Abstract
Aims/hypothesis
The aim of this study was to investigate the association of dietary macronutrient composition and energy density with the change in body weight and waist circumference and diabetes incidence in the Finnish Diabetes Prevention Study.
Subjects and methods
Overweight, middle-aged men (n=172) and women (n=350) with impaired glucose tolerance were randomised to receive either ‘standard care’ (control) or intensive dietary and exercise counselling. Baseline and annual examinations included assessment of dietary intake with 3-day food records and diabetes status by repeated 75-g OGTTs. For these analyses the treatment groups were combined and only subjects with follow-up data (n=500) were included.
Results
Individuals with low fat (<median) and high fibre (>median) intakes lost more weight compared with those consuming a high-fat (>median), low-fibre (<median) diet (3.1 vs 0.7 kg after 3 years). In separate models, hazard ratios for diabetes incidence during a mean follow-up of 4.1 years were (highest compared with lowest quartile) 0.38 (95% CI 0.19–0.77) for fibre intake, 2.14 (95% CI 1.16–3.92) for fat intake, and 1.73 (95% CI 0.89–3.38) for saturated-fat intake, after adjustment for sex, intervention assignment, weight and weight change, physical activity, baseline 2-h plasma glucose and intake of the nutrient being investigated. Compared with the low-fat/high-fibre category, hazard ratios were 1.98 (95% CI 0.98–4.02), 2.68 (95% CI 1.40–5.10), and 1.89 (95% CI 1.09–3.30) for low-fat/low-fibre, high-fat/high-fibre, and high-fat/low-fibre, respectively.
Conclusions/interpretation
Dietary fat and fibre intake are significant predictors of sustained weight reduction and progression to type 2 diabetes in high-risk subjects, even after adjustment for other risk factors.
Similar content being viewed by others
Introduction
Recent trials have demonstrated that the risk of type 2 diabetes can be successfully reduced by lifestyle intervention [1, 2]. Weight loss and increased physical activity achieved as a result of the interventions are significant predictors of risk reduction [3]. However, it is obvious that weight reduction can only be achieved by lifestyle change—that is, either by increasing energy expenditure by physical activity or by decreasing dietary energy intake.
Reduction in energy intake can be achieved either by decreasing the total amount of food by portion size control, or by changing the composition of the diet towards lower energy density while maintaining the food quantity. Typically, fat increases while water and fibre decrease energy density [4]. There is some evidence claiming that high-fat diets promote energy excess and weight gain [5, 6]; however, the issue remains controversial [7]. Intake of dietary fibre has been shown to be inversely correlated with body weight and weight change [8]. In addition to their possible indirect effect on diabetes risk through body weight regulation, several dietary factors, such as high-fat [9, 10], high-saturated-fat [10, 11], and low-fibre intake [12–15], have been proposed as independent risk factors for type 2 diabetes.
We have previously shown that in overweight, middle-aged men and women with impaired glucose tolerance who participated in the Finnish Diabetes Prevention Study (DPS), intensive lifestyle intervention, compared with the ‘standard care’ control group, resulted in modest weight loss (4.5 vs 1.0 kg after 1 year) and a 58% reduction in diabetes risk [1, 16]. However, the independent effect of the dietary composition on weight change and risk for type 2 diabetes was not analysed. The aim of the present study was to utilise the DPS data to assess the association between dietary macronutrient composition, in particular dietary fat, fibre and energy density and change in body weight and waist circumference and diabetes risk.
Subjects and methods
Altogether, 522 individuals participated in the Finnish DPS. The study design has been described in detail previously [1, 16, 17]. According to the inclusion criteria, study subjects (172 men and 350 women) were middle-aged (40–64 years) and overweight (BMI>25 kg/m2) at baseline, and had impaired glucose tolerance according to WHO 1985 criteria [18]. All study subjects gave written informed consent and the study protocol was approved by the ethics committee of the National Public Health Institute, Helsinki, Finland. Individuals who did not participate in any annual follow-up visits by year 3 (n=15) or who had missing data on dietary intake at baseline (n=1) or during the follow-up (n=6) had to be excluded from the current analyses.
The study participants were advised to lose weight, increase physical activity and consume a moderate-fat (total fat<30% of energy [E%], saturated fat<10 E%), high-fibre (>15 g/1,000 kcal) diet. For the participants in the control group the lifestyle advice was given as ‘standard care counselling’ at baseline. The participants in the intensive intervention group were given individualised, detailed dietary counselling, with seven sessions during the first year and every 3 months thereafter [1, 16]. They were also offered free-of-charge supervised resistance-training-based physical activity sessions. In addition, altogether 48 of the participants in the intervention group chose to engage in a 2- to 5-week very-low-calorie diet (VLCD) phase to boost weight reduction.
The baseline and annual clinical examination included measurements of weight (in light indoor clothes to the nearest 100 g), height (without shoes to the nearest 1 mm), and waist circumference (midway between the lowest rib and iliac crest to the nearest 1 mm). BMI was calculated dividing the weight (kg) by the height (m) squared.
Questionnaires regarding medical history, exercise and dietary habits were collected at baseline and each annual visit. Subjects were classified as having a family history of diabetes if at least one parent had diabetes. Those who smoked on at least 5 days per week were categorised as regular smokers. Leisure time physical activity during the previous year was estimated using the validated Kuopio Ischaemic Heart Disease Risk Factor Study 12-month Leisure-Time Physical Activity questionnaire [19], and physical activity (min/week) at baseline and during the intervention period were added into the adjusted models as cofactors.
The study subjects completed a 3-day food record at baseline and before every annual study visit. They were asked to write down everything they ate and drank (except plain drinking water) using a picture booklet of portion sizes of typical foods as the reference. The completeness of the food records was checked at the face-to-face session with the study nutritionist during the study visit. The nutrient intakes were calculated with a dietary analysis programme developed at the National Public Health Institute [20] as E% values for energy-yielding nutrients and fibre density per 1,000 kcal. Food weight was calculated from the food records as total amount of foods and beverages consumed (g), excluding only drinking water and mineral water. Energy density was calculated by dividing energy (kcal) of food with food weight (100 g). The averaged intake during the year 1 (n=499), 2 (n=467) and 3 (n=424) was used in the analyses.
The annually measured biochemical parameters included fasting and 2-h post-challenge (75-g OGTT) plasma glucose after a 12-h fast. Plasma glucose was determined locally according to standard guidelines. The development of type 2 diabetes was the primary endpoint. Diabetes was defined according to the WHO 1985 criteria [18], i.e. either fasting plasma glucose ≥7.8 mmol/l or 2-h post-challenge plasma glucose ≥11.1 mmol/l. The diagnosis of diabetes had to be confirmed by a second OGTT. After the diagnosis of diabetes had been established, the subject was referred to his/her own physician for treatment, and the follow-up in the DPS was discontinued. A highly significant difference in the incidence of diabetes between the treatment groups was detected after 3.2 years of follow-up [1], and therefore the intervention phase was terminated prematurely after a mean duration of 3.9 years (range 0–6 years).
Statistical analyses were performed with the statistics package Stata (release 8.0; STATA, College Station, TX, USA). In all analyses of the present paper the two treatment groups were pooled, and the group assignment was used as a cofactor in the adjusted models. Weight and waist circumference change from baseline to year 3 was calculated by subtracting the value at year 0 from the value at year 3. The last-observation-carried-forward (LOCF) method was used in the calculations for those who were diagnosed with diabetes (n=53) or dropped out (n=18) before the 3-year visit.
Analysis of covariance (ANCOVA) and χ 2-tests were used to analyse the baseline and follow-up period differences between those who developed diabetes during the follow-up and those who did not. The ANCOVA adjusting for group assignment, age, VLCD-use as part of the intensive intervention (adjusted to ‘not used’), physical activity at baseline and during the follow-up period, and baseline weight and nutrient intakes, was used to analyse the associations of quartiles of dietary intake during the follow-up with weight and waist circumference changes. Adjustment for the baseline intake of the nutrient in question was used to control for regression-to-the-mean effect, since those who report extreme intakes are, due to intra-individual variation, likely to report less extreme intakes at follow-up. Trends across the quartiles were analysed by adding the quartile into the model as a continuous variable.
The Cox model was used to calculate the hazard ratios (HRs) for developing diabetes between quartiles of dietary intake, with the lowest quartile as the reference category. These analyses were adjusted for group assignment, sex, age, physical activity at baseline and during the follow-up period, baseline weight, baseline nutrient intake, and the baseline 2-h post-challenge plasma glucose, and in further analyses, with the weight change from baseline to year 3.
To clarify the combined effect of dietary fat E% and fibre density, participants were divided into low- (below median) and high- (above median) intake groups. Between these categories, ANCOVA was used to analyse effects on the weight reduction and the Cox model to analyse effects on diabetes risk. In all analyses p<0.05 was considered statistically significant.
Results
At baseline, mean (±SD) age of the study participants was 55±7 years, mean BMI was 31±4 kg/m2, mean fasting plasma glucose was 6.1±0.7 mmol/l and mean plasma glucose 2 h after glucose load was 8.9±1.5 mmol/l. Cholesterol-lowering drugs were used by 5% and blood pressure-lowering drugs by 29% of the participants. A family history of diabetes was common: 63% of the participants had at least one parent with diabetes. Only 5% were regular smokers.
After a mean follow-up of 4.1 years, 114 of the 500 participants had been diagnosed with diabetes. Those who developed diabetes were more obese at baseline, measured as weight, BMI or waist circumference, and they had higher fasting and 2-h plasma glucose values (Table 1). The individuals who remained free of diabetes lost more weight and reduced their waist circumference more, also after adjustment for sex, group assignment and baseline value of obesity (BMI, weight or waist circumference), and they did not experience deterioration of glucose values during the first 3 years of the study.
Subjects who were diagnosed with diabetes tended to consume a diet with lower carbohydrate and fibre content, and also higher in alcohol at baseline (Table 2). The reported alcohol consumption (2–3 E%) was, however, low throughout the study. Among those who remained free of diabetes, E% of carbohydrates and fibre density increased further, and energy proportions of total, saturated and mono-unsaturated fat, and intake of cholesterol decreased compared with those who were diagnosed with diabetes during the study.
In separate models, fibre density, fat E% and energy density of the diet during the follow-up were associated with weight reduction, after adjustment for group assignment, sex, physical activity, VLCD-use, baseline weight and baseline nutrient intake (Table 3). Weight loss was related to an increase in fibre (p for trend=0.001) and decrease in fat (p for trend=0.018) and energy density (p for trend=0.001). Fibre density of the diet was inversely associated with the change in waist circumference even after adjustment for weight change (p for trend=0.033).
A total of 147 (29%) of the study subjects had lost 5% or more of their baseline weight at year 3. Fibre density, fat E%, saturated fat E% and energy density were separately associated with sustained >5% weight reduction, after adjustments for potential confounders. The most significant dietary predictor for achieving large weight reduction was energy density, the multivariate adjusted odds ratio being 0.19 (95% CI 0.08–0.41) in the highest compared with the lowest quartile (Table 4).
HRs for diabetes incidence by quartiles of dietary intakes are given in Table 5. In the analysis adjusted for group assignment, sex, age, baseline weight, baseline 2-h glucose, physical activity and baseline intake, higher fibre density (p for trend=0.01) and lower fat intake (p for trend=0.004) were associated with a reduced diabetes risk. Further adjustment for weight change during the trial did not affect the results notably. When both fat and fibre were simultaneously entered into the same adjusted prediction model, due to multicollinearity (r=0.60) neither was a significant predictor for diabetes: the HR was 0.88 (95% CI 0.68–1.16) according to increasing fibre density quartile and 1.23 (95% CI 0.95–1.58) according to increasing fat E% quartile.
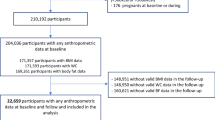
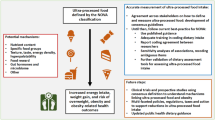
The adjusted 3-year weight reduction among those whose diet was both low in fat and high in fibre was 3.1 kg (95% CI 2.3–3.9 kg) (Fig. 1). Among the subjects whose diet was high in fat and low in fibre, weight reduction was significantly less at 0.7 kg (95% CI for weight change −1.7 to +0.1 kg). Compared with low-fat/high-fibre diet, the HR for diabetes was 1.98 (95% CI 0.98–4.02, p=0.06) in the low-fat/low-fibre category, 2.68 (95% CI 1.40–5.10, p=0.003) in the high-fat/high-fibre category and 1.89 (95% CI 1.09–3.30, p=0.024) in the high-fat/low-fibre category (Fig. 2).
Mean (white bars) and adjusted (grey bars) weight change (95% CIs) from baseline to year 3 (LOCF) by fibre (cut-off point median 13.0 g/1,000 kcal) and fat (cut-off point median 33.15 E%) intake (mean of years 1–3). Adjusted mean is calculated with ANCOVA adjusting for group assignment, VLCD-use, age, sex, baseline weight, baseline fat and fibre intake, and baseline and follow-up period physical activity
Hazard ratios (95% CIs) for diabetes by fibre (cut-off point median 13.0 g/1,000 kcal) and fat (cut-off point median 33.15 E%) intake (mean of years 1–3). Model 1 (white bars): no adjustment. Model 2 (grey bars): adjusted for group assignment, sex, age, baseline weight, baseline 2-h glucose, physical activity at baseline and during follow-up period, and baseline fat and fibre intake. Model 3 (black bars): adjusted also for weight change
Discussion
We used the DPS data to assess the association between dietary composition and change in weight and diabetes risk. The analyses revealed that a decrease in dietary fat and energy density and an increase in fibre density were associated with sustained weight reduction in a dose-dependent manner. Furthermore, low-fat and high-fibre intakes predicted decreased diabetes risk independently of body weight change and physical activity.
A debate about optimal diet for weight reduction prevails. Studies with strictly controlled energy intake have shown that weight reduction can be achieved with any dietary regimen as long as energy intake is lower than energy expenditure [21–24]. Permanently reduced energy intake, which is essential after weight reduction unless energy expenditure by physical activity is clearly increased, is more difficult to achieve [25]. Our results offer support for the validity of the current recommendations to reduce fat and increase fibre-rich carbohydrate intake, to achieve sustained long-term weight reduction.
Reduction of fat intake has for several decades been the conventional approach for weight control. According to a review by Astrup et al. [26], a 4–5 kg weight loss can be achieved with 10 E% reduction in dietary fat in obese individuals, at least in short-term (<1 year) studies. Fat contains more energy per gram than other energy-yielding nutrients and also makes the diet palatable, but simultaneously less satiating, and therefore a high-fat diet is believed to promote weight gain [5, 6]; however the issue is controversial [7]. In recent studies [27–29] a low-carbohydrate diet resulted in more pronounced short-term weight reduction compared with a conventional low-energy, low-fat dietary regimen, probably because the achieved energy deficit was larger. However, the statistically significant difference in early weight loss between the groups disappeared at 12 months [27, 30, 31], indicating that individuals are not able to adhere to such a restricted diet. Moreover, the long-term safety of low-carbohydrate diets in weight-stable individuals is not known [32].
Still another popular, and evidently efficient [22, 31] weight-loss approach is to increase protein intake up to 30% of total energy, with a decrease in either fat or carbohydrate. An increase in protein intake may increase patient satisfaction during a low-fat, energy-restricted diet [22] and has been shown to accelerate weight loss [33] and prevent weight regain [34]. In our study we emphasised adequate protein intake (0.8 g/1 kg body weight) but did not advise to increase it more than that. It is impossible to say whether advocating an increase in protein would have led to larger weight reduction than was achieved in our study. We did, however, also analyse the association of the protein intake (E%) quintile with weight reduction and diabetes incidence, but did not see any significant effects (data not shown).
The intake of dietary fibre has been shown to be inversely correlated with body weight and weight reduction [8, 35, 36]. Fibre may increase satiation directly by increasing gastric distension and thereby giving a feeling of fullness, or indirectly through secretion of gut hormones (incretins), and satiety through delaying gastric emptying and nutrient absorption. Furthermore, fibre may decrease dietary energy intake by reducing absorption of fat and protein [8]. In the present study an increase in dietary fibre intake was also associated with a reduced waist circumference, independently of weight change. A similar finding was previously seen in an observational study on American male health professionals [37]. The mechanism explaining the inverse association between waist circumference and fibre intake is not clear. The effect of dietary fibre may be mediated by changes in insulin resistance. High-fibre intake has been shown to be associated with enhanced insulin sensitivity [38–40]. On the other hand, insulin resistance may, as discussed by Kahn and Flier [41] contribute to the development of obesity. Smoking is known to increase central obesity [42]. In our study, smoking was remarkably uncommon, and thus did not confound the association between fibre intake and waist circumference. The low rate of smoking may be explained by the fact that the study participants were volunteers and probably more health-conscious than the general population.
A recently recognised factor potentially influencing nutrient intake is the energy density of the diet [43]. People have been shown to be only partly able to compensate for changes in dietary energy density by increasing or decreasing the total amount of food, at least in short-term clinical studies [44, 45]. In our analysis, dietary energy density was highly significantly associated with sustained weight reduction; on the other hand, energy density is a composite factor of dietary fat, fibre and water. Weight reduction among the low-fat/high-fibre consumers was threefold compared with the high-fat/low-fibre group, indicating that to achieve the best results one should make extensive changes in dietary pattern, rather than focusing on any single nutrient.
Obesity is a well-established risk factor for type 2 diabetes, and we have previously shown that in the DPS population diabetes risk was reduced dose-dependently with weight reduction [46]. Obesity increases insulin resistance, and in a subgroup analysis of the DPS study population a strong inverse correlation was found between the 4-year weight change and insulin sensitivity [47]. In addition, according to the present analyses the composition of the diet affected diabetes risk independently of weight change. Several epidemiological studies have shown that low intake of total fat [9, 10], saturated fat [10, 11] and high intake of cereal, cereal fibre and total fibre [12–15], are associated with decreased diabetes risk during the follow-up period. In most of these studies, dietary changes during the follow-up period were typically not taken into account. In our study, the participants were advised to make changes in their diet, and dietary intake was monitored continually. Furthermore, the association between nutrient intakes during the follow-up and diabetes risk was adjusted for baseline nutrient intakes.
Type of fat (namely, high saturated and trans-fatty acid and low unsaturated fatty acid intake), rather than total fat intake, has in several studies been associated with increased diabetes risk [48]. In our study the total and saturated fat intakes were highly correlated (r=0.81) and the intake of mono-unsaturated fat remained relatively stable throughout the study. Furthermore, the intake of trans-fatty acids was low, on average 0.7 E% (data not shown). This might explain why total fat intake was the fat-related variable most consistently associated with diabetes risk in our analyses.
Our study, like dietary intake trials in general, has several limitations. The dietary intervention was planned to encourage an increase in dietary fibre and a decrease in fat intake, and it is possible that individuals who succeeded in weight reduction were more likely to report consuming ‘the recommended diet’. In addition to dietary changes, the participants were advised to increase physical activity. Therefore, all the models to investigate the effect of dietary composition were adjusted for physical activity at baseline and during the intervention, but some residual confounding might remain. Furthermore, the energy intakes calculated from the food records revealed that under-reporting had taken place. However, this may not be too problematic, because we calculated energy proportions of nutrients and not absolute amounts. Overweight and obese people are known to be even more prone to dietary under-reporting than normal-weight individuals. Such an under-reporting has been shown to be a stable characteristic of an individual [49], and as the results were adjusted for the baseline, it may not cause a bias in our study. Changes in specific dietary intakes were correlated: those who decreased fat-containing foods increased carbohydrate- and fibre-containing foods, and simultaneously the energy density of the diet decreased. This real-life phenomenon is problematic in statistical analyses. When the predictors entered into a model simultaneously have multicollinearity, they tend to attenuate each other, as also shown in our data. Therefore, instead of calculating one model including all dietary variables, we used separate models, and selected the two most significant predictors for the combined analysis. The highest diabetes risk was seen among the high-fat/high-fibre and not, as would have been expected, among the high-fat/low-fibre consumers. The HRs, however, did not differ statistically significantly and thus the effect may be coincidental, or due to confounding by some unknown factors.
We have shown that a long-term weight reduction during the Finnish DPS was best achieved by reducing energy density and dietary fat and increasing fibre intake. As for the long-term health benefits, our results strongly support the validity of the current dietary recommendations to the general population: reducing the intake of saturated fat and increasing fibre-rich whole-grain cereals and fruit and vegetables, is important, not only in terms of overall health but also for sustained weight reduction and the prevention of type 2 diabetes in overweight individuals.
Abbreviations
- ANCOVA:
-
analysis of covariance
- DPS:
-
Diabetes Prevention Study
- E%:
-
energy proportion
- HR:
-
hazard ratio
- LOCF:
-
last-observation-carried-forward
- VLCD:
-
very-low-calorie diet
References
Tuomilehto J, Lindström J, Eriksson JG et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350
The Diabetes Prevention Program Research Group (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403
Laaksonen DE, Lindström J, Lakka TA et al (2005) Physical activity in the prevention of type 2 diabetes: the Finnish Diabetes Prevention Study. Diabetes 54:158–165
Poppitt SD (1995) Energy density of diets and obesity. Int J Obes Relat Metab Disord 19(Suppl 5):S20–S26
Blundell JE, Lawton CL, Cotton JR, Macdiarmid JI (1996) Control of human appetite: implications for the intake of dietary fat. Annu Rev Nutr 16:285–319
Bray GA, Popkin BM (1998) Dietary fat intake does affect obesity! Am J Clin Nutr 68:1157–1173
Willett WC (2002) Dietary fat plays a major role in obesity: no. Obes Rev 3:59–68
Howarth NC, Saltzman E, Roberts SB (2001) Dietary fiber and weight regulation. Nutr Rev 59:129–139
Marshall JA, Hamman RF, Baxter J (1991) High-fat, low-carbohydrate diet and the etiology of non-insulin-dependent diabetes mellitus: the San Luis Valley Diabetes Study. Am J Epidemiol 134:590–603
van Dam RM, Willett WC, Rimm EB, Stampfer MJ, Hu FB (2002) Dietary fat and meat intake in relation to risk of type 2 diabetes in men. Diabetes Care 25:417–424
Meyer KA, Kushi LH, Jacobs DR Jr, Folsom AR (2001) Dietary fat and incidence of type 2 diabetes in older Iowa women. Diabetes Care 24:1528–1535
Meyer KA, Kushi LH, Jacobs DR Jr, Slavin J, Sellers TA, Folsom AR (2000) Carbohydrates, dietary fiber, and incident type 2 diabetes in older women. Am J Clin Nutr 71:921–930
Salmeron J, Manson JE, Stampfer MJ, Colditz GA, Wing AL, Willett WC (1997) Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA 277:472–477
Stevens J, Ahn K, Juhaeri, Houston D, Steffan L, Couper D (2002) Dietary fiber intake and glycemic index and incidence of diabetes in African–American and white adults: the ARIC study. Diabetes Care 25:1715–1721
Montonen J, Knekt P, Järvinen R, Aromaa A, Reunanen A (2003) Whole-grain and fiber intake and the incidence of type 2 diabetes. Am J Clin Nutr 77:622–629
Lindström J, Louheranta A, Mannelin M et al (2003) The Finnish Diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 26:3230–3236
Eriksson J, Lindström J, Valle T et al (1999) Prevention of type II diabetes in subjects with impaired glucose tolerance: the Diabetes Prevention Study (DPS) in Finland. Study design and 1-year interim report on the feasibility of the lifestyle intervention programme. Diabetologia 42:793–801
World Health Organization (1985) Diabetes mellitus: report of a WHO Study Group. In: Technical report series No. 727. Geneva
Lakka TA, Salonen JT (1992) Intra-person variability of various physical activity assessments in the Kuopio Ischaemic Heart Disease Risk Factor Study. Int J Epidemiol 21:467–472
Ovaskainen M-L, Valsta L, Lauronen J (1996) The compilation of food analysis values as a database for dietary studies—the Finnish experience. Food Chem 57:133–136
Luscombe ND, Clifton PM, Noakes M, Farnsworth E, Wittert G (2003) Effect of a high-protein, energy-restricted diet on weight loss and energy expenditure after weight stabilization in hyperinsulinemic subjects. Int J Obes Relat Metab Disord 27:582–590
Johnston CS, Tjonn SL, Swan PD (2004) High-protein, low-fat diets are effective for weight loss and favorably alter biomarkers in healthy adults. J Nutr 134:586–591
Meckling KA, O’Sullivan C, Saari D (2004) Comparison of a low-fat diet to a low-carbohydrate diet on weight loss, body composition, and risk factors for diabetes and cardiovascular disease in free-living, overweight men and women. J Clin Endocrinol Metab 89:2717–2723
Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ (2005) Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA 293:43–53
Borg P, Fogelholm M, Kukkonen-Harjula K (2004) Food selection and eating behaviour during weight maintenance intervention and 2-y follow-up in obese men. Int J Obes Relat Metab Disord 28:1548–1554
Astrup A, Buemann B, Flint A, Raben A (2002) Low-fat diets and energy balance: how does the evidence stand in 2002? Proc Nutr Soc 61:299–309
Foster GD, Wyatt HR, Hill JO et al (2003) A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 348:2082–2090
Samaha FF, Iqbal N, Seshadri P et al (2003) A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med 348:2074–2081
McAuley KA, Hopkins CM, Smith KJ et al (2005) Comparison of high-fat and high-protein diets with a high-carbohydrate diet in insulin-resistant obese women. Diabetologia 48:8–16
Stern L, Iqbal N, Seshadri P et al (2004) The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med 140:778–785
McAuley KA, Smith KJ, Taylor RW, McLay RT, Williams SM, Mann JI (2005) Long-term effects of popular dietary approaches on weight loss and features of insulin resistance. Int J Obes (Lond) 30:342–349
Crowe TC (2005) Safety of low-carbohydrate diets. Obes Rev 6:235–245
Eisenstein J, Roberts SB, Dallal G, Saltzman E (2002) High-protein weight-loss diets: are they safe and do they work? A review of the experimental and epidemiologic data. Nutr Rev 60:189–200
Westerterp-Plantenga MS, Lejeune MP, Nijs I, van Ooijen M, Kovacs EM (2004) High protein intake sustains weight maintenance after body weight loss in humans. Int J Obes Relat Metab Disord 28:57–64
Liu S, Willett WC, Manson JE, Hu FB, Rosner B, Colditz G (2003) Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am J Clin Nutr 78:920–927
Ludwig DS, Pereira MA, Kroenke CH et al (1999) Dietary fiber, weight gain, and cardiovascular disease risk factors in young adults. JAMA 282:1539–1546
Koh-Banerjee P, Chu NF, Spiegelman D et al (2003) Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16,587 US men. Am J Clin Nutr 78:719–727
Marshall JA, Bessesen DH, Hamman RF (1997) High saturated fat and low starch and fibre are associated with hyperinsulinaemia in a non-diabetic population: the San Luis Valley Diabetes Study. Diabetologia 40:430–438
Ylönen K, Saloranta C, Kronberg-Kippilä C, Groop L, Aro A, Virtanen SM (2003) Associations of dietary fiber with glucose metabolism in nondiabetic relatives of subjects with type 2 diabetes: the Botnia Dietary Study. Diabetes Care 26:1979–1985
Lau C, Faerch K, Glumer C et al (2005) Dietary glycemic index, glycemic load, fiber, simple sugars, and insulin resistance: the Inter99 study. Diabetes Care 28:1397–1403
Kahn BB, Flier JS (2000) Obesity and insulin resistance. J Clin Invest 106:473–481
Barrett-Connor E, Khaw KT (1989) Cigarette smoking and increased central adiposity. Ann Intern Med 111:783–787
Rolls BJ, Bell EA (1999) Intake of fat and carbohydrate: role of energy density. Eur J Clin Nutr 53(Suppl 1):S166–S173
Stubbs RJ, Johnstone AM, O’Reilly LM, Barton K, Reid C (1998) The effect of covertly manipulating the energy density of mixed diets on ad libitum food intake in ‘pseudo free-living’ humans. Int J Obes Relat Metab Disord 22:980–987
Devitt AA, Mattes RD (2004) Effects of food unit size and energy density on intake in humans. Appetite 42:213–220
Lindström J, Peltonen M, Tuomilehto J (2005) Lifestyle strategies for weight control—experience from the Finnish Diabetes Prevention Study (DPS). Proc Nutr Soc 64:81–88
Uusitupa M, Lindi V, Louheranta A, Salopuro T, Lindström J, Tuomilehto J (2003) Long-term improvement in insulin sensitivity by changing lifestyles of people with impaired glucose tolerance: 4-year results from the Finnish Diabetes Prevention Study. Diabetes 52:2532–2538
Hu FB, van Dam RM, Liu S (2001) Diet and risk of type II diabetes: the role of types of fat and carbohydrate. Diabetologia 44:805–817
Black AE, Cole TJ (2001) Biased over- or under-reporting is characteristic of individuals whether over time or by different assessment methods. J Am Diet Assoc 101:70–80
Acknowledgements
The members of the DPS Study Group are S. Aunola, Z. Cepaitis, J. Eriksson, M. Hakumäki, K. Hemiö, H. Hämäläinen, P. Härkönen, P. Ilanne-Parikka, A. Ilmanen, S. Keinänen-Kiukaanniemi, K. Kettunen, M. Laakso, T. Lakka, J. Lindström, A. Louheranta, M. Mannelin, P. Nyholm, M. Peltonen, A. Putila, M. Rastas, V. Salminen, J. Sundvall, J. Tuomilehto, M. Uusitupa and T. Valle. The DPS study has been financially supported by Finnish Academy (grants 8473/2298, 40758/5767, 38387/54175, 46558), Ministry of Education, Novo Nordisk Foundation, Yrjö Jahnsson Foundation, Juho Vainio Foundation, Finnish Diabetes Research Foundation, and EVO funds from Tampere and Kuopio University Hospitals. The sponsors of the study had no role in the study design, or the collection, analysis or interpretation of the data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindström, J., Peltonen, M., Eriksson, J.G. et al. High-fibre, low-fat diet predicts long-term weight loss and decreased type 2 diabetes risk: the Finnish Diabetes Prevention Study. Diabetologia 49, 912–920 (2006). https://doi.org/10.1007/s00125-006-0198-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0198-3