Abstract
Background
Rates of colonization and infection with multidrug-resistant (MDR) bacteria are increasing worldwide, in both acute care hospitals and long-term care facilities (LTCFs). Italy has one of the highest prevalence of MDR bacteria in European countries, especially with regard to methicillin-resistant Staphylococcus aureus (MRSA) and extended-spectrum β-lactamase (ESBL) or carbapenemase producing Enterobacteriaceae (CPE).
Method
Review of studies on colonization by MDR bacteria from Italian LTCFs, risk factors for colonization and molecular characteristics of surveillance and clinical isolates, compared with other European countries.
Results
High variability of MDR colonization has been reported within and especially between European countries. Only a few surveillance studies have been performed in Italian LTCFs; these show MRSA colonization prevalence of 7.8–38.7 % for residents and 5.2–7.0 % for staff members, ESBL prevalence of 49.0–64.0 % for residents and 5.2–14.5 % for staff and prevalence of CPE of 1.0–6.3 % for residents and 0.0–1.5 % for staff. In Italian LTCFs, as well as in other European countries, the most prevalent ESBLs from surveillance or clinical Escherichia coli isolates were found to be CTX-M-type enzymes, particularly CTX-M-15, expressed by the pandemic ST131 clonal group; this lineage also expresses carbapenemase genes of the bla VIM and bla KPC types. Various risk factors for colonization of residents by MDR bacteria were identified.
Conclusions
The limited data from Italian LTCFs confirms these settings as important reservoirs for MDR organisms, allowing important considerations regarding the infection risk by these organisms. Nevertheless, more extended and countrywide screening studies for MDR colonization in Italian LTCFs are required. To promote further studies of various microbiological aspects related to LTCFs, the Association of Italian Clinical Microbiologists (Associazione Microbiologi Clinici Italiani; AMCLI) in 2016 has set up a new Working Group for the Study of Infections in LTCFs (Gruppo di Lavoro per lo Studio delle Infezioni nelle Residenze Sanitarie Assistite e Strutture Territoriali assimilabili; GLISTer), consisting of Clinical Microbiologists represented by the authors of this review article.
Similar content being viewed by others
Background
As in other European countries the aging population in Italy represents an increasing public health priority. Long-term care facilities (LTCF), according to the definition used in this review article, are facilities (nursing homes, inpatient behavioral health facilities, and long-term chronic care hospitals) that help meet both the medical and non-medical needs of elderly people with a chronic illness or disability, involving various levels of medical care that require the expertise of skilled practitioners. The older, sicker residents cared for in LTCFs have a variety of risk factors for colonization and also for infection with multidrug-resistant (MDR) organisms, increasing their morbidity and mortality [1]. Antibiotics are among the most commonly prescribed classes of medications for LTCF residents, increasing the selection pressure for MDR bacteria [2]. Cross-transmission within these facilities is also promoted, owing to various factors such as permanent living in a confined environment, the difficulty of diagnosing infections that present atypically and because of the frequent cognitive impairment of residents, reducing the compliance with basic hygiene measures. For these and other reasons LTCFs are a potentially important reservoir for MDR organisms [1, 3].
The aim of this review is to summarize the colonization prevalence studies of LTCF residents and staff published from Italian LTCFs and to compare them with studies from other European countries. MDR bacteria considered in this review are methicillin-resistant Staphylococcus aureus (MRSA), vancomycin resistant enterococci (VRE), extended-spectrum β-lactamase (ESBL) and/or carbapenemase producing Enterobacteriaceae (CPE). Furthermore, the main bacterial genotypes and resistance genes circulating in Italian LTCFs are reviewed. Finally, major risk factors for colonization by MDR bacteria identified in Italian LTCFs, compared with other European countries, are discussed.
Literature search
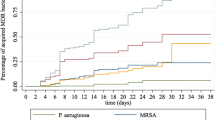
We adopted a search strategy in the Medline/Pubmed database including the following search terms: (nursing home* OR long term care facilit*) AND (colonization OR multi drug resistan* OR ESBL OR MRSA OR VRE OR carbapenemase*). We restricted the search to the date range 01.01.2000–30.08.2016 but did not impose any language restriction. Applying this search strategy we identified 641 articles and retrieved 14 full-text Italian and 68 full-text European non-Italian studies. Moreover, we included a poster referred to Italian LTCFs (reporting colonization prevalence and typing results), presented at the 26th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), in the reference list. Overall, we included 28 LTCF colonization studies from European non-Italian countries in the review; only 2 studies investigated carriage with CPE and 4 studies assessed the colonization by VRE, while 20 studies described MRSA carriage and 12 studies reported colonization by ESBL producers. Furthermore, we included 6 colonization studies from Italy, comprising 5 studies reporting MRSA, 4 studies describing ESBL, 3 studies investigating CPE and only 1 study referred to colonization by VRE. Eleven studies from the Medline/Pubmed search reported molecular characterization of Italian LTCF isolates (comprising one study reporting typing of MRSA); from the reference lists of the articles we retrieved two further Italian studies reporting molecular characterization data of isolates. Exclusion criteria for reviewing of colonization rates were studies that selected for clinical isolates or were referred to outbreak investigations, whereas similar studies were included in the analysis of resistance gene types and in typing of isolates; a structured review of the molecular characterization of isolates was done only for Italian LTCF isolates. At least two authors screened every abstract and full-text article and they discussed the results with all other authors before they were included in the review article.
Colonization of residents and staff by MDR bacteria in European LTCFs
Rates of colonization and infection with MDR bacteria are increasing worldwide, in both acute care hospitals and LTCFs [1–3]. Colonization rates by MRSA and ESBL producing Enterobacteriaceae in European LTCFs are summarized in Table 1; the surveys are quite heterogeneous in terms of facility sizes, resident characteristics and specimen types and therefore direct comparison between different studies is subject to bias. Nevertheless, high variability of colonization frequency for ESBL producing Enterobacteriaceae and MRSA, ranging from close to zero up to levels higher than 50 % can be derived from these studies; variability is high especially among countries but also among different LTCFs within single countries. Recently, the emergence and worldwide spread of CPE has generated an immediate infection threat to residents in LTCFs, but we found only two European colonization studies reporting low colonization prevalence; 0.0 % in a study from Ireland [4] and 0.3 % in a study from the Netherlands [5]. Colonization by VRE in European LTCF residents was found to be low, ranging from 0.0 % in Belgium [6], 0.4 % [7] and 2.7 % [8] in Germany, up to 3 % in Ireland [4]. LTCF staff colonization by MRSA in European LTCFs was found as high as 7.5 % in Ireland [9] and 0.0–5.2 % in Slovenia [10].
Italy has one of the highest prevalence of MDR bacteria isolated from blood cultures in European countries, especially with regard to MRSA and ESBL- or carbapenemase-producing Enterobacteriaceae [11] and residence in a LTCF is an independent risk factor for MDR blood stream infections [12]. In spite of the importance of LTCFs as reservoirs for MDR organisms, in Italian LTCFs only a few colonization studies have been performed during the last 10 years (Table 2). These surveys show MRSA colonization prevalence of 7.8–38.7 % for residents and 5.2–7.0 % for staff, ESBL prevalence of 49.0–64.0 % for residents and 5.2–14.5 % for staff, and CPE prevalence of 1.0–6.3 % for residents and 0.0–1.5 % for staff. Colonization by VRE is rare, with 2.7 % of residents found in one study [13].
All Italian and all except three European studies included in the review are point prevalence studies (Tables 1 and 2). Unfortunately, in many of these colonization studies, the only sample type for MRSA screening were nasal swabs, but by using exclusively this specimen type screening sensitivities of only 50–60 % are reached, with possible significant underestimation of the real colonization frequency; on the other hand the only use of rectal swabs for ESBL screening, as done in most of the colonization studies, permits still high sensitivity of 77–96 % [13, 14]. Screening for CPE in two of the three Italian colonization studies was done on chromogenic ESBL agar plates [13, 14]; this non-specific carbapenemase screening could have impacted on the sensitivity of the method. Finally, Italian colonization data refers mainly to a limited number of LTCFs, located in northern provinces of the country; because it is not appropriate to extrapolate data from Northern Italy to the central and southern part of the country, more extended and countrywide colonization studies are required.
Molecular characterization of MDR Enterobacteriaceae and MRSA from surveillance or clinical samples of Italian LTCFs
ESBL producing Escherichia coli isolates frequently belong to the pandemic clonal-group ST131 (mainly the H30-ST131 sub-clone) [15]; the association of this lineage with LTCFs has been widely documented [16]. In European LTCFs the clonal E. coli ST131 group frequently expresses ESBL genes belonging to various CTX-M-types (prevalently CTX-M-15) [4, 17–19]. Similarly, as shown in Table 3, in Italian LTCFs the most prevalent ESBLs in E. coli were found to be CTX-M-type enzymes (79–97 %), particularly CTX-M-15, and these E. coli mainly belonged to the ST131 clonal group [14, 20–22]; in a study of isolates from 12 LTCFs the H30-ST131 subclone strongly predominated (71 %) [23]. On the other hand, ESBLs in Klebsiella pneumoniae are mainly encoded by bla CTX-M or bla SHV-12 genes, whereas the ESBL phenotype of Proteus mirabilis and Morganella morganii isolates is generally due to production of the TEM-92 enzyme; high prevalence of the plasmidic AmpC-type enzyme CMY-16 was also found in P. mirabilis [14, 20, 22, 24, 25].
Sporadic or epidemic carbapenemase producing Enterobacteriaceae have been reported from European LTCF residents: K. pneumoniae expressing the carbapenemase OXA-48 from the Netherlands [5], E. coli and K. pneumoniae producing K. pneumoniae carbapenemase 2 (KPC-2) from Greece [26], K. pneumoniae producing KPC-3 from Portugal [27] and K. pneumoniae producing New Delhi metallo-β-lactamase-1 (NDM-1) from Poland [28]. The prevalent carbapenemase-types in enterobacterial isolates from Italian LTCFs are the Verona integron-encoded metallo-β-lactamase-1 (VIM-1) and various KPC types (Table 3). VIM-1 carbapenemases have been found to be expressed from various species of Enterobacteriaceae, isolated from acute-care hospitals and LTCFs in the Province of Bolzano [29, 30]; in this setting the bla VIM-1 gene is located on plasmids of various sizes, but with the same framework and all belonging to the incompatibility group IncN [31]. In Italian LTCFs VIM-1 enzymes have been found to be associated with E. coli belonging to the clonal group ST131 [14, 29]; subtyping of 2 isolates identified them as the subclone H30 ST131 [32]. Moreover, in a long-term care and rehabilitation facility in Milan an outbreak caused by an ST131 E. coli strain, associated with bla KPC-2 and bla KPC-8 genes located on plasmids belonging to the IncF group, has been identified [33]. KPC-producing Enterobacteriaceae are widely distributed in LTCFs of countries like the USA with high prevalence of this resistance phenotype [34]. KPC-producing K. pneumoniae are epidemically diffused in Italy, mostly belonging to the clonal complex 258 [35], yet in a study involving 489 residents from 12 LTCFs only 5 isolates were found to produce carbapenemases (1.0 % of residents colonized); of these isolates 3 K. pneumoniae harbored bla KPC-3 and 2 E. coli carried bla VIM-1 [23]. Further sporadic KPC-2 producing K. pneumoniae isolates from LTCF residents were found by other authors [36]. Finally, an outbreak of NDM-1 producing K. pneumoniae in a nursing home in Northern Italy has been identified [37].
Finally, the emergence of the transferable colistin resistance determinant mcr-1 has most recently been reported in commensal E. coli isolates from three Italian LTCFs [38].
MRSA isolates from an Italian LTCF were all negative for Panton-Valentine leukocidin (PVL) and belonged prevalently to ST8, spa t008, SCCmec IV [39]; this MRSA type is also prevalent in isolates from acute care hospitals in Northern Italy [40, 41]. In LTCF residents of other European countries various predominant MRSA types have been found: ST22, spa t022 or t032 (EMRSA-15) in the United Kingdom [42–44] and Ireland [9], the same MRSA type together with ST5, spa t003 (EMRSA-3) in Germany [45, 46], ST45, SCCmec IV in Belgium [47] and ST146, SCCmec IV in Spain [48]. Livestock-associated MRSA (LA-MRSA) genotypes belonging to CC398 have also sporadically been found in European LTCFs [49], whereas the isolation of PVL producing MRSA isolates has not yet been reported [9, 43, 44, 48].
Risk factors for colonization by MDR organisms of residents in Italian and other European LTCFs
Residents of LTCFs are uniquely vulnerable to colonization by MDR organisms and infection with these bacteria, because of the frequent and simultaneous presence of major risk factors [1, 50]; various of these risk factors have been found in screening studies in Italy and other European countries (Table 4). Particularly, the previous administration of antibiotics, especially fluoroquinolones and extended-spectrum cephalosporins, the presence of invasive medical devices, older age and the degree of dependence on nursing care, expressed as physical disability, are associated with colonization by MDR organisms. A striking feature is the high colonization of LTCF staff with MDR bacteria; this carriage probably reflects resident-to-staff, and, perhaps, staff-to-staff transmission [13]. LTCF residents frequently depend on continuous nursing care for daily living activities, with many occasions for horizontal transmission of MDR-organisms between residents and health care workers (resident-to-staff and staff-to-resident transmission). The length of stay in a LTCF is also a major risk factor, suggested by the higher colonization rates in LTCF residents compared with acute care hospital patients [13]. Moreover, the strict application of hospital hygiene measures in LTCFs is difficult because they are homes of the residents and therefore social interactions are encouraged. Previous hospitalization of LTCF residents is a further risk factor for colonization with MDR bacteria because patients can be admitted to the LTCF already colonized with MDR organisms acquired in the hospital [1]; surgical procedures and various chronic diseases and medications may increase the frequency of contact of LTCF residents with the health care system and facilitate the colonization and infection with MDR organisms. Interestingly, in a Dutch study authors found that the presence of MRSA carriers in the LTCFs more than doubled the likelihood of finding ESBL-producing E. coli [51]; this might be explained by similar transmission ways of these MDR organisms among LTCF residents. Finally, several further facility specific risk factors have been described, comprising lack of infection control policy, inadequate staffing and high staff turnover, increased number of residents per bedroom and the presence of limited facilities for hand washing [1].
Conclusions
LTCFs are important reservoirs for MDR organisms and colonization rates are similar or even higher than those found in acute care hospitals [13, 14], but the great variability in the number of residents and staff members and in the methods used for screening make it difficult to directly compare the results of various colonization studies. Nevertheless, colonization prevalence with MDR bacteria of LTCF residents has been found to be highly variable, reaching values as high as 37.6 % in France for MRSA [52] and as high as 55-75 % in Ireland for ESBL producing Enterobacteriaceae [4, 17]. In the few published surveillance studies in Italian LTCF residents similarly high ESBL colonization rates have been reported, whereas MRSA colonization was lower. Especially worrying is the emergence of carbapenemase producers in these facilities, expanding the reservoir of this health care threat. Colonization is frequently the prerequisite for infections [53]; this has many implications with regard to hospital hygiene measures and therefore reinforced infection control and surveillance programs are urgently needed, though their application in this specific setting is challenging [1]. Engaging of LTCFs in antimicrobial stewardship programs, frequently set up in acute care hospitals, is also a critical “hot topic”, focusing on drivers for antimicrobial over-use [2].
Data referred to baseline colonization by MDR bacteria in the Italian LTCF setting is not representative of the whole country and therefore the performance of proper countrywide screening studies is required; moreover, a standardized screening protocol is recommended. For this reason and to promote further studies of various microbiological aspects related to LTCFs, the Association of Italian Clinical Microbiologists (Associazione Microbiologi Clinici Italiani; AMCLI) in 2016 has set up a new Working Group for the Study of Infections in LTCFs (Gruppo di Lavoro per lo Studio delle Infezioni nelle Residenze Sanitarie Assistite e Strutture Territoriali assimilabili; GLISTer), consisting of Clinical Microbiologists represented by the authors of this review article. The mission of this group is also to support infection prevention and control initiatives in Italian LTCFs, with the aim to reduce the spread of MDR bacteria within and across acute and chronic health care facilities.
Abbreviations
- AMCLI:
-
Associazione Microbiologi Clinici Italiani
- AmpC:
-
Group of cephalosporinases
- Bla:
-
β-lactamase
- CC:
-
Clonal complex
- CMY:
-
Cephalosporinase type
- CPE:
-
Carbapenemase-producing Enterobacteriaceae
- CTX-M:
-
Cefotaximase-Munich, ESBL type
- ESBL:
-
Extended-spectrum β-lactamase
- GLISTer:
-
Gruppo di Lavoro per lo studio delle Infezioni nelle Residenze Sanitarie Assistite e Strutture Territoriali assimilabili
- Inc:
-
Incompatibility-group
- KPC:
-
Klebsiella pneumoniae carbapenemase
- LTCF:
-
Long-term care facility
- mcr:
-
Colistin resistance determinant
- MDR:
-
Multi-drug resistant
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- NDM-1:
-
New Delhi metallo-β-lactamase
- OXA-48:
-
Type of carbapenemase, OXA stays for oxacillinase
- PVL:
-
Panton-Valentine leukocidin
- SCCmec :
-
Staphylococcal chromosome cassette mec
- SHV:
-
β-lactamase type, SHV stays for sulfhydryl-variable
- spa :
-
Staphylococcal protein A type
- ST:
-
Sequence type
- TEM:
-
β-lactamase type, TEM stays for the Greek patient name “Temoneira”
- VIM:
-
Integron-encoded metallo-β-lactamase
- VRE:
-
Vancomycin-resistant enterococci
References
Moro ML, Gagliotti C. Antimicrobial resistance and stewardship in long-term care settings. Future Med. 2013;8:1011–25.
Dyar OJ, Pagani L, Pulcini C. Strategies and challenges of antimicrobial stewardship in long-term care facilities. Clin Microbiol Infect. 2015;21:10–9.
Cassone M, Mody L. Colonization with multi-drug resistant organisms in nursing homes: scope, importance, and management. Curr Geriatr Rep. 2015;4:87–95.
Ludden C, Cormican M, Vellinga A, Johnson JR, Austin B, Morris D. Colonisation with ESBL-producing and carbapenemase-producing Enterobacteriaceae, vancomycin-resistant enterococci, and meticillin-resistant Staphylococcus aureus in a long-term care facility over one year. BMC Infect Dis. 2015;15:168. doi:10.1186/s12879-015-0880-5.
Saegeman V, Van den Eynde J, Niclaes L, De Ridder D, Schuermans A, Glupczynski Y. Performance of different culture methods and of a commercial molecular assay for the detection of carbapenemase-producing Enterobacteriaceae in nursing homes and rehabilitation centers. Eur J Clin Microbiol Infect Dis. 2015;34:991–7.
Jans B, Schoevaerdts D, Huang TD, Berhin C, Latour K, Bogaerts P, et al. Epidemiology of multidrug-resistant microorganisms among nursing home residents in Belgium. PLoS One. 2013;8(5):e64908. doi:10.1371/journal.pone.0064908.
Hogardt M, Proba P, Mischler D, Cuny C, Kempf VA, Heudorf U. Current prevalence of multidrug-resistant organisms in long-term care facilities in the Rhine-Main district, Germany, 2013. Euro Surveill. 2015;2:20.
Heudorf U, Gustav C, Mischler D, Schulze J. Healthcare associated infections (HAI), antibiotic use and prevalence of multidrug-resistant bacteria (MDRO) in residents of long-term care facilities: the Frankfurt HALT plus MDRO project 2012. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2014;57:414–22.
Baldwin NS, Gilpin DF, Hughes CM, Kearney MP, Gardiner DA, Cardwell C, et al. Prevalence of methicillin-resistant Staphylococcus aureus colonization in residents and staff in nursing homes in Northern Ireland. J Am Geriatr Soc. 2009;57:620–6.
Cretnik TZ, Vovko P, Retelj M, Jutersek B, Harlander T, Kolman J, et al. Prevalence and nosocomial spread of methicillin-resistant Staphylococcus aureus in a long-term-care facility in Slovenia. Infect Control Hosp Epidemiol. 2005;26:184–90.
Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2014. http://ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-europe-2014.pdf
Venkatachalam I, Yang HL, Fisher D, Lye DC, Moi Lin L, Tambyah P, et al. Multidrug-resistant gram-negative bloodstream infections among residents of long-term care facilities. Infect Control Hosp Epidemiol. 2014;35:519–26.
March A, Aschbacher R, Dhanji H, Livermore DM, Böttcher A, Sleghel F, et al. Colonization of residents and staff of a long-term-care facility and adjacent acute-care hospital geriatric unit by multiresistant bacteria. Clin Microbiol Infect. 2010;16:934–44.
March A, Aschbacher R, Pagani E, Sleghel F, Soelva G, Hopkins KL, et al. Changes in colonization of residents and staff of a long-term care facility and an adjacent acute-care hospital geriatric unit by multidrug-resistant bacteria over a four-year period. Scand J Infect Dis. 2014;46:114–22.
Mathers AJ, Peirano G, Pitout JD. The role of epidemic resistance plasmids and international high-risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin Microbiol Rev. 2015;28:565–91.
Banerjee R, Johnston B, Lohse C, Porter SB, Clabots C, Johnson JR. Escherichia coli sequence type 131 is a dominant, antimicrobial-resistant clonal group associated with healthcare and elderly hosts. Infect Control Hosp Epidemiol. 2013;34:361–9.
Rooney PJ, O’Leary MC, Loughrey AC, McCalmont M, Smyth B, Donaghy P, et al. Nursing homes as a reservoir of extended-spectrum beta-lactamase (ESBL)-producing ciprofloxacin-resistant Escherichia coli. J Antimicrob Chemother. 2009;64:635–41.
Arvand M, Moser V, Pfeifer YJ. Prevalence of extended-spectrum-β-lactamase-producing Escherichia coli and spread of the epidemic clonal lineage ST131 in nursing homes in Hesse, Germany. J Antimicrob Chemother. 2013;68:2686–8.
Valenza G, Nickel S, Pfeifer Y, Pietsch M, Voigtländer E, Lehner-Reindl V, et al. Prevalence and genetic diversity of extended-spectrum β-lactamase (ESBL)-producing Escherichia coli in nursing homes in Bavaria, Germany. Vet Microbiol. 2015. doi:10.1016/j.vetmic.2015.10.008.
Tinelli M, Cataldo MA, Mantengoli E, Cadeddu C, Cunietti E, Luzzaro F, et al. Epidemiology and genetic characteristics of extended-spectrum β-lactamase-producing Gram-negative bacteria causing urinary tract infections in long-term care facilities. J Antimicrob Chemother. 2012;67:2982–7.
Nucleo E, Migliavacca R, Balzaretti M, Martino F, Spalla M, Terulla, et al. Spread of CTX-M-type ESβLs in isolates of E. coli from long-term care and rehabilitation facilities in Northern Italy. Microbiol Med. 2008;23:139–42.
Arnoldo L, Migliavacca R, Regattin L, Raglio A, Pagani L, Nucleo E, et al. Prevalence of urinary colonization by extended spectrum-beta-lactamase Enterobacteriaceae among catheterised inpatients in Italian long-term care facilities. BMC Infect Dis. 2013;13:124.
Giufrè M, Ricchizzi E, Accogli M, Barbanti F, Monaco M, Farina C, et al. Colonization by multidrug-resistant bacteria in long-term care facilities in Italy: a point-prevalence study. P1046, 26th ECCMID, Amsterdam, Netherlands 9–12 April 2016.
Migliavacca R, Nucleo E, D’Andrea MM, Spalla M, Giani T, Pagani L. Acquired AmpC type beta-lactamases: an emerging problem in Italian long-term care and rehabilitation facilities. New Microbiol. 2007;30:295–8.
Migliavacca R, Migliavacca A, Nucleo E, Ciaponi A, Spalla M, De Luca C, et al. Molecular epidemiology of ESβL producing P. mirabilis strains from a long-term care and rehabilitation facility in Italy. New Microbiol. 2007;30:362–6.
Mavroidi A, Miriagou V, Malli E, Stefos A, Dalekos GN, Tzouvelekis LS, et al. Emergence of Escherichia coli sequence type 410 (ST410) with KPC-2 β-lactamase. Int J Antimicrob Agents. 2012;39:247–50.
Rodrigues C, Bavlovič J, Machado E, Amorim J, Peixe L, Novais A. KPC-3-producing Klebsiella pneumoniae in Portugal linked to previously circulating non-CG258 lineages and uncommon genetic platforms (Tn4401d-IncFIA and Tn4401d-IncN). Front Microbiol. 2016;7:1000. doi:10.3389/fmicb.2016.01000. eCollection 2016.
Baraniak A, Izdebski R, Fiett J, Gawryszewska I, Bojarska K, Herda M, et al. NDM-producing Enterobacteriaceae in Poland, 2012–14: inter-regional outbreak of Klebsiella pneumoniae ST11 and sporadic cases. J Antimicrob Chemother. 2016;71:85–91.
Aschbacher R, Pagani L, Doumith M, Pike R, Woodford N, Spoladore G, et al. Metallo-β-lactamases among Enterobacteriaceae from routine samples in an Italian tertiary-care hospital and long-term care facilities during 2008. Clin Microbiol Infect. 2011;17:181–9.
Aschbacher R, Giani T, Corda D, Conte V, Arena F, Pasquetto V, et al. Carbapenemase-producing Enterobacteriaceae during 2011–12 in the Bolzano area (Northern Italy): increasing diversity in a low-endemicity setting. Diagn Microbiol Infect Dis. 2013;77:354–6.
Carattoli A, Aschbacher R, March A, Larcher C, Livermore DM, Woodford N. Complete nucleotide sequence of the IncN plasmid pKOX105 encoding VIM-1, QnrS1 and SHV-12 proteins in Enterobacteriaceae from Bolzano, Italy compared with IncN plasmids encoding KPC enzymes in the USA. J Antimicrob Chemother. 2010;65:2070–5.
Accogli M, Giani T, Monaco M, Giufrè M, García-Fernández A, Conte V, et al. Emergence of Escherichia coli ST131 sub-clone H30 producing VIM-1 and KPC-3 carbapenemases, Italy. J Antimicrob Chemother. 2014;69:2293–96.
Piazza A, Caltagirone M, Bitar I, Nucleo E, Spalla M, Fogato E, et al. Emergence of Escherichia coli sequence type 131 (ST131) and ST3948 with KPC-2, KPC-3 and KPC-8 carbapenemases from a long-term care and rehabilitation facility (LTCRF) in Northern Italy. Adv Exp Med Biol. 2016;901:77–89.
LaBombardi VJ, Urban CM, Kreiswirth BN, Chen L, Osorio G, Kopacz J, et al. Evaluation of Remel Spectra CRE agar for detection of carbapenem-resistant bacteria from rectal swabs obtained from residents of a long-term-care facility. J Clin Microbiol. 2015;53:2823–6.
Giani T, Pini B, Arena F, Conte V, Bracco S, Migliavacca R, et al. Epidemic diffusion of KPC carbapenemase-producing Klebsiella pneumoniae in Italy: results of the first countrywide survey, 15 May to 30 June 2011. Euro Surveill. 2013;18(22):20489.
Del Franco M, Paone L, Novati R, Giacomazzi CG, Bagattini M, Galotto C, et al. Molecular epidemiology of carbapenem resistant Enterobacteriaceae in Valle d’Aosta region, Italy, shows the emergence of KPC-2 producing Klebsiella pneumoniae clonal complex 101 (ST101 and ST1789). BMC Microbiol. 2015;15:260. doi:10.1186/s12866-015.
Gaibani P, Ambretti S, Berlingeri A, Cordovana M, Farruggia P, Panico M, et al. Outbreak of NDM-1-producing Enterobacteriaceae in northern Italy, July to August 2011. Euro Surveill. 2011;16(47):20027.
Giufrè M, Monaco M, Accogli M, Pantosti A, Cerquetti M, PAMURSA Study Group. Emergence of the colistin resistance mcr-1 determinant in commensal Escherichia coli from residents of long-term-care facilities in Italy. J Antimicrob Chemother. 2016;71:2329–31.
Monaco M, Bombana E, Trezzi L, Regattin L, Brusaferro S, Pantosti A, et al. Methicillin-resistant Staphylococcus aureus colonising residents and staff members in a nursing home in Northern Italy. J Hosp Infect. 2009;73:182–4.
Aschbacher R, Pichon B, Wootton M, Davies L, Binazzi R, Pike R, et al. Molecular epidemiology of methicillin-resistant Staphylococcus aureus from bacteraemia in northern Italy. Infez Med. 2012;20:256–64.
Gagliotti C, Monaco M, Sabia C, Gargiulo R, Sarti M, Sanchini A, et al. Staphylococcus aureus in a northern Italian region: phenotypic and molecular characterization. Scand J Infect Dis. 2012;44:24–8.
Barr B, Wilcox MH, Brady A, Parnell P, Darby B, Tompkins D. Prevalence of methicillin-resistant Staphylococcus aureus colonization among older residents of care homes in the United Kingdom. Infect Control Hosp Epidemiol. 2007;28:853–9.
Smith CS, Parnell P, Hodgson G, Darby B, Barr B, Tompkins D, et al. Are methicillin-resistant Staphylococcus aureus that produce Panton-Valentine leucocidin (PVL) found among residents of care homes? J Antimicrob Chemother. 2008;62:968–72.
Horner C, Parnell P, Hall D, Kearns A, Heritage J, Wilcox M. Methicillin-resistant Staphylococcus aureus in elderly residents of care homes: colonization rates and molecular epidemiology. J Hosp Infect. 2013;83:212–8.
Pfingsten-Würzburg S, Pieper DH, Bautsch W, Probst-Kepper M. Prevalence and molecular epidemiology of meticillin-resistant Staphylococcus aureus in nursing home residents in northern Germany. J Hosp Infect. 2011;78:108–12.
Nillius D, von Müller L, Wagenpfeil S, Klein R, Herrmann M. Methicillin-Resistant Staphylococcus aureus in Saarland, Germany: The Long-Term Care Facility Study. PLoS One. 2016;11(4):e0153030. doi:10.1371/journal.pone.0153030. eCollection 2016.
Denis O, Jans B, Deplano A, Nonhoff C, De Ryck R, Suetens C, et al. Epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) among residents of nursing homes in Belgium. J Antimicrob Chemother. 2009;64:1299–306.
Manzur A, Dominguez MA, Ruiz de Gopegui E, Mariscal D, Gavalda L, Segura F, et al. Natural history of methicillin-resistant Staphylococcus aureus colonisation among residents in community long term care facilities in Spain. J Hosp Infect. 2010;76:215–9.
Mossong J, Gelhausen E, Decruyenaere F, Devaux A, Perrin M, Even J, et al. Prevalence, risk factors and molecular epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) colonization in residents of long-term care facilities in Luxembourg, 2010. Epidemiol Infect. 2013;141:1199–206.
Esposito S, Leone S, Noviello S, Ianniello F, Fiore M. Antibiotic resistance in long-term care facilities. New Microbiol. 2007;30:326–31.
Verhoef L, Roukens M, de Greeff S, Meessen N, Natsch S, Stobberingh E. Carriage of antimicrobial-resistant commensal bacteria in Dutch long-term-care facilities. J Antimicrob Chemother. 2016;71:2586–92.
Eveillard M, Charru P, Rufat P, Hippeaux MC, Lancien E, Benselama F, et al. Methicillin-resistant Staphylococcus aureus carriage in a long-term care facility: hypothesis about selection and transmission. Age Ageing. 2008;37:294–9.
Moro ML, Ricchizzi E, Morsillo F, Marchi M, Puro V, Zotti CM, et al. Infections and antimicrobial resistance in long term care facilities: a national prevalence study. Ann Ig. 2013;25:109–18.
Andersson H, Lindholm C, Iversen A, Giske CG, Örtqvist Å, Kalin M, et al. Prevalence of antibiotic-resistant bacteria in residents of nursing homes in a Swedish municipality: healthcare staff knowledge of and adherence to principles of basic infection prevention. Scand J Infect Dis. 2012;44:641–9.
Jonsson K, Claesson BE, Hedelin H. Urine cultures from indwelling bladder catheters in nursing home patients: a point prevalence study in a Swedish county. Scand J Urol Nephrol. 2011;45:265–9.
Blom A, Ahl J, Månsson F, Resman F, Tham J. The prevalence of ESBL-producing Enterobacteriaceae in a nursing home setting compared with elderly living at home: a cross-sectional comparison. BMC Infect Dis. 2016;16:111. doi:10.1186/s12879-016-1430-5.
Greenland K, Rijnders MI, Mulders M, Haenen A, Spalburg E, van de Kassteele J, et al. Low prevalence of methicillin-resistant Staphylococcus aureus in Dutch nursing homes. J Am Geriatr Soc. 2011;59:768–9.
Cochard H, Aubier B, Quentin R, van der Mee-Marquet N, Réseau des Hygiénistes du Centre. Extended-spectrum β-lactamase-producing Enterobacteriaceae in French nursing homes: an association between high carriage rate among residents, environmental contamination, poor conformity with good hygiene practice, and putative resident-to-resident transmission. Infect Control Hosp Epidemiol. 2014;35:384–9.
Barrufet MP, Vendrell E, Force L, Sauca G, Rodríguez S, Martínez E, et al. Prevalence and risk factors for meticillin-resistant Staphylococcus aureus in an acute care hospital and long-term care facilities located in the same geographic area. Rev Esp Quimioter. 2014;27:190–5.
Manzur A, Gavalda L, Ruiz de Gopegui E, Mariscal D, Dominguez MA, Perez JL, et al. Prevalence of methicillin-resistant Staphylococcus aureus and factors associated with colonization among residents in community long-term-care facilities in Spain. Clin Microbiol Infect. 2008;14:867–72.
García-García JA, Santos-Morano J, Castro C, Bayoll-Serradilla E, Martín-Ponce ML, Vergara-López S, et al. Prevalence and risk factors of methicillin-resistant Staphylococcus aureus colonization among residents living in long-term care facilities in southern Spain. Enferm Infect Microbiol Clin. 2011;29:405–10.
Brugnaro P, Fedeli U, Pellizzer G, Buonfrate D, Rassu M, Boldrin C, et al. Clustering and risk factors of methicillin-resistant Staphylococcus aureus carriage in two Italian long-term care facilities. Infection. 2009;37:216–21.
Acknowledgement
Not applicable.
Funding
Funding of publication charge by the Associazione Microbiologi Clinici Italiani (AMCLI). AMCLI did not have any role in writing the manuscript.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Authors’ contribution
All authors contributed equally, read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Aschbacher, R., Pagani, E., Confalonieri, M. et al. Review on colonization of residents and staff in Italian long-term care facilities by multidrug-resistant bacteria compared with other European countries. Antimicrob Resist Infect Control 5, 33 (2016). https://doi.org/10.1186/s13756-016-0136-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-016-0136-1