a variant in exon 36 of CEP290, which is naturally skipped at low levels in the retina and involved in retinal dystrophy. AONs designed to skip exon 36 restored the reading frame and produced a functional protein able to rescue the cellular phenotype in patient-derived cells [12]. Following the same strategy, AON molecules to skip different exons of COL7A1 have been developed for dystrophic epidermolysis bullosa, a skin disease inherited in both dominant and recessive fashion [13,14,15,16].
2.1.2 Exon Inclusion
A seemingly opposite mechanism of action is at the core of nusinersen, an AON approved for the treatment of spinal muscular atrophy (SMA). In this case, mutations in the SMN1 gene cause low or lack of SMN protein production. However, SMN protein can be produced by two nearly identical genes, SMN1 and SMN2. The latter, however, contributes at very low levels due to the high rate of exon-7 skipping that disrupts the ORF. Nusinersen is used to alter the splicing of SMN2 and include exon 7, and therefore produce sufficient amounts of SMN protein to ameliorate the patient’s disease [17, 18].
2.1.3 Splicing Redirection
Variants close to the splice sites result often in either exon skipping or exon elongation. In the second scenario, mutations decrease the recognition of the original splice site and a cryptic splice site present in the intron is recognized; in the most extreme case, the entire intron is retained. Exonic variants may cause a synonymous or a predicted non-deleterious missense change at protein level, and in addition they can have a dramatic effect at RNA level by creating a novel splice site. In any case, these splicing defects are also amenable for AON intervention. For instance, a mutation in exon 3 of USH1C linked to deafness generates a novel splice donor site (SDS) upstream the regular SDS of the exon. This new SDS is preferentially used by the cells, leading to a disrupted reading frame. By using AONs to block the newly generated SDS, the normal transcript can be produced [19]. A similar approach has been used to target the exon elongation caused by near-exon intronic variants in ABCA4 linked to Stargardt macular degeneration. This study showed that by blocking the newly created SDS the normal splicing can be restored. However, this approach turned out to be not that successful when targeting exon elongations caused by variants in the splice acceptor site (SAS) [20].
Another elegant way to modulate splicing using AONs is by targeting the non-productive transcripts. These transcripts often are generated by (a) alternative splicing causing insertion or skipping of exons; (b) using alternative cryptic splice sites; and (c) retaining the introns. In any case, these splicing events lead to a disrupted ORF being the transcript degraded via nonsense-mediated decay (NMD). A very recent study has shown that 1246 potentially disease-associated genes present at least one of these non-productive transcripts. By targeting these splicing events to insert or skip an exon, exclude a retained intron, or redirect splicing when a cryptic splice site is used, the overall protein levels can be increased and this might be a promising therapeutic tool for haploinsufficiency cases [21].
2.1.4 Deep-Intronic Variants
For many years intronic variants have been ignored. This is mainly because they lay in the non-informative regions of our genome, the introns. However, the implementation of novel and more robust sequencing tools has contributed to solve the missing heritability in several diseases by discovering deep-intronic mutations with a detrimental effect on pre-mRNA splicing. The study of these variants is complex but with the help of novel bioinformatic (e.g. SpliceAI [22]) and molecular tools (mini/midi/maxi-genes [23]), it is possible to predict the effect at pre-mRNA level. These variants often result in the insertion of a pseudoexon, a piece of the intron that it is recognized as an exon and leads to a disruption of the ORF and consequently the generation of a premature stop codon. Pseudoexon exclusion can be achieved by using AONs. In the ABCA4 gene, AONs have shown splicing correction for most of the 35 intronic variants identified as cause of Stargardt disease [24,25,26,27,28,29,30].
2.2 Transcript Degradation
Antisense technology can be extremely useful to degrade transcripts and cause gene silencing (knockdown). From the therapeutic perspective, this might be a potential tool to treat autosomal dominant diseases caused by dominant-negative mutations. In this case, by degrading specifically the mutant allele, the correct protein can perform its function properly.
2.2.1 RNase H1-Activating Antisense Oligonucleotides (Gapmers)
These antisense molecules are characterized for being able to actively reduce the levels of the mRNAs in the nucleus and cytoplasm [31], therefore they are very useful to downregulate gene expression. These RNase H1-activating AONs or gapmers are chimeric molecules linked using a phosphorothioate (PS) backbone that usually present a conformation 5-10-5, where the two arms consist of five modified RNA nucleotides (2′-O-methoxyethyl (2′MOE), 2′-O-methyl (2′OMe) or locked nucleic acid (LNA)) flanking ten DNA nucleotides [32]. The first-ever AON approved by the FDA was fomivirsen, a first-generation RNase H1-activating AON [33,34,35,36] (see Subheading 3). However, this is the only RNase H1-activating AON that does not have the chimeric RNA/DNA structure. So far, four molecules using this mechanism of action have received FDA and/or EMA approval to treat different disease conditions [32].
Gapmers can be used to downregulate genes in allele-independent and allele-specific manner. Below, we review some examples of each case.
Allele-independent mRNA degradation is often used to target genes or pathways that are overexpressed in certain disease conditions or can worsen the disease progression. Thus, reducing the levels of particular genes can be very beneficial. This is the case for two of the approved AON drugs: mipomersen and volanesorsen . These molecules target the mRNA of the apolipoprotein B-100 in familial hypercholesterolemia or apolipoprotein C3 in familial chylomicronaemia syndrome, hypertriglyceridemia and familial partial lipodystrophy, respectively, to lower the levels of specific lipids increased in these diseases [37,38,39,40,41].
In contrast, allele-specific mRNA degradation aims to target only the mutant allele. This way, specific mutations that cause a dominant-negative effect can be targeted. This is the case of inotersen, a gapmer designed to target the mRNA encoding the transthyretin (TTR) protein in autosomal dominant hereditary transthyretin amyloidosis [42, 43]. A single-nucleotide change in the gene produces misfolding of the TTR protein. As TTR protein needs to tetramerize in order to conduct its function, the addition of mutant monomers into the tetramer affects the overall function. Systemic amyloid depositions are formed, leading to progressive polyneuropathy of the sensory and motor systems with multiorgan dysfunction in late-disease stages. The therapeutic gapmer targets the mutant allele to reduce the amount of tetramers containing the mutant protein, and therefore prevent the aforementioned depositions [42, 43]. Another recent example is the use of gapmers to specifically degrade the mutant allele introduced by a mutation in the COCH gene, which causes autosomal dominant hearing impairment [44]. In this study, two strategies were used to degrade the mutant transcript: directly targeting the mutation or other single-nucleotide polymorphisms (SNPs) in cis with the mutation that are part of the mutant haplotype.
2.2.2 Disrupting Reading Frame
Splice-switching AONs can also be used to induce transcript degradation. Skipping regular exons can also be used to knockdown the function of an undesired gene, by creating mRNA isoforms that encode non-functional proteins or trigger degradation of the mRNA by NMD [45]. For instance, exon skipping of hepatic APOB100 was able to sustainably reduce LDL cholesterol levels in mice [46], downregulation of MAPT gene has been proposed as a possible treatment for tauopathies [47], and skipping exon 2 of ALK5 may modulate the TGF-β signaling cascade, reducing the components related to the overproduction of extracellular matrix in hypertrophic scar [48].
3 Therapeutic Potential
While years ago oligonucleotides were considered a useful research tool and just a curiosity in the clinical market, this has rapidly changed into approved therapeutic strategies for several diseases and promising personalized treatments for many other (rare inherited) diseases. In this section, we will focus on the development of AON-based therapeutic strategies for two particular tissues: muscle and retina.
3.1 Examples of Clinical Trials for Muscle Diseases
The use of AONs to treat neuromuscular disorders has been at the forefront of the clinical development of AON-based therapies and more than half of the AONs currently in the market target either Duchenne muscular dystrophy (DMD) or spinal muscular atrophy (SMA). As previously described, AONs targeting the DMD gene aim to skip specific exons to restore the reading frame. This gene has 79 exons and patients present a large variety of mutations, mostly deletions and duplications, that require the design of specific AONs to treat a small subset to patients. The first such drug, eteplirsen, targeted exon 51 of DMD . Skipping this exon could potentially be therapeutic for 13% of DMD patients [3, 6]. Since then, golodirsen, viltolarsen, and casimersen have been approved, all applicable to decreasing percentages of patients [9, 49, 50].
All DMD exon-skipping drugs currently in the market are phosphorodiamidate morpholino oligomers (PMO). In contrast, the development of the first AON drug in clinical trials for this disorder, drisapersen (a 2′OMe/PS oligonucleotide) [51] as well as that of many others targeting DMD with the same chemistry were halted due to side effects [52]. Despite the apparent success of PMO chemistries to reach the market, these drugs are yet not very efficient, and their clinical outcomes are still poor. This is the main reason why they are yet to be approved in Europe, while in the USA and Japan have been given “accelerated approval” based on dystrophin protein expression as a surrogate endpoint, which is very low and there is debate about its clinical relevance [53]. Currently, several efforts are driven toward increasing the delivery efficacy of these drugs to the target tissue [32, 54]. Several next generation AONs targeting the same exon as eteplirsen (exon 51) have been or are being developed. This is the case of the stereopure suvodirsen, which was halted after poor results in a phase I clinical trial (NCT03907072) or the peptide-conjugated PMO currently in Phase I/II clinical trials (MOMENTUM, NCT04004065).
While AONs for DMD do not offer yet the clinical benefits that were hoped to achieve at initial stages, the journey to their development has provided very valuable lessons to stakeholders interested in developing these drugs, particularly in the context of orphan drugs [55]. A drug that benefited from some of the previous knowledge was nusinersen, a 2′MOE/PS AON targeting another neuromuscular disorder (SMA). Nusinersen was approved only months after eteplirsen and has been quickly approved worldwide due to the robust clinical data derived from the clinical trials [18, 56]. As described before, this AON is based on an exon inclusion approach to restore the expression of SMN protein in motoneurons. In this case, the target tissue is treated directly by intrathecal infusion, circumventing any delivery hurdles that may have hampered the efficacy of AONs targeting muscle or other organs when delivered systemically. Indeed, nusinersen’s delivery approach, chosen chemistry and formulation has been replicated in several n-of-1 clinical trials of other AONs targeting motoneurons, such as milasen and jacifusen (NCT04768972) [57] (see Subheading 4).
3.2 Examples of Clinical Trials for Eye Diseases
The eye is one of the most promising organs for therapeutic development. Among other characteristics, it is contained, easily accessible, and immune-privileged [58]. In fact, the first-ever FDA-approved AON (fomiversen) was a first-class oligonucleotide to treat human cytomegalovirus retinitis, an eye condition in immunocompromised patients [33,34,35,36]. Furthermore, a growing group of genes and mutations causing retinal diseases have been targeted at preclinical level using AONs. This includes pseudoexon exclusion for CEP290 [59,60,61,62,63], OPA1 [64], CHM [65] USH2A [66], and ABCA4 [24,25,26,27,28,29]; splicing modulation for USH2A [10] and CEP290 [12]; or transcript degradation for NR2E3 [67] and RHO [68]. Three of these molecules are currently in different clinical trial phases detailed below.
The most advanced molecule in a clinical setting is sepofarsen (QR-110). This is a 17-mer 2′OMe/PS oligonucleotide aiming to correct the inclusion of a pseudoexon caused by a deep-intronic mutation in CEP290-associated autosomal recessive Leber congenital amaurosis [69]. In the phase 1/2 clinical trial (NCT03140969), all patients were injected with an initial loading dose of either 320 or 160 μg followed by a maintenance dose every 3 months (160 or 80 μg) [70, 71]. Interim results showed that sepofarsen was well tolerated and safe with no serious adverse events [70, 71]. Although the final results of the trial have not yet been published, the improvement that most patients showed led to the design and approval of a phase 2/3 clinical trial (Illuminate, NCT03913143). This is a multi-center, double-masked, randomized, controlled, multiple-dose study to evaluate efficacy, safety, tolerability, and systemic exposure in patients older than 8 years carrying the specific mutation in at least one of the two alleles. Two different doses and a sham-procedure group will be assessed, for a total period of 2 years. In addition, two other clinical trials for the same molecule are ongoing. One is the extension of the phase 1/2 clinical trial to continue treating the patients of the first trial by administering sepofarsen every 3 months in both the already intervened and the contralateral eye (NCT03913130). The second is a multi-center, open-label, dose-escalation, and double-masked randomized controlled trial to evaluate safety and tolerability in children below age of 8 years old (Brighten, NCT04855045).
A multi-center phase 1/2 clinical trial to assess safety and tolerability of QR-421a (Stellar, NCT03780257) is currently ongoing. This 21-mer 2′MOE/PS oligonucleotide aims to skip the frequently mutated exon 13 of USH2A [10] causing autosomal recessive Usher syndrome or isolated retinitis pigmentosa. Preliminary results, presented in a press release seem to indicate that QR-421a is well tolerated with no serious adverse events. Furthermore, after treatment with this molecule, improvements in several measures of vision were detected. With these encouraging results, two preliminary phase 2/3 clinical trials have been designed in order to study different patient populations based on the best corrected visual acuity. Both trials will be double-masked, randomized, controlled , 24-month, and multiple-dose study (Sirius and Celeste).
The third molecule in a clinical setting is QR-1123, a gapmer designed to degrade the mutant allele (known as P23H) in the RHO gene [68], which has a dominant-negative effect leading to autosomal dominant retinitis pigmentosa. Thus, the hypothesis is that by degrading the allele carrying the mutation, the other allele will be able to produce a functional protein. This molecule is in an early stage of a multi-center open-label, double-masked, randomized, phase 1/2 trial (NCT04123626).
Other molecules for eye-related genetic diseases in late stages of preclinical development are QR-504a for TCF4-associated Fuchs endothelial corneal dystrophy and QR-411 for pseudoexon exclusion in USH2A-associated Usher syndrome or isolated retinitis pigmentosa.
As well as to target specific mutations, AONs have also been explored for multifactorial eye conditions. This is the case of primary open angle glaucoma, in which TGF-β2 was targeted with a 14-mer 3 + 3 LNA-modified gapmer in a phase I clinical trial. Results showed that the molecule was tolerated, safe and potentially clinically efficacious [72]. Besides this, other type of antisense molecules (small interference RNA, siRNA) have been clinically tested for glaucoma [73], dry eye syndrome [74], diabetic macular edema [75], and age-related macular degeneration [73, 76, 77].
4 Future of AON Trials and Personalized Medicine: n = 1 Trials?
In 2019, an AON molecule (milasen) to treat a single patient pushed the bounds of personalized medicine and raised many regulatory and ethical questions never explored before for genetic treatments [57, 78].
Milasen was customized exclusively for Mila, a child suffering from a form of Batten disease (neuronal ceroid lipofuscinosis 7) caused by the insertion of an SVA (SINE–VNTR–Alu) retrotransposon, with a detrimental effect on splicing, in the intron 6 of the MFSD8 gene [57]. Using a 22-mer 2′MOE/PS AON it was possible to redirect splicing avoiding the insertion of the SVA in the final mRNA transcript. Besides the exclusivity of this treatment, another extraordinary achievement was that it took only 13 months to go from the clinical diagnosis to the first dosing: Mila had a clinical diagnosis in mid-November of 2016, the genetic defect was identified in May 2017, approval to proceed was received in January 2018 and first patient dosing occur in the same month.
The AON delivery regime via intrathecal bolus injection was highly similar to the one of nusinersen, the AON used for SMA [17, 18, 56]. The treatment did not show any safety concerns and the frequency and duration of the seizures was reduced. Unfortunately, despite the treatment had some effect, Mila passed away early 2021. Nevertheless, this study is the hallmark of personalized medicine, and although not all diseases are amenable for this type of therapies, it has highlighted this as a possible approach and managed to re-evaluate the speed and type of safety studies and regulatory requirements. In a similar development, a drug was designed and provided to patient suffering from amyotrophic lateral sclerosis (ALS) with mutations FUS gene, following the same delivery route as nusinersen and milasen. Unfortunately, this patient, Jaci Hermstad, also died recently. However, the drug originally developed for this single patient, ION363 or jacifusen, is currently being tested in a phase III trial for patients with the same disease (NCT04768972). Thus, AON technology can be considered as a platform for individualized treatments which may, sometimes, be extended to other patients.
5 Hurdles
A drawback when compared to small molecule drugs is the relatively large size of AON molecules which limits their delivery into the cells where they exert their action. Therefore, their distribution is limited, their naked uptake is poor, and it is highly determined by the chemistry of their backbones [54]. Often, these AON molecules are not even able to reach their target organ. To circumvent this, most of these AONs rely on their conjugation or formulation with different delivery systems to be able to reach and access their intracellular targets [32]. In addition, when delivered systemically, these molecules can barely reach the central nervous system due to the blood retina and brain barriers. However, as described before, local delivery of naked modified AONs to these specific organs have shown to be efficient and safe in several clinical trials [17, 18, 56, 70, 71, 79].
Another drawback is the high exposure of certain organs upon systemic delivery of AONs. For instance, after intravenous injection of AONs a significant proportion is taken by the liver and kidney. This limits the biodistribution to other tissues and derivate on toxic effects in these organs. However, many of the liver and kidney injuries were found when using high and not clinically relevant doses of AONs [32]. In that sense, novel delivery methods or conjugates are required to be able to target the organs of interest and bypass the high clearance by the liver and kidneys.
Finding proper models to assess the sequence-dependent efficacy and safety of AONs is still a pending issue. Their safety assessment is often performed in rodents, non-human primates, and human plasma. However, these studies only provide sequence- and chemical modification-specific effects. The generation of humanized models have provided very good results, however, generating a humanized animal model for every mutation to be targeted is not feasible nor ethical. It is also possible to generate almost any human cell from patient-derived cells reprogrammed to a pluripotent stage. While these models can provide good readouts at RNA, protein, or even functional levels the entire context will still be missing. Currently, significant efforts are being made in the generation of organ-on-chips. This technology allows the combination of multiple tissues or even organs to study the interaction between them and test therapeutic interventions [80, 81]. In addition, this technology enables other type of measurements that in the near future might be very valuable to perform drug screenings and evaluate the efficacy and safety of many molecules, including AONs [80,81,82,83].
Finally, clear guidelines and novel clinical trial designs are needed to explore the full therapeutic potential of AONs when investigated as treatments for rare diseases. The case of milasen has proven that this is possible and new of such trials are being planned.
6 Conclusions
The therapeutic potential of AONs has been, for many years, subject of speculation and theoretical discussion and, while these molecules were widely applied in a research laboratory setting, their clinical application was anecdotal and limited to rare diseases. However, this landscape has recently changed completely thanks to several factors. On one hand, many of such drugs have been approved, being splice-switching AON and siRNA drugs at the forefront of this wave. Secondly, several breakthroughs in the delivery formulation of these drugs have increased the uptake of AONs targeting the liver and this has open wide open the field to consider these as reliable treatment options for several disorders where the liver is the target tissue. Thirdly, much more attention has been given to antisense technology due to the n-of-1 case of milasen. Lastly, RNA-therapies have gained extraordinary popularity due to vaccines against SAR-CoV-2 based on mRNA technology, highlighting the development of drugs based on nucleic acids. All of this will contribute to make these drugs a main resource in the therapeutic toolbox of the twenty-first century.
References
Arechavala-Gomeza V, Khoo B, Aartsma-Rus A (2014) Splicing modulation therapy in the treatment of genetic diseases. Appl Clin Genet 7:245–252. https://doi.org/10.2147/TACG.S71506
Lewandowska MA (2013) The missing puzzle piece: splicing mutations. Int J Clin Exp Pathol 6(12):2675–2682
Arechavala-Gomeza V, Graham IR, Popplewell LJ, Adams AM, Aartsma-Rus A, Kinali M, Morgan JE, van Deutekom JC, Wilton SD, Dickson G, Muntoni F (2007) Comparative analysis of antisense oligonucleotide sequences for targeted skipping of exon 51 during dystrophin pre-mRNA splicing in human muscle. Hum Gene Ther 18(9):798–810. https://doi.org/10.1089/hum.2006.061
Popplewell LJ, Adkin C, Arechavala-Gomeza V, Aartsma-Rus A, de Winter CL, Wilton SD, Morgan JE, Muntoni F, Graham IR, Dickson G (2010) Comparative analysis of antisense oligonucleotide sequences targeting exon 53 of the human DMD gene: implications for future clinical trials. Neuromuscul Disord 20(2):102–110. https://doi.org/10.1016/j.nmd.2009.10.013
Kinali M, Arechavala-Gomeza V, Feng L, Cirak S, Hunt D, Adkin C, Guglieri M, Ashton E, Abbs S, Nihoyannopoulos P, Garralda ME, Rutherford M, McCulley C, Popplewell L, Graham IR, Dickson G, Wood MJ, Wells DJ, Wilton SD, Kole R, Straub V, Bushby K, Sewry C, Morgan JE, Muntoni F (2009) Local restoration of dystrophin expression with the morpholino oligomer AVI-4658 in Duchenne muscular dystrophy: a single-blind, placebo-controlled, dose-escalation, proof-of-concept study. Lancet Neurol 8(10):918–928. https://doi.org/10.1016/S1474-4422(09)70211-X
Cirak S, Arechavala-Gomeza V, Guglieri M, Feng L, Torelli S, Anthony K, Abbs S, Garralda ME, Bourke J, Wells DJ, Dickson G, Wood MJ, Wilton SD, Straub V, Kole R, Shrewsbury SB, Sewry C, Morgan JE, Bushby K, Muntoni F (2011) Exon skipping and dystrophin restoration in patients with Duchenne muscular dystrophy after systemic phosphorodiamidate morpholino oligomer treatment: an open-label, phase 2, dose-escalation study. Lancet 378(9791):595–605. https://doi.org/10.1016/S0140-6736(11)60756-3
Anwar S, Yokota T (2020) Golodirsen for Duchenne muscular dystrophy. Drugs Today 56(8):491–504. https://doi.org/10.1358/dot.2020.56.8.3159186
Clemens PR, Rao VK, Connolly AM, Harper AD, Mah JK, Smith EC, McDonald CM, Zaidman CM, Morgenroth LP, Osaki H, Satou Y, Yamashita T, Hoffman EP, Investigators CD (2020) Safety, tolerability, and efficacy of viltolarsen in boys with Duchenne muscular dystrophy amenable to exon 53 skipping: a phase 2 randomized clinical trial. JAMA Neurol 77:1. https://doi.org/10.1001/jamaneurol.2020.1264
Shirley M (2021) Casimersen: first approval. Drugs 81:875. https://doi.org/10.1007/s40265-021-01512-2
Dulla K, Slijkerman R, van Diepen HC, Albert S, Dona M, Beumer W, Turunen JJ, Chan HL, Schulkens IA, Vorthoren L, Besten CD, Buil L, Schmidt I, Miao J, Venselaar H, Zang J, Neuhauss SCF, Peters T, Broekman S, Pennings R, Kremer H, Platenburg G, Adamson P, de Vrieze E, van Wijk E (2021) Antisense oligonucleotide-based treatment of retinitis pigmentosa caused by USH2A exon 13 mutations. Mol Ther 29:2441. https://doi.org/10.1016/j.ymthe.2021.04.024
Pendse N, Lamas V, Maeder M, Pawlyk B, Gloskowski S, Pierce EA, Chen Z-Y, Liu Q (2020) Exon 13-skipped USH2A protein retains functional integrity in mice, suggesting an exo-skipping therapeutic approach to treat USH2A-associated disease. bioRxiv. https://doi.org/10.1101/2020.02.04.934240
Barny I, Perrault I, Michel C, Goudin N, Defoort-Dhellemmes S, Ghazi I, Kaplan J, Rozet JM, Gerard X (2019) AON-mediated exon skipping to bypass protein truncation in retinal dystrophies due to the recurrent CEP290 c.4723A>T mutation. Fact or fiction? Genes (Basel) 10(5):368. https://doi.org/10.3390/genes10050368
Goto M, Sawamura D, Nishie W, Sakai K, McMillan JR, Akiyama M, Shimizu H (2006) Targeted skipping of a single exon harboring a premature termination codon mutation: implications and potential for gene correction therapy for selective dystrophic epidermolysis bullosa patients. J Investig Dermatol 126(12):2614–2620. https://doi.org/10.1038/sj.jid.5700435
Bremer J, Bornert O, Nystrom A, Gostynski A, Jonkman MF, Aartsma-Rus A, van den Akker PC, Pasmooij AM (2016) Antisense oligonucleotide-mediated exon skipping as a systemic therapeutic approach for recessive dystrophic epidermolysis bullosa. Mol Ther Nucl Acids 5(10):e379. https://doi.org/10.1038/mtna.2016.87
Ham KA, Aung-Htut MT, Fletcher S, Wilton SD (2020) Nonsequential splicing events alter antisense-mediated exon skipping outcome in COL7A1. Int J Mol Sci 21(20):7705. https://doi.org/10.3390/ijms21207705
Bornert O, Hogervorst M, Nauroy P, Bischof J, Swildens J, Athanasiou I, Tufa SF, Keene DR, Kiritsi D, Hainzl S, Murauer EM, Marinkovich MP, Platenburg G, Hausser I, Wally V, Ritsema T, Koller U, Haisma EM, Nystrom A (2021) QR-313, an antisense oligonucleotide, shows therapeutic efficacy for treatment of dominant and recessive dystrophic epidermolysis bullosa: a preclinical study. J Investig Dermatol 141(4):883–893.e886. https://doi.org/10.1016/j.jid.2020.08.018
Finkel RS, Chiriboga CA, Vajsar J, Day JW, Montes J, De Vivo DC, Yamashita M, Rigo F, Hung G, Schneider E, Norris DA, Xia S, Bennett CF, Bishop KM (2016) Treatment of infantile-onset spinal muscular atrophy with nusinersen: a phase 2, open-label, dose-escalation study. Lancet 388(10063):3017–3026. https://doi.org/10.1016/S0140-6736(16)31408-8
Finkel RS, Mercuri E, Darras BT, Connolly AM, Kuntz NL, Kirschner J, Chiriboga CA, Saito K, Servais L, Tizzano E, Topaloglu H, Tulinius M, Montes J, Glanzman AM, Bishop K, Zhong ZJ, Gheuens S, Bennett CF, Schneider E, Farwell W, De Vivo DC, Group ES (2017) Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N Engl J Med 377(18):1723–1732. https://doi.org/10.1056/NEJMoa1702752
Lentz JJ, Jodelka FM, Hinrich AJ, McCaffrey KE, Farris HE, Spalitta MJ, Bazan NG, Duelli DM, Rigo F, Hastings ML (2013) Rescue of hearing and vestibular function by antisense oligonucleotides in a mouse model of human deafness. Nat Med 19(3):345–350. https://doi.org/10.1038/nm.3106
Tomkiewicz TZ, Suárez-Herrera N, Cremers FPM, Collin RWJ, Garanto A (2021) Antisense oligonucleotide-based rescue of aberrant splicing defects caused by 15 pathogenic variants in ABCA4. Int J Mol Sci 22(9):4621
Lim KH, Han Z, Jeon HY, Kach J, Jing E, Weyn-Vanhentenryck S, Downs M, Corrionero A, Oh R, Scharner J, Venkatesh A, Ji S, Liau G, Ticho B, Nash H, Aznarez I (2020) Antisense oligonucleotide modulation of non-productive alternative splicing upregulates gene expression. Nat Commun 11(1):3501. https://doi.org/10.1038/s41467-020-17093-9
Jaganathan K, Kyriazopoulou Panagiotopoulou S, McRae JF, Darbandi SF, Knowles D, Li YI, Kosmicki JA, Arbelaez J, Cui W, Schwartz GB, Chow ED, Kanterakis E, Gao H, Kia A, Batzoglou S, Sanders SJ, Farh KK (2019) Predicting splicing from primary sequence with deep learning. Cell 176(3):535–548.e524. https://doi.org/10.1016/j.cell.2018.12.015
Sangermano R, Khan M, Cornelis SS, Richelle V, Albert S, Garanto A, Elmelik D, Qamar R, Lugtenberg D, van den Born LI, Collin RWJ, Cremers FPM (2018) ABCA4 midigenes reveal the full splice spectrum of all reported noncanonical splice site variants in Stargardt disease. Genome Res 28(1):100–110. https://doi.org/10.1101/gr.226621.117
Albert S, Garanto A, Sangermano R, Khan M, Bax NM, Hoyng CB, Zernant J, Lee W, Allikmets R, Collin RWJ, Cremers FPM (2018) Identification and rescue of splice defects caused by two neighboring deep-intronic ABCA4 mutations underlying Stargardt disease. Am J Hum Genet 102(4):517–527. https://doi.org/10.1016/j.ajhg.2018.02.008
Bauwens M, Garanto A, Sangermano R, Naessens S, Weisschuh N, De Zaeytijd J, Khan M, Sadler F, Balikova I, Van Cauwenbergh C, Rosseel T, Bauwens J, De Leeneer K, De Jaegere S, Van Laethem T, De Vries M, Carss K, Arno G, Fakin A, Webster AR, de Ravel de l’Argentiere TJL, Sznajer Y, Vuylsteke M, Kohl S, Wissinger B, Cherry T, Collin RWJ, Cremers FPM, Leroy BP, De Baere E (2019) ABCA4-associated disease as a model for missing heritability in autosomal recessive disorders: novel noncoding splice, cis-regulatory, structural, and recurrent hypomorphic variants. Genet Med 21(8):1761–1771. https://doi.org/10.1038/s41436-018-0420-y
Garanto A, Duijkers L, Tomkiewicz TZ, Collin RWJ (2019) Antisense oligonucleotide screening to optimize the rescue of the splicing defect caused by the recurrent deep-intronic ABCA4 variant c.4539+2001G>A in Stargardt disease. Genes 10(6):425. https://doi.org/10.3390/genes10060452
Sangermano R, Garanto A, Khan M, Runhart EH, Bauwens M, Bax NM, van den Born LI, Khan MI, Cornelis SS, Verheij J, Pott JR, Thiadens A, Klaver CCW, Puech B, Meunier I, Naessens S, Arno G, Fakin A, Carss KJ, Raymond FL, Webster AR, Dhaenens CM, Stohr H, Grassmann F, Weber BHF, Hoyng CB, De Baere E, Albert S, Collin RWJ, Cremers FPM (2019) Deep-intronic ABCA4 variants explain missing heritability in Stargardt disease and allow correction of splice defects by antisense oligonucleotides. Genet Med 21(8):1751–1760. https://doi.org/10.1038/s41436-018-0414-9
Khan M, Arno G, Fakin A, Parfitt DA, Dhooge PPA, Albert S, Bax NM, Duijkers L, Niblock M, Hau KL, Bloch E, Schiff ER, Piccolo D, Hogden MC, Hoyng CB, Webster AR, Cremers FPM, Cheetham ME, Garanto A, Collin RWJ (2020) Detailed phenotyping and therapeutic strategies for intronic ABCA4 variants in Stargardt disease. Mol Ther Nucl Acids 21:412–427. https://doi.org/10.1016/j.omtn.2020.06.007
Tomkiewicz TZ, Suarez-Herrera N, Cremers FPM, Collin RWJ, Garanto A (2021) Antisense oligonucleotide-based rescue of aberrant splicing defects caused by 15 pathogenic variants in ABCA4. Int J Mol Sci 22(9):4621. https://doi.org/10.3390/ijms22094621
Cremers FPM, Lee W, Collin RWJ, Allikmets R (2020) Clinical spectrum, genetic complexity and therapeutic approaches for retinal disease caused by ABCA4 mutations. Prog Retin Eye Res 79:100861. https://doi.org/10.1016/j.preteyeres.2020.100861
Liang XH, Sun H, Nichols JG, Crooke ST (2017) RNase H1-dependent antisense oligonucleotides are robustly active in directing RNA cleavage in both the cytoplasm and the nucleus. Mol Ther 25(9):2075–2092. https://doi.org/10.1016/j.ymthe.2017.06.002
Hammond SM, Aartsma-Rus A, Alves S, Borgos SE, Buijsen RAM, Collin RWJ, Covello G, Denti MA, Desviat LR, Echevarria L, Foged C, Gaina G, Garanto A, Goyenvalle AT, Guzowska M, Holodnuka I, Jones DR, Krause S, Lehto T, Montolio M, Van Roon-Mom W, Arechavala-Gomeza V (2021) Delivery of oligonucleotide-based therapeutics: challenges and opportunities. EMBO Mol Med 13(4):e13243. https://doi.org/10.15252/emmm.202013243
Crooke ST (1998) Vitravene--another piece in the mosaic. Antis Nucl Acid Drug Dev 8(4):vii–viii. https://doi.org/10.1089/oli.1.1998.8.vii
Mulamba GB, Hu A, Azad RF, Anderson KP, Coen DM (1998) Human cytomegalovirus mutant with sequence-dependent resistance to the phosphorothioate oligonucleotide fomivirsen (ISIS 2922). Antimicrob Agents Chemother 42(4):971–973. https://doi.org/10.1128/AAC.42.4.971
Roehr B (1998) Fomivirsen approved for CMV retinitis. J Int Assoc Phys AIDS Care 4(10):14–16
Jabs DA, Griffiths PD (2002) Fomivirsen for the treatment of cytomegalovirus retinitis. Am J Ophthalmol 133(4):552–556
Graham MJ, Lee RG, Bell TA III, Fu W, Mullick AE, Alexander VJ, Singleton W, Viney N, Geary R, Su J, Baker BF, Burkey J, Crooke ST, Crooke RM (2013) Antisense oligonucleotide inhibition of apolipoprotein C-III reduces plasma triglycerides in rodents, nonhuman primates, and humans. Circ Res 112(11):1479–1490. https://doi.org/10.1161/CIRCRESAHA.111.300367
Geary RS, Baker BF, Crooke ST (2015) Clinical and preclinical pharmacokinetics and pharmacodynamics of mipomersen (kynamro((R))): a second-generation antisense oligonucleotide inhibitor of apolipoprotein B. Clin Pharmacokinet 54(2):133–146. https://doi.org/10.1007/s40262-014-0224-4
Digenio A, Dunbar RL, Alexander VJ, Hompesch M, Morrow L, Lee RG, Graham MJ, Hughes SG, Yu R, Singleton W, Baker BF, Bhanot S, Crooke RM (2016) Antisense-mediated lowering of plasma apolipoprotein C-III by volanesorsen improves dyslipidemia and insulin sensitivity in type 2 diabetes. Diabetes Care 39(8):1408–1415. https://doi.org/10.2337/dc16-0126
Pechlaner R, Tsimikas S, Yin X, Willeit P, Baig F, Santer P, Oberhollenzer F, Egger G, Witztum JL, Alexander VJ, Willeit J, Kiechl S, Mayr M (2017) Very-low-density lipoprotein-associated apolipoproteins predict cardiovascular events and are lowered by inhibition of APOC-III. J Am Coll Cardiol 69(7):789–800. https://doi.org/10.1016/j.jacc.2016.11.065
Aslesh T, Yokota T (2020) Development of antisense oligonucleotide gapmers for the treatment of dyslipidemia and lipodystrophy. Methods Mol Biol 2176:69–85. https://doi.org/10.1007/978-1-0716-0771-8_5
Benson MD, Waddington-Cruz M, Berk JL, Polydefkis M, Dyck PJ, Wang AK, Plante-Bordeneuve V, Barroso FA, Merlini G, Obici L, Scheinberg M, Brannagan TH III, Litchy WJ, Whelan C, Drachman BM, Adams D, Heitner SB, Conceicao I, Schmidt HH, Vita G, Campistol JM, Gamez J, Gorevic PD, Gane E, Shah AM, Solomon SD, Monia BP, Hughes SG, Kwoh TJ, McEvoy BW, Jung SW, Baker BF, Ackermann EJ, Gertz MA, Coelho T (2018) Inotersen treatment for patients with hereditary transthyretin amyloidosis. N Engl J Med 379(1):22–31. https://doi.org/10.1056/NEJMoa1716793
Dyck PJB, Coelho T, Waddington Cruz M, Brannagan TH III, Khella S, Karam C, Berk JL, Polydefkis MJ, Kincaid JC, Wiesman JF, Litchy WJ, Mauermann ML, Ackermann EJ, Baker BF, Jung SW, Guthrie S, Pollock M, Dyck PJ (2020) Neuropathy symptom and change: inotersen treatment of hereditary transthyretin amyloidosis. Muscle Nerve 62(4):509–515. https://doi.org/10.1002/mus.27023
de Vrieze E, Canas Martin J, Peijnenborg J, Martens A, Oostrik J, van den Heuvel S, Neveling K, Pennings R, Kremer H, van Wijk E (2021) AON-based degradation of c.151C>T mutant COCH transcripts associated with dominantly inherited hearing impairment DFNA9. Mol Ther Nucl Acids 24:274–283. https://doi.org/10.1016/j.omtn.2021.02.033
Maquat LE (2004) Nonsense-mediated mRNA decay: splicing, translation and mRNP dynamics. Nat Rev Mol Cell Biol 5(2):89–99. https://doi.org/10.1038/nrm1310
Disterer P, Al-Shawi R, Ellmerich S, Waddington SN, Owen JS, Simons JP, Khoo B (2013) Exon skipping of hepatic APOB pre-mRNA with splice-switching oligonucleotides reduces LDL cholesterol in vivo. Mol Ther 21(3):602–609. https://doi.org/10.1038/mt.2012.264
Sud R, Geller ET, Schellenberg GD (2014) Antisense-mediated exon skipping decreases tau protein expression: a potential therapy for tauopathies. Mol Ther Nucl Acids 3:e180. https://doi.org/10.1038/mtna.2014.30
Raktoe RS, Rietveld MH, Out-Luiting JJ, Kruithof-de Julio M, van Zuijlen PP, van Doorn R, Ghalbzouri AE (2020) Exon skipping of TGFbetaRI affects signalling and ECM expression in hypertrophic scar-derived fibroblasts. Scars Burn Heal 6:2059513120908857. https://doi.org/10.1177/2059513120908857
Aartsma-Rus A, Corey DR (2020) The 10th oligonucleotide therapy approved: golodirsen for Duchenne muscular dystrophy. Nucl Acids Ther 30(2):67–70. https://doi.org/10.1089/nat.2020.0845
Dhillon S (2020) Viltolarsen: first approval. Drugs 80(10):1027–1031. https://doi.org/10.1007/s40265-020-01339-3
van Deutekom JC, Janson AA, Ginjaar IB, Frankhuizen WS, Aartsma-Rus A, Bremmer-Bout M, den Dunnen JT, Koop K, van der Kooi AJ, Goemans NM, de Kimpe SJ, Ekhart PF, Venneker EH, Platenburg GJ, Verschuuren JJ, van Ommen GJ (2007) Local dystrophin restoration with antisense oligonucleotide PRO051. N Engl J Med 357(26):2677–2686. https://doi.org/10.1056/NEJMoa073108
Hilhorst N, Spanoudi-Kitrimi I, Goemans N, Morren MA (2019) Injection site reactions after long-term subcutaneous delivery of drisapersen: a retrospective study. Eur J Pediatr 178(2):253–258. https://doi.org/10.1007/s00431-018-3272-1
Aartsma-Rus A, Arechavala-Gomeza V (2018) Why dystrophin quantification is key in the eteplirsen saga. Nat Rev Neurol 14(8):454–456. https://doi.org/10.1038/s41582-018-0033-8
Godfrey C, Desviat LR, Smedsrod B, Pietri-Rouxel F, Denti MA, Disterer P, Lorain S, Nogales-Gadea G, Sardone V, Anwar R, El Andaloussi S, Lehto T, Khoo B, Brolin C, van Roon-Mom WM, Goyenvalle A, Aartsma-Rus A, Arechavala-Gomeza V (2017) Delivery is key: lessons learnt from developing splice-switching antisense therapies. EMBO Mol Med 9(5):545–557. https://doi.org/10.15252/emmm.201607199
Straub V, Balabanov P, Bushby K, Ensini M, Goemans N, De Luca A, Pereda A, Hemmings R, Campion G, Kaye E, Arechavala-Gomeza V, Goyenvalle A, Niks E, Veldhuizen O, Furlong P, Stoyanova-Beninska V, Wood MJ, Johnson A, Mercuri E, Muntoni F, Sepodes B, Haas M, Vroom E, Aartsma-Rus A (2016) Stakeholder cooperation to overcome challenges in orphan medicine development: the example of Duchenne muscular dystrophy. Lancet Neurol 15(8):882–890. https://doi.org/10.1016/S1474-4422(16)30035-7
Mercuri E, Darras BT, Chiriboga CA, Day JW, Campbell C, Connolly AM, Iannaccone ST, Kirschner J, Kuntz NL, Saito K, Shieh PB, Tulinius M, Mazzone ES, Montes J, Bishop KM, Yang Q, Foster R, Gheuens S, Bennett CF, Farwell W, Schneider E, De Vivo DC, Finkel RS, Group CS (2018) Nusinersen versus sham control in later-onset spinal muscular atrophy. N Engl J Med 378(7):625–635. https://doi.org/10.1056/NEJMoa1710504
Kim J, Hu C, Moufawad El Achkar C, Black LE, Douville J, Larson A, Pendergast MK, Goldkind SF, Lee EA, Kuniholm A, Soucy A, Vaze J, Belur NR, Fredriksen K, Stojkovska I, Tsytsykova A, Armant M, DiDonato RL, Choi J, Cornelissen L, Pereira LM, Augustine EF, Genetti CA, Dies K, Barton B, Williams L, Goodlett BD, Riley BL, Pasternak A, Berry ER, Pflock KA, Chu S, Reed C, Tyndall K, Agrawal PB, Beggs AH, Grant PE, Urion DK, Snyder RO, Waisbren SE, Poduri A, Park PJ, Patterson A, Biffi A, Mazzulli JR, Bodamer O, Berde CB, Yu TW (2019) Patient-customized oligonucleotide therapy for a rare genetic disease. N Engl J Med 381(17):1644–1652. https://doi.org/10.1056/NEJMoa1813279
Vazquez-Dominguez I, Garanto A, Collin RWJ (2019) Molecular therapies for inherited retinal diseases-current standing, opportunities and challenges. Genes 10(9):654. https://doi.org/10.3390/genes10090654
Collin RW, den Hollander AI, van der Velde-Visser SD, Bennicelli J, Bennett J, Cremers FP (2012) Antisense oligonucleotide (AON)-based therapy for leber congenital amaurosis caused by a frequent mutation in CEP290. Mol Ther Nucl Acids 1:e14. https://doi.org/10.1038/mtna.2012.3
Gerard X, Perrault I, Hanein S, Silva E, Bigot K, Defoort-Delhemmes S, Rio M, Munnich A, Scherman D, Kaplan J, Kichler A, Rozet JM (2012) AON-mediated exon skipping restores ciliation in fibroblasts harboring the common leber congenital amaurosis CEP290 mutation. Mol Ther Nucl Acids 1:e29. https://doi.org/10.1038/mtna.2012.21
Garanto A, Chung DC, Duijkers L, Corral-Serrano JC, Messchaert M, Xiao R, Bennett J, Vandenberghe LH, Collin RW (2016) In vitro and in vivo rescue of aberrant splicing in CEP290-associated LCA by antisense oligonucleotide delivery. Hum Mol Genet 25(12):2552–2563. https://doi.org/10.1093/hmg/ddw118
Duijkers L, van den Born LI, Neidhardt J, Bax NM, Pierrache LHM, Klevering BJ, Collin RWJ, Garanto A (2018) Antisense oligonucleotide-based splicing correction in individuals with leber congenital amaurosis due to compound heterozygosity for the c.2991+1655A>G mutation in CEP290. Int J Mol Sci 19(3):753. https://doi.org/10.3390/ijms19030753
Dulla K, Aguila M, Lane A, Jovanovic K, Parfitt DA, Schulkens I, Chan HL, Schmidt I, Beumer W, Vorthoren L, Collin RWJ, Garanto A, Duijkers L, Brugulat-Panes A, Semo M, Vugler AA, Biasutto P, Adamson P, Cheetham ME (2018) Splice-modulating oligonucleotide QR-110 restores CEP290 mRNA and function in human c.2991+1655A>G LCA10 models. Mol Ther Nucl Acids 12:730–740. https://doi.org/10.1016/j.omtn.2018.07.010
Bonifert T, Gonzalez Menendez I, Battke F, Theurer Y, Synofzik M, Schols L, Wissinger B (2016) Antisense oligonucleotide mediated splice correction of a deep intronic mutation in OPA1. Mol Ther Nucl Acids 5(11):e390. https://doi.org/10.1038/mtna.2016.93
Garanto A, van der Velde-Visser SD, Cremers FPM, Collin RWJ (2018) Antisense oligonucleotide-based splice correction of a deep-intronic mutation in CHM underlying choroideremia. Adv Exp Med Biol 1074:83–89. https://doi.org/10.1007/978-3-319-75402-4_11
Slijkerman RW, Vache C, Dona M, Garcia-Garcia G, Claustres M, Hetterschijt L, Peters TA, Hartel BP, Pennings RJ, Millan JM, Aller E, Garanto A, Collin RW, Kremer H, Roux AF, Van Wijk E (2016) Antisense oligonucleotide-based splice correction for USH2A-associated retinal degeneration caused by a frequent deep-intronic mutation. Mol Ther Nucl Acids 5(10):e381. https://doi.org/10.1038/mtna.2016.89
Naessens S, Ruysschaert L, Lefever S, Coppieters F, De Baere E (2019) Antisense oligonucleotide-based downregulation of the G56R pathogenic variant causing NR2E3-associated autosomal dominant retinitis pigmentosa. Genes 10(5):363. https://doi.org/10.3390/genes10050363
Murray SF, Jazayeri A, Matthes MT, Yasumura D, Yang H, Peralta R, Watt A, Freier S, Hung G, Adamson PS, Guo S, Monia BP, LaVail MM, McCaleb ML (2015) Allele-specific inhibition of rhodopsin with an antisense oligonucleotide slows photoreceptor cell degeneration. Invest Ophthalmol Vis Sci 56(11):6362–6375. https://doi.org/10.1167/iovs.15-16400
den Hollander AI, Koenekoop RK, Yzer S, Lopez I, Arends ML, Voesenek KE, Zonneveld MN, Strom TM, Meitinger T, Brunner HG, Hoyng CB, van den Born LI, Rohrschneider K, Cremers FPM (2006) Mutations in the CEP290 (NPHP6) gene are a frequent cause of Leber congenital amaurosis. Am J Hum Genet 79(3):556–561. https://doi.org/10.1086/507318
Cideciyan AV, Jacobson SG, Drack AV, Ho AC, Charng J, Garafalo AV, Roman AJ, Sumaroka A, Han IC, Hochstedler MD, Pfeifer WL, Sohn EH, Taiel M, Schwartz MR, Biasutto P, Wit W, Cheetham ME, Adamson P, Rodman DM, Platenburg G, Tome MD, Balikova I, Nerinckx F, Zaeytijd J, Van Cauwenbergh C, Leroy BP, Russell SR (2019) Effect of an intravitreal antisense oligonucleotide on vision in Leber congenital amaurosis due to a photoreceptor cilium defect. Nat Med 25(2):225–228. https://doi.org/10.1038/s41591-018-0295-0
Cideciyan AV, Jacobson SG, Ho AC, Garafalo AV, Roman AJ, Sumaroka A, Krishnan AK, Swider M, Schwartz MR, Girach A (2021) Durable vision improvement after a single treatment with antisense oligonucleotide sepofarsen: a case report. Nat Med 27:785. https://doi.org/10.1038/s41591-021-01297-7
Pfeiffer N, Voykov B, Renieri G, Bell K, Richter P, Weigel M, Thieme H, Wilhelm B, Lorenz K, Feindor M, Wosikowski K, Janicot M, Packert D, Rommich R, Mala C, Fettes P, Leo E (2017) First-in-human phase I study of ISTH0036, an antisense oligonucleotide selectively targeting transforming growth factor beta 2 (TGF-beta2), in subjects with open-angle glaucoma undergoing glaucoma filtration surgery. PLoS One 12(11):e0188899. https://doi.org/10.1371/journal.pone.0188899
Moreno-Montanes J, Sadaba B, Ruz V, Gomez-Guiu A, Zarranz J, Gonzalez MV, Paneda C, Jimenez AI (2014) Phase I clinical trial of SYL040012, a small interfering RNA targeting beta-adrenergic receptor 2, for lowering intraocular pressure. Mol Ther 22(1):226–232. https://doi.org/10.1038/mt.2013.217
Benitez-Del-Castillo JM, Moreno-Montanes J, Jimenez-Alfaro I, Munoz-Negrete FJ, Turman K, Palumaa K, Sadaba B, Gonzalez MV, Ruz V, Vargas B, Paneda C, Martinez T, Bleau AM, Jimenez AI (2016) Safety and efficacy clinical trials for SYL1001, a novel short interfering RNA for the treatment of dry eye disease. Invest Ophthalmol Vis Sci 57(14):6447–6454. https://doi.org/10.1167/iovs.16-20303
Nguyen QD, Schachar RA, Nduaka CI, Sperling M, Basile AS, Klamerus KJ, Chi-Burris K, Yan E, Paggiarino DA, Rosenblatt I, Aitchison R, Erlich SS, Group DCS (2012) Dose-ranging evaluation of intravitreal siRNA PF-04523655 for diabetic macular edema (the DEGAS study). Invest Ophthalmol Vis Sci 53(12):7666–7674. https://doi.org/10.1167/iovs.12-9961
Kaiser PK, Symons RC, Shah SM, Quinlan EJ, Tabandeh H, Do DV, Reisen G, Lockridge JA, Short B, Guerciolini R, Nguyen QD, Sirna-027 Study I (2010) RNAi-based treatment for neovascular age-related macular degeneration by Sirna-027. Am J Ophthalmol 150(1):33–39.e32. https://doi.org/10.1016/j.ajo.2010.02.006
Nguyen QD, Schachar RA, Nduaka CI, Sperling M, Klamerus KJ, Chi-Burris K, Yan E, Paggiarino DA, Rosenblatt I, Aitchison R, Erlich SS, Group MCS (2012) Evaluation of the siRNA PF-04523655 versus ranibizumab for the treatment of neovascular age-related macular degeneration (MONET Study). Ophthalmology 119(9):1867–1873. https://doi.org/10.1016/j.ophtha.2012.03.043
Mullard A (2020) N-of-1 drugs push biopharma frontiers. Nat Rev Drug Discov 19(3):151–153. https://doi.org/10.1038/d41573-020-00027-x
Tabrizi SJ, Leavitt BR, Landwehrmeyer GB, Wild EJ, Saft C, Barker RA, Blair NF, Craufurd D, Priller J, Rickards H, Rosser A, Kordasiewicz HB, Czech C, Swayze EE, Norris DA, Baumann T, Gerlach I, Schobel SA, Paz E, Smith AV, Bennett CF, Lane RM, Phase 1-2a I-HSST (2019) Targeting huntingtin expression in patients with Huntington’s disease. N Engl J Med 380(24):2307–2316. https://doi.org/10.1056/NEJMoa1900907
Bhise NS, Ribas J, Manoharan V, Zhang YS, Polini A, Massa S, Dokmeci MR, Khademhosseini A (2014) Organ-on-a-chip platforms for studying drug delivery systems. J Control Release 190:82–93. https://doi.org/10.1016/j.jconrel.2014.05.004
Kimura H, Sakai Y, Fujii T (2018) Organ/body-on-a-chip based on microfluidic technology for drug discovery. Drug Metab Pharmacokinet 33(1):43–48. https://doi.org/10.1016/j.dmpk.2017.11.003
Mittal R, Woo FW, Castro CS, Cohen MA, Karanxha J, Mittal J, Chhibber T, Jhaveri VM (2019) Organ-on-chip models: implications in drug discovery and clinical applications. J Cell Physiol 234(6):8352–8380. https://doi.org/10.1002/jcp.27729
Jodat YA, Kang MG, Kiaee K, Kim GJ, Martinez AFH, Rosenkranz A, Bae H, Shin SR (2018) Human-derived organ-on-a-chip for personalized drug development. Curr Pharm Des 24(45):5471–5486. https://doi.org/10.2174/1381612825666190308150055
Acknowledgments
V.A-G holds a Miguel Servet Fellowship from the ISCIII (grants CP12/03057 and CPII17/00004), part-funded by ERDF/FEDER. V.A-G also acknowledges funding from Ikerbasque (Basque Foundation for Science). A.G. group is financially supported by the Foundation Fighting Blindness (PPA-0517-0717-RAD), the Curing Retinal Blindness Foundation as well as the Landelijke Stichting voor Blinden en Slechtzienden and Stichting Oogfonds via Uitzicht 2019-17, together with Stichting Blindenhulp, Rotterdamse Stichting Blindenbelangen and Dowilwo. The funding organizations had no role in the design or conduct of this research and provided unrestricted grants. Both authors are members of the European COST Action DARTER (CA17103).
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this protocol
Cite this protocol
Arechavala-Gomeza, V., Garanto, A. (2022). Antisense RNA Therapeutics: A Brief Overview. In: Arechavala-Gomeza, V., Garanto, A. (eds) Antisense RNA Design, Delivery, and Analysis. Methods in Molecular Biology, vol 2434. Humana, New York, NY. https://doi.org/10.1007/978-1-0716-2010-6_2
Download citation
DOI: https://doi.org/10.1007/978-1-0716-2010-6_2
Published:
Publisher Name: Humana, New York, NY
Print ISBN: 978-1-0716-2009-0
Online ISBN: 978-1-0716-2010-6
eBook Packages: Springer Protocols