Abstract
Background
Cadmium zinc telluride (CZT) solid-state detectors have been recently introduced in the field of nuclear medicine in cardiology and breast imaging. The aim of the current study was to evaluate the performance of the novel detectors (CZT) compared to that of the routine NaI(Tl) in bone scintigraphy. A dual-headed CZT-based camera dedicated originally to breast imaging has been used, and in view of the limited size of the detectors, the hands were chosen as the organ for assessment. This is a clinical study.
Methods
Fifty-eight consecutive patients (total 116 hands) referred for bone scan for suspected hand pathology gave their informed consent to have two acquisitions, using the routine camera and the CZT-based camera. The latter was divided into full-dose full-acquisition time (FD CZT) and reduced-dose short-acquisition time (RD CZT) on CZT technology, so three image sets were available for analysis. Data analysis included comparing the detection of hot lesions and identification of the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints.
Results
A total of 69 hot lesions were detected on the CZT image sets; of these, 61 were identified as focal sites of uptake on NaI(Tl) data. On FD CZT data, 385 joints were identified compared to 168 on NaI(Tl) data (p < 0.001). There was no statistically significant difference in delineation of joints between FD and RD CZT data as the latter identified 383 joints.
Conclusions
Bone scintigraphy using a CZT-based gamma camera is associated with improved lesion detection and anatomic definition. The superior physical characteristics of this technique raised a potential reduction in administered dose and/or acquisition time without compromising image quality.
Similar content being viewed by others
Background
Gamma cameras are composed of semiconductor cadmium zinc telluride (CZT) detectors dedicated to cardiac perfusion studies and to molecular breast imaging (MBI). Cardiac CZT-based cameras were found to offer ultrafast myocardial perfusion imaging with better spatial resolution and count rate, thus allowing reduction of injected dose and/or acquisition time potentially overcoming the problems of motion artifacts and improved patient comfort [1–8]. Dual-headed CZT-based cameras dedicated to MBI have been shown to be valuable in detection of small lesions of clinical relevance [9–14]. The latter system has been installed in our facilities and is being used for detection of breast pathology. The detection of small breast lesions encouraged us to conduct the current study and assess the role of the CZT-based camera for detection of bone and joint pathology on 99mTc-methylene diphosphonate (MDP) bone scintigraphy. In view of the small size of the field of view, imaging of the hands was chosen as our model.
Methods
Patient population
The study cohort consisted of 116 hands of 58 consecutive patients, 30 male and 28 female, age 17–90 years (mean 42 ± 10), referred for 99mTc-MDP bone scintigraphy for suspected hand pathology. Indications for scintigraphy included trauma (n = 26), pain (n = 28), unclear lesions on radiography (n = 2), suspected reflex sympathetic dystrophy (RSD) (n = 1), and sarcoma (n = 1).
The study was approved by the ethical committee of the Tel Aviv Sourasky Medical Center.
Bone scintigraphy
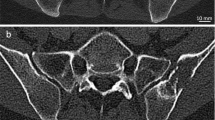
Two to three hours after the injection of 740 MBq 99mTc-MDP, data acquisition was performed using two separate systems: a routine gamma camera (Infinia or Optima, GE Healthcare) with a high-resolution collimator and a CZT-based camera (Discovery NM750b, GE Healthcare) originally aimed for breast imaging. Using the routine camera, the hands were placed on one of the camera heads for 10 min. For acquisition using the CZT-based camera, the hands were placed on the lower detector while the upper detector was used to immobilize the hands without pressure. Acquisition on the CZT-based camera was in dynamic mode, ten images of 1 min each. The combined data of all ten images reflect the full-dose full-acquisition time (full data, FD). A second set of images combining data of the first 4 min only (reduced data, RD) were generated reflecting the images obtained by a short (4 min) acquisition or simulating a reduced (296 MBq) injected dose. Thus, for each patient, three image sets of the hands were available for assessment: a set obtained by routine camera, FD, and RD data (Fig. 1).
A 74-year-old man with non-specific pain in the skeleton including the hands. From left to right: routine NaI(Tl) camera, full-dose (FD) CZT detector, and reduced-dose (RD) CZT detector image sets. Note the anatomic details of the bones (including the sesamoid bones) and joints on the CZT data, either FD or RD
Data analysis
Images were interpreted by two nuclear medicine experts (VK, HL) in consensus reading. The three data sets were reviewed at least 2 weeks apart, with the readers blinded to the patient’s name and clinical data. For assessment of lesion detection, any site of increased uptake was recorded. Interpretation of increased uptake was based on comparison with the contralateral bone or with the adjacent bone if both hands showed abnormality.
The criterion for assessment of image quality was the ability to visualize the location of the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints. Experts also commented on the ability to identify the joint space, i.e., to visualize the cold area representing the joint space separating the proximal and distal bones. On the CZT data of Fig. 2, for instance, the joint space of the MCP joint of the third finger is clearly seen while the location of the DIP joint of this finger can be identified but the joint space of this joint is not visualized. This figure also illustrates the ability to determine on the CZT data whether abnormality is present in the bone on both sides or only at one side of the joint space.
The ability to determine the joints’ location on the data sets was compared using the McNemar test with p < 0.05 considered statistically significant.
Results
Sixty-nine hot lesions were identified on CZT data whereas only 61 focal sites of increased uptake were recorded on NaI(Tl) images (no statistically significant difference) (Figs. 3 and 4).
A 71-year-old man with rheumatoid arthritis. On both image data, multiple joints appear to be associated with increased uptake. On the CZT data, uptake is located on both sides of the joint space (arrow) and the increased uptake at the metacarpophalangeal region of the index finger appears to be a sesamoid bone (arrowhead)
Table 1 summarizes the visualization of the MCP, PIP, and DIP joints by each of the three image sets. Of the 1624 joints present in the 116 evaluated hands, locations of 168 joints were identified using routine detectors compared to 385 joints when using FD CZT (sensitivity 0.1 compared to 0.24, p < 0.001, 95 % CI 0.145–0.186). No difference was found between FD and RD images as the latter identified 383 joints. Figures 3 and 4 demonstrate the better detection of the joints on the CZT data, identifying also whether increased uptake is present in the bone on both sides or only at one side of the articulation.
Discussion
Novel gamma cameras with CZT detectors have been recently introduced in the routine of nuclear medicine, and currently, there are systems dedicated to molecular breast imaging (MBI) and cardiac perfusion imaging. The novel geometric design and new detector material combined with new reconstruction algorithms have been shown in the literature to improve the diagnostic performance of gamma cameras in cardiac perfusion studies and scintimammography with superior image quality, shorter acquisition times, and reduced radiation exposure [1–14].
Bone scintigraphy is the most common procedure in nuclear medicine departments that plays an important role in the diagnosis of various skeletal disorders, including trauma, joint disease, infection, inflammation, and neoplastic conditions. The role of CZT detectors for bone scintigraphy has not been fully appreciated. As the CZT camera available in our facility is that composed of a 20 × 20 cm2 detection area tailored from breast imaging, we chose a small organ of interest, the hands, to explore the potential benefit of CZT detectors in bone scintigraphy. Bone scintigraphy is a common procedure for assessment of bone and joint pathology in the hand allowing the detection of posttraumatic changes, infection, inflammatory or degenerative changes, avascular necrosis, reflex sympathetic dystrophy, and neoplastic processes. Bone scintigraphy of the peripheral skeleton mainly of the small bones and joints of the hands burdens a potential suboptimal spatial resolution and poor anatomical definition often requiring a longer acquisition time, zoomed acquisition, and even change of collimators. Image quality may be even more deteriorated in patients with poor blood perfusion secondary to cardiovascular disease or peripheral vascular disease, who are overweight, or with renal and metabolic diseases resulting in a decreased tracer dose in the extremities. In children, the bones and joints composing the hands are of particular small size and there should be an ongoing effort to reduce administered dose and radiation exposure.
Evaluation of arthritis is an ongoing imaging challenge. Scintigraphy using 99mTc-MDP, labeled immunoglobulin G (IgG) gamma imaging, and 18F-FDG PET are used for joint imaging [15–20]. Improved image quality and visualization of the hand joints was achieved by using a positron emission mammography (PEM) scanner (arthro-PEM) [21]. The detection of active inflammation using non-specific tracers is primarily based on non-specific mechanisms such as hyperemia and increased vascular permeability. Recently, specific radiolabeled mAb including anti-CD20 and anti-TNF-α have been introduced for imaging of chronic inflammatory autoimmune joint diseases such as rheumatoid arthritis. In addition to evaluation of disease extent and severity, findings of immunoscintigraphy may assist in selection of patients that could benefit from immunotherapy and for monitoring response to therapy, maintaining the approach of personalized medicine [22–26]. The results of our study indicate that image quality reflected by visualization of joints is significantly improved with the CZT detectors compared to imaging using the routine NaI(Tl)-based camera, occasionally allowing to define whether the scintigraphic abnormality is one sided or present on both sides of the articulation. These results raise a potential improved performance of immunoscintigraphy of the joints using a CZT-based device. However, at present, the commercially available CZT systems are organ specific and/or small while imaging of joint diseases warrants imaging of larger joints and a whole-body approach.
In the current study, we did not find a significant difference neither in lesion detection nor in image quality between full-dose data and data that simulated reduced acquisition time or reduced injected dose. This is a major potential benefit of CZT detectors in the clinical practice of nuclear medicine.
There are several limitations to the study. First is the inherent lack of a gold standard for the final diagnosis of the abnormal scintigraphic findings. The other is the variable indications of bone scan of the hands and therefore the heterogeneous study cohort. This is however a pilot study, and its results encourage further evaluation of the role of CZT technology in specific indications of bone scan as well as scintigraphy using other tracers.
Conclusions
Bone scintigraphy with the novel CZT detectors is associated with improved image quality. Radiation dose and/or acquisition time can be considerably reduced without compromising lesion detection or image quality using this technology.
References
Herzog BA, Buechel RR, Katz R, Brueckner M, Husmann L, Burger IA, et al. Nuclear myocardial perfusion imaging with a cadmium-zinc-telluride detector technique: optimized protocol for scan time reduction. J Nucl Med. 2010;51(1):46–51.
Buechel RR, Herzog BA, Husmann L, Burger IA, Pazhenkottil AP, Treyer V, et al. Ultrafast nuclear myocardial perfusion imaging on a new gamma camera with semiconductor detector technique: first clinical validation. Eur J Nucl Med Mol Imaging. 2010;37(4):773–8.
Duvall WL, Croft LB, Ginsberg ES, Einstein AJ, Guma KA, George T, et al. Reduced isotope dose and imaging time with a high-efficiency CZT SPECT camera. J Nucl Cardiol. 2011;18(5):847–57.
Fiechter M, Ghadri JR, Kuest SM, Pazhenkottil AP, Wolfrum M, Nkoulou RN, et al. Nuclear myocardial perfusion imaging with a novel cadmium-zinc-telluride detector SPECT/CT device: first validation versus invasive coronary angiography. Eur J Nucl Med Mol Imaging. 2011;38(11):2025–30.
Mouden M, Timmer JR, Ottervanger JP, Reiffers S, Oostdijk AH, Knollema S, et al. Impact of a new ultrafast CZT SPECT camera for myocardial perfusion imaging: fewer equivocal results and lower radiation dose. Eur J Nucl Med Mol Imaging. 2012;39(6):1048–55.
Imbert L, Poussier S, Franken PR, Songy B, Verger A, Morel O, et al. Compared performance of high-sensitivity cameras dedicated to myocardial perfusion SPECT: a comprehensive analysis of phantom and human images. J Nucl Med. 2012;53(12):1897–903.
Oddstig J, Hedeer F, Jögi J, Carlsson M, Hindorf C, Engblom H. Reduced administered activity, reduced acquisition time, and preserved image quality for the new CZT camera. J Nucl Cardiol. 2013;20(1):38–44.
Jensen MM, Schmidt U, Huang C, Zerahn B. Gated tomographic radionuclide angiography using cadmium-zinc-telluride detector gamma camera; comparison to traditional gamma cameras. J Nucl Cardiol. 2014;21(2):384–96.
Mueller B, O’Connor MK, Blevis I, Rhodes DJ, Smith R, Collins DA, et al. Evaluation of a small cadmium zinc telluride detector for scintimammography. J Nucl Med. 2003;44(4):602–9.
Hruska CB, Phillips SW, Whaley DH, Rhodes DJ, O’Connor MK. Molecular breast imaging: use of a dual-head dedicated gamma camera to detect small breast tumors. AJR Am J Roentgenol. 2008;191(6):1805–15.
Rhodes DJ, Hruska CB, Phillips SW, Whaley DH, O’Connor MK. Dedicated dual-head gamma imaging for breast cancer screening in women with mammographically dense breasts. Radiology. 2011;258(1):106–1.
Hruska CB, Weinmann AL, O’Connor MK. Proof of concept for low-dose molecular breast imaging with a dual-head CZT gamma camera. Part I. Evaluation in phantoms. Med Phys. 2012;39(6):3466–75.
Hruska CB, Weinmann AL, Tello Skjerseth CM, Wagenaar EM, Conners AL, Tortorelli CL, et al. Proof of concept for low-dose molecular breast imaging with a dual-head CZT gamma camera. Part II. Evaluation in patients. Med Phys. 2012;39(6):3476–83.
Fowler AM. A molecular approach to breast imaging. J Nucl Med. 2014;55(2):177–80.
Duer A, Østergaard M, Hørslev-Petersen K, Vallø J. Magnetic resonance imaging and bone scintigraphy in the differential diagnosis of unclassified arthritis. Ann Rheum Dis. 2008;67(1):48–51. Epub 2007 Feb 8.
Kim JH, Kim YK, Kim SG, Yun PY, Kim JD, Min JH. Effectiveness of bone scans in the diagnosis of osteoarthritis of the temporomandibular joint. Dentomaxillofac Radiol. 2012;41(3):224–9.
Elzinga EH, van der Laken CJ, Comans EF, Lammertsma AA, Dijkmans BA, Voskuyl AE. 2-Deoxy-2-[F-18]fluoro-D-glucose joint uptake on positron emission tomography images: rheumatoid arthritis versus osteoarthritis. Mol Imaging Biol. 2007;9(6):357–60.
Guermazi A, Hayashi D, Eckstein F, Hunter DJ, Duryea J, Roemer FW. Imaging of osteoarthritis. Rheum Dis Clin North Am. 2013;39(1):67–105.
Rosado-de-Castro PH, Lopes de Souza SA, Alexandre D, Barbosa da Fonseca LM, Gutfilen B. Rheumatoid arthritis: nuclear medicine state-of-the-art imaging. World J Orthop. 2014;5(3):312–8.
Chopra A. 99mTc-labeled anti-tumor necrosis factor-alpha monoclonal antibody. Molecular Imaging and Contrast Agent Database (MICAD), National Center for Biotechnology Information (US); 2004–2013. 2007 Sep 25 [updated 2007 Oct 22].
Mhlanga JC, Carrino JA, Lodge M, Wang H, Wahl RL. 18F-FDG PET of the hands with a dedicated high-resolution PEM system (arthro-PET): correlation with PET/CT, radiography and clinical parameters. Eur J Nucl Med Mol Imaging. 2014;41:2337–45.
Conti F, Priori R, Chimenti MS, Coari G, Annovazzi A, Valesini G, et al. Successful treatment with intraarticular infliximab for resistant knee monoarthritis in a patient with spondyloarthropathy: a role for scintigraphy with 99mTc-infliximab. Arthritis Rheum. 2005;52(4):1224–6.
Chianelli M, D’Alessandria C, Conti F, Priori R, Valesini G, Annovazzi A, et al. New radiopharmaceuticals for imaging rheumatoid arthritis. Q J Nucl Med Mol Imaging. 2006;50:217–25.
Malviya G, Conti F, Chianelli M, Scopinaro F, Dierckx RA, Signore A. Molecular imaging of rheumatoid arthritis by radiolabelled monoclonal antibodies: new imaging strategies to guide molecular therapies. Eur J Nucl Med Mol Imaging. 2010;37(2):386–98.
Roimicher L, Lopes FP, de Souza SA, Mendes LF, Domingues RC, da Fonseca LM, et al. (99m)Tc-anti-TNF-α scintigraphy in RA: a comparison pilot study with MRI and clinical examination. Rheumatology. 2011;50:2044–50.
Malviya G, Anzola KL, Podestà E, Laganà B, Del Mastro C, Dierckx RA, et al. (99m)Tc-labeled rituximab for imaging B lymphocyte infiltration in inflammatory autoimmune disease patients. Mol Imaging Biol. 2012;14:637–46.
Acknowledgements
The authors wish to thank Mr. Rabia Abdelhai for his technical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None of the authors have competing interests.
Authors’ contributions
VK review of the three sets of images, summarizing the data and writing the manuscript. HL review of three sets of images images and summarizing the data. MK preparation of figures and participation in summarizing the data. EES design of the study, statistical analysis and revision of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Koulikov, V., Lerman, H., Kesler, M. et al. 99mTc-MDP bone scintigraphy of the hand: comparing the use of novel cadmium zinc telluride (CZT) and routine NaI(Tl) detectors. EJNMMI Res 5, 63 (2015). https://doi.org/10.1186/s13550-015-0139-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13550-015-0139-6