Abstract
Purpose
We sought to determine the prevalence of and factors associated with acute cor pulmonale (ACP) and patent foramen ovale (PFO) at the early phase of acute respiratory distress syndrome (ARDS), and to assess their relation with mortality.
Methods
In this prospective multicenter study, 200 patients submitted to protective ventilation for early moderate to severe ARDS [PaO2/FIO2: 115 ± 39 with FIO2: 1; positive end-expiratory pressure (PEEP): 10.6 ± 3.1 cmH2O] underwent transthoracic (TTE) and transesophageal echocardiography (TEE) <48 h after admission. Echocardiograms were independently interpreted by two experts. Factors associated with ACP, PFO, and 28-day mortality were identified using multivariate regression analysis.
Results
TEE depicted ACP in 45/200 patients [22.5%; 95 % confidence interval (CI) 16.9–28.9 %], PFO in 31 patients (15.5 %; 95 % CI 10.8–21.3 %), and both ACP and PFO in 9 patients (4.5 %; 95 % CI 2.1–8.4 %). PFO shunting was small and intermittent in 27 patients, moderate and consistent in 4 patients, and large or extensive in no instances. PaCO2 >60 mmHg was strongly associated with ACP [odds ratio (OR) 3.70; 95 % CI 1.32–10.38; p = 0.01]. No factor was independently associated with PFO, with only a trend for age (OR 2.07; 95 % CI 0.91–4.72; p = 0.08). Twenty-eight-day mortality was 23 %. Plateau pressure (OR 1.15; 95 % CI 1.05–1.26; p < 0.01) and air leaks (OR 5.48; 95 % CI 1.30–22.99; p = 0.02), but neither ACP nor PFO, were independently associated with outcome.
Conclusions
TEE screening allowed identification of ACP in one-fourth of patients submitted to protective ventilation for early moderate to severe ARDS. PFO shunting was less frequent and never large or extensive. ACP and PFO were not related to outcome.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) is associated with injuries to the alveolar epithelium and microvascular endothelium which result in severe hypoxemia, decreased pulmonary compliance, and increased pulmonary vascular resistance [1, 2]. Acute pulmonary hypertension increases right ventricular (RV) afterload, which may be further increased by positive-pressure ventilation required to correct ARDS-induced hypoxemia [3, 4]. Acute cor pulmonale (ACP) is the most severe clinical presentation of acute RV failure secondary to an abrupt increase of RV afterload. Diagnosis of ACP currently relies on echocardiography when it depicts the conjunction of RV dilatation and paradoxical septal motion [5]. Pulmonary hypertension associated with ARDS may reverse the pressure gradient between the right and left atria, thereby facilitating shunting through a patent foramen ovale (PFO). PFO shunting may, in turn, contribute to the systemic hypoxemia and reduce the response to positive end-expiratory pressure (PEEP) [6]. The prevalence of ACP and PFO in ventilated ARDS patients have only been reported in single-center studies using transesophageal echocardiography (TEE). The frequency of ACP has been diversely reported, ranging from 22 to 61 % [6–8], and the diagnostic value of transthoracic echocardiography (TTE) has not yet been evaluated in this specific setting.
Using right-heart catheterization, Monchi et al. [9] showed long ago that RV systolic dysfunction was an independent predictive factor of mortality in ARDS patients, when ventilated without airway pressure limitation. These results were not confirmed in more recent studies using a protective ventilation strategy [7, 10]. Although ACP has been described as a prognostic factor in acute pulmonary embolism [11], its potential impact on outcome in patients sustaining ARDS has not yet been elucidated.
Accordingly, the present multicenter study was primarily conducted to determine the prevalence of ACP and PFO in ventilated patients with early ARDS when assessed using TEE during the 48 h following admission to the intensive care unit (ICU). Secondary objectives were: (1) to assess the feasibility and diagnostic ability of TTE in this specific setting, (2) to determine factors associated with the development of ACP and PFO, and (3) to assess the potential impact of ACP and PFO on outcome.
Patients and methods
Patients
Between November 2009 and June 2012, nine intensive care units (ICUs) participated in this prospective observational study. Consecutive patients were enrolled if they were older than 18 years and mechanically ventilated for ARDS as defined by the American–European consensus conference [12]. The presence of bilateral infiltrates was confirmed offline by an independent radiologist after centralized review of all digital chest radiographs performed at inclusion and on day 1. The oxygenation criterion was PaO2/FIO2 ≤ 200 using FIO2 of 1 and PEEP ≥ 5 cmH2O. The absence of elevated left atrial pressure was ascertained by the identification of lateral E/E′ <8 during the echocardiographic assessment systematically performed within the first 48 h after ICU admission [13]. Persistent ARDS was defined as persistence of all ARDS diagnostic criteria 24 h after study inclusion [14]. Exclusion criteria were contraindication to TEE performance [15], medical history of chronic respiratory insufficiency with oxygen therapy or noninvasive ventilation, or pregnancy. Patients were ventilated using current expert recommendations from the Société de Réanimation de Langue Française, and ventilator settings were optimized to maintain oxygen saturation between 88 and 96 % and plateau pressure ≤30 cmH2O [14]. Alveolar recruitment procedures, prone ventilation, administration of inhaled nitric oxide, and management of associated circulatory failure were left to the discretion of the attending physician, according to the standard of care of participating centers. In each patient, baseline characteristics were recorded on admission, vital parameters were obtained at time of TEE examination, and 28-day outcome was assessed. Air leaks corresponded to development of pneumothorax, pneumomediastinum, or subcutaneous emphysema attributed to mechanical ventilation. This observational study was approved by the Ethics Committee of the Société de Réanimation de Langue Française, which waived informed consent.
Echocardiography
TTE and TEE examinations were performed by intensivists experienced in critical care echocardiography, according to the standard of care of participating centers [16]. TEE studies were performed under sedation and neuromuscular blockers, when necessary. ACP was defined as the conjunction of a dilated RV in the long-axis view of the heart [end-diastolic RV area/end-diastolic left ventricular (LV) area >0.6] and an abnormal septal curvature at end systole (flattened interventricular septum or bulging towards LV cavity) with paradoxical motion (towards RV cavity) at the onset of systole in the short-axis view of the heart [5]. Diagnosis of PFO relied on identification of a right-to-left interatrial shunt during the contrast study, which consisted of intravenous injection of 10 mL agitated saline as a bolus. A positive contrast study corresponded to the presence of microcavitations in the left atrium (LA) within three cardiac cycles after the total opacification of the right atrium (RA) [17]. Three consecutive injections of microcavitations were performed in the TTE/TEE four-chamber view and in the TEE bicaval view. In the presence of PFO, a semiquantitative assessment of the associated anatomical shunt was graded as follows: “small” in the presence of a few LA macrocavitations, “moderate” in the presence of partial LA opacification, “large” in the presence of total LA opacification, and “extensive” in the presence of total LA opacification of intensity similar to the RA opacification [18]. The RV–RA systolic pressure gradient (ΔPmax) was conventionally obtained using Bernoulli’s equation, by measuring the maximal velocity of the tricuspid regurgitant jet when present and suitable for quantification: ΔPmax = 4 × V 2 [19]. Digital loops were recorded for centralized, offline, independent visual interpretation by two experts in critical care echocardiography. Adjudication of discrepant analyses for the diagnoses of ACP and PFO was secondarily performed jointly by the two experts. Specifically, the septal curvature and motion were reviewed frame by frame throughout the cardiac cycle for adjudication of ACP diagnoses.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) or median with interquartile range (IQR), and categorical variables are reported as number and percentage. The prevalence of ACP and PFO were also assessed using the recent definition of ARDS which was not available at the time of study design [20]. The sensitivity and specificity of TTE for diagnosis of ACP and PFO were determined conventionally using TEE as reference. Intergroup comparisons were performed using the Student t test, a χ 2 test or a Fisher exact test, when necessary. Independent factors associated with CPA and PFO, and predictors of 28-day mortality, were identified using a logistic regression model. All parameters with p value <0.20 on univariate analysis were included in the multivariate regression model. Continuous variables for which the assumption of linear relationship with the logit was not met were further dichotomized in the logistic regression models according to clinically relevant thresholds. Odds ratios (ORs) and their 95 % CIs were calculated. p-value <0.05 was considered statistically significant.
Results
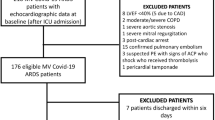
Among 204 consecutive patients eligible for the study (median: 9 patients/center; IQR: 4–17), 3 were secondarily excluded due to erroneous diagnosis of ARDS (interstitial pneumonia: n = 2) and diagnosis of atrial septal defect. Finally, 201 patients were studied [age 57 ± 15 years; 138 males; simplified acute physiology score (SAPS) II: 46 ± 17; sequential organ failure assessment (SOFA) score: 7.7 ± 3.5]; the echocardiographic study was not recorded in one patient (Fig. 1). Patients were admitted to the ICU predominantly for a medical disease (n = 186), and less frequently for scheduled (n = 4) or unplanned surgery (n = 5), or for trauma (n = 5). ARDS was primarily related to infective pneumonia (62 %), and mean PaO2/FIO2 was as low as 115 ± 39 under FIO2 of 1 and mean PEEP of 10.6 ± 3.1 cmH2O (Table 1). Eighty-three patients (41 %) had severe ARDS with PaO2/FIO2 ≤ 100, and 173 patients (89 %) had persistent ARDS 24 h after inclusion. Air leaks complicating mechanical ventilation was diagnosed in 11 patients (5.5 %). Median ICU stay was 14 days (IQR: 9–23 days), and 28-day mortality was 23 % (95 % CI 17–29 %).
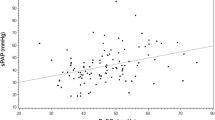
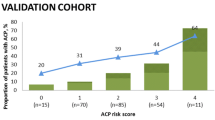
TEE provided good to excellent imaging quality in 173 patients (87 %) and was suitable for interpretation in all patients (n = 200). ACP was identified in 45 patients (22.5 %; 95 % CI 16.9–28.9 %) (figure, supplementary material), PFO in 31 patients (15.5 %; 95 % CI 10.8–21.3 %) (figure, supplementary material), and both in 9 patients (4.5 %; 95 % CI 2.1–8.4 %) (Fig. 1). The prevalence of TEE-diagnosed ACP and PFO tended to be higher in patients with severe ARDS when compared with those with moderate ARDS [20], the difference being not quite significant [22/83 (26.8 %) versus 23/118 (19.5 %), p = 0.22 and 17/83 (20.7 %) versus 14/118 (11.9 %), p = 0.09]. The prevalence of PFO depicted by TEE was similar whether patients had associated ACP or not (9/45 versus 22/155; p = 0.34). PFO shunting disclosed by TEE was small and intermittent in 27 patients (87.1 %; 95 % CI: 70.2–96.4 %) and moderate and consistent in 4 patients (12.9 %; 95 % CI 3.6–29.8 %). In no instance was the interatrial shunt large or extensive (Fig. 1). Microcavitations were injected through an internal jugular vein in 107 patients (54 %), a subclavian vein in 66 patients (33 %), and a femoral vein in the remaining 27 patients (13 %). Total RA opacification was obtained in 158 patients (79 %) during TEE contrast study. ΔPmax tended to be higher in the presence of ACP [35 ± 12 (n = 31) versus 31 ± 12 mmHg (n = 89); p = 0.13] and of PFO [36 ± 14 (n = 18) versus 31 ± 12 mmHg (n = 102); p = 0.11], the difference being not significant. In contrast, ΔPmax was significantly higher in patients with severe hypercapnia (PaCO2 ≥ 60 mmHg) [38 ± 11 (n = 11) versus 31 ± 12 mmHg (n = 106); p = 0.047] and correlated with the PaCO2 level (Pearson correlation coefficient: r = 0.33; p < 0.001).
TTE provided image quality adequate for identification of ACP in 123 patients (61 %), PFO in 90 patients (45 %), and both ACP and PFO in only 88 patients (44 %). ACP was identified in 19/123 patients (15.4 %; 95 % CI 9.6–23.1 %), PFO in 6/90 patients (6.7 %; 95 % CI 2.5–13.9 %), and both ACP and PFO in 3/88 patients (3.4 %; 95 % CI 0.7–9.6 %) (Fig. 1). Using TEE as reference, the sensitivity and specificity of TTE for the diagnoses of ACP and PFO were 60 % (95 % CI 41–77 %) and 99 % (95 % CI 94–100 %), and 36 % (95 % CI 13–65 %) and 99 % (95 % CI 93–100 %), respectively.
Patients with ACP had higher mean PaCO2, and tended to have greater plateau pressure and to be treated more frequently using alveolar recruitment maneuvers, inhaled NO, prone ventilation, and vasopressor support than those without ACP (Table 2). Patients with PFO were significantly older and had lower respiratory-system compliance than those without interatrial shunt (Table 2). The only independent factor associated with ACP was PaCO2 ≥60 mmHg (Table 3), and PaCO2 level was significantly associated with ACP (OR 1.03; 95 % CI 1.00–1.06; p = 0.04). No factor was independently associated with PFO, with only a trend for age (Table 3). When included in the multivariate analysis, ACP was not significantly associated with PFO (OR 1.36; 95 % CI 0.55–3.36; p = 0.51). Plateau pressure and air leaks were independently associated with 28-day mortality (Table 4). In contrast, presence of ACP (OR 1.11; 95 % CI 0.51–2.41; p = 0.79), PFO (OR 1.20; 95 % CI 0.50–2.90; p = 0.69), or both (OR 0.96; 95 % CI 0.19–4.76; p = 0.96) was not associated with outcome.
Discussion
In this cohort of patients with early moderate to severe ARDS persistent at 24 h, the prevalence of ACP and PFO identified by TEE reached 22.5 and 15.5 %, respectively. In keeping with our results, a recent 5-year single-center study reported a 22 % prevalence of ACP using TEE performed within the first 3 days after diagnosis of ARDS [6]. Similarly, Vieillard-Baron et al. [7] reported that the prevalence of ACP reached 25 % in a single-center cohort of 75 patients assessed over a 5-year period. Overall, these results convincingly confirm that approximately one-fourth of patients submitted to protective mechanical ventilation exhibit ACP during the early course of ARDS. In the 1980s, a prevalence of ACP as high as 61 % was reported in ARDS patients who were ventilated without airway pressure limitation [8]. ACP denotes acute dilatation secondary to excessive RV afterload [5]. Due to the relation between pulmonary vascular resistance and airway pressure [21], the level of targeted plateau pressure may substantially influence the development of ACP in ARDS patients. When analyzing echocardiographic findings obtained in ARDS patients during two consecutive time periods with distinct ventilatory strategies (1980–1992: liberal ventilation for normal PaCO2 level; 1993–2006: protective ventilation with airway pressure limitation), Jardin et al. [22] showed that the frequency of ACP significantly increased with the level of plateau pressure, the prevalence being maximal (42 %) when the plateau pressure exceeded 35 cmH2O and minimal (20 %) when it ranged between 18 and 26 cmH2O. In keeping with these results, mean plateau pressure tended to be higher in our patients with ACP despite protective ventilation than in patients without ACP. In the present study, the level of PaCO2 was the single independent factor associated with ACP, when considered as either a continuous or a binary variable. Vieillard-Baron et al. [7] reported the same result in a smaller population of ARDS patients submitted to protective ventilation, with a similar OR (1.15; 95 % CI 1.05–1.25; p = 0.0001). In the present study, ΔPmax, which indirectly reflects pulmonary vascular tone [23], was correlated with the level of PaCO2 and significantly higher in the subset of patients with severe hypercapnia (PaCO2 ≥60 mmHg). Hypercapnia has been shown to increase pulmonary vascular resistance [23], and to impair systolic function of afterloaded RV in both experimental [24] and clinical settings [25]. Interestingly, the detrimental effect of excessive afterload on RV function is maximized by the conjunction of hypercapnic acidosis [24]. This suggests a synergism which could be operant in ARDS patients under protective ventilation with resulting hypercapnia and associated ACP. TEE assessment of ARDS patients with relevant hypercapnia allows early identification of ACP and provides the best guide for ventilator settings and adjunct therapy [26]. In the absence of ACP, TEE helps determine, for a given range of plateau pressures, the level of tidal volume which avoids excessive RV afterloading while limiting detrimental hypercapnia [22].
The 15.5 % prevalence of PFO found in the present study is slightly lower than the prevalence previously reported (19.2 %) in a single-center study with the same sample size [6]. We injected the microcavitations through the superior vena cava in most of our patients (87 %), and the resulting RA opacification was partial in 21 % of cases. This may have resulted in underestimation of the prevalence of PFO and of the severity of the associated shunt. Gin et al. [27] advocated use of femoral vein contrast delivery to increase the sensitivity of echocardiography for diagnosis of PFO, since the inferior vena cava blood flow is anatomically directed towards the fossa ovalis [28]. This presumably accounts for the higher prevalence of PFO and larger interatrial shunts reported by Mekontso-Dessap et al. [6], since a substantial number of their patients were equipped with a femoral venous catheter. In addition, these authors used agitated colloids which generate smaller microcavitations and stronger contrast intensity in cardiac cavities [29]. These authors showed that patients with PFO had poor response to PEEP titration when compared with patients without interatrial shunt [6]. Since the interatrial shunt was moderate and consistent in only four of our patients, and large or extensive in no instance, PFO shunting presumably failed to contribute to their severe hypoxemia.
When compared with TEE, which is widely considered the reference imaging modality for diagnosis of ACP [30] and PFO [31, 32], TTE was inconclusive in a large proportion of our ventilated ARDS patients and lacked sensitivity. The presence of numerous interferences with image acquisition from the chest wall in ventilated ICU patients presumably explains these results [15]. Accordingly, TTE should not be routinely used for assessment of ARDS patients due to its poor diagnostic capacity for identification of ACP and PFO.
As previously suggested, neither ACP [7] nor PFO [6] was associated with 28-day mortality in our ARDS patients. In contrast, acute RV dysfunction, defined as RA pressure greater than pulmonary artery occlusion pressure, was shown to be strongly associated with mortality in a series of 259 ARDS patients monitored by right-heart catheter [9]. Interestingly, the median plateau pressure was markedly higher in those patients (31 cmH2O; IQR 27–38 cmH2O) than in our patients under protective ventilation (26 cmH2O; IQR 23–28 cmH2O). In addition, our patients diagnosed with ACP during early TEE assessment were presumably managed more aggressively, as reflected by the more frequent use of prone ventilation and inhaled NO known to reduce RV afterload [26, 33]. As suggested previously [7, 10], early identification and treatment of RV dysfunction presumably account for the absence of influence of ACP on mortality in the present study. The fairly high incidence of ACP in early moderate to severe ARDS, its apparent lack of prognostic value when taken into account in the therapeutic strategy [7, 10], and the potential role of ventilator settings in its development [3, 4, 22] suggest that all patients should be screened using TEE during the first 48 h following admission. Whether a contrast study should be routinely performed during TEE examination remains debatable, since we only found a 4 % incidence of moderate and consistent PFO shunting, and no instance of large or extensive shunt, in contrast to a recent study [6]. Despite the routine use of an airway pressure limitation strategy in our ARDS patients, plateau pressure and air leaks were the two independent factors associated with 28-day mortality.
The present study has several limitations. We did not use the Berlin definition of ARDS [20], but rather the definition of the American–European consensus conference [12], because of the time frame of our study. Nevertheless, we also presented our results using the Berlin diagnostic criteria and showed that ARDS was severe and persistent in a large proportion of our patients. The potential impact of PFO shunting on hypoxemia was not studied in our patients. Nevertheless, a relation between PFO and sustained severe hypoxemia is unlikely due to the large proportion of small and intermittent interatrial shunts. Whether the more aggressive management triggered by early TEE identification of ACP influenced the outcome of our ARDS patients cannot be addressed due to the study design. A selection bias cannot be fully excluded, since eligible patients with a contraindication to TEE were not systematically assessed using an alternative imaging technique (e.g., contrast-enhanced chest computed tomography for identification of ACP), and ACP was not excluded in moribund patients. Finally, TTE and TEE were not randomly and independently performed. The strengths of the current study are its multicenter design, the independent assessment of the primary criterion, and the sample size constituted of patients with early, moderate to severe, persistent ARDS.
Conclusions
In the present study, the prevalence of ACP and PFO in patients with moderate to severe ARDS submitted to protective ventilation and assessed using TEE during the first 48 h was 22.5 and 15.5 %, respectively. PFO shunting was predominantly small and intermittent, and large or extensive in no instance. TTE is not adequately suited for identification of ACP and PFO in ventilated ARDS patients due to its poor sensitivity. The level of PaCO2 was the only independent factor associated with ACP, whereas PFO tended to be associated with age. Despite the use of protective ventilation, plateau pressure and air leaks, but neither ACP nor PFO, were independently associated with 28-day mortality.
Key points
-
The prevalence of ACP and PFO in patients with moderate to severe ARDS submitted to protective ventilation was 22.5 and 15.5 %, respectively.
-
PFO shunting was predominantly small and intermittent (87.1 %).
-
TTE is not adequately suited for identification of ACP and PFO in ventilated ARDS patients due to its poor sensitivity.
-
The level of PaCO2 appeared as the only independent factor associated with ACP, while PFO tended to be associated with age.
-
Despite the use of protective ventilation, plateau pressure and air leaks, but neither ACP nor PFO, were independently associated with 28-day mortality.
References
Ware LB, Matthay MA (2000) The acute respiratory distress syndrome. New Engl J Med 342:1334–1349
Zapol W, Snider M (1977) Pulmonary hypertension in severe acute respiratory failure. N Engl J Med 296:476–480
Jardin F, Farcot JC, Boisante L, Curien N, Margairaz A, Bourdarias JP (1981) Influence of positive end-expiratory pressure on left ventricular performance. N Engl J Med 304:387–392
Jardin F, Delorme G, Hardy A, Auvert B, Beauchet A, Bourdarias JP (1990) Reevaluation of hemodynamic consequences of positive pressure ventilation: emphasis on cyclic right ventricular afterloading by mechanical lung inflation. Anesthesiology 72:966–970
Jardin F, Dubourg O, Bourdarias JP (1997) Echocardiographic pattern of acute cor pulmonale. Chest 111:209–217
Mekontso Dessap A, Boissier F, Leon R, Carreira S, Roche Campo F, Lemaire F, Brochard L (2010) Prevalence and prognosis of shunting across patent foramen ovale during acute respiratory distress syndrome. Crit Care Med 38:1786–1792
Vieillard-Baron A, Schmitt JM, Augarde R, Fellahi JL, Prin S, Page B, Beauchet A, Jardin F (2001) Acute cor pulmonale in acute respiratory distress syndrome submitted to protective ventilation: incidence, clinical implication, and prognosis. Crit Care Med 29:1551–1555
Jardin F, Gueret P, Dubourg O, Farcot JC, Margairaz A, Bourdarias JP (1985) Two-dimensional echocardiographic evaluation of right ventricular size and contractility in acute respiratory failure. Crit Care Med 13:952–956
Monchi M, Bellenfant F, Cariou A, Joly LM, Thebert D, Laurent I, Dhainaut JF, Brunet F (1998) Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med 158:1076–1081
Osman D, Monnet X, Castelain V, Anguel N, Warszawski J, Teboul JL, Richard C, For the French Pulmonary Artery Catheter Group (2009) Incidence and prognostic value of right ventricular failure in acute respiratory distress syndrome. Intensive Care Med 35:69–76
Konstantinides S, Geibel A, Kasper W, Olschewski M, Blümel L, Just H (1998) Patent foramen ovale is an important predictor of adverse outcome in patients with major pulmonary embolism. Circulation 97:1946–1951
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R, The Consensus Committee (1994) The American-European consensus conference of ARDS. Am J Respir Crit Care Med 149:818–824
Vignon P, AitHssain A, François B, Preux PM, Pichon N, Clavel M, Frat JP, Gastinne H (2008) Echocardiographic assessment of pulmonary artery occlusion pressure in ventilated patients: a transoesophageal study. Crit Care 12:R18
Richard JC, Girault C, Leteurtre S, Leclerc F et le groupe d’experts de la SRLF (2005) Prise en charge ventilatoire du syndrome de détresse respiratoire aiguë de l’adulte et de l’enfant (nouveau-né exclu). Recommandations d’experts de la Société de Réanimation de Langue Française. http://www.srlf.org/rc/org/srlf/htm/Article/2011/20110907-224245-640/src/htm_fullText/fr/2005_recommandations_d_experts_SRLF_prise_en_charge_ventilatoire_du%20SDRA_de%20l_adulte_et_de_l_enfant_%28nouveau_ne_exclus%29.pdf
Vignon P, Mayo P (2011) Echocardiography in the critically ill: an overview. In: De Backer D, Cholley BP, Slama M, Vieillard-Baron A, Vignon P (eds) Hemodynamic monitoring using echocardiography in the critically ill, 1st edn. Springer, Berlin, pp 1–9
Mayo P, Beaulieu Y, Doelken P, Feller-Kopman D, Harrod C, Kaplan A, Oropello J, Vieillard-Baron A, Axler O, Lichtenstein D, Maury E, Slama M, Vignon P (2009) American College of Chest Physicians/La Société de Réanimation de Langue Française statement on competence in critical care ultrasonography. Chest 135:1050–1060
Gin KG, Fenwick JC, Pollick C, Thompson CR (1993) The diagnostic utility of contrast echocardiography in patients with refractory hypoxemia. Am Heart J 125:1136–1141
Vedrinne JM, Duperret S, Bizollon T, Magnin C, Motin J, Trepo C, Ducerf C (1997) Comparison of transesophageal and transthoracic contrast echocardiography for detection of an intrapulmonary shunt in liver disease. Chest 111:1236–1240
Currie PJ, Seward JB, Chan K-L, Fyfe DA, Hagler DJ, Mair DD, Reeder GS, Nishimura RA, Tajik AJ (1985) Continuous wave Doppler estimation of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients. J Am Coll Cardiol 6:750–756
Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni L, Rhodes A, Slutsky AS, Vincent JL, Rubenfeld GD, Thompson BT, Ranieri VM (2012) The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med 38:1573–1582
Whittenberger J, Mc Gregor M, Berglund E, Borst HG (1960) Influence of state of inflation of the lung on pulmonary vascular resistance. J Appl Physiol 15:878–882
Jardin F, Vieillard-Baron A (2007) Is there a safe plateau pressure in ARDS? The right heart only knows. Intensive Care Med 33:444–447
Balanos GM, Talbot NP, Dorrington KL, Robins PA (2003) Human pulmonary resistance vascular response to 4 h of hypercapnia and hypocapnia measured using Doppler echocardiography. J Appl Physiol 94:1543–1551
Rose CE, Van Benthuysen K, Jackson JT, Tucker CE, Kaiser DL, Grover RF, Weil JV (1983) Right ventricular performance during increased afterload impaired by hypercapnic acidosis in conscious dogs. Circ Res 52:76–84
Mekontso-Dessap A, Charron C, Devaquet J, Aboab J, Jardin F, Brochard L, Vieillard-Baron A (2009) Impact of hypercapnia and augmented positive end-expiratory pressure on right ventricle function in severe acute respiratory distress syndrome. Intensive Care Med 35:1850–1858
Vieillard-Baron A, Charron C, Caille V, Belliard G, Page B, Jardin F (2007) Prone positioning unloads the right ventricle in severe ARDS. Chest 132:1440–1446
Gin KG, Huckell VF, Pollick C (1993) Femoral vein delivery of contrast medium enhances transthoracic echocardiographic detection of patent foramen ovale. J Am Coll Cardiol 22:1994–2000
Woods TD, Patel A (2006) A critical review of patent foramen ovale detection using saline contrast echocardiography: when bubbles lie. J Am Soc Echocardiogr 19:215–222
Beppu S, Tanabe K, Shimizu T, Ishikura F, Nakatani S, Terasawa A, Matsuda H, Miyatake K (1991) Contrast enhancement of Doppler signals by sonicated albumin for estimating right ventricular systolic pressure. Am J Cardiol 67:1148–1150
Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F (2002) Echo-Doppler demonstration of acute cor pulmonale at the bedside in the medical intensive care unit. Am J Respir Crit Care Med 166:1310–1319
Kerut EK, Norfleet WT, Plotnick GD, Giles TD (2001) Patent foramen ovale: a review of associated conditions and the impact of physiological size. J Am Coll Cardiol 38:613–623
Hara H, Virmani R, Ladich E, Mackey-Bojack S, Titus J, Reisman M, Gray W, Nakamura M, Mooney M, Poulose A, Schwartz RS (2005) Patent foramen ovale: current pathology, pathophysiology, and clinical status. J Am Coll Cardiol 46:1768–1776
Rossaint R, Falke KJ, Lopez F, Slama K, Pison U, Zapol WM (1993) Inhaled nitric oxide for the adult respiratory distress syndrome. N Engl J Med 328:399–405
Acknowledgments
We gratefully thank Isabelle Herafa and Paul Bourzeix for their invaluable help in the study. We are also indebted to Dr. Yves Roudaut and Dr. Vincent Hummel for their independent interpretation of chest radiographs. This work was supported by a bourse de recherche clinique de la Société de Réanimation de Langue Française (2008).
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Association des Réanimateurs du Centre-Ouest (ARCO) and Clinical Research in Intensive Care and Sepsis (CRICS) network.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2013_3017_MOESM1_ESM.mp4
Supplementary material 1 (MP4 482 kb) Loop 1. Transesophageal echocardiography in a ventilated patient with ARDS: four-chamber view of the heart disclosing an enlarged right ventricle
134_2013_3017_MOESM2_ESM.mp4
Supplementary material 2 (MP4 476 kb) Loop 2. Transesophageal echocardiography in a ventilated patient with ARDS: short-axis view of the heart disclosing an enlarged right ventricle associated with paradoxical septal motion. These two findings are consistent with acute cor pulmonale
Supplementary material 3 (MP4 745 kb) Loop 3. Transesophageal echocardiography in a ventilated patient with ARDS: bicaval view disclosing a patent foramen ovale during a contrast study. Note that microcavitations fully opacified the right atrium and rapidly entered the left atrium through the foramen ovale
List of investigators
List of investigators
Chartres:
Juliette Audibert, MD; Alexandre Conia, MD; Olivier Gontier, MD; Mouldi Hamrouni, MD; Pierre Kalfon, MD; Abdelkader Ouchenir, MD.
Limoges:
Pauline Champy, MD; Marc Clavel, MD; Caroline Etchecopar-Chevreuil, MD; Bruno François, MD; Nicolas Pichon, MD.
Orléans:
Dalila Benzekri-Lefevre, MD; Isabelle Runge, MD.
Poitiers:
Delphine Chatellier, MD; Anne Veinstein, MD.
Saint-Brieuc:
Nicolas Barbarot, MD.
Saint-Malo:
Vlad Botoc, MD.
Tours:
Emmanuelle Mercier, MD.
Rights and permissions
About this article
Cite this article
Lhéritier, G., Legras, A., Caille, A. et al. Prevalence and prognostic value of acute cor pulmonale and patent foramen ovale in ventilated patients with early acute respiratory distress syndrome: a multicenter study. Intensive Care Med 39, 1734–1742 (2013). https://doi.org/10.1007/s00134-013-3017-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3017-6