Abstract
Shiga-toxigenic Escherichia coli (STEC) is incriminated in severe hemorrhagic enteritis in dogs, which is considered a veterinary and public health alarm. To investigate the prevalence, antimicrobial resistance patterns, virulence determinants, and distribution of antimicrobial resistance genes in STEC strains isolated from dogs: 80 fecal samples were obtained from diseased dogs suffering from hemorrhagic diarrhea from pet animal clinics in Ismailia governorate, Egypt. The obtained samples were examined bacteriologically. Moreover, the retrieved isolates were tested for serogrouping, Congo-red binding, antimicrobial resistance, and PCR-based determination of virulence and antimicrobial resistance genes. The prevalence of E. coli in the examined diseased dogs was 23.75% (19/80). The serogrouping of the recovered isolates revealed that 84.2% of the tested isolates were distributed into three serogroups: O146 (36.8%), O111 (31.5%), and O26 (15.7%). Meanwhile, three isolates were untypable (15.8%). Moreover, all the tested E. coli serovars were positive for CR-binding. PCR revealed that the prevalence of stx1, eaeA, hlyA, and stx2 virulence genes was 100%, 100%, 100%, and 47.3%, respectively. Our findings revealed that 31.5% of the recovered isolates showed MDR to five antimicrobial classes and harbored blaTEM, blaCTX-M, tetA, tetB, and sul1 genes. Alarmingly, three isolates were carbapenem-resistant. Two strains harbored the blaKPC gene, while one strain carried the blaNDM-1 gene. Concisely, as far as we know, this is the first study that reported the existence of MDR-STEC in dogs in Egypt. The stx1 gene is the most predominant Shiga toxin gene that accompanied the STEC isolated from hemorrhagic enteritis in dogs. The emerging MDR-STEC in dogs commonly harbors blaTEM, blaCTX-M, sul1, tetA, tetB, and qnrA resistance genes. Meropenem, levofloxacin, and tigecycline exhibited talented antimicrobial activity against MDR-STEC isolated from dogs.
Similar content being viewed by others
Introduction
Acute diarrhea in canine puppies is one of the most common and serious gastrointestinal problems, potentially leading to severe dehydration and death (Duijvestijn et al. 2016). Escherichia coli (E. coli) is found frequently in the gastrointestinal tract of both humans and animals as natural commensals (Cho et al. 2006). Based on the mechanism of disease occurrence, the pathogenic E. coli is classified into Enterohemorrhagic E. coli (EHEC), Enterotoxigenic E. coli (ETEC), Enteropathogenic E. coli (EPEC), Enteroaggregative E. coli (EAEC), and Enteroinvasive E. coli (Kaper et al. 2004). Moreover, regarding the virulence determinants, E. coli are divided into three main categories: 1-Commensals E. coli, 2-Intraintestinal-pathogenic E. coli, and 3-Extraintestinal-pathogenic E. coli (ExPEC). Each pathotype has specific virulence factors that play a major role in developing the disease, such as the production of toxins, hemolysins, siderophores, proteases, and adhesions (Pitout 2012).
Shiga toxigenic E. coli (STEC) is a common zoonotic diarrheagenic pathotype that can produce Shiga-toxins family (Stxs) cytotoxins (Melton-Celsa 2014). STEC possesses over 400 serotypes, some of which are associated with severe illnesses in animals and humans (Torres et al. 2018). The most predominant STEC serovars are O157:H7 and non-O157 serogroups (Such as O45, O121, O111, O26, O145, and O103) (Miko et al. 2014; Conrad et al. 2014). The emergence of STEC in dogs was reported with a prevalence ranging from 4 to 15.5% (Bentancor et al. 2007; Galarce 2019). The serotype O157: H7 is incriminated in most food-borne outbreaks in humans. In contrast, the non-O157 serovars are commonly associated with severe illness in animals (Rangel et al. 2005; Hedican et al. 2009).
The most important virulent determinants associated with STEC include 1-Shiga-toxins (stx1 and stx2) encoded by Shiga-toxins genes stx1 and stx2, respectively, 2-Intimin encoded by E. coli attaching and effacing gene (eae), and 3-Hemolysin that is necessary for STEC pathogenicity, especially hlyA (Puño-Salvadori et al. 2003; Puño-Sarmiento et al. 2013). The polymerase chain reaction is an accurate, sensitive, and consistent diagnostic assay used for bacterial identification and the determination of virulence determinants and antimicrobial resistance genes (Carvalho et al. 2021).
The multidrug resistance (MDR) patterns have increased worldwide, especially in the last decade. Several recent epidemiological studies have revealed the emergence of MDR bacterial pathogens from different origins that reflect a public health threat (Vega-Manriquez et al. 2020; Dazio et al. 2021). Multidrug resistance is common in E. coli and is primarily caused by the presence of antimicrobial resistance genes such as; blaTEM (responsible for penicillin-resistance), blaCTX-M (cephalosporins-resistance), tetA and tetB (tetracycline-resistance), qnrA, qnrB, and qnrS (Plasmid-mediated quinolone resistance), and sul1 (sulfonamide resistance). Although the emergence of carbapenem-resistant bacterial pathogens is low, it has increased recently worldwide. The carbapenem-resistance is mediated mainly by blaKPC and blaNDM-1 genes (Wedley et al. 2017; Peterhans et al. 2018; Alba et al. 2021).
The present study aimed to elucidate the clinical findings in naturally infected puppies with STEC. Also, to detect the rate, Cong-red binding, antimicrobial resistance patterns, virulence and antimicrobial resistance genes in STEC isolated from the examined puppies.
Materials and methods
Clinical examination and sampling
The clinical examination was conducted in small animal clinics in Ismailia province, Egypt, from March 2020 to June 2020. A total of 80 puppies (n = 80; 45 male and 35 female German Shepherd dogs) aged between 2 and 3 months old with an average weight of 5–10 kg were involved in the present study. The examined puppies suffered from bloody diarrhea. The clinical examination was performed according to the procedures described previously (Cote and Cohn 2019). Eighty fecal swabs were collected from the examined dogs under aseptic conditions into tryptic soy broth (Oxoid, UK), then transported to the microbiology laboratory as soon as possible for further bacteriological identification.
Isolation and identification of E. coli
The collected fecal swabs were inoculated in MacConkey broth (Difco, USA) and left incubated at 37 °C for 24 h. A loopful of the incubated broth was streaked on MacConkey agar and Eosin Methylene Blue agar (EMB) plates (Difco, USA) and left incubated at 37 °C for 24 h. The purified colonies were identified according to their cultural characteristics, Grams's staining, hemolysis on blood agar, motility test, and biochemical tests (lactose fermentation, oxidase, Voges-Proskauer, indole, methyl-red, citrate-utilization, catalase, urease, and H2S production) as previously described by MacFaddin (MacFaddin 1985).
Serogrouping of the retrieved isolates
The serogrouping of the recovered isolates was carried out at the Serology Division of the AHRI, Giza, Egypt, using the slide agglutination test for detection of O antigen, where polyvalent and specific monovalent E. coli antisera were involved (Mast Group Ltd.-Co., Merseyside, UK) (Starr 1986).
Congo-red binding test
To evaluate the in-vitro invasiveness and virulence of the retrieved isolates, the Congo-red binding assay was performed using tryptic soy agar (containing 0.03% Congo-red dye) (Difco, USA). The retrieved isolates were streaked on tryptic soy agar and left incubated at 37 °C for 24 h. The positive result is indicated by the appearance of red colonies, as previously reported by Panigrahy and Yushen (1990).
Antimicrobial susceptibility testing of E. coli
The in-vitro antimicrobial resistance patterns of the recovered isolates were determined on Mueller–Hinton agar (Oxoid, UK) using the disc diffusion method according to the procedures of (CLSI 2017). E. coli-ATCC 35218 was involved as a quality control strain. A blank disc impregnated with 30 μl of sterile distilled water was used as a negative control. The main concentration of bacteria was 1 × 108 CFU/mL, which is equivalent to the McFarland 0.5 Turbidity Standard. Moreover, twelve antimicrobial discs were tested include ceftazidime (CAZ) (30 μg), amikacin (AK) (30 μg), cefotaxime (CTX) (30 μg), tigecycline (TCG) (15 μg), trimethoprim-sulfamethoxazole (SXT) (25 μg), amoxicillin-clavulanic acid (AMC) (30 μg), tetracycline (TE) (30 μg), levofloxacin (LEV) (5 μg), aztreonam (ATM) (30 μg), amoxicillin (AMX) (30 μg), colistin sulfate (CT) (10 μg), and meropenem (MEM) (10 μg) (ThermoFisher Scientific, USA). The tested antimicrobial agents are the most commonly used antibiotics in Egypt in both the veterinary and health sectors. The examined isolates are categorized as MDR (MDR: resistant to ≥ one antibiotic in ≥ three antimicrobial classes) as previously described by Magiorakos et al. (2012).
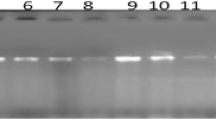
Screening of virulence and antimicrobial resistance genes using PCR
The bacterial DNA was extracted consistently with the manufacturer’s guidelines of the GenElute DNA Kit (Sigma Aldrich, USA). Briefly, the DNA Kit uses spin column technology. An optimized combination of mechanical and chemical lysis is used to disrupt bacterial cells subsequently, and carefully designed buffer chemistry promotes the binding of the released DNA to the silica membrane. Finally, the bacterial DNA is eluted from the column after washing away unwanted components. Nanodrop (Nanodrop 1000, Thermo Scientific, UK) was used to quantify genomic DNA templates, which were then adjusted to 100 ng l−1 and stored at − 20 °C until used for PCR. The PCR reactions were carried out in a volume of 25 μl (12.5 μl of Taq Green Master Mix 2X (Promega, Wisconsin, USA), one μl of each primer, 5 μl of DNA template, and PCR grade water up to 25 μL. Positive controls were involved in all reactions (E. coli strains previously isolated and kindly supported by the Animal Health Research Institute, Egypt). Besides, a reaction with no DNA template was used as a negative control. The oligonucleotide sequences (ThermoFisher Scientific, USA), specific amplicon size, and cycling conditions are shown in Table 1. Amplified PCR products were screened by 1.5% (w/v) agarose gel electrophoresis (Applichem GmbH, Darmstadt, Germany) for 45 min at 100 V in 1X TAE buffer (0.04 M Tris, 0.0001 M EDTA, pH 8.0), visualized using 15 µL of ethidium bromide (Sigma Aldrich, USA) and photographed under a UV transilluminator.
Statistical analyses
The Chi-square was carried out to analyze the resistance phenotype using the statistical analysis software (SAS, software version 9.4), and significance was determined at a p value < 0.05. The results of antimicrobial susceptibility testing were graphed by a heatmap through GraphPad Software (version 8.0.1, GraphPad Software Inc., La Jolla, CA, USA). A heatmap with hierarchical clustering was performed to visualize the overall distribution of virulence genes among recovered isolates using the “heatmap” package in R software (version 4.0.2; https://www.r-project.org/).
The association among various variables (resistance phenotypes and antimicrobial resistance genes) was carried out using Spearman correlations. The correlation coefficients and their p-values were visualized using a correlation plot.
The correlation analyses and visualization were done using the R packages rcorr: (https://hbiostat.org/R/Hmisc/), corrplot: (https://github.com/taiyun/corrplot/), and ggcorrplot: (https://github.com/taiyun/ggcorrplot/).
Results
Clinical manifestations of hemorrhagic diarrhea in the examined dogs
The prominent recorded clinical signs included anorexia, lethargy, depression, vomiting, foul-smelling bloody watery diarrhea, and severe dehydration manifested by retardation of skin turgor tests for up to 10 s. Besides, the affected dogs showed an elevation in body temperature (≥ 39.5 °C) that gradually decreased with the progression of the disease.
The phenotypic characteristics and the prevalence of E. coli in the examined dogs
Morphologically, the recovered isolates were moderate-sized Gram-negative, motile, and non-spore-forming bacilli. On MacCkoney agar, the obtained isolates were lactose fermenters (pink colonies). Moreover, the colonies were metallic sheen colonies on EMB and were hemolytic on Blood agar. Besides, all the retrieved isolates were negative for oxidase, H2S production, citrate-utilization, urease production, and Voges-Proskauer tests. Concurrently, they were positive for lactose fermentation, methyl-red, catalase, indole, and nitrate reduction tests. The prevalence of E. coli in the examined fecal swabs collected from diseased dogs was 23.75% (19/80).
E. coli serogrouping
The serogrouping of the recovered isolates revealed that 16 isolates (16/19, 84.2%) belonged to three O serogroups: O146 (7/19, 36.8%), O111 (6/19, 31.5%), and O26 (3/19, 15.8%). Furthermore, three isolates (3/19, 15.8%) were untypable. Statistically, there was no significant difference (p ˃ 0.05) in the frequency of the recovered E. coli serovars.
Congo-red binding assay
Our findings revealed that 84.2% of the tested isolates (16/19) were positive for Congo-red binding. All the examined E. coli serotypes were positive: O111 (6/19), O146 (7/19), and O26 (3/19). Moreover, the untyped isolates were negative for CR-binding (3/19).
Antimicrobial resistance profiles of the recovered E. coli
The antimicrobial susceptibility proved that the tested isolates showed remarkable resistance to trimethoprim-sulfamethoxazole, tetracycline, amoxicillin, amoxicillin-clavulanic acid, ceftazidime, cefotaxime, and colistin sulfate with a prevalence of 100%, 100%, 84.2%, 68.4%, 42.1%, 42.1%, and 42.1%, respectively. Moreover, the recovered isolates exhibited intermediate resistance to amikacin (68.4%). Besides, three isolates (15.8%) were resistant to meropenem (carbapenem-resistant). Our findings revealed that the retrieved isolates were sensitive to meropenem (78.94%), levofloxacin, and tigecycline (63.2% for each), as illustrated in Table 2 and Fig. 1. The statistical analysis revealed a significant difference in the susceptibility of the recovered strains to different involved antimicrobial agents (p < 0.001).
The correlation coefficient was determined among various tested antimicrobial agents. As illustrated in Fig. 2, significant positive correlations were observed between: TCG and ATM (r = 0.99); CAZ and CTX (r = 0.99); AMX, TE, and SXT (r = 0.98); LEV and CT (r = 0.96); AMC, TE, and SXT (r = 0.94); LEV and MEM (r = 0.88); AMX and AMC (r = 0.87).
Screening of virulence and antimicrobial resistance genes in the retrieved isolates (n = 19)
Using PCR, the recovered isolates possess the virulence genes; stx1, eaeA, hlyA, and stx2, with a prevalence of 100%, 100%, 100%, and 47.3%, respectively. Concerning the antimicrobial resistance genes, the recovered isolates possess blaTEM, blaCTX-M, tetA, tetB, sul1, qnrA, and qnrS resistance genes with a prevalence of 84.2%, 42.1%, 100%, 57.9%, 100%, 36.8%. 10.5%, respectively. Our findings revealed that tetA gene was detected in all tested E. coli strains either found alone or in combination with tetB gene (11/19, 57.9%). Furthermore, qnrA gene was detected in seven tested strains alone or combined with qnrS gene (2/19. 10.5%). Besides, qnrB gene was absent in all tested E. coli strains. Concerning carbapenem resistance genes, the blaKPC gene was found in two isolates (2/19, 10.5%), while blaNDM-1 (1/19, 5.26%) was found only in one isolate (Fig. 3).
Phenotypic multidrug-resistance profiles and the frequency of the antimicrobial resistance genes among the recovered isolates
In the present study, 84.2% (16/19) of the recovered isolates were recognized as multidrug-resistant (MDR: resistant to ≥ one antimicrobial agent in ≥ three different classes). Our findings revealed that 31.5% (6/19) of the recovered isolates showed MDR to 5 antimicrobial classes (sulfonamides: trimethoprim-sulfamethoxazole, tetracyclines: tetracycline, penicillins: amoxicillin and amoxicillin-clavulanic acid, cephalosporins: ceftazidime and cefotaxime, and polymyxins: colistin sulfate) and harbored blaTEM, blaCTX.-M, tetA, tetB, and sul genes.
Furthermore, 26.3% (5/19) of the recovered isolates expressed MDR to 4 different classes (tetracyclines: tetracycline, sulfonamides: trimethoprim-sulfamethoxazole, penicillins: amoxicillin and quinolones: levofloxacin) and harbored blaTEM, tetA, tetB, qnrA, and sul1 genes.
Besides, 10.5% (2/19) of the retrieved isolates displayed MDR to 7 different classes (tetracyclines: tetracycline, sulfonamides: trimethoprim-sulfamethoxazole, penicillins: amoxicillin carbapenems: meropenem, aminoglycoside: amikacin, cephalosporins: ceftazidime and cefotaxime, and polymyxins: colistin sulfate) and harbored blaTEM, blaCTX-M, blaKPC, tetA, and sul1 genes.
Moreover, 10.5% (2/19) of the recovered isolates expressed MDR to 4 different classes (tetracyclines: tetracycline, sulfonamides: trimethoprim-sulfamethoxazole, penicillins: amoxicillin and quinolones: levofloxacin) and harbored blaTEM, tetA, qnrA, qnrS, and sul1 genes. Furthermore, one strain displayed MDR to 5 antimicrobial classes (tetracyclines: tetracycline, sulfonamides: trimethoprim-sulfamethoxazole, penicillins: amoxicillin carbapenems: meropenem, and aminoglycosides: amikacin) and harbored blaTEM, blaNDM-1, tetA, and sul1 genes as illustrated in Table 3. Our findings revealed that three recovered E. coli strains were carbapenem-resistant. Two strains harbored the blaKPC gene, and one strain carried the blaNDM-1 gene.
The distribution of phenotypic resistance patterns, virulence, and antimicrobial resistance genes between the recovered E.coli serotypes (n = 19) is illustrated at the serovar level in Table 4 and Fig. 4.
The correlation analysis among the antimicrobial agents and the corresponding resistance genes revealed significant positive correlations between: sul1gene and SXT (r = 1); blaTEM gene and AMX (r = 1); blaCTX-M and CAZ (r = 1); tetA gene and TE (r = 1); qnrA gene and LEV (r = 1); blaKPC gene and MEM (r = 1); blaNDM-1 gene and MEM (r = 1); blaTEM gene and AMC (r = 0.87); blaCTX-M gene and CAZ (r = 0.87) tetB gene and TE (r = 0.71) as illustrated in Fig. 5.
Discussion
The current study was directed to investigate the rate, antimicrobial resistance patterns, screening of virulence and antimicrobial resistance genes in STEC isolated from dogs suffering from hemorrhagic diarrhea. The clinically examined diseased dogs suffered from fever, vomiting, dehydration, and foul-smelling bloody diarrhea. Our findings agreed with those reported by (Nayel et al. 2019). Bloody diarrhea is attributed mainly to the destruction of the epithelium of the intestinal crypts and subsequent villous atrophy (Unterer and Busch 2020). Moreover, dehydration was also a characteristic clinical sequel caused by losing fluids due to vomiting and diarrhea (Sykes and Greene 2013).
In the present study, the phenotypic characteristics of the recovered E. coli isolates are similar to those reported by (Sengupta et al. 2011). Besides, the prevalence of E. coli is nearly similar to that reported by a previous study in urban dogs in France (24.5%) (Haenni et al. 2014). Moreover, a lower prevalence was reported in Tunisia (17.5%) (Sallem et al. 2013). Furthermore, a higher prevalence of E. coli was reported in Brazil (31.3%) (Carvalho et al. 2016). These disparities are attributed mainly to geographical variation, differences in the hygienic conditions, and the time of investigations conduction (Carvalho et al. 2021). Regarding E. coli serogrouping, the retrieved serovars are similar to those reported by Jay-Russell et al. (2014). The determination of E. coli serotypes reflects epidemiological and public health importance. All the examined E. coli serotypes (O111, O146, and O26) were positive for Congo-red binding that emphasized the virulence and invasiveness of the tested serovars. Furthermore, all the non-typeable isolates were negative. These results are consistent with those reported by (Algammal et al. 2020b).
In the present work, the obtained isolates displayed a remarkable resistance to trimethoprim-sulfamethoxazole, tetracycline, amoxicillin, amoxicillin-clavulanic acid, ceftazidime, and cefotaxime, which is greatly threatening public health. Our findings agreed with those recorded by Jay-Russell et al. (2014) and Gupta et al. (2017). Recently, antimicrobial resistance has increased globally due to the widespread unregulated application of antimicrobial agents in the health and veterinary sectors and the dissemination of antibiotic-resistant genes carried on the bacterial chromosome or plasmid (Yamamoto et al. 2013).
In the present study, the PCR revealed that the stx1 gene is the most predominant virulence gene associated with STEC isolated from diseased dogs. Our findings emphasized the presence of the stx1 gene in combination with the eaeA and hlyA genes and/or the stx2 gene. On the other hand, a previous study reported that the stx2 gene was the most predominant virulence gene (23%) in STEC strains isolated from diarrheic dogs in the USA (Staats et al. 2003). The pathogenicity of Shiga toxin-producing E.coli is attributed mainly to a variety of virulence determinants, including 1-Shiga toxins (encoded by stx1 and stx2 genes), which regularly destruct the eukaryotic ribosomes and prevent protein-biosynthesis in the host, 2-Intimin (encoded by the eae gene) that is responsible for E. coli attachment to the intestinal mucosa, and 3-Hemolysin-A (plasmid gene EHEC-hlyA) is an exotoxin that lyses the erythrocytes in the intestinal mucosa (El-Baky et al. 2020). The virulence genes detected in E. coli of animal origin showed more toxin expression than those obtained from human strains (Keen and Elder 2002).
Regarding the multidrug resistance (MDR) profiles and the dissemination of antimicrobial resistance genes, our findings emphasized that most obtained isolates express MDR to 4 or more different antimicrobial classes and harbored sul1, tetA, tetB, blaTEM, blaCTX.M-1, and qnrA genes. The existence of MDR-E. coli reflects a public health alarm and suggests a poor prognosis of diseases induced by these isolates. Pet animals, especially dogs, are known as potential reservoirs of antimicrobial resistance. However, the available data are limited. The extensive application of antibiotics in both veterinary practice and the health sector predispose to the emergence of new superbugs. A recent study by Joosten et al. (2020) reported that 16% of the recovered E. coli isolates from dogs and cats from three European countries were recognized as multidrug-resistant strains (resistant to 6 antibiotics). One E. coli strain from Italy was resistant to 10 different antibiotics. Moreover, three E. coli strains (2 from Italy and one from Belgium) were multidrug-resistant to ampicillin, cefotaxime, and ceftazidime. The Extended-spectrum β-lactamases (ESBLs) are responsible for the hydrolysis of Broad-spectrum β-lactam antibiotics such as penicillins and cephalosporins. ESBLS are frequently detected in E. coli (Schultz et al. 2015). The high prevalence of the blaTEM and blaCTX-M genes among the retrieved E. coli strains enables them to resist penicillins and cephalosporins.
Tetracycline resistance is mainly attributed to tetracycline resistance genes. In the current study, the tetA gene was detected frequently in the recovered MDR E. coli strains, either alone or combined with the tetB gene. These findings agreed with a previous study performed on E. coli isolated from pigs in Spain (Jurado-Rabadán et al. 2014). Plasmid-mediated quinolone resistance (PMQR) was reported firstly in K. pneumoniae in the USA in 1998s. The qnrA gene codes for a 218 amino acid protein (QnrA protein) that prevents the binding of quinolones to DNA gyrase. Moreover, two other PMQR genes, including qnrB and qnrS genes, have been recognized to code for the same protein family and share 41% and 60% amino acid identity with QnrA, respectively (Robicsek et al. 2006). Alarmingly, in the present study, three E.coli strains were carbapenem-resistant. Worldwide, the existence of carbapenem-resistant strains is somewhat low; however, it has increased over time. The resistance to carbapenems is endorsed by blaKPC and blaNDM-1 resistance genes (Cole et al. 2020). Moreover, a lower resistance rate against amikacin was recorded in the current study. These findings agreed with those reported by Qekwana et al. (2018), who stated that the aminoglycoside resistance in E. coli strains isolated from urinary tract infections in dogs was relatively low (22%). This lower resistance rate could be attributed to the less frequent use of amikacin in treating bacterial infections in dogs in Egypt. The resistance mechanisms in E. coli include: a-A common resistance mechanism that occurs in antibiotics of the same class due to the expression of extended-spectrum β-lactamases or mutations in the penicillin-binding proteins, b-The repeated combined antimicrobial therapies, and c-The association between the antimicrobial resistance genes; this type exhibits a vital role in the occurrence of resistance to various antimicrobial agents (Algammal et al. 2020a, 2020b).
As far as the authors know, this is the first study that reported the existence of MDR-Shiga toxigenic E. coli (STEC) in dogs in Egypt. The stx1 gene is the most predominant Shiga toxin gene, found mainly in combination with the eaeA and hlyA genes and/or the stx2 gene. The emerging MDR-STEC in dogs commonly harbors blaTEM, blaCTX-M, sul1, tetA, tetB, and qnrA resistance genes. Meropenem, levofloxacin, and tigecycline exhibited talented antimicrobial activity against MDR-STEC isolated from dogs. The regular conduction of antimicrobial susceptibility testing is necessary to detect the most effective antibiotic and determine the emergence of new MDR strains. The emergence of virulent MDR-STEC strains comprises a vital threat to pet animals and human health, especially carbapenem-resistant strains harboring blaKPC or blaNDM-1 resistance genes.
Availability of data and materials
Not applicable.
References
Alba P, Taddei R, Cordaro G, Fontana MC, Toschi E, Gaibani P, Marani I, Angelo Giacomi A, Franco A (2021) Carbapenemase IncF-borne blaNDM-5 gene in the E. coli ST167 high-risk clone from canine clinical infection, Italy. Vet Microbiol 256:109045
Algammal AM, El-Kholy AW, Riad EM, Mohamed HE, Elhaig MM, Yousef SAA, Ghobashy MO (2020) Genes encoding the virulence and the antimicrobial resistance in enterotoxigenic and Shiga-toxigenic E. coli isolated from diarrheic calves. Toxins 12:383
Algammal AM, Hetta HF, Batiha GE, Hozzein WN, El Kazzaz WM, Hashem HR, El-Tarabili RM (2020b) Virulence-determinants and antibiotic-resistance genes of MDR-E. coli isolated from secondary infections following FMD-outbreak in cattle. Sci Rep 10:1–13
Archambault M, Petrov P, Hendriksen RS, Asseva G, Bangtrakulnonth A, Hasman H, Aarestrup FM (2006) Molecular characterization and occurrence of extended-spectrum β-lactamase resistance genes among Salmonella enterica serovar corvallis from Thailand, Bulgaria, and Denmark. Microb Drug Resist 12:192–198
Bentancor A, Rumi MV, Gentilini MV, Sardoy C, Irino K, Agostini A, Cataldi A (2007) Shiga toxin-producing and attaching and effacing Escherichia coli in cats and dogs in a high hemolytic uremic syndrome incidence region in Argentina. FEMS Microbiol Lett 267:251–256
Bisi-Johnson MA, Obi CL, Vasaikar SD, Baba KA, Hattori T (2011) Molecular basis of virulence in clinical isolates of Escherichia coli and Salmonella species from a tertiary hospital in the Eastern Cape, South Africa. Gut Pathog 3(1):1–8
Carvalho AC, Barbosa AV, Arais LR, Ribeiro PF, Carneiro VC, Cerqueira AMF (2016) Resistance patterns, ESBL genes, and genetic relatedness of Escherichia coli from dogs and owners. Braz J Microbiol 47:150–158
Carvalho I, Cunha R, Martins C, Martínez-Álvarez S, Safia Chenouf N, Pimenta P, Poeta P (2021) Antimicrobial resistance genes and diversity of clones among faecal ESBL-producing Escherichia coli isolated from healthy and sick dogs living in Portugal. Antibiotics 10:1013
Cattoir V, Poirel L, Rotimi V, Soussy CJ, Nordmann P (2007) Multiplex PCR for detection of plasmid-mediated quinolone resistance qnr genes in ESBL-producing enterobacterial isolates. J Antimicrob Chemother 60:394–397
Cho M, Lee Y, Choi W, Chung H, Yoon J (2006) Study on Fe (VI) species as a disinfectant: quantitative evaluation and modeling for inactivating Escherichia coli. Water Res 40:3580–3586
CLSI (2017) Clinical and Laboratory Standards Institute: Performance standards for antimicrobial susceptibility testing: 27th ed 424 informational; supplement. CLSI Doc. M100-S20.
Cole SD, Peak L, Tyson GH, Reimschuessel R, Ceric O, Rankin SC (2020) New Delhi Metallo-β-Lactamase-5-Producing Escherichia coli in Companion Animals. United States Emerging Infectious Diseases 26(2):381–383
Colom K, Pérez J, Alonso R, Fernández-Aranguiz A, Lariño E, Cisterna R (2003) Simple and reliable multiplex PCR assay for detection of blaTEM, blaSHV and blaOXA-1 genes in Enterobacteriaceae. FEMS Microbiol Lett 223:147–151
Conrad CC, Stanford K, McAllister TA, Thomas J, Reuter T (2014) Further development of sample preparation and detection methods for O157 and the top 6 non-O157 STEC serogroups in cattle feces. J Microbiol Methods 105:22–30
Cote E, Cohn L (2019) Cote’s Clinical Veterinary Advisor: Dogs and Cats - 4th Edition. https://www.elsevier.com/books/cotes-clinical-veterinary-advisor-dogs-and-cats/cohn/978-0-323-55451-0.
Dazio V, Nigg A, Schmidt JS, Brilhante M, Mauri N, Kuster SP, Schuller S (2021) Acquisition and carriage of multidrug-resistant organisms in dogs and cats presented to small animal practices and clinics in Switzerland. J Vet Intern Med 35:970–979
Dipineto L, Santaniello A, Fontanella M, Lagos K, Fioretti A, Menna LF (2006) Presence of Shiga toxin-producing Escherichia coli O157:H7 in living layer hens. Lett Appl Microbiol 43:293–295
Duijvestijn M, Mughini-Gras L, Schuurman N, Schijf W, Wagenaar JA, Egberink H (2016) Enteropathogen infections in canine puppies: (Co)-occurrence, clinical relevance and risk factors. Vet Microbiol 195:115–122
El-Baky RMA, Ibrahim RA, Mohamed DS, Ahmed EF, Hashem ZS (2020) Prevalence of virulence genes and their association with antimicrobial resistance among pathogenic E. coli isolated from Egyptian patients with different clinical infections. Infect Drug Resist 13:1221–1236
Galarce N (2019) Virulence Genes, Shiga Toxin Subtypes, Serogroups, and Clonal Relationship of Shiga Toxin-Producing Escherichia coli Strains Isolated from Livestock and Companion Animals. Animals 9:733
Gupta R, Eswar NKR, Modak JM, Madras G (2017) Effect of morphology of zinc oxide in ZnO-CdS-Ag ternary nanocomposite towards photocatalytic inactivation of E. coli under UV and visible light. Chem Eng J 307:966–980
Haenni M, Saras E, Métayer V, Médaille C, Madec JY (2014) High Prevalence of blaCTX-M-1/IncI1/ST3 and blaCMY-2/IncI1/ST2 Plasmids in Healthy Urban Dogs in France. Antimicrob Agents Chemother 58:5358
Hedican EB, Medus C, Besser JM, Juni BA, Koziol B, Taylor C, Smith KE (2009) Characteristics of O157 versus non-O157 Shiga toxin-producing Escherichia coli infections in Minnesota, 2000–2006. Clin Infect Dis 49:358–364
Ibekwe AM, Murinda SE, Graves AK (2011) Genetic Diversity and Antimicrobial Resistance of Escherichia coli from Human and Animal Sources Uncovers Multiple Resistances from Human Sources. PLoS One 6: e20819.
Jay-Russell MT, Hake AF, Bengson Y, Thiptara A, Nguyen T (2014) Prevalence and characterization of Escherichia coli and Salmonella strains isolated from stray dog and coyote feces in a major leafy greens production region at the United States-Mexico border. PLoS One 9.
Joosten P, Ceccarelli D, Odent E, Sarrazin S, Graveland H, Van Gompel L, Dewulf J (2020) Antimicrobial Usage and Resistance in Companion Animals: A Cross-Sectional Study in Three European Countries. Antibiotics 9:87
Jurado-Rabadán S, de la Fuente R, Ruiz-Santa-Quiteria JA, Orden JA, de Vries LE, Agersø Y (2014) Detection and linkage to mobile genetic elements of tetracycline resistance gene tet(M) in Escherichia coli isolates from pigs. BMC Vet Res 10:155
Kaper JB, Nataro JP, Mobley HLT (2004) Pathogenic Escherichia coli. Nat Rev Microbiol 2(2):123–140
Keen JE, Elder RO (2002) Isolation of Shiga-toxigenic Escherichia coli O157 from hide surfaces and the oral cavity of finished beef feedlot cattle. J Am Vet Med Assoc 220:756–763
MacFaddin JF (1985) Media for isolation-cultivation-identification-maintenance of medical bacteria.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Monnet DL (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281
Melton-Celsa AR (2014) Shiga Toxin (Stx) Classification, Structure, and Function. Microbiol Spectr 2(4):2–42
Miko A, Rivas M, Bentancor A, Delannoy S, Fach P, Beutin L (2014) Emerging types of Shiga toxin-producing E. coli (STEC) O178 present in cattle, deer, and humans from Argentina and Germany. Frontiers in cellular and infection microbiology 4: 78.
Nayel M, Zaghawa A, Abualkhier M (2019) Genetic and Molecular Typing of Canine Parvovirus Strains Circulating in Symptomatic Dogs in Egypt. J Curr Vet Res 1:75–85
Panigrahy B, Yushen L (1990) Differentiation of pathogenic and nonpathogenic Escherichia coli isolated from poultry. Avian Dis 34:941–943
Peterhans S, Stevens M, Nüesch-Inderbinen M, Schmitt S, Stephan R, Zurfluh K (2018) First report of a blaNDM-5-harbouring Escherichia coli ST167 isolated from a wound infection in a dog in Switzerland. J Glob Antimicrob Resist 15:226–227
Pitout J (2012) Extraintestinal Pathogenic Escherichia coli: A Combination of Virulence with Antibiotic Resistance. Front Microbiol 3:9
Piva IC, Pereira AL, Ferraz LR, Silva RS, Vieira AC, Blanco JE, Giugliano LG (2003) Virulence markers of enteroaggregative Escherichia coli isolated from children and adults with diarrhea in Brasília. Brazil J Clin Microbiol 41:1827–1832
Puño-Sarmiento J, Medeiros L, Chiconi C, Martins F, Pelayo J, Rocha S, Nakazato G (2013) Detection of diarrheagenic Escherichia coli strains isolated from dogs and cats in Brazil. Vet Microbiol 166:676–680
Qekwana DN, Phophi L, Naidoo V (2018) Antimicrobial resistance among Escherichia coli isolates from dogs presented with urinary tract infections at a veterinary teaching hospital in South Africa. BMC Vet Res 14:228
Randall LP (2004) Antibiotic resistance genes, integrons and multiple antibiotic resistance in thirty-five serotypes of Salmonella enterica isolated from humans and animals in the UK. J Antimicrob Chemother 53:208–216
Rangel JM, Sparling PH, Crowe C, Griffin PM, Swerdlow DL (2005) Epidemiology of Escherichia coli O157:H7 outbreaks, United States, 1982–2002. Emerg Infect Dis 11:603–609
Robicsek A, Jacoby GA, Hooper DC (2006) The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect Dis 6:629–640
Sallem RB, Gharsa H, Slama KB, Rojo-Bezares B, Estepa V, Porres-Osante N, Torres C (2013) First detection of CTX-M-1, CMY-2, and QnrB19 resistance mechanisms in fecal Escherichia coli isolates from healthy pets in Tunisia. Vector Borne Zoonotic Dis 13:98–102
Salvadori MR, Valadares GF, Leite DDS, Blanco J, Yano T (2003) Virulence factors of Escherichia coli isolated from calves with diarrhea in Brazil. Braz J Microbiol 34:230–235
Schultz E, Haenni M, Mereghetti L, Siebor E, Neuwirth C, Madec JY, Doublet B (2015) Survey of multidrug resistance integrative mobilizable elements SGI1 and PGI1 in Proteus mirabilis in humans and dogs in France, 2010–13. J Antimicrob Chemother 70:2543–2546
Sengupta R, Das R, Ganguly S, Mukhopadhayay S (2011) Survey on microbial quality of chicken meat in Kolkata, India. International Journal of Research in Pure and Applied Microbiology 1:32–33
Staats JJ, Chengappa MM, DeBey MC, Fickbohm B, Oberst RD (2003) Detection of Escherichia coli Shiga toxin (stx) and enterotoxin (estA and elt) genes in fecal samples from non-diarrheic and diarrheic greyhounds. Vet Microbiol 94(4):303–312
Starr MP (1986) Edwards and Ewing’s Identification of Enterobacteriaceae.: Fourth Edition. By William H. Ewing. Elsevier Science Publishing Co., Inc., New York. 1986. 536 pages. $65.00. ISBN 0–444–00981–7. Int. J. Syst. Bacteriol. 36:581–582.
Sykes JE, Greene CE (2013) Infectious Diseases of the Dog and Cat-E-Book, 4th edn. Elsevier Health Sciences, USA
Torres AG, Amaral MM, Bentancor L, Galli L, Goldstein J, Krüger A, Rojas-Lopez M (2018) Recent Advances in Shiga Toxin-Producing Escherichia coli Research in Latin America. Microorganisms 6:100
Unterer S, Busch K (2020) Acute Hemorrhagic Diarrhea Syndrome in Dogs. Veterinary Clinics Small Animal Practice 51(1):79–92
Vega-Manriquez XD, Ubiarco-López A, Verdugo-Rodríguez A, Hernandez-Chins U, Ahumada-Cota RE, Eslava CA (2020) Pet dogs potential transmitters of pathogenic Escherichia coli with resistance to antimicrobials. Arch Microbiol 202:1173–1179
Wedley AL, Dawson S, Maddox TW, Coyne KP, Pinchbeck GL, Clegg P, Nuttall T, Kirchner M, Williams NJ (2017) Carriage of antimicrobial resistant Escherichia coli in dogs: Prevalence, associated risk factors and molecular characteristics. Vet Microbiol 199:23–30
Xia Y, Liang Z, Su X, Xiong Y (2012) Characterization of carbapenemase genes in Enterobacteriaceae species exhibiting decreased susceptibility to carbapenems in a university hospital in Chongqing. China Ann Lab Med 32:270–275
Yamamoto S, Iwabuchi E, Hasegawa M, Esaki H, Muramatsu M, Hirayama N, Hirai K (2013) Prevalence and molecular epidemiological characterization of antimicrobial-resistant Escherichia coli isolates from Japanese black beef cattle. J Food Prot 76:394–404
Acknowledgements
Not applicable.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
AMA, AEM, and RME: conceptualization and study design. AMA, AEM, RME, and MEA: conducted the experiments. AMA, AEM, KJA, ASA, MME, and RME: drafted the manuscript. AMA, AEM, RME, KJA, ASA, MME, and MEA: carried out the statistical analysis, investigation, data validation, data accuracy, and supervision. AEM: performed the clinical examination of diseased cases and sampling. AMA: wrote and critically revised the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was performed in compliance with the ARRIVE guidelines. All protocols were conducted according to relevant guidelines and regulations. Handling of dogs and all protocols were approved by the Scientific Research Ethics Committee on animal research, Suez Canal University, Egypt (Approval number: 2021011).
Consent for publication
All authors gave their informed consent prior to their inclusion in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Algammal, A.M., El-Tarabili, R.M., Alfifi, K.J. et al. Virulence determinant and antimicrobial resistance traits of Emerging MDR Shiga toxigenic E. coli in diarrheic dogs. AMB Expr 12, 34 (2022). https://doi.org/10.1186/s13568-022-01371-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13568-022-01371-4