Abstract
Dual-energy CT (DECT) has emerged into clinical routine as an imaging technique with unique postprocessing utilities that improve the evaluation of different body areas. The virtual non-calcium (VNCa) reconstruction algorithm has shown beneficial effects on the depiction of bone marrow pathologies such as bone marrow edema. Its main advantage is the ability to substantially increase the image contrast of structures that are usually covered with calcium mineral, such as calcified vessels or bone marrow, and to depict a large number of traumatic, inflammatory, infiltrative, and degenerative disorders affecting either the spine or the appendicular skeleton. Therefore, VNCa imaging represents another step forward for DECT to image conditions and disorders that usually require the use of more expensive and time-consuming techniques such as magnetic resonance imaging, positron emission tomography/CT, or bone scintigraphy. The aim of this review article is to explain the technical background of VNCa imaging, showcase its applicability in the different body regions, and provide an updated outlook on the clinical impact of this technique, which goes beyond the sole improvement in image quality.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Key points
-
Virtual non-calcium (VNCa) computed tomography (CT) imaging provides new relevant clinical information compared to standard CT.
-
VNCa improves CT sensitivity and specificity to assess bone marrow disorders.
-
VNCa CT may serve as an alternative to magnetic resonance imaging in case of contraindications.
Background
Since the advent of dual-energy computed tomography CT (DECT), numerous and noteworthy advantages over conventional CT have been investigated such as image optimization, artifact reduction, and the ability to provide additional information regarding tissue composition [1,2,3,4,5,6,7,8].
Among different DECT applications, virtual non-calcium (VNCa) has become an increasingly popular technique due to its ability to subtract calcium from anatomical structures, resulting in better assessment of numerous pathological conditions that might be masked on standard CT. Firstly introduced in 2009, VNCa has found its mainstream applications in removing calcified plaques from vessels and depicting cancellous bone and bone marrow changes [9,10,11,12,13].
Bone marrow edema (BME) or “bone bruise,” is considered the biomarker of injury of the skeletal system and is associated with a reduction of fat component in the trabecular bone, replaced by edema and hemorrhage. Magnetic resonance imaging (MRI) represents the reference standard technique for the assessment of bone marrow disorders [14]. DECT may be considered a potentially cheaper, faster, and comprehensive imaging alternative through the creation of VNCa reconstructions, and it is aiming to provide as detailed information as MRI for a number of clinical indications [15].
A large body of evidence has shown the potential of DECT for collagen-based tendon and ligament imaging or to differentiate hyperdense lesions from calcium, such as urate crystals in patients with gout [16,17,18,19,20]. In this setting, DECT’s ability to provide information regarding an additional imaging parameter such as BME derived from VNCa images might be particularly helpful for a multiparametric approach to inflammatory, infiltrative, and degenerative disorders as well as in an emergency setting for traumatized patients.
This article discusses and summarizes the current clinical applications of VNCa imaging including different DECT platforms, their basic principles of physics, and areas of potential development.
Basic principles of DECT
While standard single-energy CT uses a single polychromatic x-ray beam with a single peak energy of 120 kV, DECT systems allow for simultaneous image acquisition at two different voltages.
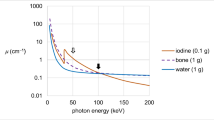
At the energy levels used in clinical routine, attenuation of biological tissues is dependent on two major interactions: Compton scattering and photoelectric effects. Compton scattering is proportional to electron density and has little energy dependence. On the other hand, the photoelectric effect is dependent on the energy of the x-ray beam (E), as well as on the atomic number (Z) of the element, and it is predominant at lower energies and near the element K-edge.
On single-energy CT platforms, the measurement of attenuation using a single x-ray spectrum does not allow for the differentiation of materials, because the attenuation coefficient is not unique. In particular, it depends either on the energy of the x-ray beam or on the concentration of a material. This means that at a given energy, a lower concentration of a higher Z material (i.e., iodine) may have the same attenuation as the higher concentration of a lower Z material (i.e., calcium). However, since materials have unique attenuation profiles at different energy levels, DECT aims to identify different elements exploiting mathematical algorithms based on their linear attenuation coefficients in order to achieve the so-called material decomposition [21,22,23].
DECT’s ability to discriminate between different materials is highly proportional to the dual-energy ratio (DEratio). Since DECT uses two different energies for measuring attenuation, DEratio is defined as the ratio of the attenuation of a given material on a low-kV dataset to the attenuation of the same material on a high-kV dataset. The energy-dependent attenuation differences of elements within a voxel allow DECT to exploit two- and three-material decomposition. The ability to differentiate the DEratio of two materials also depends on the separation between low- and high-energy spectra and the Z of the evaluated materials.
However, DECT algorithms work better when materials have high atomic numbers, because these are characterized by large differences in attenuation at different photon energies (i.e., iodine and calcium). At tube voltages used in clinical routine, it is possible to generate virtual unenhanced images by subtraction of iodine from contrast-enhanced DECT examinations or VNCa series by subtraction of calcium [5, 15, 20, 24, 25].
Different vendors offer diverse DECT technologies:
-
1)
Dual-source CT (DSCT) platforms, consisting of two x-ray tubes that generate two beams at different voltages installed at about 90° from each other, which have the advantage of high temporal resolution; although two x-ray sources are involved, the radiation dose administered to the patient is usually divided between the two, resulting in dose neutrality of second- and third-generation DSCT scanners compared with conventional CT [25, 26];
-
2)
Single-source with sequential acquisition CT platforms, which consist of two scans acquired consecutively at different tube potentials followed by co-registration for post-processing, offering the advantage of a full field of view and the drawback of poor temporal resolution as the patient is scanned twice, with an increase of radiation dose;
-
3)
Single-source twin-beam platforms, in which a two-material filter splits the x-ray beam into high- and low-energy spectra on the z-axis before it reaches the patient;
-
4)
Single-source tube voltage switching CT platforms, in which the x-ray tube alternates high and low potentials several times within the same rotation, which have the advantage of a full field of view;
-
5)
Dual-layer detector CT platforms, which involve a superficial and a deep layer within the same detector plate that simultaneously collect low-energy data by the superficial layer, and high-energy data by the deep layer.
However, most of the current experience with VNCa algorithms published in scientific literature has been performed on second- and third-generation DSCT platforms (Tables 1, 2, 3, and 4), which may be explained with wider availability of this particular DECT technology compared to the other ones.
Technical background of VNCa CT imaging
Due to three-material decomposition, the VNCa algorithm estimates the amount of calcium on the DECT dataset and subtracts it from images to highlight the anatomical structures that can be covered with bone mineral or gross calcifications.
On VNCa imaging, the bone marrow attenuation represents CT values of yellow and red marrow. In particular, using the characteristic slope of the DEratio of calcium, bone mineral voxels are projected to the CT value of water (0 HU for both 100 kV and Sn140 kV) [27, 28]. As a consequence, the differences among voxels reflect mainly the water and fat content in the bone marrow. These differences can be visually interpreted, using color-coded maps, or quantitatively assessed by means of regions of interest and expressed in HU [22, 29,30,31].
However, most of the cutoff values that have been suggested to differentiate BME from normal bone marrow are still quite heterogeneous, and range between -80 and 6 HU. These differences might depend either on the anatomical region evaluated or on the type of DECT platform used.
Image quality on VNCa datasets is also influenced by DECT scanning parameters. The use of higher spectral separation allows for a precise assessment of bone mineral content [32]. Best results have been obtained with a DEratio of 70/150 kV. However, when a wide DEratio may not be recommended because of the increase in image noise, such as scanning the abdomen and pelvis, higher radiation doses help provide optimal image quality [31]. Pitch and rotation time do not considerably affect image quality, although spiral artifacts can appear when the pitch is too low.
Color-coded VNCa datasets are usually automatically processed from raw data of most modern DECT platforms, with processing time lasting few minutes, and showing the potential to be used in routine clinical practice [33, 34]. Slice thickness of 1–2 mm and smoother reconstruction kernels are recommended and datasets should be reformatted along two anatomical planes for optimal qualitative evaluation [35].
Technical limitations of VNCa imaging should also be taken into account. In fact, it has been demonstrated the inability to accurately visualize minor alterations in marrow attenuation directly adjacent to cortical bone due to incomplete masking of the cortex and to spatial averaging. Incomplete subtraction of cortical or cancellous bone might also occur in the case of arthrosis, and in the presence of gas or severe osteosclerosis, which causes beam hardening artifacts that may result in a lack of visible edema even in the presence of a fracture. For this reason, any potential user of VNCa imaging should be aware of its potential pitfalls [36, 37].
VNCa clinical applications
Head
Intracranial calcifications are common findings on head CT scans [38]. They are often caused by dystrophic processes within the choroid plexus and basal ganglia or might occur as part of different disorders, such as tuberous sclerosis, cysticercosis, Sturge-Weber syndrome, and slowly growing brain tumors (i.e., meningiomas, dermoids, craniopharyngiomas, and oligodendrogliomas) [39].
In an emergency setting, any focal source of intracranial hyperattenuation might confound diagnosis, especially if intracranial hemorrhage needs to be excluded. In a conventional CT scan of the head, any lesion with attenuation levels greater than 100 HU is classified as a calcification [40]. However, fresh blood usually has a density of 50–65 HU whereas attenuation of calcifications can vary between 70 and 200 HU [41]. Hence, this standard criterion may fail for lesions with attenuation levels inferior to 100 HU, where values tend to overlap.
Currently, the proposed imaging techniques for differentiating hemorrhage from calcification include MRI-based techniques such as quantitative susceptibility mapping and gradient-echo imaging [40].
VNCa has been shown to accurately differentiate between calcification and hemorrhage, even in lesions with attenuation comprised between 50 and 100 HU (Fig. 1) [18]. In clinical studies, VNCa with a cutoff of 44 HU has shown high diagnostic performance for differentiation of small foci of intracranial hemorrhage from calcium (Table 1) [17, 19].
Head dual-energy computed tomography scan shows a focal hyperattenuation in the pons classified as indeterminate at standard grayscale series (a). This 80-year-old patient with a history of hypertension presented to the emergency department with altered mental status. On the calcium-overlay image (b), the hyperattenuation focus remains visible, while it is not apparent on the virtual non-calcium image (c), suggestive for parenchymal calcification. The finding was confirmed by magnetic resonance imaging. From Hu et al. [17]
Spine
Fractures
MRI and CT are currently considered the diagnostic imaging modalities of choice to evaluate spine disorders [42]. CT imaging is indicated in emergency trauma settings to detect hypodense fracture lines due to its excellent spatial resolution [42, 43]. On the other hand, MRI is the reference standard technique for the evaluation of nerves, musculotendinous structures, and bone marrow disorders. Moreover, MRI is particularly useful to diagnose BME secondary to trauma, which allows establishing the chronicity of a fracture by the presence of interstitial fluid [44,45,46]. However, MRI access can be limited in routine trauma settings due to its high costs and long acquisition times, which require prolonged and potentially painful patient positioning [32, 46,47,48].
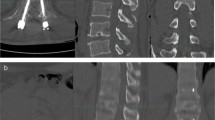
While single-energy CT is not able to remove bone trabeculations and to uncover subtle bone marrow attenuation changes, DECT allows for BME assessment [20, 49,50,51,52,53,54,55]. Moreover, its rapid acquisition time lends it favorably to emergency settings [46]. Several studies have been carried out to evaluate the diagnostic performance of VNCa reconstructions to detect acute vertebral fractures [56,57,58]. BME detection has been qualitatively assessed by using color-coded images and quantitatively using region-of-interest-based measurements of bone marrow attenuation. When microfractures are present within the cancellous bone, bone marrow attenuation increases since its fatty content is replaced by edema and microhemorrhages. Color-coded VNCa reconstructions show good to excellent results for qualitative assessment of BME, either in terms of sensitivity (range 72–96%), specificity (range 70–100%), and accuracy (range: 90–99%) (Table 2).
Similarly, receiver operating characteristic curve analysis of bone marrow attenuation on VNCa datasets has also demonstrated excellent sensitivity, specificity, and accuracy, ranging 85–96%, 82–90%, and 85–91%, respectively, using cutoff values from -80 and -12 HU [46, 56,57,58].
Interesting results have also been obtained for the diagnosis of sacral insufficiency fractures (Fig. 2), showing high sensitivity and specificity (93% and 95%, respectively) for qualitative assessment, and values of 85% and 95% for quantitative assessment using a cutoff value of -43 HU [29]. This may allow DECT to act as a promising technique to avoid misinterpretation of insufficiency fractures and their related complications, particularly in patients suffering from osteoporosis or diffuse bone disease [59].
Head dual-energy computed tomography scan shows focal hyperattenuation in the pons, classified as indeterminate at standard grayscale series (a). This 58-year-old patient had a history of hypertension and diabetes and presented to the emergency department with right arm tremor, blurry vision, and increased systolic blood pressure. On the calcium-overlay image, the focal hyperattenuation in the pons was not apparent (b). On the virtual non-calcium image (c), the focal hyperattenuation in the pons manifests as a focal area of high attenuation, compatible with hemorrhage. From Hu et al. [17]
Degenerative disc disease
Degenerative disease of intervertebral disc apparatus is a common age-related condition, causing lower back pain and entailing substantial social and economic burden [34].
Common complications are compressions of the spinal cord or spinal nerve root. Fast and accurate diagnosis is necessary for rapid initiation of optimal therapy and to avoid compressions that can result in irreversible morbidity. MRI is the preferred diagnostic imaging modality due to its ability to provide excellent demarcation between the intervertebral disc and cerebrospinal fluid [60]. However, MRI has several limitations in clinical routine, such as patients with ferromagnetic metallic implants, claustrophobia, or difficulties in staying supine and still for long acquisition times.
DECT imaging has been introduced as an attractive alternative, especially due to VNCa imaging, which achieved promising results for the identification of early stages of intervertebral disc degeneration. Using a maximum CT value of 800 HU and a threshold of -200 HU, VNCa color-coded maps with mixed CT overlay have demonstrated the ability to detect different grades of the modified Pfirrmann classification, which is widely used for disc degeneration grading [61]. In particular, VNCa imaging is able to detect an increase in disc attenuation that positively correlates to dehydration of nucleus pulposus and in a loss of its proteoglycan and water content.
More advanced stages of intervertebral disc degeneration are characterized by disc height reduction, fissuration of the annulus fibrosus, and herniation of the nucleus polposus. Standard CT has shown moderate sensitivity and specificity for the detection of lumbar disk herniation, despite the improved results coming from new iterative reconstruction algorithms [34, 62, 63]. More recently, DECT has overcome the impaired contrast resolution of intervertebral discs by application of color-coded VNCa reconstructions (Fig. 3).
Spine dual-energy computed tomography. Standard grayscale series (a) shows typical findings of spondylarthrosis with vacuum phenomena in L3/L4 and L4/L5 intervertebral discs. Virtual non-calcium reconstruction with optimization for intervertebral disc analysis (b) can finely show the protrusion of lumbar discs (arrows), confirmed by magnetic resonance imaging T2-weighted sequence (c) (arrows). From Booz et al. [34]
Color-coded maps help distinguish small disc herniations from cerebrospinal fluid, with better sensitivity and specificity compared to standard CT, respectively of 91% and 92%, using MRI as a reference standard (Table 3) [34].
Infiltrative disease
The spine represents the most common site of bone metastases. Only breast, prostate and lung cancers are together responsible for more than 80% of cases of metastatic bone disease [64].
A contrast-enhanced CT scan is typically performed in oncologic patients either for staging and follow-up purposes [56]. However, despite iodine-based contrast agents helping enhance soft tissue contrast, the assessment of bone lesions on standard CT remains challenging. In a meta-analysis, conventional CT images reported a sensitivity and specificity of 77% and 83% for detection of spine metastasis [65]. Moreover, patients may need to undergo additional imaging techniques, such as MRI, scintigraphy, or positron emission tomography when there is high suspicion for bone metastasis presence [56].
The efficacy of VNCa reconstructions to detect metastatic spine lesions has been recently assessed with different calcium suppression indices. In particular, the use of low- and medium-suppression indices resulted in an increase in sensitivity to 85%, compared to 78% of conventional CT, and it was associated with a good inter-reader agreement at subjective image analysis [56].
In a study from Abdullayev et al. [56], quantitative analysis using low- and medium-suppression indices showed promising results to discriminate between normal and metastatic bone, using a cutoff of -143 HU and -31 HU, respectively (Table 3).
The role of DECT in infiltrative spine disorders has also been focused on patients with multiple myeloma. In this malignant hematological tumor, the unbridled clonal proliferation of plasma cells causes an alteration of the normal components of bone marrow [66]. Low-dose total body CT scans are usually performed to detect osteolytic lesions [66]. In this setting, DECT has shown promising results, with better sensitivity compared to standard CT (Fig. 4).
Hand dual-energy computed tomography scan in a patient with a non-displaced scaphoid fracture, which was confirmed at magnetic resonance imaging (not shown). Standard grayscale series (a) shows a subtle cortical interruption, which is not clearly suggestive for fracture (arrow). Color-coded virtual non-calcium image (b) depicts the presence of bone marrow edema confirming the hypothesis of a traumatic lesion. Of note, the epiphyseal line on the distal radius and ulna are also color-coded in green (arrowhead). From Dareez et al. [84]
Different studies have proposed threshold values ranging between -45 HU and -36 HU to achieve optimal sensitivity by quantitative assessment and to allow fine depiction either of focal and diffuse patterns of disease, with accuracy ranging from 93 to 99% [12, 66, 67].
Appendicular skeleton
Hip
VNCa reconstructions are particularly helpful to detect subtle hip fractures that might be missed on conventional radiographs or standard CT, especially in patients affected by diffuse skeletal disorders such as osteoporosis or Paget’s disease [36].
Prompt identification of pelvic fractures is crucial for therapeutical planning and misdiagnosis is related to disability and higher mortality rates, with complications such as avascular necrosis and thromboembolism [68]. Different authors focused on the diagnostic performance of VNCa reconstructions to detect pelvic fractures, using clinical follow-up as a reference standard (Table 3). In these studies, DECT performed significantly better than standard CT, showing an improvement of sensitivity (> 5%) when color-coded VNCa images were evaluated [37, 69]. Moreover, quantitative analysis with a cutoff of -55.3 HU yielded sensitivity and specificity of 100% and 94%, respectively [36].
Different conditions such as axial spondylarthritis and sacroiliitis, involving either the spine or the pelvic girdle, usually require patients to undergo MRI. The VNCa algorithm has also been investigated for inflammatory changes of the bone marrow (Table 3), with results showing good diagnostic performance to highlight BME caused by active inflammation [70,71,72,73,74]. Promising results have also been shown for infiltrative lesions, and VNCa has been used as a guide for biopsy of malignant pelvic neoplasms that are barely visible on standard CT because of isodense bone marrow [75].
Limbs
A recent meta-analysis [76] compared the diagnostic performance of CT and MRI to establish a definitive diagnosis of a suspected fracture in small bones. MRI yielded superior sensitivity and specificity compared to CT (respectively 88% and 100% versus 72% and 99%), using bone scintigraphy as a reference standard. In case of suspected or subtle fractures, MRI is considered the best advanced imaging option after conventional radiography, as it finely depicts bone marrow and adjacent soft tissues. On the other hand, MRI alone may not depict fracture lines in case of intense BME, and conventional radiographs or CT may be needed for diagnosis [77]. Additionally, high cost, low access, and contraindications prevent MRI from playing a role as an advanced imaging option for suspected and occult fractures in emergency settings [76, 78]. However, bone bruise is considered the key finding of bone injury at MRI, as it allows uncovering subtle fractures even in small bones that might be occult at conventional radiography and standard CT [79].
An increasing number of studies have shown the feasibility of DECT to detect traumatic BME in small bones of appendicular skeleton exploiting VNCa imaging (Table 4), with improved diagnostic performance compared to standard CT either for qualitative and quantitative evaluation [80,81,82,83].
DECT can complement the information provided by standard CT imaging and enhance the diagnostic capabilities of VNCa for the evaluation of acute knee fractures (Fig. 5). In a study by Booz et al. [82], qualitative assessment of knee fractures by color-coded VNCa images yielded sensitivity and specificity of 95%, while at quantitative analysis, these values were 96% and 97%, respectively, using a -51 HU cutoff. Similar results have been shown by Wang et al. [80], who proposed a cutoff of -67 HU, yielding a sensitivity of 81% and specificity of 99%. Compared with standard CT, DECT has demonstrated a 15–20% increase in sensitivity to detect fractures, especially for less experienced radiologists [81]. The VNCa algorithm has been shown to perform well even with a low radiation-dose protocol, with excellent agreement with standard-dose DECT [48]. Bipartite patella and osteoarthritis can represent a pitfall of the VNCa algorithm, since they may determine false positives and negatives [81]. An additional limitation represents also the presence of prostheses or osteosynthesis implants [81].
Dual-energy computed tomography scan in a patient presenting with right-sided acute ankle trauma. Standard grayscale series (a) does not depict any fracture line. Color-coded virtual non-calcium image (b) shows a distinct traumatic bone marrow edema of the right calcaneus, displayed as a green area (arrow). The finding was confirmed by magnetic resonance imaging (c) using a proton density-weighted sequence (arrow)
Several authors have investigated the performance of VNCa reconstructions to detect traumatic BME in small bones of distal joints, such as the scaphoid [47, 84,85,86,87,88]. In these studies, DECT was able to highlight traumatic BME with higher sensitivity and specificity than standard CT either for qualitative assessment and quantitative analysis (Table 4) [85]. Some case reports also highlighted the ability of DECT to depict Achilles tendon tears with improved confidence over conventional CT [89]. Similar outcomes have been reported for evaluation of cruciate ligament rupture in acute knee trauma, with rather good sensitivity (79%) and excellent specificity (100%), using MRI as a reference standard [16].
VNCa imaging performs well on small bones also to depict inflammatory BME, related to rheumatoid arthritis, in either large or small joints (Fig. 6), showing good qualitative assessment and excellent agreement with MRI [72].
Dual-energy computed tomography scan of hands in a patient with rheumatoid arthritis. Magnification on the second metacarpophalangeal joint shows a normal and smooth outline of cartilage and bone plate (short arrows) on standard grayscale series (a) and normal virtual non-calcium attenuation (b). Conversely, bone marrow edema is evident on the third metacarpophalangeal joint presenting as an extensive and ill-defined green area (long arrows). Magnetic resonance imaging by means of T2-weighted fat-saturation sequence confirmed the presence of inflammatory bone marrow edema (c). From Jans et al. [72]
Vascular applications
Sufficient removal of calcified plaques from vessels represents a current challenge for CT angiography (CTA) studies. Calcified plaques commonly cause overestimation of vascular stenosis assessment, especially in small vessels, and may lead to unnecessary invasive procedures [90].
Usually, a fixed HU value is used as a threshold to remove calcifications in conventional CTA, despite this method often failing due to calcium blooming. Alternatively, unenhanced CT acquisition can serve as a mask for subtraction of calcified plaques. However, misregistration artifacts may occur due to patient’s movements or arterial pulsations between the two scans [13, 91]. DECT algorithms are well known to improve image quality, to reduce the contrast medium volume and the radiation dose to patients undergoing CTA studies [6, 13, 92,93,94]. DECT-based three-material decomposition also allows for subtraction of the calcium signal from iodinated vessels, permitting the removal of hard plaques from a CTA scan [95].
In this context, VNCa imaging has been shown to improve the quantification of carotid artery stenoses caused by hard plaques compared to conventional CTA, using digital subtraction angiography as reference [95]. Moreover, lumen assessment did not show to be impacted by blooming artifacts, probably because the algorithm recognizes and removes the spectral behavior of calcium blooming components [95].
Future outlook
Energy-integrating detectors used in modern DECT platforms are based on an indirect process of x-ray conversion into an electrical signal, which passes by photodiodes and conversion into light photons [96]. On the other hand, new photon-counting detectors directly convert x-ray photons to an electrical signal, increasing dose efficiency and spatial resolution, and improving spectral separation together with its spatial registration. In the near future, photon-counting detector CT platforms may enable not only to visualize BME more in detail, especially in small bones, but also to differentiate among urate crystals, hydroxyapatite, and calcium pyrophosphate deposits [97]. Moreover, preliminary data have shown promising results for subtraction of calcified plaques from vessels, and separation between blood and brain calcifications, overcoming current VNCa limitations of suboptimal material decomposition and resolution restrictions of DECT platforms [98, 99].
However, we are still at the doorstep of this new era of CT technology and further investigation needs to be performed prior to introduction of photon-counting detector CT platforms into clinical routine.
Conclusions
In the last ten years, DECT-based VNCa imaging has been shown to provide additional clinically relevant information compared to standard CT in several neuroradiology, vascular, and musculoskeletal applications. The greatest experience in using VNCa reconstructions exists in bone marrow imaging to date, particularly for trauma, but also for inflammatory and oncologic bone marrow pathologies. Several studies have demonstrated its potential also for the differentiation of hyperdense lesions as well as for intervertebral disc assessment. In addition, inflammatory or infiltrative bone marrow disorders that are conventionally assessed by means of MRI or bone scintigraphy can be assessed in more detail with DECT in comparison to standard CT. Subjective as well as objective analysis of VNCa images has shown high diagnostic accuracy and demonstrated its potential to serve as a viable imaging alternative to MRI, bone scintigraphy, or PET/CT in case of contraindications or limited availability. Especially in emergency/trauma settings, patients can substantially benefit from this technique due to time savings, early accurate diagnosis, and prompt therapy initiation. However, despite multiple studies having shown the potential of DECT-based VNCa imaging, this technique still has not gained ground in clinical routine, probably because of its limited availability considering that most of available studies have been performed on second- and third-generation DSCT platforms. This might have limited inter-vendor correlation studies and hampered the integration of VNCa imaging into clinical routine.
It is crucial to be aware of VNCa technical limitations and differences related to acquisition protocols and reconstruction software, which may differ across vendors, and generate different cutoff values for quantitative assessment. Further investigation of VNCa imaging algorithms is needed to gain a more comprehensive understanding of its potential.
Availability of data and materials
Not applicable
Abbreviations
- BME:
-
Bone marrow edema
- CTA:
-
Computed tomography angiography
- DECT:
-
Dual-energy computed tomography
- DEratio :
-
Dual-energy ratio
- DSCT:
-
Dual-source computed tomography
- MRI:
-
Magnetic resonance imaging
- HU:
-
Hounsfield units
- PET:
-
Positron emission tomography
- VNCa:
-
Virtual non-calcium
References
D’Angelo T, Cicero G, Mazziotti S et al (2019) Dual energy computed tomography virtual monoenergetic imaging: technique and clinical applications. Br J Radiol 92:20180546 https://doi.org/10.1259/bjr.20180546
Lenga L, Lange M, Arendt CT et al (2020) Measurement eeliability and diagnostic accuracy of virtual monoenergetic dual-energy CT in patients with colorectal liver metastases. Acad Radiol 27:e168–e175 https://doi.org/10.1016/j.acra.2019.09.020
Lenga L, Czwikla R, Wichmann JL et al (2018) Dual-energy CT in patients with abdominal malignant lymphoma: impact of noise-optimised virtual monoenergetic imaging on objective and subjective image quality. Clin Radiol 73:833.e19-833.e27. https://doi.org/10.1016/j.crad.2018.04.015.
D'Angelo T, Mazziotti S, Ascenti G, Wichmann JL (2017) Miscellaneous and emerging applications of dual-energy computed tomography for the evaluation of pathologies in the head and neck. Neuroimaging Clin N Am 27:469–482 https://doi.org/10.1016/j.nic.2017.04.008
Lenga L, Trapp F, Albrecht MH et al (2019) Single- and dual-energy CT pulmonary angiography using second- and third-generation dual-source CT systems: comparison of radiation dose and image quality. Eur Radiol 29:4603–4612 https://doi.org/10.1007/s00330-018-5982-1
Arendt CT, Czwikla R, Lenga L et al (2020) Improved coronary artery contrast enhancement using noise-optimised virtual monoenergetic imaging from dual-source dual-energy computed tomography. Eur J Radiol 122:108666 https://doi.org/10.1016/j.ejrad.2019.108666
Martin SS, Trapp F, Wichmann JL et al (2019) Dual-energy CT in early acute pancreatitis: improved detection using iodine quantification. Eur Radiol 29:2226–2232 https://doi.org/10.1007/s00330-018-5844-x
Lenga L, Albrecht MH, Othman AE et al (2017) Monoenergetic dual-energy computed tomographic imaging: cardiothoracic applications. J Thorac Imaging 32:151–158 https://doi.org/10.1097/RTI.0000000000000259
Akisato K, Nishihara R, Okazaki H et al (2020) Dual-energy CT of material decomposition analysis for detection with bone marrow edema in patients with vertebral compression fractures. Acad Radiol 27:227–232 https://doi.org/10.1016/j.acra.2019.02.015
Bierry G, Venkatasamy A, Kremer S, Dosch JC, Dietemann JL (2014) Dual-energy CT in vertebral compression fractures: performance of visual and quantitative analysis for bone marrow edema demonstration with comparison to MRI. Skelet Radiol 43:485–492 https://doi.org/10.1007/s00256-013-1812-3
Burns JE, Yao J, Summers RM (2017) Vertebral body compression fractures and bone density: automated detection and classification on CT images. Radiology 284:788–797 https://doi.org/10.1148/radiol.2017162100
Kosmala A, Weng AM, Heidemeier A et al (2018) Multiple myeloma and dual-energy CT: diagnostic accuracy of virtual noncalcium technique for detection of bone marrow infiltration of the spine and pelvis. Radiology 286:205–213 https://doi.org/10.1148/radiol.2017170281
Uotani K, Watanabe Y, Higashi M et al (2009) Dual-energy CT head bone and hard plaque removal for quantification of calcified carotid stenosis: utility and comparison with digital subtraction angiography. Eur Radiol 19:2060–2065 https://doi.org/10.1007/s00330-009-1358-x
Boks SS, Vroegindeweij D, Koes BW, Hunink MGM, Bierma-Zeinstra SMA (2006) Follow-up of occult bone lesions detected at MR imaging: systematic review. Radiology 238:853–862 https://doi.org/10.1148/radiol.2382050062
Omoumi P, Becce F, Racine D, Ott JG, Andreisek G, Verdun FR (2015) Dual-energy CT: basic principles, technical approaches and applications in musculoskeletal imaging. Semin Musculoskelet Radiol 19:431–437 https://doi.org/10.1055/s-0035-1569253
Peltola EK, Koskinen SK (2015) Dual-energy computed tomography of cruciate ligament injuries in acute knee trauma. Skeletal Radiol 44:1295–1301 https://doi.org/10.1007/s00256-015-2173-x
Hu R, Daftari Besheli L, Young J et al (2016) Dual-energy head CT enables accurate distinction of intraparenchymal hemorrhage from calcification in emergency department patients. Radiology 280:177–183 https://doi.org/10.1148/radiol.2015150877
Nute JL, Le Roux L, Chandler AG, Baladandayuthapani V, Schellingerhout D, Cody DD (2015) Differentiation of low-attenuation intracranial hemorrhage and calcification using dual-energy computed tomography in a phantom system. Invest Radiol 50:9–16 https://doi.org/10.1097/RLI.0000000000000089
Wiggins WF, Potter CA, Sodickson AD (2020) Dual-energy CT to differentiate small foci of intracranial hemorrhage from calcium. Radiology 294:129–138 https://doi.org/10.1148/radiol.2019190792
Johnson TRC, Krauß B, Sedlmair M et al (2007) Material differentiation by dual energy CT: initial experience. Eur Radiol 17:1510–1517 https://doi.org/10.1007/s00330-006-0517-6
Booz C, Hofmann PC, Sedlmair M et al (2017) Evaluation of bone mineral density of the lumbar spine using a novel phantomless dual-energy CT post-processing algorithm in comparison with dual-energy X-ray absorptiometry. Eur Radiol Exp 1 https://doi.org/10.1186/s41747-017-0017-2
Primak AN, Ramirez Giraldo JC, Liu X, Yu L, McCollough CH (2009) Improved dual-energy material discrimination for dual-source CT by means of additional spectral filtration. Med Phys 36:1359–1369 https://doi.org/10.1118/1.3083567
Liu X, Yu L, Primak AN, McCollough CH (2009) Quantitative imaging of element composition and mass fraction using dual-energy CT: three-material decomposition. Med Phys 36:1602–1609 https://doi.org/10.1118/1.3097632
Albrecht M, Vogl T, Martin S et al (2019) Review of clinical applications for virtual monoenergetic dual-energy CT. Radiology 293:182297 https://doi.org/10.1148/radiol.2019182297
Lenga L, Leithner D, Peterke JL et al (2019) Comparison of radiation dose and image quality of contrast-enhanced dual-source CT of the chest: single- versus dual-energy and second-versus third-generation technology. AJR Am J Roentgenol 212:741–747 https://doi.org/10.2214/AJR.18.20065
Uhrig M, Simons D, Kachelrieß M, Pisana F, Kuchenbecker S, Schlemmer HP (2016) Advanced abdominal imaging with dual energy CT is feasible without increasing radiation dose. Cancer Imaging 16:15 https://doi.org/10.1186/s40644-016-0073-5
Wang CK, Tsai JM, Chuang MT, Wang MT, Huang KY, Lin RM (2013) Bone marrow edema in vertebral compression fractures: detection with dual-energy CT. Radiology 269:525–533 https://doi.org/10.1148/radiol.13122577
Noguchi K, Itoh T, Naruto N, Takashima S, Tanaka K, Kuroda S (2017) A novel imaging technique (X-Map) to identify acute ischemic lesions using noncontrast dual-energy computed tomography. J Stroke Cerebrovasc Dis 26:34–41 https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.08.025
Booz C, Nöske J, Albrecht MH et al (2020) Diagnostic accuracy of color-coded virtual noncalcium dual-energy CT for the assessment of bone marrow edema in sacral insufficiency fracture in comparison to MRI. Eur J Radiol 129:109046 https://doi.org/10.1016/j.ejrad.2020.109046
Kelcz F, Joseph PM, Hilal SK (1979) Noise considerations in dual energy CT scanning. Med Phys 6:418–425 https://doi.org/10.1118/1.594520
Müller FC, Børgesen H, Gosvig K et al (2019) Optimising dual-energy CT scan parameters for virtual non-calcium imaging of the bone marrow: a phantom study. Eur Radiol Exp 3:46 https://doi.org/10.1186/s41747-019-0125-2
Pache G, Krauss B, Strohm P et al (2010) Dual-energy CT virtual noncalcium technique: detecting post-traumatic bone marrow lesions—feasibility study. Radiology 256:617–624 https://doi.org/10.1148/radiol.10091230
Wortman JR, Uyeda JW, Fulwadhva UP, Sodickson AD (2018) Dual-energy CT for abdominal and pelvic trauma. Radiographics. 38:586–602 https://doi.org/10.1148/rg.2018170058
Booz C, Nöske J, Martin SS et al (2019) Virtual noncalcium dual-energy CT: detection of lumbar disk herniation in comparison with standard gray-scale CT. Radiology 290:446–455 https://doi.org/10.1148/radiol.2018181286
Suh CH, Yun SJ, Jin W, Lee SH, Park SY, Ryu CW (2019) Diagnostic performance of dual-energy CT for the detection of bone marrow oedema: a systematic review and meta-analysis. Eur Radiol 28:4182–4194 https://doi.org/10.1007/s00330-018-5411-5
Jang SW, Chung BM, Kim WT, Gil JR (2019) Nondisplaced fractures on hip CT: added value of dual-energy CT virtual non-calcium imaging for detection of bone marrow edema using visual and quantitative analyses. Acta Radiol 60:1465–1473 https://doi.org/10.1177/0284185119831690
Kellock TT, Nicolaou S, Kim SSY et al (2017) Detection of bone marrow edema in nondisplaced hip fractures: utility of a virtual noncalcium dual-energy CT application. Radiology 284:798–805 https://doi.org/10.1148/radiol.2017161063
Deng H, Zheng W, Jankovic J (2015) Genetics and molecular biology of brain calcification. Ageing Res Rev 22:20–38 https://doi.org/10.1016/j.arr.2015.04.004
Martin V, Lemmen LJ (1952) Calcification in intracranial neoplasms. Am J Pathol 28:1107–1131
Chen W, Zhu W, Kovanlikaya I et al (2014) Intracranial calcifications and hemorrhages: characterization with quantitative susceptibility mapping. Radiology 270:496–505 https://doi.org/10.1148/radiol.13122640
Panagos PD, Jauch EC, Broderick JP (2002) Intracerebral hemorrhage. Emerg Med Clin North Am 20:631–655 https://doi.org/10.1016/s0733-8627(02)00015-9
Tanigawa N, Komemushi A, Kariya S et al (2006) Percutaneous vertebroplasty: relationship between vertebral body bone marrow edema pattern on MR images and initial clinical response. Radiology 239:195–200 https://doi.org/10.1148/radiol.2391050073
Han IH, Chin DK, Kuh SU et al (2009) Magnetic resonance imaging findings of subsequent fractures after vertebroplasty. Neurosurgery 64:740–745 https://doi.org/10.1227/01.NEU.0000339120.41053.F1
Klazen CAH, Lohle PNM, de Vries J et al (2010) Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 376:1085–1092 https://doi.org/10.1016/S0140-6736(10)60954-3
Frellesen C, Azadegan M, Martin SS et al (2018) Dual-energy computed tomography-based display of bone marrow edema in incidental vertebral compression fractures: diagnostic accuracy and characterization in oncological patients undergoing routine staging computed tomography. Invest Radiol 53:409–416 https://doi.org/10.1097/RLI.0000000000000458
Yang P, Wu G, Chang X (2018) Diagnostic accuracy of dual-energy computed tomography in bone marrow edema with vertebral compression fractures: A meta-analysis. Eur J Radiol 99:124–129 https://doi.org/10.1016/j.ejrad.2017.12.018
Guggenberger RC, Gnannt R, Hodler J et al (2012) Diagnostic performance of dual-energy CT for the detection of traumatic bone marrow lesions in the ankle: comparison with MR imaging. Radiology 264:164–173 https://doi.org/10.1148/radiol.12112217
Pache G, Bulla S, Baumann T et al (2012) Dose reduction does not affect detection of bone marrow lesions with dual-energy CT virtual noncalcium technique. Acad Radiol 19:1539–1545 https://doi.org/10.1016/j.acra.2012.08.006
Yeh BM, Shepherd JA, Wang ZJ, Teh HS, Hartman RP, Prevrhal S (2009) Dual-energy and low-kVp CT in the abdomen. AJR Am J Roentgenol 193:47–54 https://doi.org/10.2214/AJR.09.2592
Flohr TG, McCollough CH, Bruder H et al (2006) First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol 16:256–268 https://doi.org/10.1007/s00330-005-2919-2
Wang Y, Chen Y, Zheng H, Huang X, Shan C, Bao Y (2020) Detection of different degree traumatic vertebral bone marrow oedema by virtual non-calcium technique of dual-source dual-energy CT. Clin Radiol 75:156.e11–156.e19 https://doi.org/10.1016/j.crad.2019.09.143
Jeong SY, Jeon SJ, Seol M, Ahn TH, Juhng SK (2020) Diagnostic performance of dual-energy computed tomography for detection of acute spinal fractures. Skeletal Radiol. https://doi.org/10.1007/s00256-020-03450-8
Diekhoff T, Engelhard N, Fuchs M et al (2019) Single-source dual-energy computed tomography for the assessment of bone marrow oedema in vertebral compression fractures: a prospective diagnostic accuracy study. Eur Radiol 29:31–39 https://doi.org/10.1007/s00330-018-5568-y
Petritsch B, Kosmala A, Weng AM et al (2017) Vertebral compression fractures: third-generation dual-energy CT for detection of bone marrow edema at visual and quantitative analyses. Radiology 284:161–168 https://doi.org/10.1148/radiol.2017162165
Kaup M, Wichmann JL, Scholtz JE et al (2016) Dual-energy CT-based display of bone marrow edema in osteoporotic vertebral compression fractures: impact on diagnostic accuracy of radiologists with varying levels of experience in correlation to MR imaging. Radiology 280:510–519 https://doi.org/10.1148/radiol.2016150472
Abdullayev N, Große Hokamp N, Lennartz S et al (2019) Improvements of diagnostic accuracy and visualization of vertebral metastasis using multi-level virtual non-calcium reconstructions from dual-layer spectral detector computed tomography. Eur Radiol 29:5941–5949 https://doi.org/10.1007/s00330-019-06233-5
Diekhoff T, Hermann KG, Pumberger M, Hamm B, Putzier M, Fuchs M (2017) Dual-energy CT virtual non-calcium technique for detection of bone marrow edema in patients with vertebral fractures: A prospective feasibility study on a single- source volume CT scanner. Eur J Radiol 87:59–65 https://doi.org/10.1016/j.ejrad.2016.12.008
Foti G, Beltramello A, Catania M, Rigotti S, Serra G, Carbognin G (2019) Diagnostic accuracy of dual-energy CT and virtual non-calcium techniques to evaluate bone marrow edema in vertebral compression fractures. Radiol Med 124:487–494 https://doi.org/10.1007/s11547-019-00998-x
Herman MP, Kopetz S, Bhosale PR et al (2009) Sacral insufficiency fractures after preoperative chemoradiation for rectal cancer: incidence, risk factors, and clinical course. Int J Radiat Oncol Biol Phys 74:818–823 https://doi.org/10.1016/j.ijrobp.2008.08.054
Kushchayev SV, Glushko T, Jarraya M et al (2018) ABCs of the degenerative spin. Insights Imaging 9:253–274 https://doi.org/10.1007/s13244-017-0584-z
Shinohara Y, Sasaki F, Ohmura T, Itoh T, Endo T, Kinoshita T (2020) Evaluation of lumbar intervertebral disc degeneration using dual energy CT virtual non-calcium imaging. Eur J Radiol 124:108817 https://doi.org/10.1016/j.ejrad.2020.108817
van Rijn RM, Wassenaar M, Verhagen AP et al (2012) Computed tomography for the diagnosis of lumbar spinal pathology in adult patients with low back pain or sciatica: a diagnostic systematic review. Eur Spine J 21:228–239 https://doi.org/10.1007/s00586-011-2012-2
Notohamiprodjo S, Stahl R, Braunagel M et al (2017) Diagnostic accuracy of contemporary multidetector computed tomography (MDCT) for the detection of lumbar disc herniation. Eur Radiol 27:3443–3451 https://doi.org/10.1007/s00330-016-4686-7
Abeloff MD, Armitage JO, Niederhuber JE, Kastan MB, McKenna WG (2008) Abeloff’s Clinical Oncology, 4th edn. Churchill Livngstone Elsevier, Philadelphia, Pa, USA
Yang HL, Liu T, Wang XM, Xu Y, Deng SM (2011) Diagnosis of bone metastases: a meta-analysis comparing 18FDG PET, CT, MRI and bone scintigraphy. Eur Radiol 21:2604–2617 https://doi.org/10.1007/s00330-011-2221-4
Kosmala A, Weng AM, Krauss B, Knop S, Bley TA, Petritsch B (2018) Dual-energy CT of the bone marrow in multiple myeloma: diagnostic accuracy for quantitative differentiation of infiltration patterns. Eur Radiol 28:5083–5090 https://doi.org/10.1007/s00330-018-5537-5
Wang Q, Sun Z, Li S et al (2017) Bone marrow imaging by third-generation dual-source dual-energy CT using virtual noncalcium technique for assessment of diffuse infiltrativelesions of multiple myeloma. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 39:114–119 https://doi.org/10.3881/j.issn.1000-503X.2017.01.019
Ensrud KE (2013) Epidemiology of fracture risk with advancing age. J Gerontol A Biol Sci Med Sci 68:1236–1242 https://doi.org/10.1093/gerona/glt092
Reddy T, McLaughlin PD, Mallinson PI et al (2015) Detection of occult, undisplaced hip fractures with a dual-energy CT algorithm targeted to detection of bone marrow edema. Emerg Radiol 22:25–29 https://doi.org/10.1007/s10140-014-1249-6
Wu H, Zhang G, Shi L et al (2019) Axial spondyloarthritis: dual-energy virtual noncalcium CT in the detection of bone marrow edema in the sacroiliac joints. Radiology 290:157–164 https://doi.org/10.1148/radiol.2018181168
Chen M, Herregods N, Jaremko JL et al (2020) Bone marrow edema in sacroiliitis: detection with dual-energy CT. Eur J Radiol 30:3393–3400 https://doi.org/10.1007/s00330-020-06670-7
Jans L, De Kock I, Herregods N et al (2018) Dual-energy CT: a new imaging modality for bone marrow oedema in rheumatoid arthritis. Ann Rheum Dis 77:958–960 https://doi.org/10.1136/annrheumdis-2018-213152
Guggenberger R (2019) Dual-energy CT in the detection of bone marrow edema in the sacroiliac joints: is there a case for axial spondyloarthritis? Radiology 290:165–166 https://doi.org/10.1148/radiol.2018182224
Foti G, Faccioli N, Silva R, Oliboni E, Zorzi C, Carbognin G (2020) Bone marrow edema around the hip in non-traumatic pain: dual-energy CT vs MRI. Eur Radiol 30:4098–4106 https://doi.org/10.1007/s00330-020-06775-z
Burke MC, Garg A, Youngner JM, Deshmukh SD, Omar IM (2019) Initial experience with dual-energy computed tomography-guided bone biopsies of bone lesions that are occult on monoenergetic CT. Skeletal Radiol 48:605–613 https://doi.org/10.1007/s00256-018-3087-1
Mallee WH, Wang J, Poolman RW et al (2015) Computed tomography versus magnetic resonance imaging versus bone scintigraphy for clinically suspectedscaphoid fractures in patients with negative plain radiographs. Cochrane Database Syst Rev:CD010023 https://doi.org/10.1002/14651858.CD010023
Peh WC, Gilula LA, Wilson AJ (1996) Detection of occult wrist fractures by magnetic resonance imaging. Clin Radiol 51:285–292 https://doi.org/10.1016/s0009-9260(96)80348-5
Newton EJ, Love J (2007) Emergency department management of selected orthopedic injuries. Emerg Med Clin North Am 25:763–793 https://doi.org/10.1016/j.emc.2007.07.003
Markhardt BK, Gross JM, Monu JUV (2009) Schatzker Classification of Tibial Plateau Fractures: Use of CT and MR Imaging Improves Assessment. Radiographics 29:585–597 https://doi.org/10.1148/rg.292085078
Wang MY, Zhang XY, Xu L et al (2019) Detection of bone marrow edema in knee joints using a dual-energy CT virtual non-calcium technique. Clin Radiol 74:815.e1–815.e7 https://doi.org/10.1016/j.crad.2019.06.020
Yang SJ, Jeon JY, Lee SW, Jeong YM (2020) Added value of color-coded virtual non-calcium dual-energy CT in the detection of acute knee fractures in non-radiology inexpert readers. Eur J Radiol 129:109112 https://doi.org/10.1016/j.ejrad.2020.109112
Booz C, Nöske J, Lenga L et al (2020) Color-coded virtual non-calcium dual-energy CT for the depiction of bone marrow edema in patients with acute knee trauma: a multireader diagnostic accuracy study. Eur Radiol 30:141–150 https://doi.org/10.1007/s00330-019-06304-7
Yadav H, Khanduri S, Yadav P, Pandey S, Yadav VK, Khan S (2020) Diagnostic accuracy of dual energy CT in the assessment of traumatic bone marrow edema of lower limb and its correlation with MRI. Indian J Radiol Imaging 30:59–63 https://doi.org/10.4103/ijri.IJRI_59_19
Dareez NM, Dahlslett KH, Engesland E, Lindland ES (2017) Scaphoid fracture: bone marrow edema detected with dual-energy CT virtual non-calcium images and confirmed with MRI. Skeletal Radiol 46:1753–1756 https://doi.org/10.1007/s00256-017-2730-6
Booz C, Nöske J, Albrecht MH et al (2019) Traumatic bone marrow edema of the calcaneus: evaluation of color-coded virtual non-calcium dual-energy CT in a multi-reader diagnostic accuracy study. Eur J Radiol 118:207–214 https://doi.org/10.1016/j.ejrad.2019.07.023
Ali IT, Wong WD, Liang T et al (2018) Clinical utility of dual-energy CT analysis of bone marrow edema in acute wrist fractures. AJR Am J Roentgenol 210:842–847 https://doi.org/10.2214/AJR.17.18673
Foti G, Catania M, Caia S et al (2019) Identification of bone marrow edema of the ankle: diagnostic accuracy of dual-energy CT in comparison with MRI. Radiol Med 124:1028–1036 https://doi.org/10.1007/s11547-019-01062-4
Koch V, Müller FC, Gosvig K et al (2021) Incremental diagnostic value of color-coded virtual non-calcium dual-energy CT for the assessment of traumatic bone marrow edema of the scaphoid. Eur Radiol. https://doi.org/10.1007/s00330-020-07541-x
Mallinson PI, Stevens C, Reisinger C, Nicolaou S, Munk PL, Ouellette H (2013) Achilles tendinopathy and partial tear diagnosis using dual-energy computed tomography collagen material decomposition application. J Comput Assist Tomogr 37:475–477 https://doi.org/10.1097/RCT.0b013e318287efa0
Hachamovitch R, Nutter B, Hlatky MA et al (2012) SPARC investigators, patient management after noninvasive cardiac imaging results from SPARC (Study of myocardial perfusion and coronary anatomy imaging roles in coronary artery disease). J Am Coll Cardiol 59:462–474 https://doi.org/10.1016/j.jacc.2011.09.066
Lell MM, Ditt H, Panknin C et al (2007) Bone-subtraction CT angiography: evaluation of two different fully automated image-registration procedures for interscan motion compensation. AJNR Am J Neuroradiol 28:1362–1368 https://doi.org/10.3174/ajnr.A0558
Tabari A, Gee MS, Singh R et al (2020) Reducing eadiation dose and contrast medium volume with application of dual-energy CT in children and young adults. AJR Am J Roentgenol 214:1199–1205 https://doi.org/10.2214/AJR.19.22231
D’Angelo T, Lenga L, Arendt CT et al (2020) Carotid and cerebrovascular dual-energy computed tomography angiography: Optimization of window settings for virtual monoenergetic imaging reconstruction. Eur J Radiol 130:109166 https://doi.org/10.1016/j.ejrad.2020.109166
Leithner D, Mahmoudi S, Wichmann JL et al (2018) Evaluation of virtual monoenergetic imaging algorithms for dual-energy carotid and intracerebral CT angiography: Effects on image quality, artefacts and diagnostic performance for the detection of stenosis. Eur J Radiol 99:11–117 https://doi.org/10.1016/j.ejrad.2017.12.024
Mannil M, Ramachandran J, Vittoria de Martini I et al (2017) Modified dual-energy algorithm for calcified plaque removal: evaluation in carotid computed tomography angiography and comparison with digital subtraction angiography. Invest Radiol 52:680–685 https://doi.org/10.1097/RLI.0000000000000391
Alkadhi H, Euler A (2020) The future of computed tomography: personalized, functional, and precise. Invest Radiol 55:545–555 https://doi.org/10.1097/RLI.0000000000000668
Stamp LK, Anderson NG, Becce F et al (2019) Clinical utility of multi-energy spectral photon-counting computed tomography in crystal arthritis. Arthritis Rheumatol 71:1158–1162 https://doi.org/10.1002/art.40848
Riederer I, Si-Mohamed S, Ehn S et al (2019) Differentiation between blood and iodine in a bovine brain-initial experience with spectral photon-counting computed tomography (SPCCT). PLoS One 14:e0212679 https://doi.org/10.1371/journal.pone.0212679
Sartoretti T, Eberhard M, Rüschoff JH et al (2020) Photon-counting CT with tungsten as contrast medium: experimental evidence of vessel lumen and plaque visualization. Atherosclerosis. 310:11–16 https://doi.org/10.1016/j.atherosclerosis.2020.07.023
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
TD, DC, MHA, and CB have contributed to the design and implementation of the research, to the analysis of the data, and to the writing of the manuscript. All authors have approved the submitted final version of the manuscript and have agreed to be personally accountable for the author’s own contributions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Consent for publication has been obtained.
Competing interests
MHA received speaking fees from Siemens Healthineers and GE Healthcare. CB received speaking fees from Siemens Healthineers. TA and MHA are members of the European Radiology Experimental Editorial Board and they have not taken part in the review or acceptance process of this article. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
D’Angelo, T., Albrecht, M.H., Caudo, D. et al. Virtual non-calcium dual-energy CT: clinical applications. Eur Radiol Exp 5, 38 (2021). https://doi.org/10.1186/s41747-021-00228-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41747-021-00228-y