Abstract
The biological effects and physiological consequences of hypercapnia are increasingly understood. The literature on hypercapnia is confusing, and at times contradictory. On the one hand, it may have protective effects through attenuation of pulmonary inflammation and oxidative stress. On the other hand, it may also have deleterious effects through inhibition of alveolar wound repair, reabsorption of alveolar fluid, and alveolar cell proliferation. Besides, hypercapnia has meaningful effects on lung physiology such as airway resistance, lung oxygenation, diaphragm function, and pulmonary vascular tree.
In acute respiratory distress syndrome, lung-protective ventilation strategies using low tidal volume and low airway pressure are strongly advocated as these have strong potential to improve outcome. These strategies may come at a price of hypercapnia and hypercapnic acidosis. One approach is to accept it (permissive hypercapnia); another approach is to treat it through extracorporeal means. At present, it remains uncertain what the best approach is.
Similar content being viewed by others
Background
Patients with acute respiratory failure almost always develop gas exchange derangements that may result in hypercapnia [1]. Lung-protective ventilation strategies are strongly recommended to prevent additional lung injury [2, 3], but these strategies have a strong potential to increase plasma carbon dioxide levels further. One approach is to accept this, i.e., “permissive hypercapnia,” with the option to correct respiratory acidosis by slow bicarbonate infusion for blood buffering. Extracorporeal decapneization by utilizing “extracorporeal CO2 removal” (ECCO2R) is an appealing alternative for permissive hypercapnia but comes with the typical risks of extracorporeal circulation.
Hypercapnia has been suggested to have beneficial effects, including a reduction in pulmonary inflammation and alveolar oxidative stress [4,5,6,7]. Hypercapnia, however, may also have deleterious effects, such as impairments in tissue repair and decreased alveolar fluid clearance [8,9,10,11]. Seen these seemingly opposite effects, it becomes increasingly important to determine the net consequence of hypercapnia. Indeed, the number one question in patients with acute respiratory distress syndrome (ARDS), who either have hypercapnia or develop hypercapnia as a consequence of lung-protective ventilator settings, is whether hypercapnia should be accepted, or prevented and corrected.
This narrative review provides an overview of the various biological and physiological effects of hypercapnia and discusses current strategies affecting the plasma carbon dioxide levels in ARDS patients.
Biological effects of hypercapnia—preclinical studies
Several preclinical studies have shown hypercapnia displays profound impact on alveolar cells and humoral factors that all could play a role in lung injury. Some of these effects can be seen as potentially beneficial, while others, in theory, could be harmful.
Effects of hypercapnia on alveolar cells (Table 1)
Hypercapnia has been found to decrease microvascular permeability, lung edema formation, and bronchoalveolar lavage protein content in the rabbit lungs subjected to ex vivo ventilation with high pressures [4]. Hypercapnia also reduced histologically confirmed lung injury in ventilated mice [5]. The plausible mechanisms are related to the action of carbon dioxide upon the nuclear factor kappa pathway, which prevents p65 translocation and reducing inflammation [12, 13].
It also attenuated apoptosis in rabbits subjected to ischemia and reperfusion injury [6], and buffering hypercapnic acidosis worsened lung injury in this model [14]. One of the proposed mechanisms is the inhibitory action of CO2 on the ADAM-17 (a sheddase), thus preventing the activation of the p44/p42 MAPK pathway and, by this way, reducing apoptosis [15]. Finally, hypercapnia resulted in less cell injury and neutrophil adherence to endothelial monolayers in stimulated pulmonary endothelial cells [16].
Contrasting, in rats exposed to hypercapnia for 48 h, a challenge with Escherichia coli caused neutrophils to have impaired phagocytic activity, with higher bacterial colony counts in the lungs of these animals, possibly because of impairment in neutrophil function under sustained hypercapnic acidotic environment [17]. Hypercapnia worsened injury and induce apoptosis in alveolar type 2 epithelial cells via a nitric oxide-dependent pathway in an in vitro model with fetal rat alveolar cells pre-incubated with lipopolysaccharide (LPS) and cytokines [18]. Also, hypercapnia dose-dependently impaired alveolar cell proliferation and delayed wound repair in an in vitro scratch wound model of three different types of human lung cells [8]. These effects persisted with buffering of the hypercapnic acidosis. In line with this observation, in ex vivo and in vitro rat models of ventilator-induced lung injury (VILI), hypercapnic acidosis impaired membrane wound resealing. Carbon dioxide rather than pH reduced the rate of wound closure (cell migration) in a dose-dependent manner via NF-kB pathway inhibition. Furthermore, hypercapnia caused mitochondrial dysfunction and impaired cell proliferation in an in vitro model of cultured human alveolar epithelial cells by induction of miR-183, a microRNA, which in turn downregulated isocitrate dehydrogenase 2, a key enzyme of the tricarboxylic acid cycle that catalyzes the conversion of isocitrate to α-ketoglutarate, leading to mitochondrial dysfunction and impaired proliferation of alveolar epithelial cells [19].
Effects of hypercapnia on humoral processes (Table 2)
Hypercapnia has been found to attenuate cytokine production and oxygen free radical formation in mice subjected to alveolar stretch [5, 15]. Furthermore, hypercapnia markedly reduced apoptosis, oxidative stress, and inflammation in alveolar epithelial cells from high-pressure ventilation-stimulated rat lungs [20]. Hypercapnic acidosis (HCA) exerts anti-inflammatory effects in rabbits with endotoxin-induced lung injury [16].
On the contrary, hypercapnia has been found to selectively inhibit the expressions of proinflammatory cytokines in human and mouse macrophage cell lines [21]. In in vitro human cells’ experiments, hypercapnia inhibited activation of the NF-κB pathway [13, 22], independent of pH.
Effects of hypercapnia on alveolar fluid clearance
Hypercapnic acidosis reduced alveolar edema formation by inhibiting an increase in pulmonary capillary included by free radicals [7], ischemia-reperfusion [14], and high-stretch ventilation in in vitro and in vivo models [23].
However, hypercapnia has also been found to decrease alveolar fluid clearance by decreasing Na+, K+-ATPase activity in the alveoli basal membrane in in vivo studies in large and small animal models [9, 24], in ex vivo studies using a rodent lung model [10], and in human alveolar epithelial cells [11].
Physiologic effects of hypercapnia—animal and human studies
Several studies have shown various effects of hypercapnia on the respiratory system.
Effects of hypercapnia on airway resistance
Hypercapnia may either decrease or increase airway resistance. Alveolar hypercapnia decreases airway resistance by relaxing smooth muscle small bronchi (a direct effect) in healthy subjects [25], while systemic hypercapnia causes vagal nerve-mediated constriction of the larger airway (an indirect effect) in animal models [26]. These opposing but balanced effects may produce a little net alteration in airway resistance [27].
Effects of hypercapnia on the oxygenating capacity of the lung
Hypercapnia potentiates hypoxic pulmonary vasoconstriction with a reduction in intrapulmonary shunt, improving gas exchange in normal [28,29,30] and diseased lungs [31, 32]. Hypercapnia also increases lung compliance, directing ventilation to the underventilated lung regions resulting in a better match between ventilation and perfusion in the lung of dogs [33]. The mechanism might be through increased alveolar surfactant secretion and more effective surface tension-lowering properties of surfactant under acidic conditions [31]. However, in an in vivo rat model of prolonged E. coli pneumonia, hypercapnia lowered static lung compliance compared to normocapnia [17]. Sustained hypercapnia may impair neutrophil function, increasing bacterial load, contributing to increased lung injury and worst compliance [14].
Both hypercapnia and hypercapnic acidosis shift the hemoglobin–oxygen dissociation curve to the right and may increase hematocrit, augmenting the release of oxygen to the tissues in a canine model [34]. It also increases cardiac output through sympathoadrenal mechanisms [35]. The secondary rise in cardiac output is associated with increased preload, afterload, contractility, and elevated heart rate [36]. The overall effect is better oxygenation and improved global oxygen supply.
On the other hand, hypercapnia lowers alveolar oxygen tension by the following formula PAO2 = FiO2 (PB-47)—(PaCO2/R), where PAO2 is the alveolar oxygen tension, PB is the barometric pressure, and R is the respiratory quotient. However, compared to alterations in FiO2 [37], the effect on alveolar oxygenation by alterations in alveolar ventilation is small.
The overall effect of these mechanisms is that blood oxygenation may remain mostly unchanged or improved.
Effects of hypercapnia on diaphragm function
Hypercapnic acidosis preserves diaphragmatic contractility and prevents ventilation-induced diaphragmatic myosin loss and inflammation in pigs [38]. However, hypercapnic acidosis impairs diaphragmatic function in spontaneously breathing patients, through effects on afferent transmission by the vagal nerve [39].
The clinical effect of hypercapnia upon diaphragmatic function needs to be further elucidated.
Effects of hypercapnia on pulmonary vasculature
In models of pulmonary hypertension induced by chronic hypoxia and right ventricular dysfunction, hypercapnic acidosis attenuates pulmonary hypertension, normalizes right ventricular function, and preserves the endothelial integrity and pulmonary vascular remodeling [40,41,42]. The effects of hypercapnic acidosis on vasoconstriction and resistance in the pulmonary circulation have also been found in humans [35]. These effects are exacerbated in the setting of preexisting pulmonary hypertension, such as found with ARDS [43].
The impact of hypercapnia in acute respiratory distress syndrome
Supportive care with mechanical ventilation remains the mainstay of ARDS management with a goal to minimize lung injury caused by the forces created by mechanical ventilation. Treatment algorithms for ARDS typically begin with optimization of the settings to achieve the so-called lung-protective ventilation and proceed through increasing invasiveness based on physiological goals of gas exchange. These include higher positive end-expiratory pressures, lung recruitment manoeuvers, prone positioning, and extracorporeal removal of carbon dioxide.
Permissive hypercapnia
Lung-protective ventilation with volumes limited to 6–8 mL/kg of predicted body weight (PBW) or lower, and plateau pressure < 30 cm H2O, dramatically increases survival [2]. As a consequence of reducing alveolar ventilation with lower tidal volumes, hypercapnia results. Recognizing that low tidal volume ventilation confers survival benefits by reducing lung stretch and the cyclical collapse of alveoli, clinicians have accepted hypercapnia, giving rise to the concept of permissive hypercapnia [44]. However, it remains unclear whether hypercapnic acidosis carries survival benefits independent of using low tidal volumes (Table 3).
In a retrospective analysis of the ARDS network, hypercapnic acidosis was associated with lower mortality in the group of patients receiving tidal volumes of 12 mL/kg PBW. However, there was no survival benefit in patients ventilated at tidal volumes of 6 mL/kg PBW [45]. It was hypothesized that lung-protective ventilation reduced lung injury caused by the ventilator to a point where the protective effect of hypercapnic acidosis could not be detected.
In a multicenter randomized clinical trial comparing low (7 mL/kg PBW) with conventional tidal volumes (10 mL/kg PBW), a trend towards higher mortality was observed in patients who developed hypercapnia and acidosis [46]. These findings resulted in a premature stop of that trial, making interpretation of the results difficult.
Recently, a post hoc analysis of three prospective non-interventional international studies in ARDS patients was published [47]. In this analysis, severe hypercapnia (PaCO2 > 50 mmHg) was associated with higher mortality and more organ failures compared to patients with normocapnia. Acidosis or the combination of hypercapnia and acidosis independently increased the risk of mortality in the intensive care unit. The incidence of severe hypercapnia increased significantly with the time (1998, 2004, and 2010) as a consequence of the diverse respiratory strategies practiced over the years, which may reflect the feeling of many intensivists that hypercapnia could be beneficial [47].
Finally, one retrospective analysis including over 250,000 ARDS patients receiving mechanical ventilation showed that patients who developed hypercapnic acidosis (pH < 7.35 PaCO2 > 65 mmHg) during the first 24 h of mechanical ventilation had significantly higher mortality than those who had compensated hypercapnia or normocapnia [48].
Lung overdistension
The rationale for using positive end-expiratory pressure (PEEP) is to mitigate the injurious effects of repetitive opening and closing of lung units by restoring the functional size of the lung, promoting lung protection, and improving gas exchange and lung mechanics. However, high levels of PEEP may lead to overdistension of lung units, especially those that remained normally aerated within heterogeneous ARDS lungs, and this may increase alveolar dead space [49,50,51]. The consequence of this will be a rise of carbon dioxide levels.
In a recent international randomized clinical trial in ARDS patients, the use of the “open lung approach” actually increased 28-day mortality [52]. Notably, this trial used aggressive recruitment manoeuvers and “super high” levels of positive end-expiratory pressure compared to previous trials [53,54,55]. It is also worth to note that patients in this trial had much higher blood carbon dioxide levels than patients in previous trials that tested the “open lung approach.” It could be hypothesized that this reflects an increase in dead space secondary to overdistension.
Extracorporeal CO2 removal (Table 4 and Additional file 1)
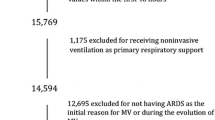
Despite lung-protective ventilation strategies, up to 30% of patients with ARDS have evidence of tidal hyperinflation, representing a potential risk of VILI [56]. A strategy of “ultraprotective ventilation” with tidal volumes lower than 6 mL/kg PBW requires extracorporeal decapneization.
This approach has been tested in two trials in ARDS patients, resulting in less lung injury caused by ventilation [57] and a decrease in the number of ventilation days [58]. In one feasibility study, ECCO2R facilitated ventilation with ultralow tidal volumes near to 3 mL/kg PBW, while preventing hypercapnic acidosis [59]. These findings were confirmed in a recently completed international multicenter randomized clinical trial (ClinicalTrials.gov/ct2/show/NCT02282657). One currently recruiting randomized clinical trial evaluates whether ultraprotective ventilation by employing ECCO2R affects 90-day mortality in patients with hypoxemic acute respiratory failure (ClinicalTrials.gov/ct2/show/NCT02654327).
Although ECCO2R seems to be effective in mitigating hypercapnic acidosis and possibly in reducing VILI and mechanical ventilation days, ECCO2R may have pulmonary and hemodynamic consequences. It can be associated to adverse effects such worsening hypoxemia and increased FiO2 requirements due to a decrease in mean airway pressure, low ventilation-perfusion ratio, and lower partial pressure of alveolar oxygen secondary to a decreased lung respiratory quotient [60, 61]. Besides, because of the low flow system of ECCO2R, higher anticoagulation requirements are needed in order to maintain ECCO2R efficiency and performance. Therefore, significant complications may occur as a consequence of anticoagulation or catheter insertion with hemodynamic instability and a higher number of red blood cell transfusions needed [59, 62,63,64].
It is worth to say that ECCO2R may be a promising adjuvant therapeutic strategy for reducing the impact of mechanical ventilation through ultraprotective ventilation rather than to mitigate hypercapnia in patients under conventional lung-protective ventilation. For the time being, the available literature does not provide definitive information on the usefulness of ECCO2R in patients with acute respiratory failure. Its use for the moment is experimental.
Conclusion
It is increasingly recognized that CO2 is much more than just a waste product of cellular metabolism. Indeed, it should be seen as a potent biological agent that exerts protective as well as harmful effects. Hypercapnia may develop in ARDS patients, and what the exact impact of high carbon dioxide levels on the outcome remains uncertain. More importantly, whether it should be accepted or whether it should be prevented or treated with invasive techniques for extracorporeal removal remains highly uncertain.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CO2 :
-
Carbon dioxide
- ECCO2R:
-
Extracorporeal carbon dioxide removal
- HCA:
-
Hypercapnic acidosis
- LPS:
-
Lipopolysaccharide
- NF-kB:
-
Nuclear factor kappa B
- PaCO2 :
-
Partial arterial pressure of carbon dioxide
- PaO2 :
-
Partial alveolar pressure of oxygen
- PBW:
-
Predicted body weight
- VILI:
-
Ventilator-induced lung injury
References
Nuckton TJ, Alonso JA, Kallet RH et al (2002) Pulmonary dead-space fraction as a risk factor for death in the acute respiratory distress syndrome. N Engl J Med 346:1281–1286
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Putensen C, Theuerkauf N, Zinserling J et al (2009) Meta-analysis: ventilation strategies and outcomes of the acute respiratory distress syndrome and acute lung injury. Ann Intern Med 151(8):566–576
Broccard AF, Hotchkiss JR, Vannay C et al (2001) Protective effects of hypercapnic acidosis on ventilator-induced lung injury. Am J Respir Crit Care Med 164:802–806
Peltekova V, Engelberts D, Otulakowski G et al (2010) Hypercapnic acidosis in ventilator-induced lung injury. Intensive Care Med 36:869–878
Laffey JG, Tanaka M, Engelberts D et al (2000) Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med 162:2287–2294
Shibata K, Cregg N, Engelberts D et al (1998) Hypercapnic acidosis may attenuate acute lung injury by inhibition of endogenous xanthine oxidase. Am J Respir Crit Care Med 158(5 Pt):1578–1584
O’Toole D, Hassett P, Contreras M et al (2009) Hypercapnic acidosis attenuates pulmonary epithelial wound repair by an NF-kappaB dependent mechanism. Thorax. 64:976–982
Briva A, Vadász I, Lecuona E et al (2007) High CO2 levels impair alveolar epithelial function independently of pH. PLoS One 2:e1238
Welch LC, Lecuona E, Briva A et al (2010) Extracellular signal-regulated kinase (ERK) participates in the hypercapnia-induced Na,K-ATPase downregulation. FEBS Lett 584:3985–3989
Lecuona E, Sun H, Chen J et al (2013) Protein kinase A-Ialpha regulates Na,K-ATPase endocytosis in alveolar epithelial cells exposed to high CO2 concentrations. Am J Respir Cell Mol Biol 48:626–634
Contreras M, Ansari B, Curley G et al (2012) Hypercapnic acidosis attenuates ventilation-induced lung injury by a nuclear factor-kappaB-dependent mechanism. Crit Care Med 40:2622–2630
Cummins EP, Oliver KM, Lenihan CR et al (2010) NF-κB links CO2 sensing to innate immunity and inflammation in mammalian cells. J Immunol 185:4439–4445
Laffey JG, Engelberts D, Kavanagh BP (2000) Buffering hypercapnic acidosis worsens acute lung injury. Am J Respir Crit Care Med 161:141–146
Otulakowski G, Engelberts D, Gusarova GA et al (2014) Hypercapnia attenuates ventilator induced lung injury via a disintegrin and metalloprotease-17. J Physiol 592:4507–4521
Takeshita K, Suzuki Y, Nishio K et al (2003) Hypercapnic acidosis attenuates endotoxin-induced nuclear factor-[kappa]B activation. Am J Respir Cell Mol Biol 29(1):124–132
O’Croinin DF, Nichol AD, Hopkins N et al (2008) Sustained hypercapnic acidosis during pulmonary infection increases bacterial load and worsens lung injury. Crit Care Med 36(7):2128–2135
Lang JD Jr, Chumley P, Eiserich JP et al (2000) Hypercapnia induces injury to alveolar epithelial cells via a nitric oxide-dependent pathway. Am J Phys Lung Cell Mol Phys 279:L994–L1002
Vohwinkel CU, Lecuona E, Sun H et al (2011) Elevated CO(2) levels cause mitochondrial dysfunction and impair cell proliferation. J Biol Chem 286(43):37067–37076
Yang WC, Song CY, Wang N et al (2013) Hypercapnic acidosis confers antioxidant and anti-apoptosis effects against ventilator-induced lung injury. Lab Investig 93:1339–1349
Wang N, Gates KL, Trejo H et al (2010) Elevated CO2 selectively inhibits interleukin-6 and tumor necrosis factor expression and decreases phagocytosis in the macrophage. FASEB J 24:2178–2190
Oliver KM, Lenihan CR, Bruning U et al (2012) Hypercapnia induces cleavage and nuclear localization of RelB protein, giving insight into CO2 sensing and signaling. J Biol Chem 287:14004–14011
Laffey JG, Engelberts D, Duggan M et al (2003) Carbon dioxide attenuates pulmonary impairment resulting from hyperventilation. Crit Care Med 31:2634–2640
Lecuona E, Trejo HE, Sznajder JI (2007) Regulation of Na,K-ATPase during acute lung injury. J Bioenerg Biomembr 39(5–6):391–395
D’Angelo E, Calderini IS, Tavola M (2001) The effects of CO2 on respiratory mechanics in anesthetized paralyzed humans. Anesthesiology. 94(4):604–610
Lele EE, Hantos Z, Bitay M et al (2011) Bronchoconstriction during alveolar hypocapnia and systemic hypercapnia in dogs with a cardiopulmonary bypass. Respir Physiol Neurobiol 175(1):140–145
Butler J, Caro CG, Alcala R et al (1960) Physiological factors affecting airway resistance in normal subjects and in patients with obstructive respiratory disease. J Clin Invest 39:584–591
Swenson ER, Robertson HT, Hlastala MP (1994) Effects of inspired carbon dioxide on ventilation-perfusion matching in normoxia, hypoxia, and hyperoxia. Am J Respir Crit Care Med 149:1563–1569
Brogan TV, Hedges RG, McKinney S et al (2000) Pulmonary NO synthase inhibition and inspired CO2: effects on V’/Q’ and pulmonary blood flow distribution. Eur Respir J 16:288
Brogan TV, Robertson HT, Lamm WJ et al (2004) Carbon dioxide added late in inspiration reduces ventilation-perfusion heterogeneity without causing respiratory acidosis. J Appl Physiol 96:1894–1898
Keenan RJ, Todd TR, Demajo W et al (1990) Effects of hypercarbia on arterial and alveolar oxygen tensions in a model of gram-negative pneumonia. Appl Phys 68:1820–1825
Sinclair SE, Kregenow DA, Starr I et al (2006) Therapeutic hypercapnia and ventilation-perfusion matching in acute lung injury: low minute ventilation vs inspired CO2. Chest. 130:85–92
Wildeboer-Venema F (1980) The influences of temperature and humidity upon the isolated surfactant film of the dog. Respir Physiol 39:63–71
Torbati D, Mangino MJ, Garcia E et al (1998) Acute hypercapnia increases the oxygen-carrying capacity of the blood in ventilated dogs. Crit Care Med 26(11):1863–1867
Kregenow DA, Swenson ER (2002) The lung and carbon dioxide: implications for permissive and therapeutic hypercapnia. Eur Respir J 20:6–11
Cullen DJ, Eger EI 2nd (1974) Cardiovascular effects of carbon dioxide in man. Anesthesiology. 41(4):345–349
Bidani A, Tzouanakis AE, Cardenas VJ et al (1994) Permissive hypercapnia in acute respiratory failure. JAMA. 272(12):957–962
Jung B, Sebbane M, Le Goff C et al (2013) Moderate and prolonged hypercapnic acidosis may protect against ventilator-induced diaphragmatic dysfunction in healthy piglet: an in vivo study. Crit Care 17:R15
Jonville S, Delpech N, Dejean A (2002) Contribution of respiratory acidosis to diaphragmatic fatigue at exercise. Eur Respir J 19:1079–1086
Dunlop K, Gosal K, Kantores C et al (2014) Therapeutic hypercapnia prevents inhaled nitric oxide-induced right-ventricular systolic dysfunction in juvenile rats. Free Radic Biol Med 69:35–49
Peng G, Ivanovska J, Kantores C et al (2012) Sustained therapeutic hypercapnia attenuates pulmonary arterial Rho-kinase activity and ameliorates chronic hypoxic pulmonary hypertension in juvenile rats. Am J Physiol Heart Circ Physiol 302:H2599–H2611
Ketabchi F, Ghofrani HA, Schermuly RT et al (2012) Effects of hypercapnia and NO synthase inhibition in sustained hypoxic pulmonary vasoconstriction. Respir Res 13:7
Lhéritier G, Legras A, Caille A et al (2013) Prevalence and prognostic value of acute cor pulmonale and patent foramen ovale in ventilated patients with early acute respiratory distress syndrome: a multicenter study. Intensive Care Med 39:1734–1742
Curley GF, Laffey JG, Kavanagh BP (2013) CrossTalk proposal: there is added benefit to providing permissive hypercapnia in the treatment of ARDS. J Physiol 591(11):2763–2765
Kregenow DA, Rubenfeld GD, Hudson LD et al (2006) Hypercapnic acidosis and mortality in acute lung injury. Crit Care Med 34:1–7
Brochard L, Roudot-Thoraval F, Roupie E et al (1998) Tidal volume reduction for prevention of ventilator-induced lung injury in acute respiratory distress syndrome. Am J Respir Crit Care Med 158:1831–1838
Nin N, Muriel A, Peñuelas O et al (2017) Severe hypercapnia and outcome of mechanically ventilated patients with moderate or severe acute respiratory distress syndrome. Intensive Care Med 43:200–208
Tiruvoipati R, Pilcher D, Buscher H et al (2017) Effects of hypercapnia and hypercapnic acidosis on hospital mortality in mechanically ventilated patients. Crit Care Med 45:e649–e656
Suter PM, Fairley B, Isenberg MD (1975) Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med 292(6):284–289
Blanch L, Lucangelo U, Lopez-Aguilar J et al (1999) Volumetric capnography in patients with acute lung injury: effects of positive end-expiratory pressure. Eur Respir J 13(5):1048–1054
Beydon L, Uttman L, Rawal R et al (2002) Effects of positive end-expiratory pressure on dead space and its partitions in acute lung injury. Intensive Care Med 28(9):1239–1245
Cavalcanti AB, Suzumura ÉA, Laranjeira LN et al (2017) Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 318(14):1335–1345
Brower RG, Lanken PN, MacIntyre N et al (2004) Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 351(4):327–336
Mercat A, Richard JC, Vielle B et al (2008) Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 299(6):646–655
Meade MO, Cook DJ, Guyatt GH et al (2009) Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 299(6):637–645
Terragni PP, Rosboch G, Tealdi A et al (2007) Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med 175(2):160–166
Terragni PP, Del Sorbo L, Mascia L et al (2009) Tidal volume lower than 6 ml/kg enhances lung protection: role of extracorporeal carbon dioxide removal. Anesthesiology. 111(4):826–835. https://doi.org/10.1097/ALN.0b013e3181b764d2
Bein T, Weber-Carstens S, Goldmann A et al (2013) Lower tidal volume strategy (≈3 ml/kg) combined with extracorporeal CO2 removal versus “conventional” protective ventilation (6 ml/kg) in severe ARDS: the prospective randomized Xtravent-study. Intensive Care Med 39:847–856
Fanelli V, Ranieri MV, Mancebo J et al (2016) Feasibility and safety of low-flow extracorporeal carbon dioxide removal to facilitate ultra-protective ventilation in patients with moderate acute respiratory distress syndrome. Crit Care 20(1):36. https://doi.org/10.1186/s13054-016-1211-y
Gattinoni L (2016) Ultra-protective ventilation and hypoxemia. Crit Care 20:130–131
Gattinoni L, Kolobow T, Tomlinson T et al (1978) Low-frequency positive pressure ventilation with extracorporeal carbon dioxide removal (LFPPV-ECCO2R): an experimental study. Anesth Analg 57(4):470–477
Kluge S, Braune SA, Engel M et al (2012) Avoiding invasive mechanical ventilation by extracorporeal carbon dioxide removal in patients failing noninvasive ventilation. Intensive Care Med 38:1632–1639
Burki NK, Mani RK, Herth FJF et al (2013) COPD a novel extracorporeal CO2 removal results of a pilot study of hypercapnic respiratory failure in patients with COPD. Chest. 143(3):678–686. https://doi.org/10.1378/chest.12-0228
Del Sorbo L, Fan E, Nava S et al (2016) ECCO2R in COPD exacerbation only for the right patients and with the right strategy. Intensive Care Med 42(11):1830–1831
Doerr CH, Gajic O, Berrios JC et al (2005) Hypercapnic acidosis impairs plasma membrane wound resealing in ventilator-injured lungs. Am J Respir Crit Care Med 171:1371–1377
Amato MB, Barbas CS, Medeiros DM et al (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Brower RG, Shanholtz CB, Fessler HE et al (1999) Prospective, randomized, controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. Crit Care Med 27:1492–1498
Stewart TE, Meade MO, Cook DJ et al (1998) Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. Pressure- and Volume-Limited Ventilatory Strategy Group. N Engl J Med 338:355–361
Schmidt M, Jaber S, Zogheib E et al (2018) Feasibility and safety of low-flow extracorporeal CO2 removal managed with a renal replacement platform to enhance lung-protective ventilation of patients with mild-to-moderate ARDS. Crit Care 22(1):122
Combes A, Fanelli V, Pham T et al (2019) Feasibility and safety of extracorporeal removal to enhance protective ventilation in acute respiratory distress syndrome: the SUPERNOVA study. Intensive Care Med. (Epub ahead of print).
Acknowledgements
Not applicable.
Funding
This article did not receive sponsorship for publication
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
About this supplement
This article has been published as part of the supplement Intensive Care Medicine Experimental Volume 7 Supplement 1 2019: Proceedings from the Third International Symposium on Acute Pulmonary Injury and Translational Research (INSPIRES III). The full contents of the supplement are available at https://icm-experimental.springeropen.com/articles/supplements/volume-7-supplement-1.
Author information
Authors and Affiliations
Contributions
All the authors have contributed equally to the elaboration of this article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Ongoing studies of ECCO2R in ARDS. (DOCX 16 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Morales-Quinteros, L., Camprubí-Rimblas, M., Bringué, J. et al. The role of hypercapnia in acute respiratory failure. ICMx 7 (Suppl 1), 39 (2019). https://doi.org/10.1186/s40635-019-0239-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-019-0239-0