Abstract
Background
The evidence base for the prevention of type 2 diabetes mellitus (T2DM) has progressed rapidly from efficacy trials to real-world translational studies and practical implementation trials over the last 15 years. However, evidence for the effective implementation and translation of diabetes programs and their population impact needs to be established in ways that are different from measuring program effectiveness. We report the findings of a systematic review that focuses on identifying the critical success factors for implementing diabetes prevention programs in real-world settings.
Methods
A systematic review of programs aimed at diabetes prevention was undertaken in order to evaluate their outcomes using the penetration, implementation, participation, and effectiveness (PIPE) impact metric. A search for relevant articles was carried out using PubMed (March 2015) and Web of Science, MEDLINE, CENTRAL, and EMBASE. A quality coding system was developed and included studies were rated independently by three researchers.
Results
Thirty eight studies were included in the review. Almost all (92 %) provided details on participation; however, only 18 % reported the coverage of their target population (penetration). Program intensity or implementation—as measured by frequency of contacts during first year and intervention duration—was identified in all of the reported studies, and 84 % of the studies also reported implementation fidelity; however, only 18 % of studies employed quality assurance measures to assess the extent to which the program was delivered as planned. Sixteen and 26 % of studies reported ‘highly’ or ‘moderately’ positive changes (effectiveness) respectively, based on weight loss. Six (16 %) studies reported ‘high’ diabetes risk reduction but ‘low’ to ‘moderate’ weight loss only.
Conclusion
Our findings identify that program intensity plays a major role in weight loss outcomes. However, programs that have high uptake—both in terms of good coverage of invitees and their willingness to accept the invitation—can still have considerable impact in lowering diabetes risk in a population, even with a low intensity intervention that only leads to low or moderate weight loss. From a public health perspective, this is an important finding, especially for resource constrained settings. More use of the PIPE framework components will facilitate increased uptake of T2DM prevention programs around the world.
Similar content being viewed by others
Background
Type 2 diabetes mellitus (T2DM) has emerged as a major public health challenge with an estimated 387 million people living with T2DM globally [1]. Efforts to prevent or delay the onset of diabetes are an urgent public health priority with health, social, and economic benefits. Several large randomized controlled trials (RCTs) from the US, Finland, China, and India have demonstrated that lifestyle interventions can be successful in reducing the incidence of T2DM from 29–58 % in high-risk populations [2–5], with generally good maintenance for up to 20 years [6, 7]. However, these trials have mainly focused on efficacy and effectiveness outcomes. It is now important that more emphasis is given to the implementation and transferability of diabetes prevention programs into real-world settings. ‘Implementation’ research focuses on understanding the processes, results, and factors affecting implementation under real-world conditions by answering questions such as ‘why and how interventions work in real-world settings’ [8]. ‘Transferability’ describes the process of applying the results of research in one situation to other similar situations’ [9]. ‘Real-world’ contexts are settings where health research findings are applied in practice. The latter include primary healthcare settings, work organizations, churches, and schools. Major transferability gaps still remain in translating diabetes prevention from research into practice [10].
Several reviews of diabetes prevention trials have been conducted to examine their effectiveness [11–23]. Some recent reviews have examined how implementation influences effectiveness, most particularly in relation to the US diabetes prevention program (US-DPP). One of these reviews [24] summarized lifestyle interventions based on the US-DPP curriculum and described how different curricula (as a measure of implementation) affected outcomes. They found that the less-intense version of the US-DPP core curriculum may influence long-term outcomes. Ali et al. [25] conducted a systematic review and meta-analysis of 28 translational studies based on the US-DPP and concluded that the utilization of non-medical personnel in delivering diabetes prevention interventions can lower the overall costs without compromising effectiveness. Johnson and colleagues [26] synthesized evidence from translational studies and assessed the impact of interventions delivered outside large randomized trials. The review included 17 translational studies from a range of settings and concluded that there is potential for less intensive interventions to have an impact on future progression to diabetes in at-risk individuals. However, these reviews included studies where subjects had either already progressed to diabetes [25, 26] or had short follow-up (e.g. less than 12 months [26]).
Another systematic review by Dunkley et al. [27] concluded that pragmatic diabetes prevention programs are effective and adherence to international guideline recommendations is significantly associated with a greater weight loss; however, the authors mainly focussed on the effectiveness of the selected translational studies in relation to the main outcome without giving consideration to the adaptability and scalability dimensions of translation.
A more recent systematic review [28] assessing combined diet and physical activity promotion programs of between 3 months and 6 years duration concluded that more intensive programs resulted in greater weight loss and lowered the risk of T2DM more than less intensive programs and this was also found to be cost-effective. Based on the accumulated evidence from this and other reviews, the US Community Preventive Services Task Force (CPSTF) has recently recommended combined diet and physical activity promotion programs to prevent T2DM [28]. Importantly, however, the above review examining the translation of diabetes prevention programs like US-DPP did not address issues specifically related to the long-term scalability and sustainability of such programs.
Another comprehensive review to evaluate the generalizability of diabetes prevention trials was conducted by Whittemore [29] using Glasgow’s [30] reach, efficacy, adoption, implementation, maintenance (RE-AIM) framework. This is a framework designed to summarize how well research trials report on elements related to research translation. Generalizability is an important element of translational research, i.e. the degree to which findings from a study or set of studies can be more broadly generalized to populations and settings beyond those in the original studies [31, 32]. This review included 16 studies that translated the US-DPP protocol into four distinct settings: (a) hospital outpatient, (b) primary care, (c) community, and (d) work and church. The author found positive outcomes in terms of the reach, efficacy, adoption, implementation, and maintenance of programs. However, this review had a narrow focus and only included those studies that were based on the US-DPP; no other protocols were considered or included. Another limitation was that several studies considered only short-term effectiveness of up to 3 months, and some of the included studies also recruited patients who already had diabetes. Laws and colleagues [31] conducted a systematic review examining the adequacy of reporting of external validity components of lifestyle intervention trials aimed at T2DM prevention. The authors assessed the generalizability of the findings of 31 studies. Laws reported that all studies lacked full reporting on external validity elements. One of the limitations of this review was the use of a dichotomous rating scale (‘reported’ or ‘not reported’) which did not take into account external validity elements which were reported as continuous measures [31].
In summary, a number of recent reviews have focused on the real-world effectiveness of T2DM prevention, in particular, programs derived from the US-DPP. However, these reviews have not systematically examined the adaptability and scalability dimensions of translation, that is, what works, under what ‘real-world’ conditions and in which contexts; yet this information is critically important for policy makers and program implementers who need to identify diabetes prevention programs with significant population impact.
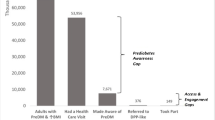
To address this knowledge gap, we have undertaken a systematic review that focuses on identifying the critical success factors for implementing diabetes prevention programs in real-world settings. We consider the importance of program and product design elements that are important to real-world implementation including the effect size, scope of services, scalability potential, and long-term sustainability [33]. We use the penetration, implementation, participation, effectiveness (PIPE) impact metric, a framework that is highly relevant to implementation and a formal assessment of the net impact of health improvement programs that is explicitly linked to the program design elements noted above [33]. The four key elements of the PIPE framework are as follows: (1) penetration of the program into the population of interest, (2) implementation of the proposed set of services, (3) participation in the program, and (4) effectiveness in generating expected outcomes. Each of the PIPE Impact Metric elements may be expressed as a coefficient, and the product of these four coefficients is referred to as the PIPE impact metric. The PIPE Impact Metric can be used to provide feedback to program administrators on gaps in performance, and it also enables the integration of program design features and identifies where to focus on for performance improvement changes. This paper aims to review the current evidence about success factors for implementing diabetes prevention programs in real-world settings using the PIPE Impact Metric.
Methods
Data sources and searches
A comprehensive search was carried out using PubMed, Web of Science, MEDLINE, CENTRAL, and EMBASE (February 2014). Search terms were ‘diabetes’ AND ‘prevention’ AND (‘program’ OR ‘intervention’) AND (implementation’ OR ‘translation’). The search was repeated using PubMed to include relevant articles from February 2014 to March 2015. A detailed search strategy is provided in Additional file 1.
Study selection
We included all published studies in the last 15 years (i.e. 2001–2015) that reported on the evaluation of a lifestyle-focused program aimed at individuals at moderate or high risk of diabetes (e.g. impaired glucose tolerance (IGT), elevated haemoglobin A1c (HbA1c), high body mass index (BMI) or overweight). The inclusion criteria were adults aged 18 years or older; English language publications; and full text. The exclusion criteria were studies that were published prior to 2001; that did not report at least 1-year follow-up; included participants with known diabetes; included participants not at elevated risk of developing diabetes; and reported on multiple intervention components in a single study. Studies were also excluded if they were exclusively ‘diet-based’ or ‘exercise-based’ instead of referring to lifestyle or behavioural interventions or if they used lifestyle and pharmacological interventions.
Data extraction
An evaluation of T2DM prevention program impact was conducted using the PIPE Impact Metric [33]. The PIPE Impact Metric expresses four elements of program initiation and long-term delivery needed to maximize the population impact (i.e., penetration, implementation, participation, and effectiveness) as a coefficient. The product of all coefficients becomes the PIPE Impact Metric. For example, a study may report having reached 250 out of 350 individuals at high risk for T2DM workers at a company. In this example, penetration is reported as (250/350) = 0.714 (71 %). Similar coefficients are calculated for implementation, participation, and effectiveness. As numeric data was not available for some of the elements in some of the included studies, an alternative coding system, also informed by PIPE, was developed for this paper.
Data synthesis and analysis
The coding system is summarized in Table 1. It included two steps: (1) an initial scoring and (2) coding of the scores into ‘high’, ‘medium’, ‘low’, or ‘not able to calculate (NAC)’ where relevant data was not available. In the initial scoring, coefficients were calculated for penetration and participation. For implementation, the initial scoring was done on three aspects: frequency over the first 12 months; duration of the entire intervention including follow-up contacts; and intervention fidelity. To overcome heterogeneity in the kinds of contacts when scoring frequency, a system was developed to standardize the degree of contact based on number, length, and type (Table 1). Similarly, for effectiveness, the initial scoring was on three criteria: proportion of participants successful in achieving the main outcome; weight loss (in kilogrammes); and diabetes risk reduction (absolute/relative). The coding of the scores (into high, medium, low, and NAC) for each element was agreed-upon by the review team, and ratings were independently derived by three researchers (ZA, PA, JO). The ratings of all studies were then reviewed by all authors, and when disagreement on rating occurred, they were resolved with consensus among all authors.
Results
A detailed PRISMA flow diagram is attached (Fig. 1). The initial literature search (February 2014) returned 2992 publications and 61 additional articles were identified through hand searching of references from the bibliographies of articles identified. Two thousand thirty-nine articles were screened after removing duplicates. An additional 5 articles were included after updating the search until March 2015. A total of 180 articles were assessed for eligibility. A total of 76 articles from 38 studies were included in the review. Table 2 describes the characteristics of the included studies.
Studies that met the eligibility criteria for this review were mainly based on either the US-DPP or Finnish-DPS. Seventeen (45 %) studies were implemented in the USA, 4 in the UK, 4 in the Netherlands, 8 in other European countries, 3 in Australia, and 2 in Japan. There were no studies from low and middle income countries that met our eligibility criteria. The sample size for the participants enrolled in each of these studies ranged between 8 and 2553 participants. The studies were conducted in a range of settings including primary health care, faith-based, workplace, and other community-based settings.
Each study was assessed on the four components of PIPE Impact Metric using a coding system described in Table 1. Table 3 describes the ratings of all included studies based on the elements of the PIPE Impact Metric.
Program penetration
Our analysis shows that only nine (24 %) studies reported their estimated target population, from which only seven studies reported the proportion of the target population that was reached with invitations to engage in the program or intervention. Out of these seven studies, five had ‘high’, one had ‘moderate’, and one had ‘low’ penetration into their target populations (see Table 3 and Additional file 2: Table S4). Target populations included patients, employees, and church attendees. Each study used various strategies to recruit potential participants including mail invitations, posted flyers, advertising through media, contacting local physicians, local churches, or using intranet or work meetings in the workplace setting.
The five studies that were rated as having ‘high’ penetration in our analysis applied heterogeneous strategies to reach their target group. Two studies contacted a pre-defined group of people at risk: one at worksite, where all employees who had above average waist circumference were invited for screening [34], and in the other study [35] all eligible subjects with high risk for glucose intolerance from a cohort representing general population were contacted. Three studies contacted 100 % [36], 68 % [37], and 70 % [38] of the target population for selective screening either by mail or by appointment. The only study rated as having ‘moderate’ penetration, was a church-based study [39]. The church roster included 407 members, whereas 37 % of adults (approximately 150) who attended Sunday gatherings were invited to complete a diabetes risk assessment. The study rated as having ‘low’ penetration in our analysis [40] included 18 participating centres that covered all primary care services for 4.5 % of the population in Catalonia, out of which less than 1 % of the population was invited for screening.
Program implementation
In order to assess implementation, we evaluated the degree of contact (based on number, length, and type) during the first year of the intervention as frequency; the duration of the entire intervention; and the fidelity of the intervention (see Table 1). All studies in our analysis reported on frequency and duration. Thirty-four percent of all studies implemented ‘high’ frequency interventions, and 39 % studies delivered intervention over the period of 12 months or more. The number of contacts varied from a single small group session to 32 group sessions. About two thirds (66 %) of the programs based on the US-DPP model adopted a ‘low-’ to ‘moderately intense’ version (based on the degree of contact) as compared to the original. The main adaptation was the reduction from 16 to fewer sessions. In addition, groups led by volunteers as opposed to health care professionals and use of telephone as opposed to face-to-face delivery of individual sessions were also frequently observed adaptations. Only a small proportion (16 %) of studies reported ‘low’ duration, i.e. intervention delivered over the period of 6 months or less.
Implementation fidelity was defined as intervention being based on a standard curriculum for example the US-DPP and whether any quality assurance measures were applied to monitor the implementation of the intervention. Twenty-seven (71 %) studies were based on a standard curriculum, out of which only 7 studies had quality assurance measures applied to monitor the implementation. In some of these studies, while authors reported on the efforts made to minimize the potential lack of fidelity, none of these studies provided information on the extent to which the various components were delivered except one where the program components were more frequently added (40 %) than omitted (28 %) [41]. Refer to Table 3 and Additional file 2: Table S5 for further details.
Program participation
The majority of the studies in our analysis (n = 35; 92 %) reported participation. Twenty-five (71 %) of these 35 studies achieved ‘low’ participation rates. Half of these studies achieved participation rates equivalent to or lower than 10 %. Only 7 (18 %) studies had ‘high’ participation rates. For four of these studies [41–44], participants were recruited by referral from physicians, general practitioners (GPs), or nurses from the participating health facilities and invited to attend a screening clinic. Two of the 7 studies [45, 46] used a combination of strategies to recruit potential participants including contacting local physicians and primary healthcare practices; advertising through media; and recruiting through local employers, work sites, churches, and service groups. One study [47] recruited participants from online advertisement, seeking individuals with a self-reported clinical diagnosis of prediabetes occurring within the past year; however, recruitment was based on self-selection by participants, which does not reflect a truly random sample [47].
Three studies were scored as having ‘moderate’ participation, where 63 % [48], 57 % [49], and 44 % [50] of the individuals were enrolled after assessing all ‘invited’ individuals, for study eligibility (see Table 3 and Additional file 2: Table S6). In most of the remaining studies, the ‘low’ participation was attributed to either the non-eligibility of potential participants or the refusal to participate.
For studies where information was available for both penetration and participation, it was observed that ‘high’ penetration into the target population did not have positive effect on participation. All five studies rated as ‘high’ penetration in the analysis, reported ‘low’ participation. Also, none of the seven studies that were rated as ‘high’ participation provided enough information on reaching out to their target populations, and hence, penetration could not be calculated. However, the information available suggests that the studies where high-risk participants were identified and referred through their GPs or nurses resulted in ‘high’ participation rates.
Program effectiveness
Effectiveness was rated based on three criteria: proportion of successful participants; average weight loss; and diabetes risk reduction (absolute/relative) (Refer to Table 1). None of the studies reported on all three criteria. Seventeen (45 %) studies reported the use of intent-to-treat analysis; however, for the purpose of our analysis, effectiveness indicators were considered as presented in each of the studies.
One third (n = 12, 32 %) of the studies reported the proportion of successful participants who achieved the primary outcome (i.e. 5 % weight loss). The proportion of successful participants ranged between 20 and 64 %. Thirty-two (84 %) studies reported average weight loss by participants at 12 months, with a range from 0.45 to 7.7 kg. Only six of these studies were rated ‘high’ where average weight loss by participants was more than 4.6 kg. Sixteen (42 %) studies were rated ‘low’ on the basis of average weight loss of ≤2.3 kg. Only seven (18 %) studies reported the data on diabetes risk reduction (absolute/relative), where six studies were rated ‘high’ and one was rated ‘moderate’. Scores could not be calculated in three studies due to the lack of numerical data.
Thirteen studies (34 %) were rated ‘high’ on at least one of the three criteria. One study [45] that was rated ‘high’ on both success rate and weight loss, reported that 64 % of participants achieved 5 % weight loss goal with the average 12-month weight loss of 7.7 kg. This study was not only ‘highly’ effective but also had ‘high’ participation rates. The intervention included ‘high’ number of sessions with ‘moderate’ duration and ‘moderate’ fidelity. Another study [38] that had ‘high’ penetration into its target population appeared to be ‘highly’ effective based on the proportion of successful participants (50 %) and average weight loss (6.3 kg at 15 months). This study however, reported ‘low’ participation and delivered ‘high’ number of sessions and had ‘high’ duration of intervention.
Five out of six studies that reported ‘high’ weight loss delivered ‘high’ number of sessions.
Out of 10 studies that reported ‘moderate’ weight loss, 6 (60 %) implemented interventions with ‘low’ number of sessions/contacts. Sixteen (42 %) studies had ‘low’ effectiveness based on average weight loss, out of these, 8 (50 %) studies delivered ‘moderate’ number of sessions, whereas 4 (25 %) delivered ‘high’ and 4 (25 %) delivered ‘low’ number of sessions. Six studies reported ‘high’ effectiveness in risk reduction despite ‘low’ (4 studies) or ‘moderate’ (2 studies) effectiveness in weight loss, and these were also all studies with only ‘low’ (4 studies) or ‘moderate’ (2 studies) frequency, but with ‘high’ duration (6 studies). See Table 3 and Additional file 2: Table S7 for more details.
Discussion
This is the first systematic review to evaluate the implementation of real-world diabetes prevention programs using the PIPE Impact Metric framework that deploys four highly relevant elements for monitoring program impact in real-world settings. As such, this review complements other recent reviews, e.g. Dunkley et al. 2014 [27], by providing a more detailed understanding of key factors underlying successful translation and implementation of diabetes prevention programs in real-world contexts. We have also defined the specific scope of services for calculating the overall costs of services being provided. From both an organizational and societal perspectives, these issues are important to consider since the relative costs and benefits of such services and programs are important determinants of their uptake and adoption. Our review of studies published over the last 15 years aims to identify the components of diabetes prevention programs with the highest population impact.
Our review highlights several important findings. First, confirming earlier reviews, our analysis demonstrates that lifestyle-focused diabetes prevention programs that have a ‘high’ degree of contact have more potential to achieve effective outcomes, especially when measured by weight loss. These programs have typically been based on the US-DPP model and have used a very structured protocol to maximize program fidelity. However, the problem with this approach is that in these studies, program participation tends to be quite low; and furthermore, none of these studies reported diabetes risk reduction.
Second, six of the studies showed different degrees of effectiveness for different outcomes. For example, diabetes risk reduction could be ‘high’ even when effectiveness in weight loss was ‘low’ or ‘moderate’. Surprisingly, these were all studies of ‘low’ or ‘moderate’ frequency, but ‘high’ duration. This could be very promising especially for settings where intervention resources are constrained but when large populations can be reached by such programs.
Third, we found that ‘high’ penetration into the target population with invitations to engage prospective participants in the program do not necessarily result in ‘high’ participation. However, three studies with ‘high’ penetration resulted in either ‘high’ weight loss or ‘high’ diabetes risk reduction. Hence, scalability of the program to reach a large audience appears to be an important ingredient for population-level impact.
In summary, while an intensive intervention plays an important role in achieving successful weight loss outcomes, highly scalable moderate- to low-frequency interventions appear to have major potential to achieve diabetes risk reduction in populations.
From a program implementation perspective, it is important to clearly define and estimate the size of the target population. Without a reasonable estimate of the size of the target population, there is a risk that the program will not be scalable or sustainable [33]. We found estimates of target populations to be reported by less than one third of included studies. Hence, it is possible that many of these programs were delivered to highly selected populations which limit their generalizability.
We used the US-DPP intervention as a benchmark to assess the intensity of dose-delivered (including frequency, duration, and fidelity) in our included studies. In order to deal with heterogeneity in the types of contacts, we constructed a framework to standardize the degree of contact based on number, length, and type. We found that many programs adopted a ‘low-’ to ‘moderately intense’ version, compared to the US-DPP intervention. In practice, this also means that many of the components were either omitted or modified from the original US-DPP curriculum. As stated earlier, we also note that ‘high’-frequency interventions with ‘high’ to ‘moderate’ duration and fidelity were associated with greater weight loss. This is consistent with a systematic review and meta-analysis by Dunkley et al. [27], where reviewers coded intervention content based on the recommendations for lifestyle interventions for the prevention of diabetes provided by both the European Guideline and Training Standard for Diabetes Prevention (IMAGE) project [51] and National Institute for Health and Care Excellence (NICE) [52] and found that adherence to guidelines on the content and delivery was significantly associated with a greater weight loss. Our findings on the potential of ‘low’ to ‘moderate’ frequency interventions with longer duration to achieve significant risk reduction support earlier findings [25, 26]. A recent CPSTF review [28] shows lower weight loss than the US-DPP but still concluded strong evidence of effectiveness. The recommendations from this review were further supported by an effectiveness and economic review [53, 54]. So, in general, it seems that studies beyond the original US-DPP generate somewhat lower effect for weight loss but still generate meaningful positive impact on the reduction of incidence of T2DM. Lindstrom et al. have also previously discussed the positive effects of decreased fat and increased fibre intake on diabetes risk reduction in the absence of weight loss [55]. We also know that in many populations diabetes risk can be high at lower levels of weight, with other factors besides weight loss playing a critical role in risk reduction [56, 57].
Examining the implementation component further, in calculating ‘frequency’, we have used contacts made in the initial 12 months only because most of the studies did not extend beyond 12 months. In those that did, the initial 12 months can be considered as the ‘action’ phase, bringing about the lifestyle changes, and beyond that is a follow-up and maintenance phase, which some studies support with less frequent contacts.
In translational research, a systematic evaluation of program fidelity is important to assess the extent to which program was implemented as designed. We based our definition of fidelity on whether a standard curriculum was used to guide the delivery of intervention and whether quality assurance measures were placed to monitor the implementation of the intervention. Not many studies clearly reported whether the quality assurance measures were able to guarantee ‘high’ fidelity, this clearly being one of the next important steps in program development. This needs to be examined in future studies.
All but three studies in our review reported participation, and only seven studies scored ‘high’ on participation rates. The high participation may be a reflection of highly targeted penetration, but because of unavailability of information, we could not calculate penetration coefficients for any of these seven studies. However, the information available suggests that the studies where high-risk participants were identified and referred through their GPs or nurses resulted in ‘high’ participation rates, underlying the important role of providers. The high participation could also be a reflection of high motivation for change among at-risk individuals, a factor that the providers can further enhance in face-to-face contact, e.g. by applying strategies from motivational interviewing [58]. In our review, of the seven studies that scored ‘high’ for participation, five studies reported ‘high’ to ‘moderate’ effectiveness based on success rate and/or weight loss.
The PIPE Impact Metric elements are interrelated in that participation is always a proportion of penetration and effectiveness can only be attributed to those who participated. Effectiveness, in this context, is defined as the number or proportion of participating cases who reached a priori defined success criterion. In prevention of T2DM, diabetes risk reduction is one such success criterion. In many studies, however, weight loss was also a main outcome—either in individual cases as a percentage of overall body weight or across a population as an average percentage of weight loss. In our review, we used either criterion—diabetes risk reduction or weight loss—to assess effectiveness.
We found that weight loss was reported in several different ways. For example, the percentage weight lost could be interpreted to mean weight loss to percentage achieving a particular weight loss target or the average percentage of weight that subject lost. One study [45] reported both 5 and 7 % weight loss, whereas another [40] reported the proportion of successful participants who achieved at least 3 % weight loss. For consistency, in our review, we only used 5 % weight loss when it was reported in several different ways.
However, examination of studies with ‘low’ effectiveness reveals that for some of the studies the reported changes in weight loss were very small. Some of these studies reported a significant reduction in weight following the active intervention phase, but the weight was partly or, in some studies, entirely regained by the end of 12 months. Lack of consistency in the way weight loss outcomes are reported and analysed needs to be addressed in future translational research [29]. Cardona-Morrell and colleagues [21] suggests the establishment of a registry of translational projects using consistent, measurable outcomes to add more certainty to effectiveness analyses.
Our review includes diabetes prevention translational programs published since 2001 and until 2015. The studies included in this review have implemented ‘high’ (34 %), ‘moderate’ (37 %), and ‘low’ (29 %) frequency interventions; however, we noticed that most of the ‘low-frequency’ interventions were conducted in earlier years, whereas, designing ‘moderate’ to ‘high’ intensity interventions occurred in more recent years. However, ‘participation’ has been consistently low in a majority of the studies over the last 15 years. One of the reasons for this may be the fact that program planners focus on the content of the interventions instead of balancing the content with the experience of the participant—that is, on the ‘participation’ dimension and the engagement factor that connects the participant with the intervention.
Future translational research in this field needs to invest in designing recruitment more carefully to ensure high program reach; examining factors that optimize engagement and retention in the structured lifestyle programs; and maximizing adherence to the long-term behaviour changes [59].
Limitations
Several studies did not provide relevant numeric data to allow the calculation of PIPE coefficients. Hence we were unable to compare the overall program impact of the included studies. Additionally, any successfully translated diabetes program should ideally be accessible to those most in need and should have some clear relationship with the health care delivery system, and we were not able to evaluate these two elements in most of the studies included in this review.
In our analysis of implementation, we only considered standard sessions and have not included the extracurricular or optional activities offered by some of the programs that may have impact on the future adoption of these kinds of programs. This was mainly due to the heterogeneity in how the extracurricular activities were organized and also how they were reported. However, we do acknowledge that these ‘spinoff’ activities are likely to be very important for sustainability and the wider diffusion of programs, their maintenance, and sustainability.
Although there has been a lot of emphasis on the need for translating T2DM programs in low and middle income countries where the majority of people in the world at high risk of diabetes and its progression live [60], we did not find any studies from such countries that met our eligibility criteria. The Kerala Diabetes Prevention Program [61] in India is one of the first such implementation trials to evaluate a peer-led, group-based lifestyle intervention program (based on the Finnish GOAL study) [41] among individuals at high risk of developing T2DM in rural India. The trial is currently being implemented and will provide important reference to the translation of diabetes prevention programs in India and similar countries.
Also, we did not find any studies that have previously utilized the PIPE Impact Metric framework in diabetes prevention. More research is needed to understand and apply the few but essential elements of the PIPE model to measure the overall public health impact of diabetes prevention interventions.
Implications for practice
The original US-DPP [2] and Finnish-DPS [3] efficacy trials demonstrated that lifestyle intervention is an effective way to reduce the risk of T2DM in high-risk adults. However, achieving better translation of these programs still remains challenging after 15 years of research. Our findings suggest that program planners and implementers should aim to design high-intensity program with frequent contacts if the primary target is weight loss. However, if the primary aim is diabetes risk reduction, this can also be achieved with lower frequency of contacts but with a program duration of at least 12 months. With this program design, program planners should expect only low or moderate weight loss. To have a broader public health impact, programs with lower frequency of contacts but with a program duration of at least 12 months might be more feasible but this requires program strategies that simultaneously address both penetration and participation. Future translational research needs to identify effective recruitment and program implementation strategies for targeting both reach and program participation that also emphasizes long-term program adherence.
To improve the translation of diabetes prevention programs in real-world settings, we suggest a more rigorous reporting of program elements and components to evaluate these programs to assess the practical value [27] of the diabetes prevention programs. In particular, more detailed reporting on the four key PIPE Metric components will provide important insights and has the potential to facilitate increased uptake of T2DM prevention programs worldwide. We also suggest a greater consistency of reporting main outcomes and a standardization of reporting criteria for translational diabetes prevention programs implemented in real-world settings.
Conclusions
Our findings based on program implementation over the period of 15 years suggest that while a high-frequency intervention plays an important role in achieving high weight loss outcomes, programs with ‘low’-intense interventions have also shown high reductions in the incidence of T2DM. This suggests that even when the effectiveness of an intervention is moderate in terms of weight loss, it can have a profound impact on the development of a disease at the population level—provided enough effort is put into guaranteeing high penetration and participation as well. From a translation perspective, not many studies provide the necessary information to estimate the overall impact of such programs. Key elements of the PIPE Impact Metric are not routinely reported in many published implementation trials of diabetes prevention which therefore reduces their utility for information resource allocation and ‘real-world’ implementation. More rigorous evaluation methods are required to better understand the factors that influence the likely success of such interventions in the future.
References
International Diabetes Federation. IDF diabetes atlas. 6th ed. Brussels: International Diabetes Federation; 2013. http://www.idf.org/diabetesatlas.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine. 2002;346(6):393–403.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. The New England journal of medicine. 2001;344(18):1343–50.
Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and diabetes study. Diabetes care. 1997;20(4):537–44.
Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V, et al. The Indian diabetes prevention programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49(2):289–97.
Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. The Lancet. 2009;374(9702):1677–86.
Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing diabetes prevention study: a 20-year follow-up study. Lancet. 2008;371(9626):1783–9.
Peters DH, Adam T, Alonge O, Agyepong IA, Tran N. Implementation research: what it is and how to do it. Bmj. 2013;347:f6753.
Jensen D. In: Given LM, editor. “Transferability.” The SAGE encyclopedia of qualitative research methods. Thousand Oaks: SAGE Publications, Inc; 2008. p. 887. SAGE knowledge. Web. 12 Mar. 2015.
Yates T, Davies M, Khunti K. Preventing type 2 diabetes: can we make the evidence work? Postgraduate medical journal. 2009;85(1007):475–80.
Yamaoka K, Tango T. Efficacy of lifestyle education to prevent type 2 diabetes: a meta-analysis of randomized controlled trials. Diabetes care. 2005;28(11):2780–6.
Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. Bmj. 2007;334(7588):299.
Orozco LJ, Buchleitner AM, Gimenez-Perez G, Roque IFM, Richter B, Mauricio D. Exercise or exercise and diet for preventing type 2 diabetes mellitus. The Cochrane database of systematic reviews. 2008;3:CD003054.
Angermayr L, Melchart D, Linde K. Multifactorial lifestyle interventions in the primary and secondary prevention of cardiovascular disease and type 2 diabetes mellitus—a systematic review of randomized controlled trials. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2010;40(1):49–64.
Baker MK, Simpson K, Lloyd B, Bauman AE, Singh MA. Behavioral strategies in diabetes prevention programs: a systematic review of randomized controlled trials. Diabetes research and clinical practice. 2011;91(1):1–12.
Gillett M, Royle P, Snaith A, Scotland G, Poobalan A, Imamura M, et al. Non-pharmacological interventions to reduce the risk of diabetes in people with impaired glucose regulation: a systematic review and economic evaluation. Health technology assessment. 2012;16(33):1–236. iii-iv.
Schellenberg ES, Dryden DM, Vandermeer B, Ha C, Korownyk C. Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Annals of internal medicine. 2013;159(8):543–51.
Terranova CO, Brakenridge CL, Lawler SP, Eakin EG, Reeves MM. Effectiveness of lifestyle-based weight loss interventions for adults with type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2015;17(4):371–8. doi: 10.1111/dom.12430. Epub 2015 Jan 14.
Stevens JW, Khunti K, Harvey R, Johnson M, Preston L, Woods HB, et al. Preventing the progression to type 2 diabetes mellitus in adults at high risk: a systematic review and network meta-analysis of lifestyle, pharmacological and surgical interventions. Diabetes Res Clin Pract. 2015;107(3):320–31. doi: 10.1016/j.diabres.2015.01.027. Epub 2015 Jan 21.
Yuen A, Sugeng Y, Weiland TJ, Jelinek GA. Lifestyle and medication interventions for the prevention or delay of type 2 diabetes mellitus in prediabetes: a systematic review of randomised controlled trials. Australian and New Zealand journal of public health. 2010;34(2):172–8.
Cardona-Morrell M, Rychetnik L, Morrell SL, Espinel PT, Bauman A. Reduction of diabetes risk in routine clinical practice: are physical activity and nutrition interventions feasible and are the outcomes from reference trials replicable? A systematic review and meta-analysis. BMC public health. 2010;10:653.
Taylor J, Cottrell C, Chatterton H, Hill J, Hughes R, Wohlgemuth C, et al. Identifying risk and preventing progression to type 2 diabetes in vulnerable and disadvantaged adults: a pragmatic review. Diabetic medicine : a journal of the British Diabetic Association. 2013;30(1):16–25.
Li R, Zhang P, Barker LE, Chowdhury FM, Zhang X. Cost-effectiveness of interventions to prevent and control diabetes mellitus: a systematic review. Diabetes care. 2010;33(8):1872–94.
Jackson L. Translating the diabetes prevention program into practice: a review of community interventions. The Diabetes educator. 2009;35(2):309–20.
Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the diabetes prevention program? Health affairs. 2012;31(1):67–75.
Johnson M, Jones R, Freeman C, Woods HB, Gillett M, Goyder E, et al. Can diabetes prevention programmes be translated effectively into real-world settings and still deliver improved outcomes? A synthesis of evidence. Diabetic medicine : a journal of the British Diabetic Association. 2013;30(1):3–15.
Dunkley AJ, Bodicoat DH, Greaves CJ, Russell C, Yates T, Davies MJ, et al. Diabetes prevention in the real world: effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes and of the impact of adherence to guideline recommendations: a systematic review and meta-analysis. Diabetes care. 2014;37(4):922–33.
Pronk NP, Remington PL; Community Preventive Services Task Force. Combined diet and physical activity promotion programs for prevention of diabetes: community preventive services task force recommendation statement. Ann Intern Med. 2015; 163. doi:10.7326/M15-1029.
Whittemore R. A systematic review of the translational research on the diabetes prevention program. Translational behavioral medicine. 2011;1(3):480–91.
Glasgow RE. Evaluation of theory-based interventions: the RE-AIM model. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education. 3rd ed. San Francisco: Jossey-Bass; 2002. p. 531–44.
Laws RA et al. A systematic review of external validity in lifestyle interventions. Am J Prev Med. 2012;43(2):205–14.
Green LW, Glasgow RE. Evaluating the relevance, generalization, and applicability of research—issues in external validation and translation methodology. Eval Health Prof. 2006;29(1):126–53.
Pronk NP. Designing and evaluating health promotion programs: simple rules for a complex issue. Disease Management & Health Outcomes. 2003;11(3):149–57.
Zyriax BC, Letsch B, Stock S, Windler E. DELIGHT (delay of impaired glucose tolerance by a healthy lifestyle trial)—a feasibility study on implementing a program of sustainable diabetes prevention in German companies. Experimental and clinical endocrinology & diabetes: official journal, German Society of Endocrinology [and] German Diabetes Association. 2014;122(1):20–6.
Mensink M, Feskens EJ, Saris WH, De Bruin TW, Blaak EE. Study on lifestyle intervention and impaired glucose tolerance Maastricht (SLIM): preliminary results after one year. International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity. 2003;27(3):377–84.
Bo S, Ciccone G, Baldi C, Benini L, Dusio F, Forastiere G, et al. Effectiveness of a lifestyle intervention on metabolic syndrome. A randomized controlled trial. J Gen Intern Med. 2007;22(12):1695–703.
Lakerveld J, Bot S, Chinapaw M, van Tulder M, Kingo L, Nijpels G. Process evaluation of a lifestyle intervention to prevent diabetes and cardiovascular diseases in primary care. Health promotion practice. 2012;13(5):696–706.
Ma J, Yank V, Xiao L, Lavori PW, Wilson SR, Rosas LG, et al. Translating the diabetes prevention program lifestyle intervention for weight loss into primary care: a randomized trial. JAMA internal medicine. 2013;173(2):113–21.
Davis-Smith YM, Boltri JM, Seale JP, Shellenberger S, Blalock T, Tobin B. Implementing a diabetes prevention program in a rural African-American church. Journal of the National Medical Association. 2007;99(4):440–6.
Costa B, Barrio F, Cabre JJ, Pinol JL, Cos X, Sole C, et al. Delaying progression to type 2 diabetes among high-risk Spanish individuals is feasible in real-life primary healthcare settings using intensive lifestyle intervention. Diabetologia. 2012;55(5):1319–28.
Absetz P, Valve R, Oldenburg B, Heinonen H, Nissinen A, Fogelholm M, et al. Type 2 diabetes prevention in the “real world”: one-year results of the GOAL implementation trial. Diabetes Care. 2007;30(10):2465–70.
Nilsen V, Bakke PS, Gallefoss F. Effects of lifestyle intervention in persons at risk for type 2 diabetes mellitus—results from a randomised, controlled trial. BMC public health. 2011;11:893.
Penn L, Lordon J, Lowry R, Smith W, Mathers JC, Walker M, et al. Translating research evidence to service provision for prevention of type 2 diabetes: development and early outcomes of the ‘new life, new you’ intervention. British Journal of Diabetes and Vascular Disease. 2011;11(4):175–81.
Savas LA, Grady K, Cotterill S, Summers L, Boaden R, Gibson JM. Prioritising prevention: implementation of IGT care call, a telephone based service for people at risk of developing type 2 diabetes. Primary care diabetes. 2015;9(1):3–8.
Vanderwood KK, Hall TO, Harwell TS, Butcher MK, Helgerson SD, Montana Cardiovascular D, et al. Implementing a state-based cardiovascular disease and diabetes prevention program. Diabetes Care. 2010;33(12):2543–5.
Janus ED, Best JD, Davis-Lameloise N, Philpot B, Hernan A, Bennett CM, et al. Scaling-up from an implementation trial to state-wide coverage: results from the preliminary Melbourne diabetes prevention study. Trials. 2012;13:152.
Sepah SC, Jiang L, Peters AL. Translating the diabetes prevention program into an online social network: validation against CDC standards. The Diabetes educator. 2014;40(4):435–43.
Kumanyika S, Fassbender J, Phipps E, Tan-Torres S, Localio R, Morales KH, et al. Design, recruitment and start up of a primary care weight loss trial targeting African American and Hispanic adults. Contemporary Clinical Trials. 2011;32(2):215–24.
Duijzer G, Haveman-Nies A, Jansen SC, ter Beek J, Hiddink GJ, Feskens EJ. Feasibility and potential impact of the adapted SLIM diabetes prevention intervention in a Dutch real-life setting: the SLIMMER pilot study. Patient education and counseling. 2014;97(1):101–7.
Kanaya AM, Santoyo-Olsson J, Gregorich S, Grossman M, Moore T, Stewart AL. The live well, be well study: a community-based, translational lifestyle program to lower diabetes risk factors in ethnic minority and lower-socioeconomic status adults. Am J Public Health. 2012;102(8):1551–8.
Paulweber B, Valensi P, Lindstrom J, et al. A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res. 2010;42 Suppl 1:S3–36.
National Institute for Health and Clinical Excellence. Preventing type 2 diabetes: risk identification and interventions for individuals at high risk. London: National Institute for Health and Clinical Excellence; 2012.
Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL, Task Force on Community Preventive Services. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the community preventive services task force. Ann Intern Med. 2015;163(6):437–51 doi: 10.7326/M15-0452.
Li R, Qu S, Zhang P, Chattopadhyay S, Gregg EW, Albright A, Hopkins D, Pronk NP, [Task Force on Community Preventive Services]. Economic evaluation of combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the community preventive services task force. Ann Intern Med. 2015; 163. doi:10.7326/M15-0469.
Lindstrom J, Peltonen M, Eriksson JG, Louheranta A, Fogelholm M, Uusitupa M, et al. High-fibre, low-fat diet predicts long-term weight loss and decreased type 2 diabetes risk: the Finnish diabetes prevention study. Diabetologia. 2006;49:912–20.
Yajnik CS, Lubree HG, Rege SS, Naik SS, Deshpande JA, Deshpande SS, et al. Adiposity and hyperinsulinemia in Indians are present at birth. The Journal of clinical endocrinology and metabolism. 2002;87(12):5575–80.
Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. Jama. 2009;301(20):2129–40.
Resnicow K, McMaster F. Motivational interviewing: moving from why to how with autonomy support. The international journal of behavioral nutrition and physical activity. 2012;9:19.
Spring B, Sohn MW, Locatelli SM, Hadi S, Kahwati L, Weaver FM. Individual, facility, and program factors affecting retention in a national weight management program. BMC public health. 2014;14:363.
Daivadanam M, Absetz P, Sathish T, Thankappan KR, Fisher EB, Philip NE, et al. Lifestyle change in Kerala, India: needs assessment and planning for a community-based diabetes prevention trial. Bmc Public Health. 2013;13:95.
Sathish T, Williams ED, Pasricha N, Absetz P, Lorgelly P, Wolfe R, et al. Cluster randomised controlled trial of a peer-led lifestyle intervention program: study protocol for the Kerala diabetes prevention program. BMC public health. 2013;13:1035.
Kosaka K, Noda M, Kuzuya T. Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes research and clinical practice. 2005;67(2):152–62.
Oldroyd JC, Unwin NC, White M, Mathers JC, Alberti KG. Randomised controlled trial evaluating lifestyle interventions in people with impaired glucose tolerance. Diabetes Res Clin Pract. 2006;72(2):117–27.
Laatikainen T, Dunbar JA, Chapman A, Kilkkinen A, Vartiainen E, Heistaro S, et al. Prevention of type 2 diabetes by lifestyle intervention in an Australian primary health care setting: greater green triangle (GGT) diabetes prevention project. Bmc Public Health. 2007;7:249.
Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the diabetes prevention program into the community. The DEPLOY pilot study. American Journal of Preventive Medicine. 2008;35(4):357–63.
Boltri JM, Davis-Smith YM, Seale JP, Shellenberger S, Okosun IS, Cornelius ME. Diabetes prevention in a faith-based setting: results of translational research. Journal of Public Health Management and Practice. 2008;14(1):29–32.
Payne WR, Walsh KJ, Harvey JT, Livy MF, McKenzie KJ, Donaldson A, et al. Effect of a low-resource-intensive lifestyle modification program incorporating gymnasium-based and home-based resistance training on type 2 diabetes risk in Australian adults. Diabetes Care. 2008;31(12):2244–50.
Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, et al. Translating the diabetes prevention program. A comprehensive model for prevention training and program delivery. American Journal of Preventive Medicine. 2009;37(6):505–11.
Kulzer B, Hermanns N, Gorges D, Schwarz P, Haak T. Prevention of diabetes self-management program (PREDIAS): effects on weight, metabolic risk factors, and behavioral outcomes. Diabetes Care. 2009;32(7):1143–6.
Penn L, White M, Oldroyd J, Walker M, Alberti KG, Mathers JC. Prevention of type 2 diabetes in adults with impaired glucose tolerance: the European Diabetes Prevention RCT in Newcastle upon Tyne, UK. BMC Public Health. 2009;9:342.
Almeida FA, Shetterly S, Smith-Ray RL, Estabrooks PA. Reach and effectiveness of a weight loss intervention in patients with prediabetes in Colorado. Preventing Chronic Disease. 2010;7(5):A103.
Makrilakis K, Liatis S, Grammatikou S, Perrea D, Katsilambros N. Implementation and effectiveness of the first community lifestyle intervention programme to prevent type 2 diabetes in Greece. The DE-PLAN study. Diabetic Medicine. 2010;27(4):459–65.
Parikh P, Simon EP, Fei K, Looker H, Goytia C, Horowitz CR. Results of a pilot diabetes prevention intervention in East Harlem, New York City: project HEED. American journal of public health. 2010;100 Suppl 1:S232–9.
Vermunt PW, Milder IE, Wielaard F, van Oers JA, Westert GP. An active strategy to identify individuals eligible for type 2 diabetes prevention by lifestyle intervention in Dutch primary care: the APHRODITE study. Family practice. 2010;27(3):312–9.
Boltri JM, Davis-Smith M, Okosun IS, Seale JP, Foster B. Translation of the National Institutes of Health diabetes prevention program in African American churches. Journal of the National Medical Association. 2011;103(3):194–202.
Gilis-Januszewska A, Szybinski Z, Kissimova-Skarbek K, Piwonska-Solska B, Pach D, Topor-Madry R, et al. Prevention of type 2 diabetes by lifestyle intervention in primary health care setting in Poland: diabetes in Europe prevention using lifestyle, physical activity and nutritional intervention (DE-PLAN) project. Br J Diabetes Vasc Dis. 2011;11(4).
Katula JA, Vitolins MZ, Rosenberger EL, Blackwell CS, Morgan TM, Lawlor MS, et al. One-year results of a community-based translation of the diabetes prevention program: healthy-living partnerships to prevent diabetes (HELP PD) project. Diabetes Care. 2011;34(7):1451–7.
Ruggiero L, Oros S, Choi YK. Community-based translation of the diabetes prevention program's lifestyle intervention in an underserved Latino population. Diabetes Educator. 2011;37(4):564–72.
Sakane N, Sato J, Tsushita K, Tsujii S, Kotani K, Tsuzaki K, et al. Prevention of type 2 diabetes in a primary healthcare setting: three-year results of lifestyle intervention in Japanese subjects with impaired glucose tolerance. BMC Public Health. 2011;11(1):40.
Ockene IS, Tellez TL, Rosal MC, Reed GW, Mordes J, Merriam PA, et al. Outcomes of a Latino community-based intervention for the prevention of diabetes: the Lawrence Latino diabetes prevention project. American Journal of Public Health. 2012;102(2):336–42.
Piatt GA, Seidel MC, Chen H-Y, Powell RO, Zgibor JC. Two-year results of translating the diabetes prevention program into an urban, underserved community. Diabetes Educator. 2012;38(6):798–804.
Jiang LH, Manson SM, Beals J, Henderson WG, Huang HX, Acton KJ, et al. Translating the diabetes prevention program into American Indian and Alaska native communities results from the special diabetes program for Indians diabetes prevention demonstration project. Diabetes Care. 2013;36(7):2027–34.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
The ratings of the included studies were independently derived by three authors (ZA, PA, JO). The ratings of all studies were then reviewed by all authors and when disagreement on rating occurred they were resolved with consensus among all authors. ZA drafted the manuscript. All authors read, provided feedback, and approved the final manuscript.
Authors’ information
Zahra Aziz MPH is a PhD candidate in the School of Population and Global Health University of Melbourne in Australia. Her PhD is on an evaluation of the translation of diabetes prevention programs in ‘real-world’ settings with a particular focus on the National Health and Medical Research Council (NHMRC) funded study titled the Kerala Diabetes Prevention program based in rural India. She is also involved in evaluating the Australasian Peers for Progress trial in Victoria, Australia. Before commencing her PhD, she has worked as an evaluation specialist with the Aga Khan Health Service, Pakistan for 5 years and has also completed a Master of Public Health degree from the University of Melbourne, Australia. She has led the conducting of this systematic review.
Pilvikki Absetz PhD is an Adjunct Professor of Health Promotion at University of Tampere, School of Health Sciences, Finland. She is a global expert in lifestyle interventions in prevention and management of type 2 diabetes and other chronic conditions. She has been a lead or co-investigator of the following major studies that are directly relevant to type 2 diabetes: the Finnish GOAL Lifestyle Implementation Trial; the TERVA tele health coaching intervention trial in Finland; the Greater Green Triangle DPP in Australia; the Peers for Progress trial for diabetes self-management in Australia; and the Kerala DPP in India. She is also involved in the European Community Horizon 2020 funded SMART2D project promoting cross learning in diabetes prevention and management in Sweden, South Africa, and Uganda.
John Oldroyd PhD is a research fellow in the Department of Epidemiology and Preventive Medicine, Monash University. His PhD was in lifestyle interventions for the prevention of diabetes in people with impaired glucose tolerance in the UK.
Nicolaas P. Pronk PhD is vice president and chief science officer at HealthPartners and a researcher in the HealthPartners Institute for Education and Research in Minneapolis, Minnesota, USA. He is also an adjunct professor of Social and Behavioral Sciences at the Harvard School of Public Health, Boston, MA. He undertakes research in the area of health behaviour change and population health. He developed the PIPE model that is used in our systematic review and is an expert in the evaluation of complex interventions.
Brian Oldenburg PhD is Professor and Chair of Non-Communicable Disease Control in the School of Population and Global Health, University of Melbourne, Australia. He is a behavioural scientist and an expert in the prevention and control of chronic conditions. His research program focuses on improving the prevention and control of cardiometabolic conditions such as diabetes, heart disease, and their co-morbidities in Australia and other countries.
Additional files
Additional file 1:
Search Strategy. Search strategy used for identifying included studies. (PDF 371 KB)
Additional file 2: Table S4–Table S7
Detailed scoring of all included studies based on the elements of the PIPE Impact Metric framework. (PDF 772 KB)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Aziz, Z., Absetz, P., Oldroyd, J. et al. A systematic review of real-world diabetes prevention programs: learnings from the last 15 years. Implementation Sci 10, 172 (2015). https://doi.org/10.1186/s13012-015-0354-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-015-0354-6