Abstract
According to the 2008 World Health Organization classification, chronic neutrophilic leukemia, chronic myelomonocytic leukemia and atypical chronic myeloid leukemia are rare diseases. The remarkable progress in our understanding of the molecular genetics of myeloproliferative neoplasms and myelodysplastic/myeloproliferative neoplasms has made it clear that there are some specific genetic abnormalities in these 3 rare diseases. At the same time, there is considerable overlap among these disorders at the molecular level. The various combinations of genetic abnormalities indicate a multi-step pathogenesis, which likely contributes to the marked clinical heterogeneity of these disorders. This review focuses on the current knowledge and challenges related to the molecular pathogenesis of chronic neutrophilic leukemia, chronic myelomonocytic leukemia and atypical chronic myeloid leukemia and relationships between molecular findings, clinical features and prognosis.
Similar content being viewed by others
Introduction
Chronic neutrophilic leukemia (CNL), chronic myelomonocytic leukemia (CMML) and atypical chronic myeloid leukemia (CML) are rare diseases categorized into the 2008 World Health Organization (WHO) as either myeloproliferative neoplasms (MPN; CNL) or myelodysplastic/myeloproliferative neoplasms (MDS/MPN; CMML and a CML). These diseases share several characteristics including an enlarged liver and spleen, an increased WBC and a hyper-cellular bone marrow. They are distinguished from each other based on numbers and types of leukemia cells in the blood, appearance of leukemia cells in the blood and bone marrow cells and cytogenetic and molecular abnormalities including absence of t(9:22) and BCR/ABL1 and rearrangement of platelet-derived growth factor receptor, alpha polypeptide (PDGFRA), platelet-derived growth factor receptor, beta polypeptide (PDGFRB) or fibroblast growth factor receptor 1 (FGFR1). Previously, it was sometimes difficult to distinguish these disease from each other and from other MPNs including chronic myeloid leukemia (CML), polycythaemia vera (PV), essential thrombocythaemia (ET) and primary myelofibrosis (PMF) which have different molecular abnormalities including mutations in Janus kinase 2 (JAK2), calreticulin (CALR) and MPL proto-oncogene, thrombopoietin receptor (MPL). Molecular characterization of CNL, CMML and atypical CML has advanced even further with the use of next generation sequencing. Important genetic abnormalities have been identified which help to distinguish between these diseases. This review focuses on the current knowledge and challenges related to the molecular pathogenesis of CNL, CMML and atypical CML and relationships between molecular findings, clinical features and prognosis.
Molecular genetics of CNL
Colony stimulating factor 3 receptor (CSF3R) mutations
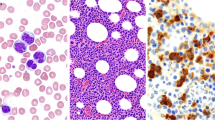
In 2013, Maxson et al. reported frequent mutations in CSF3R in patients with CNL and atypical CML [1]. Such mutations are rare in patients with AML. Two types of mutations were found. CSF3RT618I and CSF3RT615A are most common mutations, which are in the membrane proximal region which mediates proliferative and survival signals. These mutations occur alone or with another nonsense mutations truncating the cytoplasmic tail of the coding region important in transduction of maturation and suppression of proliferation [1],[2]. Membrane proximal mutations result in activation of JAK signaling pathways and truncation mutations in preferential activation of SRC family–TNK2 kinase signaling (Figure 1A) [1]. The aetiological role of CSF3RT618I mutation in these diseases was studied in a model in which mice transplanted with CSF3RT618I–expressing hematopoietic cells. These mice developed a CNL-like phenotype characterized by hyper-cellular bone marrow and granulocyte infiltrates in the spleen and liver and died [3].
Pardanani et al.[4] sequenced the implicated exons of CSF3R in 35 suspected subjects with CNL, 12 subjects with confirmed CNL and 6 subjects with CNL and a monoclonal gammopathy or lymphoid neoplasm. All subjects who fulfilled the 2008 WHO criteria for CNL had a CSF3R proximal membrane mutation, most frequently CSF3RT618I. One subject had CSF3RM696T and 1, CSF3RI598I. One of these subjects also had a truncating CSF3R mutation. No one with WHO-defined CNL but with a monoclonal gammopathy or lymphoid neoplasm had a CSF3R mutation. These data explain the different bases and prognoses between CNL with and without a monoclonal gammopathy [5]-[8]. Our study in Chinese with WHO-defined CNL confirmed these findings [9]. We found a CSF3RT618I mutation in all subjects with CNL without a monoclonal gammopathy but not in 2 subjects with features of CNL with a monoclonal gammopathy. These data indicate CSF3R mutations are a highly sensitive and specific molecular marker for WHO-defined CNL and we suggest it be included into the revised criteria.
JAK2 V617F
JAK2 V617F is common in patients with BCR/ABL1 negative MPNs and is rare in patients with CML but not in those with lymphoid neoplasms, reactive myelo-proliferative disorders or normals [10],[11]. About 13 patients with CNL with JAK2 V617F are reported [12]-[20]. These patients had typical features of CNL without the erythrocytosis, thrombocytosis and bone marrow fibrosis typical of PV, ET and PMF, but CSF3R mutations were not tested. Other recent studies report no JAK2 V617F in patients with CNL with CSF3R mutations [4],[9]. Also controversial is whether patients with CNL and JAK2 V617F have a different prognosis than patients with CNL without JAK2 V617F. Some data suggest CNL with JAK2V617F mutation has an indolent course with long intervals of stable disease on hydroxyurea [12]. Other data suggest person with CNL and JAK2V617F have a worse prognosis and a high risk of transformation to AML [13],[14]. The underlying issue, of course, is whether the current WHO-criteria are sufficient to accurately diagnose CNL. Do patients with seeming CNL but with JAK2V617F rather than a CSF3R mutation really have CNL or a different disorder not currently recognized in the WHO-criteria. This distinction is arbitrary but we favor reserving the CNL-designation in future revisions of the WHO-criteria for patients with CSF3R mutations. This would, of course, require a new designator for patients with a clinical phenotype resembling CNL but with JAK2V617F. This situation is distinct than those in which a person with a CNL phenotype and a CSF3R mutation can also have a 2nd mutation such as SETBP1 (see below).
SET binding protein 1 (SETBP1) mutations
Three small studies reported SETBP1 mutations in some patients with CNL [4],[9],[21]. Pardanani et al.[4] reported 6 of 34 patients with clinically-suspected CNL had SETBP1 mutations and 4 of 12 patients with WHO-defined CNL had SETBP1 mutation and CSF3RT618I. We found SETBP1 mutations in 6 of 8 patients with CNL with CSF3RT618I[9]. Piazza et al.[21] reported a SETBP1 mutation in 4 patients with CNL and a CSF3R mutation. These patients had a worse prognosis than those with CNL without a SETBP1 mutation [4],[21],[22], an observation requires confirmation.
Molecular genetics of CMML
Mutations are detected in about 90 percent of patients with CMML [23]-[25]. These mutations are clustered into four categories: (1) mutations involving epigenetic regulator genes (Figure 1B) [23]-[26]; (2) mutations involving the spliceosome component pathway (Figure 1C) [27]-[30]; (3) mutations involving transcription factors [24],[31]-[33]; and (4) mutations involving signaling regulator genes [24],[26],[34]-[37].
Epigenetic regulator gene mutations
Mutations in tet methylcytosine dioxygenase 2 (TET2) mutations are detected in 40–60 percent of patients with CMML [24],[26],[38],[39]. There is controversy whether TET2 mutations in patients with CMML is associated with prognosis. Kosmider et al.[38] reported TET2 mutation was associated with a poor prognosis but this was not confirmed in 2 recent large series [24],[30]. Mutations in DNA (cytosine-5-)-methylthransferase 3 alpha (DNMT3A) and isocitrate dehydrogenase 1/2 (IDH1/2) are rare in CMML [24],[26],[40]. DNMT3A mutations trended to occur in CMML-2 and were reported in 6 of 20 patients with CMML-derived AML [26]. Additional sex combs like transcriptional regulator 1 (ASXL1) mutations are detected in 40–50 percent of patients with CMML [24],[30],[41] who are reported to have a higher WBC and higher levels of monocytes and immature myeloid cells in the blood [24],[30]. Clinical features of patients with CMML and c.1934dupG;p.G646WfsX12 are similar to those of patients with other ASXL1 mutations [24],[30]. Conclusions from 2 large series about prognostic impact of ASXL1 mutations on survival are contradictory. Itzykson et al. reported ASXL1 mutation was an unfavorable independent prognostic factor [24]. However, data from Patnaik et al. showed that ASXL1 mutations had no impact on survival [30]. This controversy requires resolution. Enhancer of zeste 2 polycomb repressive complex 2 subunit (EZH2) mutations are uncommon in CMML [24].
Spliceosome component mutations
About 60 percent of patients with CMML have mutations in genes involved in RNA-splicing [24]. Most common are mutations in serine/arginine-rich splicing factor 2 (SRSF2) in 30–50 percent of cases. These mutations are associated with increased age, less pronounced anemia and a diploid karyotype but not with prognosis [24],[28],[29],[42]. SRSF2 or zinc finger (CCCH type), RNA-binding motif and serine/arginine rich 2 (ZRSR2) mutations are frequently concordant with TET2 mutations [24],[28],[43].
Mutations affecting transcription
Mutations in the runt-related transcription factor 1 (RUNX1) transcription factor are detected in 15–40 percent of patients with CMML [24],[31]-[33]. Patients with CMML and RUNX1 mutations may have a higher risk of transformation to AML [31],[33]. CCAAT/enhancer binding protein, alpha (CEBPA) mutations are rare in patients with CMML [33].
Signaling regulator gene mutations
Kosmider et al.[35] reported variant CSF3R somatic mutations in about 4 percent of patients with CMML with high concordance for ASXL1 mutations. These patients were reported to have a poor prognosis. SETBP1 mutations are detected in about 5 percent of patients with CMML and are associated with a poor prognosis in patients who also have an ASXL1 mutation [35]-[37]. SETBP1 and CSF3R mutations seem mutually exclusive in CMML. Cbl proto-oncogene, E3 ubiquitin protein ligase (CBL) mutations are detected in about 10 percent of patients with CMML [24],[34],[44],[45].
Recently, Itzykson et al. tracked mutations in single-cell-derived myeloid colonies after in vitro culture in patients with CMML [25]. Their data indicate a preferential order of mutation acquisition in progenitor cells. Mutations in TET2 (or IDH1 and IDH2) or ASXL1 occur 1st followed by mutations in SRSF2 or spliceosome component pathway genes followed by mutations in signal transduction-related genes [25]. These data recall data from studies of the relationship between temporal acquisition of mutations of JAK2V617F and TET2 or ASXL1 in patients with other MPNs where clinical and laboratory features are correlated with which mutation occurs 1st[46],[47].
Molecular genetics of atypical CML
SETBP1 mutations
SETBP1 mutations are detected in about 25–30 percent of patients with atypical CML [21],[48]. These patients have higher WBCs and a worse prognosis than patients without SETBP1 mutations [21]. SETBP1 mutations are associated with del(7) and iso(17)(q10)), ASXL1 and CBL mutations are exclusive of JAK2 and TET2 mutations in patients with atypical CML [48]. Recent study [49] showed that overexpression of SETBP1 associated with micro-RNA desregulation in MPN.
Other mutations
CSF3R mutations do not occur in patients with atypical CML [4]. In contrast, TET2 mutations are common [23],[37],[48],[50]. ASXL1 mutations [20],[51] are detected in 20–70 percent of patients with atypical CML and SRSF2 mutations about 40 percent [51]. SRFS2, SETBP1 and ASXL1 mutations are often confounded [51].
Next-generation sequencing (NGS) in MPN and MDS/MPN
NGS technology, such as whole-exons sequencing (WES) has demonstrated its power in re-sequecing human genomes to enhance our understanding of how molecular genetics affect MPN and MDS/MPN [1],[15],[16],[21],[25]. However, the challenge is to provide genetic information in a timely and affordable way. Thus, the utility of detailed targeted resequencing by capturing technologies is currently reasonable in clinical practicality. Consequently, molecular biomarkers will soon no longer be sequenced individually. Instead, panels of biomarkers will be assessed in a massively parallel way with high sensitivity and multiplexing in patients with MPN or MDS/MPN for diagnosis and individualized treatment regimens.
Conclusion
The mutational landscapes or terrains of CNL, CMML and atypical CML are complex, but some mutations are relatively specific in these 3 disorders. Furthermore, the order in which mutations are acquired may correlate with clinical features and prognosis. Therefore, analyse of mutations in MPNs is increasingly important for several reasons. 1st, mutation analyses is useful in trying to determine the aetiology of an increased WBC. For example, mutations in CSF3R suggest CNL, SETBP1 mutations, atypical CML and concurrent TET2 and SRSF2 or ZRSR2 mutations, CMML. Analyses of these frequently mutated genes can determine clonality and distinguish neoplasms from non-neoplastic increases in the WBC (Figure 2). 2nd, mutations in ASXL1, SEBP1, DNMT3A are associated, albeit inconsistently, with a poor prognosis in MPNs and MDS/MPNs. These data, if confirmed, could be added to prognostic scoring systems. 3rd, identifying specific molecular abnormalities can suggest new therapy targets for these diseases, such as hedgehog pathway inhibitors [52].
A schematic approach, outlining the evaluation for a patient presenting with peripheral blood leukocytosis. * Molecular genetics test should include mutations involved JAK2, CALR, MPL, CSF3R, TET2, SRSF2, ZRSR2, ASXL1, SETBP1 and BCR-ABL1 fusion genes and rearrangement of PDGFRA, PDGFRB or FGFR1. AML, Acute myeloid leukaemia; CML, chronic myelogenous leukemia; CNL,Chronic neutrophilic leukemia; CMML, chronic myelomonocytic leukemia; MDS, myelodysplastic syndromes; MPN, myeloproliferative neoplasms; MDS/MPN, myelodysplastic/myeloproliferative neoplasms.
References
Maxson JE, Gotlib J, Pollyea DA, Fleischman AG, Agarwal A, Eide CA, Bottomly D, Wilmot B, McWeeney SK, Tognon CE, Pond JB, Collins RH, Goueli B, Oh ST, Deininger MW, Chang BH, Loriaux MM, Druker BJ, Tyner JW: Oncogenic CSF3R mutations in chronic neutrophilic leukemia and atypical CML. N Engl J Med. 2013, 368: 1781-1790. 10.1056/NEJMoa1214514.
Dong F, van Buitenen C, Pouwels K, Hoefsloot LH, Lowenberg B, Touw IP: Distinct cytoplasmic regions of the human granulocyte colony-stimulating factor receptor involved in induction of proliferation and maturation. Mol Cell Biol. 1993, 13: 7774-7781.
Fleischman AG, Maxson JE, Luty SB, Agarwal A, Royer LR, Abel ML, MacManiman JD, Loriaux MM, Druker BJ, Tyner JW: The CSF3R T618I mutation causes a lethal neutrophilic neoplasia in mice that is responsive to therapeutic JAK inhibition. Blood. 2013, 122: 3628-3631. 10.1182/blood-2013-06-509976.
Pardanani A, Lasho TL, Laborde RR, Elliott M, Hanson CA, Knudson RA, Ketterling RP, Maxson JE, Tyner JW, Tefferi A: CSF3R T618I is a highly prevalent and specific mutation in chronic neutrophilic leukemia. Leukemia. 2013, 27: 1870-1873. 10.1038/leu.2013.122.
Ito T, Kojima H, Otani K, Komeno T, Mitsuhashi S, Hasegawa Y, Kobayashi T, Ninomiya H, Nagasawa T, Abe T: Chronic neutrophilic leukemia associated with monoclonal gammopathy of undetermined significance. Acta Haematol. 1996, 95: 140-143. 10.1159/000203863.
Rovira M, Cervantes F, Nomdedeu B, Rozman C: Chronic neutrophilic leukaemia preceding for seven years the development of multiple myeloma. Acta Haematol. 1990, 83: 94-95. 10.1159/000205176.
Kohmura K, Miyakawa Y, Kameyama K, Kizaki M, Ikeda Y: Granulocyte colony stimulating factor-producing multiple myeloma associated with neutrophilia. Leuk Lymphoma. 2004, 45: 1475-1479. 10.1080/10428190310001645870.
Standen GR, Steers FJ, Jones L: Clonality of chronic neutrophilic leukaemia associated with myeloma: analysis using the X-linked probe M27 beta. J Clin Pathol. 1993, 46: 297-298. 10.1136/jcp.46.4.297.
Cui Y, Li B, Gale RP, Jiang Q, Xu Z, Qin T, Zhang P, Zhang Y, Xiao Z: CSF3R, SETBP1 and CALR mutations in chronic neutrophilic leukemia. J Hematol Oncol. 2014, 7: 77-10.1186/s13045-014-0077-1.
Levine R, Loriaux M, Huntly BJ, Loh ML, Beran M, Stoffregen E, Berger R, Clark JJ, Willis SG, Nguyen KT, Flores NJ, Estey E, Gattermann N, Armstrong S, Look AT, Griffin JD, Bernard OA, Heinrich MC, Gilliland DG, Druker B, Deininger MW: The JAK2V617F activating mutation occurs in chronic myelomonocytic leukemia and acute myeloid leukemia, but not in acute lymphoblastic leukemia or chronic lymphocytic leukemia. Blood. 2005, 106: 3377-3379. 10.1182/blood-2005-05-1898.
Pastore F, Schneider S, Christ O, Hiddemann W, Spiekermann K: Impressive thrombocytosis evolving in a patient with a BCR-ABL positive CML in major molecular response during dasatinib treatment unmasks an additional JAK2V617F. Exp Hematol Oncol. 2013, 2: 24-10.1186/2162-3619-2-24.
Ortiz-Cruz K, Amog-Jones G, Salvatore JR: Chronic neutrophilic leukemiawith JAK2 gene mutation. Commun Oncol. 2012, 9: 127-131. 10.1016/j.cmonc.2012.03.012.
Mc Lornan DP, Percy MJ, Jones AV, Cross NC, Mc Mullin MF: Chronic neutrophilic leukemia with an associated V617F JAK2 tyrosine kinase mutation. Haematologica. 2005, 90: 1696-1697.
Lee J-H, Ha JS, Ryoo NH, Jeon DS, Kim JR: A case of acute myeloid leukemia transformed from JAK2 V617F-positive chronic neutrophilic leukemia. Lab Med Online. 2012, 2: 101-104. 10.3343/lmo.2012.2.2.101.
Klampfl T, Gisslinger H, Harutyunyan AS, Nivarthi H, Rumi E, Milosevic JD, Them NC, Berg T, Gisslinger B, Pietra D, Chen D, Vladimer GI, Bagienski K, Milanesi C, Casetti IC, Sant’Antonio E, Ferretti V, Elena C, Schischlik F, Cleary C, Six M, Schalling M, Schonegger A, Bock C, Malcovati L, Pascutto C, Superti-Furga G, Cazzola M, Kralovics R: Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med. 2013, 369: 2379-2390. 10.1056/NEJMoa1311347.
Nangalia J, Massie CE, Baxter EJ, Nice FL, Gundem G, Wedge DC, Avezov E, Li J, Kollmann K, Kent DG, Aziz A, Godfrey AL, Hinton J, Martincorenal I, Van Loo P, Jones AV, Guglielmelli P, Tarpey P, Harding HP, Fitzpatrick JD, Goudie CT, Ortmann CA, Loughran SJ, Raine K, Jones DR, Butler AP, Teague JW, O’Meara S, McLaren S, Bianchi M: Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. N Engl J Med. 2013, 369: 2391-2405. 10.1056/NEJMoa1312542.
Rotunno G, Mannarelli C, Guglielmelli P, Pacilli A, Pancrazzi A, Pieri L, Fanelli T, Bosi A, Vannucchi AM: Associazione Italiana per la Ricerca sul Cancro Gruppo Italiano Malattie Mieloproliferative Investigators. Impact fo calreticulin mutations on clinical and hematological phenotype and outcome in essential thrombocythemia. Blood. 2014, 123: 1552-1555. 10.1182/blood-2013-11-538983.
Tefferi A, Lasho TL, Finke CM, Finke CM, Knudson RA, Ketterling R, Hanson CH, Maffioli M, Caramazza D, Passamonti F, Pardanani A: CALR vs JAK2 vs MPL-mutated or triple-negative myelofibrosis: clinical, cytogenetic and molecular comparisons. Leukemia. 2014, 28: 1472-1477. 10.1038/leu.2014.3.
Gajendra S, Gupta R, Chandgothia M, Kumar L, Gupta R, Chavan SM: Chronic neutrophilic leukemia with V617F JAK2 mutation. Indian J Hematol Blood Transfus. 2014, 30: 139-142. 10.1007/s12288-012-0203-6.
Lasho TL, Elliott MA, Pardanani A, Tefferi A: CALR mutation studies in chronic neutrophilic leukemia. Am J Hematol. 2014, 89: 450-10.1002/ajh.23665.
Piazza R, Valletta S, Winkelmann N, Winkelmann N, Redaelli S, Spinelli R, Pirola A, Antolini L, Mologni L, Donadoni C, Papaemmanuil E, Schnittger S, Kim DW, Boultwood J, Rossi F, Gaipa G, De Martini GP, di Celle PF, Jang HG, Fantin V, Bignell GR, Magistroni V, Haferlach T, Pogliani EM, Campbell PJ, Chase AJ, Tapper WJ, Cross NC, Gambacorti-Passerini C: Recurrent SETBP1 mutations in atypical chronic myeloid leukemia. Nat Genet. 2013, 45: 18-24. 10.1038/ng.2495.
Lasho TL, Mims A, Elliott MA, Finke C, Pardanani A, Tefferi A: Chronic neutrophilic leukemia with concurrent CSF3R and SETBP1 mutations: single colony clonality studies, in vitro sensitivity to JAK inhibitors and lack of treatment response to ruxolitinib. Leukemia. 2014, 28: 1363-1365. 10.1038/leu.2014.39.
Gelsi-Boyer V, Brecqueville M, Devillier R, Murati A, Mozziconacci MJ, Birnbaum D: Mutations in ASXL1 are associated with poor prognosis across the spectrum of malignant myeloid diseases. J Hematol Oncol. 2012, 5: 12-10.1186/1756-8722-5-12.
Itzykson R, Kosmider O, Renneville A, Gelsi-Boyer V, Meggendorfer M, Morabito M, Berthon C, Ades L, Fenaux P, Beyne-Rauzy O, Vey N, Braun T, Haferlach T, Dreyfus F, Cross NC, Preudhomme C, Bernard OA, Fontenay M, Vainchenker W, Schnittger S, Birnbaum D, Droin N, Solary E: Prognostic score including gene mutations in chronic myelomonocytic leukemia. J Clin Oncol. 2013, 31: 2428-2436. 10.1200/JCO.2012.47.3314.
Itzykson R, Kosmider O, Renneville A, Morabito M, Preudhomme C, Berthon C, Ades L, Fenaux P, Platzbecker U, Gagey O, Rameau P, Meurice G, Orear C, Delhommeau F, Bernard OA, Fontenay M, Vainchenker W, Droin N, Solary E: Clonal architecture of chronic myelomonocytic leukemias. Blood. 2013, 121: 2186-2198. 10.1182/blood-2012-06-440347.
Jankowska AM, Makishima H, Tiu RV, Szpurka H, Huang Y, Traina F, Visconte V, Sugimoto Y, Prince C, O’Keefe C, His ED, List A, Sekeres MA, Rao A, McDevitt MA, Maciejewski JP: Mutational spectrum analysis of chronic myelomonocytic leukemia includes gene associated with epigenetic regulation: UTX, EZH2, and DNMT3A. Blood. 2011, 118: 3932-3941. 10.1182/blood-2010-10-311019.
Yoshida K, Sanada M, Shiraishi Y, Nowak D, Nagata Y, Yamamoto R, Sato Y, Sato-Otsubo A, Kon A, Nagasaki M, Chalkidis G, Suzuki Y, Shiosaka M, Kawahata R, Yamaguchi T, Otsu M, Obara N, Sakata-Yanagimoto M, Ishiyama K, Mori H, Nolte F, Hofmann WK, Miyawaki S, Sugano S, Haferlach C, Koeffler HP, Shih LY, Haferlach T, Chiba S, Nakauchi H: Frequent pathway mutations of splicing machinery in myelodysplasia. Nature. 2011, 478: 64-69. 10.1038/nature10496.
Meggendorfer M, Roller A, Haferlach T, Eder C, Dicker F, Grossmann V, Kohlmann A, Alpermann T, Yoshida K, Ogawa S, Koeffler HP, Kern W, Haferlach C, Schnittger S: SRSF2 mutations in 275 cases with chronic myelomonocytic leukemia (CMML). Blood. 2012, 120: 3080-3088. 10.1182/blood-2012-01-404863.
Kar SA, Jankowska A, Makishima H, Visconte V, Jerez A, Sugimotto Y, Muramatsu H, Traina F, Afable M, Guinta K, Tiu RV, Przychodzen B, Sakaguchi H, Kojima S, Sekeres MA, List AF, McDevitt MA, Maciejewski JP: Spliceosomal gene mutations are frequent events in the diverse mutational spectrum of chronic myelomonocytic leukemia but largely absent in juvenile myelomonocytic leukemia. Haematologica. 2013, 98: 107-113. 10.3324/haematol.2012.064048.
Patnaik MM, Padron E, LaBorde RR, Lasho TL, Finke CM, Hanson CA, Hodnefield JM, Knudson RA, Ketterling RP, Al-kali A, Pardanani A, Ali NA, Komrokji RS, Tefferi A: Mayo prognostic model for WHO-defined chronic myelomonocytic leukemia: ASXL1 and spliceosome component mutations and outcomes. Leukemia. 2013, 27: 1504-1510. 10.1038/leu.2013.88.
Kuo MC, Liang DC, Huang CF, Shih YS, Wu JH, Lin TL, Shih LY: RUNX1 mutations are frequent in chronic myelomonocytic leukemia and mutations at the C-terminal region might predict acute myeloid leukemia transformation. Leukemia. 2009, 23: 1426-1431. 10.1038/leu.2009.48.
Gelsi-Boyer V, Trouplin V, Adelaide J, Aceto N, Remy V, Pinson S, Houdayer C, Arnoulet C, Sainty D, Bentires-Alj M, Olschwang S, Vey N, Mozziconacci MJ, Birnbaum D, Chaffanet M: Genome profiling of chronic myelomonocytic leukemia: frequent alterations of RAS and RUNX1 genes. BMC Cancer. 2008, 8: 299-10.1186/1471-2407-8-299.
Ernst T, Chase A, Zoi K, Waghorn K, Hidalgo-Curtis C, Score J, Jones A, Grand F, Reiter A, Hochhaus A, Cross NC: Transcription factor mutations in myelodysplastic/myeloproliferative neoplasms. Haematologica. 2010, 95: 1473-1480. 10.3324/haematol.2010.021808.
Kohlmann A, Grossmann V, Klein H, Schindela S, Weiss T, Kazak B, Dicker F, Schnittger S, Dugas M, Kern W, Haferlach C, Haferlach T: Next-generation sequencing technology reveals a characteristic pattern of molecular mutations in 72.8% of chronic myelomonocytic leukemia by detecting frequent alterations in TET2, CBL, RAS, and RUNX1. J Clin Oncol. 2010, 28: 3858-3865. 10.1200/JCO.2009.27.1361.
Kosmider O, Itzykson R, Chesnais V, Lasho T, Laborde R, Knudson R, Gauthier A, Merlevede J, Ades L, Morabito M, Fontenay M, Tefferi A, Droin N, Solary E: Mutations of the colony-stimulating factor-3 receptor gene is a rare event with poor prognosis in chronic myelomonocytic leukemia. Leukemia. 2013, 27: 1946-1949. 10.1038/leu.2013.182.
Damm F, Itzykson R, Kosmider O, Droin N, Renneville A, Chesnais V, Gelsi-Boyer V, de Botton S, Vey N, Preudhomme C, Clavert A, Delabesse E, Park S, Birnbaum D, Fontenay M, Bernard OA, Solary E: SETBP1 mutations in 658 patients with myelodysplastic syndromes, chronic myelomonocytic leukemia and secondary acute myeloid leukemias. Leukemia. 2013, 27: 1401-1403. 10.1038/leu.2013.35.
Laborde RR, Patnaik MM, Lasho TL, Finke CM, Hanson CA, Knudson RA, Ketterling RP, Pardanani A, Tefferi A: SETBP1 mutations in 415 patients with primary myelofibrosis or chronic myelomonocytic leukemia: independent prognostic impact in CMML. Leukemia. 2013, 27: 2100-2102. 10.1038/leu.2013.97.
Kosmider O, Gelsi-Boyer V, Ciudad M, Racoeur C, Jooste V, Vey N, Quesnel B, Fenaux P, Bastie JN, Beyne-Rauzy O, Stamatoulas A, Dreyfus F, Ifrah N, de Botton S, Vainchenker W, Bernard OA, Birnbaum D, Fontenay M, Solary E: Groupe Francophone des Myelodysplasies. TET2 gene mutations is a frequent and adverse event in chronic myelomonocytic leukemia. Haematologica. 2009, 94: 1676-1681. 10.3324/haematol.2009.011205.
Tefferi A, Lim KH, Abdel-Wahab O, Lasho TL, Patel J, Patnaik MM, Hanson CA, Pardanani A, Gilliland DG, Levine RL: Detection of mutant TET2 in myeloid malignancies other than myeloproliferative neoplasms: CMML, MDS, MDS/MPN and AML. Leukemia. 2009, 23: 1343-1345. 10.1038/leu.2009.59.
Abdel-Wahab O, Pardanani A, Rampal R, Lasho RL, Tefferi A: DNMT3A mutational analysis in primary myelofibrosis, chronic myelomonocytic leukemia and advanced phases of myeloproliferative neoplasms. Leukemia. 2011, 25: 1219-1220. 10.1038/leu.2011.82.
Gelsi-Boyer V, Trouplin V, Adelaide J, Bonansea J, Cervera N, Carbuccia N, Lagarde A, Prebet T, Nezri M, Sainty D, Olschwang S, Xerri L, Chaffanet M, Mozziconacci MJ, Vey N, Birnbaum D: Mutations of polycomb-associated gene ASXL1 in myelodysplastic syndromes and chronic myelomonocytic leukaemia. Br J Haematol. 2009, 145: 788-800. 10.1111/j.1365-2141.2009.07697.x.
Patanaik MM, Lasho TL, Finke CM, Hanson CA, Hodnefield JM, Knudson RA, Ketterling RP, Pardanani A, Tefferi A: Spliceosome mutations involving SRSF2, SF3B1, and U2AF35 in chronic myelomonocytic leukemia: prevalence, clinical correlates, and prognostic relevance. Am J Hematol. 2013, 88: 201-206. 10.1002/ajh.23373.
Malcovati L, Papaemmanuil E, Ambaglio I, Elena C, Galli A, Della Porta MG, Travaglino E, Pietra D, Pascutto C, Ubezio M, Bono E, Davia MC, Brisci A, Bruno F, Cremonesi L, Ferrari M, Boveri E, Invernizzi R, Campbell PJ, Cazzola M: Driver somatic mutations identify distinct disease entities within myeloid neoplasms with myelodysplasia. Blood. 2014, 124: 1513-1521. 10.1182/blood-2014-03-560227.
Makishima H, Cazzolli H, Szpurka H, Dunbar A, Tiu R, Huh J, Muramatsu H, O’Keefe C, His E, Paquette RL, Kojima S, List AF, Sekeres MA, McDevitt MA, Maciejewski JP: Mutations of e3 ubiquitin ligase cbl family members constitute a novel common pathogenic lesion in myeloid malignancies. J Clin Oncol. 2009, 27: 6109-6116. 10.1200/JCO.2009.23.7503.
Sanada M, Suzuki T, Shih LY, Otsu M, Kato M, Yamazaki S, Tamura A, Honda H, Sakata-Yanagimotto M, Kumano K, Oda H, Yamagata T, Takita J, Gotoh N, Nakazaki K, Kawamata N, Onodera M, Nobuyoshi M, Hayashi Y, Harada H, Kurokawa M, Chiba S, Mori H, Ozawa K, Omine M, Hirai H, Nakauchi H, Koeffler HP, Ogawa S: Gain-of-function of mutated C-CBL tumor suppressor in myeloid neoplasms. Nature. 2009, 460: 904-908. 10.1038/nature08240.
Beer PA, Delhommeau F, Lecouedic JP, Dawson MA, Chen E, Bareford D, Kusec R, McMullin MF, Harrison CN, Vannucchi AM, Vainchenker W, Green AR: Two routes to leukemic transformation after a JAK2 mutation-positive myeloproliferative neoplasm. Blood. 2010, 115: 2891-2900. 10.1182/blood-2009-08-236596.
Ferrer-Marin F, Bellosillo B, Martinez-Aviles L, Soler G, Carbonell P, Luengo-Gil G, Caparros E, Torregrosa JM, Besses C, Vicente V: Leukemic transformation driven by an ASXL1 mutation after a JAK2V617F-positive primary myelofibrosis: clonal evolution and hierarchy revealed by next-generation sequencing. J Hematol Oncol. 2013, 6: 68-10.1186/1756-8722-6-68.
Meggendorfer M, Bacher U, Alpermann T, Haferlach C, Kern W, Gambacorti-Passerini C, Haferlach T, Schnittger S: SETBP1 mutations occur in 9% of MDS/MPN and in 4% of MPN cases and are strongly associated with atypical CML, monosomy 7, isochromosome i(17)(q10), ASXL1 and CBL mutations. Leukemia. 2013, 27: 1852-1860. 10.1038/leu.2013.133.
Albano F, Anelli L, Zagaria A, Coccaro N, Casieri P, Minervini A, Specchia G: SETBP1 and miR-4319 dysregulation in primary myelofibrosis progression to acute myeloid leukemia. J Hematol Oncol. 2012, 5: 48-10.1186/1756-8722-5-48.
Jankowska AM, Szpurka H, Tiu RV, Makishima H, Afable M, Huh J, O’Keefe CL, Ganetzky R, McDevitt MA, Maciejewski JP: Loss of heterozygosity 4q24 and TET2 mutations associated with myelodysplastic/myeloproliferative neoplasms. Blood. 2009, 113: 6403-6410. 10.1182/blood-2009-02-205690.
Meggendorfer M, Haferlach T, Alpermann T, Jeromin S, Haferlach C, Kern W, Schnittger S: Specific molecular mutation patterns delineate chronic neutrophilic leukemia, atypical chronic myeloid leukemia, and chronic myelomonocytic leukemia.Haematologica 2014, 113159. in press.,
Tibes R, Mesa RA: Targeting hedgehog signaling in myelofibrosis and other hematologic malignancies. J Hematol Oncol. 2014, 7: 18-10.1186/1756-8722-7-18.
Acknowledgements
Supported in part by National Natural Science Funds (No.81370611, No. 81270585), Tianjin Key Natural Science Funds (12JCZDJC23900), National Public Health Grand Research Foundation (No.201202017) (to ZX). RPG acknowledges support from the NIHR Biomedical Research Centre funding scheme.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
RPG is a part-time employee of Celgene Corp., Summit, NJ and scheme. The remaining authors declare no competing financial interests.
Authors’ contributions
LB, RPG and XZJ wrote the typescript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Li, B., Gale, R.P. & Xiao, Z. Molecular genetics of chronic neutrophilic leukemia, chronic myelomonocytic leukemia and atypical chronic myeloid leukemia. J Hematol Oncol 7, 93 (2014). https://doi.org/10.1186/s13045-014-0093-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13045-014-0093-1