Abstract
Background
The clinical effectiveness of intensive lifestyle interventions in preventing or delaying diabetes in people at high risk has been established from randomised trials of structured, intensive interventions conducted in several countries over the past two decades. The challenge is to translate them into routine clinical settings. The objective of this review is to determine whether lifestyle interventions delivered to high-risk adult patients in routine clinical care settings are feasible and effective in achieving reductions in risk factors for diabetes.
Methods
Data sources: MEDLINE (PubMed), EMBASE, CINAHL, The Cochrane Library, Google Scholar, and grey literature were searched for English-language articles published from January 1990 to August 2009. The reference lists of all articles collected were checked to ensure that no relevant suitable studies were missed. Study selection: We included RCTs, before/after evaluations, cohort studies with or without a control group and interrupted time series analyses of lifestyle interventions with the stated aim of diabetes risk reduction or diabetes prevention, conducted in routine clinical settings and delivered by healthcare providers such as family physicians, practice nurses, allied health personnel, or other healthcare staff associated with a health service. Outcomes of interest were weight loss, reduction in waist circumference, improvement of impaired fasting glucose or oral glucose tolerance test (OGTT) results, improvements in fat and fibre intakes, increased level of engagement in physical activity and reduction in diabetes incidence.
Results
Twelve from 41 potentially relevant studies were included in the review. Four studies were suitable for meta-analysis. A significant positive effect of the interventions on weight was reported by all study types. The meta-analysis showed that lifestyle interventions achieved weight and waist circumference reductions after one year. However, no clear effects on biochemical or clinical parameters were observed, possibly due to short follow-up periods or lack of power of the studies meta-analysed. Changes in dietary parameters or physical activity were generally not reported. Most studies assessing feasibility were supportive of implementation of lifestyle interventions in routine clinical care.
Conclusion
Lifestyle interventions for patients at high risk of diabetes, delivered by a variety of healthcare providers in routine clinical settings, are feasible but appear to be of limited clinical benefit one year after intervention. Despite convincing evidence from structured intensive trials, this systematic review showed that translation into routine practice has less effect on diabetes risk reduction.
Similar content being viewed by others
Background
The clinical effectiveness of intensive lifestyle interventions in preventing or delaying development of diabetes in people at high risk has been established from randomised controlled trials of structured, intensive interventions conducted over the past two decades in the USA [1, 2], China [3], Finland [4, 5], and India[6]. These interventions, promoting healthy eating and moderate physical activity, have shown that sustained weight loss of 3.5 kg or more can be achieved with lifestyle interventions, and that onset rates of diabetes can be reduced by as much as 58% in the first few years. A protective effect of the lifestyle intervention of about 43% has also been shown 20 years following the initial intervention in a Chinese study [7]; and a 34% reduction in diabetes incidence was shown to persist 10 years following an intervention in the USA [8]. There is also evidence, from a large cohort study, that even without a formal intervention, diabetes risk was lowered in people whose lifestyle change was consistent with at least three of the goals of the Finnish Diabetes Prevention program [9]. The study's authors estimated that a further 20% reduction in the incidence of diabetes after 4.6 years of follow-up would occur if a further goal were met.
Calls for broader implementation of lifestyle interventions for diabetes prevention in clinical settings are not uncommon in the literature [10–17], although there has been recognition that translation or replication of randomised controlled trials is not straightforward, and long-term sustainability is uncertain [18, 19]. Application of lifestyle recommendations and demonstrated replication of clinical trial approaches in routine clinical practice often are hindered by lack of resources or reimbursement [20], lack of practitioners' time or skill [21, 22], practical difficulties with recruitment, measurement error, and poor patient retention due to the complexities of the transition between awareness, motivation and action [18, 23, 24]. Little systematic information exists on the feasibility or effectiveness of replications of these interventions (or less intensive and more generalisable settings for lifestyle intervention), and on achievement of expected associated benefits as part of routine clinical practice.
To our knowledge, no compilations of trials or reviews of replication studies as part of preventive care in routine clinical practice appear to have been reported. Accordingly, this review presents a summary of outcomes from the routine clinical context and examines the feasibility of transferring the diabetes prevention research to real-world settings. In short, the review assesses the extent that outcomes from clinical trials of lifestyle interventions into physical activity and nutrition to lower diabetes risk have been replicated in routine clinical practice.
Methods
Search strategy
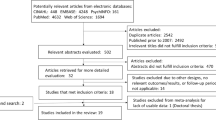
The search was confined to English language articles published between January 1990 and August 2009. Three authors (MC-M, LR, AB) separately interrogated different data sources using the same search terms (see appendix). This was supplemented with hand searches of the reference sections of other systematic reviews [2, 18, 19, 25–40]. Only studies which investigated at least one of our research questions above, and which were consistent with our inclusion criteria below, were considered in this review (Figure 1).
Study selection
The review focused on translational research studies where interventions were based on any of the large reference diabetes prevention RCTs mentioned above. These could be: replication studies in the form of RCTs, before/after evaluations, cohort studies with or without a control group, or interrupted time series analyses, where participants have been exposed to a lifestyle intervention of at least 3 months duration and followed up for at least 3 months. Routine clinical practice was defined as a health service setting providing patient care such as primary health clinics, hospital outpatient clinics or specialist medical centres.
Intervention types
Interventions were classified as single (either nutrition or physical activity programs with or without medication), or combined nutrition and/or physical activity programs (structured or unstructured) whether or not they included medication. Structured intervention components were defined as those in which participants received a standard set of sessions with instructions on specific dietary and/or physical activity requirements and goals. In unstructured interventions participants were given generic advice on healthy living without specific goals other than improving diet or physical activity in relation to baseline. The comparison group might be 'no intervention group' or an 'alternative intervention' (single or combined). Prevention programs delivering diabetes education materials only were excluded. Likewise, medication-only studies were excluded. Only programs conducted in routine health services, delivered on-site or in associated facilities, with outcomes measured in healthcare settings by general medical practitioners, specialist physicians, practice nurses, dietitians, physiotherapists, allied health professionals, community health staff, or research staff attached to the health service, were included in this review. Interventions either had to be replications or modification of all or some components of the US Diabetes Prevention Program [DPP] [1] or Finnish Diabetes Prevention Study [DPS] [5] or any other reference trial, or had to include the reduction of diabetes risk or diabetes incidence explicitly as a goal or objective.
Target group
Participants were adult men or women with any degree of impaired glucose regulation (impaired fasting glucose or impaired glucose tolerance) or with normal glycaemia but at risk of diabetes as determined by risk factors such as obesity or family history. They may have been recruited from the primary or other healthcare patient clientele or from the general population but had to receive the intervention through routine healthcare services. Participants' risk of diabetes may have been determined by a diabetes risk score, either measured or from self-report, and may have had accompanying blood glucose tests to either identify impaired glucose regulation or exclude diabetes before receiving the intervention. Studies including patients with diagnosed diabetes were included in this review only if they were a replication of the reference trials and whose outcomes were reported separately from participants without diabetes.
Outcomes of interest
Studies were included if they reported at least one of the following main outcome measures of interest:
-
Improvement in objectively measured risk factors such as weight loss or waist circumference reduction.
-
Metabolic outcomes indicative of diabetes risk reduction (improvement of fasting glucose levels, improved 2-hour post-prandial plasma glucose, or reduction of HbA1c)
-
Self-reported or objectively measured behavioural outcomes such as increased physical activity (minutes per day or METS per hour), increased fibre consumption (grams per day or gm per KJ), or reduction of fat intake (% of total energy intake).
The secondary outcome examined was:
-
Prevention of diabetes (incidence %, or delay in onset or reduction in incidence over a given follow-up time).
Bias assessment
To assess the potential for bias, and given the heterogeneity of studies included in this review, a generalisability and bias assessment tool covering elements of various checklists and resources from the literature was specifically designed. Items examined included participant recruitment source, selection criteria, treatment allocation, blindness of outcome assessment, simultaneous collection of data for intervention and control groups, measurement error, subgroup analysis and discussion of study limitations (tool available from the authors on request). Reference tools used for this design were STROBE, COCHRANE Collaboration, CLEAR NPT, EQUATOR, PRISMA, TREND and MOOSE [41–46]. One of the authors (MC-M) conducted the bias and quality assessment of all studies and three other authors (LR, SM & PTE) independently conducted the second bias and quality assessment of some of the studies. Two of the authors (MC-M & SM) independently extracted results and assessed the appropriateness of statistical analyses and conclusions.
Assessment of study quality
Study quality was assessed and graded on the following criteria: (1) evidence of assessment of risk for diabetes at enrolment; (2) explicit eligibility and exclusion criteria; (3) reported participation rate of at least 50% of eligible people; (4) follow-up assessment rates of ≥ 65% of program participants by study conclusion or follow-up; (5) evidence of measurable or explicit outcome assessment; (6) appropriate statistical methods, including adequate control for confounders (in non-RCTs); (7) explicit intervention components; (8) conclusions supported by findings. A numeric score giving equal weight to each of the above criteria was used to determine quality. The maximum possible score was thus 8, indicating highest quality.
Statistical analysis
The denominator for the effect sizes was the number of subjects in whom the outcome had been assessed. Study results were categorised as positive (statistically significant difference observed), negative (no difference or statistically significant negative effect), or inconclusive (showed no difference but lacked sufficient power to detect a difference). Given the heterogeneity of designs, length of follow-up and outcome measurements of the available studies, pooling of selected results for a meta-analysis was feasible only for four RCTs reporting 12-month follow-up results [47–50]. The remaining eight studies were critically reviewed but not meta-analysed. Changes in means, and tests of heterogeneity between trials were calculated using random effects models. When not reported in individual studies, standard deviations of mean differences in outcome measures were calculated from supplied study participant numbers and standard errors or from 95% confidence limits, either of before-and-after means or from before-and-after differences in mean values. Meta-analysis was conducted using NCSS software version 7.1.1.9 [51] on the four main outcomes of interest: changes in weight, fasting plasma glucose, waist circumference and 2-hour OGTT.
Sensitivity analysis by study quality was not deemed necessary as all four studies finally selected for meta-analysis had a quality score of 7 or 8 out of the possible 8 maximum score. Our search did not identify unpublished replication studies of diabetes prevention in routine clinical practice. Accordingly, we expected findings not to be significantly affected by publication bias.
Results
Our searches identified 41 potentially eligible diabetes prevention studies of lifestyle interventions in clinical practice that included various combinations of diet and/or exercise for diabetes risk reduction or diabetes prevention. Of these, 18 studies were excluded because: their replications of lifestyle interventions were conducted in non-routine clinical settings (e.g. in community settings such as homes, public centres, churches, or workplaces) [52–59], or in a research setting [47, 60–65]; or they did not include at least one of the outcomes of interest [66, 67]. A further 5 were excluded because they were trials underway and/or had not published results to date [16, 68–70]; or they replicated a reference trial for people who already had diabetes [71]. A further 6 studies were excluded because: the study compared results retrospectively with reference trials without conducting an intervention [9]; the intervention was confined to a diabetes education component only [72, 73]; the intervention was telephone-based only and had not replicated components of the reference trials [74]; or they were either duplicates, companion or interim reports, of studies already selected [75–77].
Differences in presentation of results (e.g. monthly weight change without SD [78], or BMI change instead of weight change [79], or FPG ranges instead of group means [79]) precluded inclusion of two studies in the meta-analysis. One study, with the largest sample size [80], could not be meta-analysed to estimate the effects of a lifestyle intervention, as both the medication and placebo arms received the lifestyle intervention, i.e. the study measured the effects of medication as an adjunct to lifestyle intervention.
The final set of 12 studies covered in this review included 7 randomised controlled trials (including one cluster RCT), 3 before-after designs without a control group and two before-after designs with a control group (Table 1). The studies were conducted in 8 OECD countries, and had sample sizes ranging from 58 to 3,304 (median 311), with participant ages ranging from 20 to 79 years; six of the studies targeted middle-aged people only. All interventions combined physical activity and dietary advice, two studies also included medication as part of the intervention [50, 80], and all were delivered in routine clinical settings, such as specialist services or hospital outpatient clinics (5), general practitioner consulting rooms (5) or community health services (2). Staff delivering the intervention were usually nurses or allied health staff (8/12). The target groups were people at high risk, defined either by the presence of impaired glucose tolerance, severe obesity, or metabolic syndrome or some of its components. Eight of these studies also included normoglycaemic patients and two replication studies included both subjects with and without diabetes and pre-diabetes.
Types of lifestyle interventions reported
All studies included a combined lifestyle intervention but two eligible studies included a medication arm in addition to lifestyle. Seven studies attempted replication of the reference trial approaches from either the U.S DPP [1] or the Finnish DPS [81] with adaptation to routine clinical practice, mostly to cater for limitations in practitioner's time and health service budgets [14, 48, 49, 78, 82–84]. Modifications included: shorter duration of program (2/7); delivery of group sessions instead of individual face-to-face counselling (4/7); reduced number and frequency of individual or group counselling sessions to which participants were exposed (5/7); and mixed group and individual program approaches (1/7).
Modifications of interventions during the maintenance phase included intermittent support sessions, more economical versions of the resources given to participants, and multidisciplinary teams, either available on site or hired as an additional service. For interventions delivered in a group-based modality, the maximum number of sessions per program was 16, as per the reference trial [1] (median of 6 sessions), but over a shorter period of time. Among the 5 studies reporting delivery of individual counselling sessions, the median number of individual counselling sessions was 13.5.
All dietary interventions were structured and half the physical activity interventions were unstructured (Table 2). While some interventions were delivered with a core intensive phase and an intermittent approach for the maintenance phase, the median duration of intervention was 32 weeks; follow-up periods also varied from 4 to 60 months with a median follow-up duration of 12 months. Delivery of the modified versions of the reference trial interventions was mostly by nurses, psychologists or allied health staff such as health promotion counsellors, dietitians or exercise physiologists alone (8/12) who provided the training, demonstration, counselling or education sessions. Physicians were mainly involved in assessing participant eligibility, referral and outcome measurement (7/12). Two studies did not report the professional background of people delivering the intervention or assessing the participants [49, 80].
Type of outcomes reported
Reported measured outcomes of interest were weight (12/12), fasting plasma glucose (9/12) waist circumference (7/12), and 2-hour OGTT (3/12) (Table 3). Six studies had follow-up periods enabling the examination of diabetes incidence or incidence reduction, with the remainder confined to reporting risk improvement via behavioural modification or improvement in metabolic or anthropometric parameters. Self-reported dietary and physical activity outcomes of interest amenable to statistical comparison were not often reported and were confined to mean reduction in fat intake as a percentage of total energy (3/12), and changes in fibre intake (3/12). These are summarised in Table 4. Due to the heterogeneity of units used for measuring and repporting changes in physical activity, it was not possible to meta-analyse these outcomes.
Study quality findings
While three of the 12 studies justified their sample sizes on statistical grounds, and not all adjusted for potential confounders, the quality of study design and reporting overall was good in 10 of the 12 studies included, based on quality criteria scores of 7 or 8 out of 8 (Table 1). Two studies were considered suboptimal, with quality scores of 3 or 5 out of 8 respectively [14, 84].
Limited generalisability was identified in five studies, where participants recruited were either self-referred healthy volunteers [50] or a convenience sample of males only [49, 79], or mostly severely obese middle-age women [14, 78]. Two studies reported higher success rates for participants who had already met the goals at baseline [78, 82]. In two studies [14, 84] the intervention incurred charges and out-of-pocket expenses for each session, which lead to differential exposure to intensity and duration of intervention on the basis of participant's ability to pay. Participation rates for the 8 studies reporting them were satisfactory (median 83.5%). However, in one of the studies, where the participation rate was ostensibly 100%, the control group comprised all those people who did not participate due to financial reasons (on whom outcome measures were collected, but possible exposure to other risk reduction regimes was not recorded) [84].
Loss-to-follow up rates in the 12 studies varied greatly, from 5% to 57% (median 14%). Differential withdrawal rates were reported in a further three studies, where a larger proportion of drop-outs were observed: in participants at highest baseline risk [78]; in those from the intensive arm of the intervention [50]; or in subjects who perceived a poor response to the allocated treatment [80].
Consistency of findings with reference trials
The meta-analysis showed that the pooled weight loss in the intervention group from the four RCTs yielded a weight loss of 1.82 Kg at one year (Figure 2), less than the 5.6 Kg loss observed in the lifestyle-only group of the reference DPP trial or the 4.2 Kg reported in the intervention group of the Finnish DPS. While all studies showed a positive effect on weight loss, only four of the seven studies, 1 RCT and 3 B-A studies [14, 79, 80, 84] reported weight changes at 1 year similar in magnitude to the DPP in the US (around 5 Kg, Table 5). Excepting the XENical in the Prevention of Diabetes in Obese Subjects [XENDOS] trial [80], studies reporting proportions achieving a pre-defined weight loss goal of 5% or 7% were less encouraging. Most studies reported half or less of participants than in the US reference DPP trial, where 50% of participants achieved 7% weight loss at 6 months [1], or in the Finnish DPS where 43% of participants achieved 5% weight loss at 1 year.
The one-year improvements in fasting plasma glucose were similar to the DPP across several studies but were too small to be clinically important; and reductions of diabetes incidence in the two studies reporting them at 12 months follow-up [79, 83] were somewhat less (37% and 23% respectively) than the reductions apparent from the cumulative risk/incidence plots in the Finnish (~70-80%) and DPP (~70%) trials. For the five studies in this review measuring waist circumference, all concluded that waist circumference reductions were possible with modified lifestyle interventions, but after 1 year only two achieved reductions of sufficient magnitude that cannot be attributed to measurement error (≥ 4 cm) [85]. Decreases in fat consumption and increases in fibre consumption resulting from interventions generally were not reported, and the few studies that did showed no substantial improvements. The exception was the Absetz et al. trial which reported half the participants meeting the fibre goal and achieving the total fat intake goal and a third achieving the saturated fat goal [82].
Feasibility of implementation in routine clinical care
Nine of the 12 studies explored whether translation of the reference trials into clinical care was feasible. Eight concluded that modification of the original trial approaches for adaptation to real life practice made the lifestyle interventions feasible, affordable or replicable in clinical care settings despite barriers to implementation [14, 49, 78, 82–84, 86, 87]. The remaining study reported that the transferability of the results from original trials to other settings remains questionable, as the positive effect on outcomes diminishes over time [48].
Meta-analysis results
Seven trials which randomised a total of 4,905 participants to lifestyle intervention or control were identified. The shortest follow-up period was 4 months and the longest follow-up period was six years. Four of these, randomising a total of 1,129 to intervention or control, reported selected outcomes in comparable units at one year [48–50, 87]. These were meta-analysed, although not all outcomes of interest were available from all these studies (Figure 2). We chose not to meta-analyse outcomes at four [80] or six years [79], as these relate to the maintenance phase of a program rather than the medium term impact and it would be inappropriate to compare them with one-year results.
The systematic review of RCT results at 12-month follow-up showed: mean weight reduction was 1.82 Kg greater in treatment than control groups which was statistically significant (95% CI:-2.7 to -0.99 Kg); pooled mean waist measurement reductions in treatment exceeded control groups by 4.6 cm, and this was also significant (95% CI:-5.8 to -3.4 cm); fasting plasma glucose reduction was 0.19 mmol/l greater in treatment than controls but non-significant (95% CI: -0.44 to +0.06 mmol/l); and a non-significant greater increase in 2-hour oral glucose tolerance test result of 0.04 mmol/l (95%CI: -0.49 to +0.42 mmol/l). From the above, it is apparent that the interventions can achieve significant weight and waist measurement reductions at one year but do not significantly change the main metabolic indicators of diabetes risk such as FPG or OGTT.
Four of the 12 studies achieved the greatest weight loss, i.e. 5 Kg or more at 12 months. As only two of these successful studies had optimal quality scores [79, 80], we further examined the characteristics of these studies to identify common determinants of success in diabetes prevention programs. Common features were RCT design, being based in Sweden, and having long interventions (1 and 4 years) and longer follow-up periods (6 years in Malmo, 4 years in XENDOS). They were not replication studies, and the frequency of participant contact was amongst the highest, with Malmo providing 12 group sessions and XENDOS providing up to 54 individual counselling sessions. Another common feature was that following initial substantial weight loss, the final outcome after several years of follow-up was only an average of 3 Kg weight loss in both studies. We may conclude that the outcomes of these two studies involve social, cultural and health system characteristics unique to that part of Europe that may not be generalisable.
Discussion
It is apparent that clinical services are making concerted efforts to translate lifestyle intervention trials into routine practice in several countries, whether as pilot studies or as full-scale interventions. All studies included in this review recruited individuals at high-risk of diabetes from IGT, obesity, metabolic syndrome, a combination of these, or based on other standard inclusion criteria. All interventions combined dietary and physical activity and attempted replication of previously published studies. The wide range of intervention intensities, durations of follow-up and outcome assessments reflected the availability of service time, staff skills, levels of reimbursement for prevention services, and limited funding and resources for translation research within the health systems.
Results from the lifestyle intervention studies that relied on weight change show promise in achieving some degree of risk reduction. The weight reduction in intervention subjects exceeded controls by 1.8 kg, which was less than that found in the reference U.S. DPP (5.6 Kg) or the Finnish DPS (4.2 Kg). Results from studies that relied on changes in fasting plasma glucose or 2-hr plasma glucose as a measure of success, were less convincing. However, similarly small changes in FPG after the intervention were also observed in the reference trials (Table 5). Controlled studies meta-analysed here were not successful in showing improved glucose tolerance to a clinically meaningful level that could lead to diabetes prevention.
The independent effects of physical activity and diet and other lifestyle changes in the treatment of pre-diabetes were not examined in many of the studies included in this review. Adjustment for covariates/confounders generally was not conducted or at least not reported in those observational studies we examined. It is possible to combine, 'meta-analytically', outcome measures from observational studies but these must be adjusted for confounding, preferably the same confounding variables measured similarly across studies. We excluded from the meta-analysis all observational studies and some RCT studies due to the heterogeneity of reported outcome measurements [88].
The results from RCTs of routine clinical practice presented here would be expected to occur in a real-world non-experimental setting. However, generalisability from the observational studies examined here is limited given the selection bias of some of the intervention and control groups. The participant population expected through routine care services is 'real-life', self-selected even if programs are offered to all those eligible free of charge. The behaviour of people at risk involves refusals, absenteeism from critical measurement time points and self-selection of healthier and/or more motivated patients. In order to achieve results similar to the RCT evidence, these practical issues of non-compliance would need particular attention in a real world setting. The Diabetes in Europe - Prevention using Lifestyle, Physical Activity and Nutritional intervention (DE-PLAN) [89] is developing the structures for a prevention management model which can be implemented in routine clinical practice settings. Results from this project should shed further light on specific success factors for research translation.
This review also examined the feasibility of implementation of interventions as an integral part of routine clinical care, as this can inform policy on dissemination of diabetes prevention programs or associated subsidies within healthcare systems. To this end, we examined authors' conclusions on whether the given intervention could sustainably be incorporated into usual care provided, for example, without the need for excessive time beyond usual consultation, additional funding or contracting of external staff.
Finally, while the outcomes of the two US studies, where participation incurred a fee, probably are the most representative of real life in USA, such market-based rationing of diabetes prevention might not be acceptable in other health systems, and certainly would not reach those most in need of such interventions, including low socio-economic groups and people with higher prevalence of risk factors for diabetes.
Strengths of this review
To our knowledge, this is the first attempt to comprehensively compile feasibility and effectiveness of translation of diabetes prevention trials specifically for routine clinical settings.
We used a purpose-built comprehensive quality scoring system based on individual components of relevance from checklists widely used by others in quality assessment of the literature. Our quality criteria allowed for the inclusion of several study types to maximise the chances of identifying and assessing relevant diabetes prevention programs. The search was extensive and individual study authors were contacted to either confirm that their study was conducted under routine clinical care or to exclude any translation study conducted in research settings or under simulated clinical care. Meta-analytic techniques were used when feasible.
Limitations
Despite the good quality of papers covered in this review, the total number of studies finally included was small; some were exploratory (3 pilots) and many of them had short follow-ups and only modest sample sizes which essentially reflect the financial and time restrictions of real-life interventions in routine clinical practice. We included studies with intervention and follow-up durations of at least 3 months. These are not unusual in routine practice, as modifications to duration and intensity of the strict approaches in the reference trials are common in the replication literature. While longer interventions and follow-up times are ideal, in real-world situations longer studies inevitably are affected by sample attrition and attendant generalisability issues. We wanted to include some measurement of short-term impact and avoid attrition bias and selection bias in our assessment of what is being evaluated in routine practice and therefore we allowed for feasibility and pilot studies to be incorporated.
Analyses from before-and-after studies often did not report on adjustment for confounders. More importantly, the reporting of outcomes of interest was often incomplete or in disparate units of measurement precluding inclusion in the meta-analysis. However, the overall good quality of these studies enabled their inclusion in the broader systematic review.
Many weight-loss-only programs and other lifestyle interventions for reduction of cardiovascular disease risk were excluded as they did not specifically mention replication of the diabetes prevention trials. However, we acknowledge that results from these may also be applicable to diabetes risk reduction, and while examples of reviews of these are available in the literature, their focus is beyond the scope of our review.
Conclusions
Despite convincing evidence from structured intensive randomised controlled trials in research settings, this systematic review shows that translation into routine practice has somewhat less of an impact on diabetes risk reduction. Given the heterogeneity and limitations of the studies included in this review, it is also not possible to determine conclusively whether the type of clinical setting, the frequency or intensity of interventions, or the modality of the intervention (face-to-face, telephone, written materials, etc) are critical success factors for translation of diabetes prevention programs in routine clinical care. Nor was it possible to assess the separate contributions of individual lifestyle change components to diabetes risk reduction. Accordingly, we cannot yet make specific recommendations on the most effective features of these targeted lifestyle interventions.
However, based on our findings, the direction of the effects on the four most commonly reported outcomes (weight, FPG, waist circumference and 2-hour OGTT) are encouraging; and the consensus on feasibility of their modification as part of routine care without excessive cost suggest that it is still worth promoting the translation of modified, group-based lifestyle interventions, and conducting more rigorous evaluations in these settings. The establishment of a register of translation projects using consistent, measurable outcomes would add more certainty to the effectiveness of routine practice interventions, and when more studies with larger sample sizes and data on intermediate end-points become available they could be included in a more comprehensive meta-analysis.
Appendix - Description of the search strategy
Electronic sources searched
-
Articles were identified through searches in MEDLINE, PubMED, The Cochrane Library, Google Scholar, CINAHL and EMBASE.
-
Internet searches and searches of the grey literature were conducted to identify non peer-reviewed internal reports from government and health services websites and non-government sources.
Supplementary sources
-
Hand searches of reference lists from related articles found whether or not they were eligible for inclusion in this review
-
Hard copy Australian government publications and unpublished internal reports from key informants for non-indexed publications.
-
Authors of reviewed articles were contacted by MC-M if it was unclear from their papers whether the intervention was conducted in a research or community-based or a routine clinical setting. However, due to resource constraints, no attempt was made to contact the investigators whose papers did not report all measured outcomes.
Search terms
Diabetes, Pre-diabetes, Type 2 diabetes, Impaired glucose tolerance OR glucose intolerance, Lifestyle intervention OR lifestyle program OR strategy, Physical activity OR Exercise OR Resistance Training, Healthy eating OR diet OR dietary modification OR weight loss, Behavioural modification, AND (Primary health care, General practi$., clinical practice, routine clinical care), AND (Prevent$. Ti, ab, Translating OR Translation OR Translat$. Ti, ab., Translation research OR translational study OR Replication study).
References
Diabetes Prevention Program Research Group, Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM: Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002, 346 (6): 393-403. 10.1056/NEJMoa012512.
Norris SL, Zhang X, Avenell A, Gregg E, Schmid CH, Lau J: Long-term non-pharmacological weight loss interventions for adults with prediabetes. Cochrane Database of Systematic Reviews. 2005, The Cochrane Collaboration, CD005270-
Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JX, Cao HB, et al: Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997, 20 (4): 537-544. 10.2337/diacare.20.4.537.
Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, Hämäläinen H, Härkönen P, Keinänen-Kiukaanniemi S, Laakso M, et al: Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006, 368: 1673-1679. 10.1016/S0140-6736(06)69701-8.
Tuomılehto J, Lindstrom J, Eriksson JG, Valle TT, The Finnish Diabetes Prevention Study Group: Prevention of type 2 diabetes mellıtus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001, 344: 1343-1350. 10.1056/NEJM200105033441801.
Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V: The Indian Diabetes Prevention Programme (IDPP) shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006, 49: 289-297. 10.1007/s00125-005-0097-z.
Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, Li H, Li H, Jiang Y, An Y, et al: The long-term eff ect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008, 371: 1783-1789. 10.1016/S0140-6736(08)60766-7.
Diabetes Prevention Program Research Group: 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. The Lancet. 2009, 374 (9702): 1677-1686. 10.1016/S0140-6736(09)61457-4.
Simmons RK, Harding AH, Jakes RW, Welch A, Wareham NJ, Griffin SJ: How much might acievement of diabetes prevention behaviour goals reduce the incidence of diabetes if implemented at the population level?. Diabetologia. 2006, 49: 905-911. 10.1007/s00125-006-0163-1.
American Diabetes Association and National Institute of Diabetes Digestive and Kidney Disease: The Prevention or Delay of Type 2 Diabetes (Position statement). Diabetes Care. 2002, 25 (4): 742-749. 10.2337/diacare.25.4.742.
Narayan KMV, Imperatore G, Benjamin SM, Engelgau MM: Targeting people with pre-diabetes. Lifestyle interventions should also be aimed at people with pre-diabetes [Editorial]. BMJ. 2002, 325: 403-404. 10.1136/bmj.325.7361.403.
Burnet DL, Elliot LD, Quinn MT, Plaut AJ, Schwartz MA, Chin MH: Preventing diabetes in the clinical setting. J Gen Intern Med. 2006, 21 (84): 93-
Harris SB, Petrella RJ, Leadbetter W: Lifestyle interventions for type 2 diabetes. Relevance for clinical practice. Canadian Family Physician · Le Médecin de famille canadien. 2003, 49: 1618-1625.
Pagoto SL, Kantor L, Bodenlos JS, Gitkind M, Ma Y: Translating the Diabetes Prevention Program into a hospital-based weight loss program. Health Psychology. 2008, 27 (1 suppl): S91-S98. 10.1037/0278-6133.27.1.S91.
Davis N, Forbes B, Wylie-Rosett J: Role of obesity and lifestyle interventions in the prevention and management of type 2 diabetes. Minerva Medica. 2009, 100: 221-228.
Ma J, King A, Wilson S, Xiao L, Stafford R: Evaluation of lifestyle interventions to treat elevated cardiometabolic risk in primary care (E-LITE): a randomized controlled trial (Study Protocol). BMC Family Practice. 2009, 10 (1): 71-10.1186/1471-2296-10-71.
Schwellnus MP, Patel DN, Nossel C, Dreyer M, Whitesmans S, Derman EW: Healthy lifestyle interventions in general practice. Part 6: Lifestyle and Metabolic Syndrome. South African Family Practice. 2009, 51 (3): 177-181.
Simpson RW, Shaw JE, Zimmer PZ: The prevention of type 2 diabetes - lifestyle change or pharmacotherapy? A challenge for the 21st century. Diabetes Research and Clinical Practice. 2003, 59: 165-180. 10.1016/S0168-8227(02)00275-9.
Davies MJ, Tringham JR, Troughton J, Khunti KK: Prevention of Type 2 diabetes mellitus. A review of the evidence and its application in a UK setting. Diabetic Medicine. 2004, 21: 403-414. 10.1111/j.1464-5491.2004.01176.x.
Ben-Arye E, Lear A, Hermoni D, Margalit RS: Promoting lifestyle self-awareness among the medical team by the use of an integrated teaching approach: a primary care experience. The Journal of Alternative and Complementary Medicine. 2007, 13 (4): 461-470. 10.1089/acm.2007.6313.
Chakravarthy MV, Joyner MJ, Booth FW: An Obligation for Primary Care Physicians to Prescribe Physical Activity to Sedentary Patients to Reduce the Risk of Chronic Health Conditions. Mayo Clinic Proceedings. 2002, 77 (2): 165-173. 10.4065/77.2.165.
Whitlock EP, Orleans CT, Pender N, Allan J: Evaluating primary care behavioral counseling interventions: An evidence-based approach. American Journal of Preventive Medicine. 2002, 22 (4): 267-284. 10.1016/S0749-3797(02)00415-4.
Roumen C, Blaak EE, Corpeleijn E: Lifestyle intervention for prevention of diabetes: determinants of success for future implementation. Nutrition Reviews. 2009, 67 (3): 132-146. 10.1111/j.1753-4887.2009.00181.x.
Koenigsberg MR, Bartlett D, Kramer JS: Facilitating Treatment Adherence with Lifestyle Changes in Diabetes. Am Fam Physician. 2004, 69: 309-316.
Yamaoka K, Tango T: Efficacy of lifestyle education to prevent type 2 diabetes. A meta-analysis of randomized controlled trials (Health Module). Diabetes Care. 2005, 28 (11): 2780-2786. 10.2337/diacare.28.11.2780.
Yates T, Khunti K, Bull F, Gorelly T, Davies MJ: The role of physical activity in the management of Impaired Glucose Tolerance- A systematic review. Diabetologia. 2007, 50: 1116-1126. 10.1007/s00125-007-0638-8.
Innes KE, Bourguignon C, Gill Taylor A: Risk indices associated with the inslin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. J AM Board Farm Pract. 2005, 18: 491-519. 10.3122/jabfm.18.6.491.
Lauritzena T, Borch-Johnsenb K, Sandbæka A: Is prevention of Type-2 diabetes feasible and efficient in primary care? A systematic PubMed review. Primary Care Diabetes Europe. 2007, 1: 5-11. 10.1016/j.pcd.2006.11.001.
Prisant LM: Preventing Type II Diabetes Mellitus. Journal of Clinical Pharmacology. 2004, 44: 406-413. 10.1177/0091270004263018.
Fleming P, Godwin M: Lifestyle interventions in primary care. Systematic review of randomized controlled trials. Canadian Family Physician · Le Médecin de famille canadien. 2008, 54: 1706-1713.
Hays NP, Galassetti PR, Coker RH: Prevention and treatment of type 2 diabetes: Current role of lifestyle, natural product, and pharmacological interventions. Pharmacology & Therapeutics. 2008, 118: 181-191.
Orozco LJ, Buchleitner AM, Gimenez-Perez G, Roqué i Figuls M, Richter B, Mauricio D: Exercise or exercise and diet for preventing type 2 diabetes mellitus (Review). Cochrane Database of Systematic Reviews. 2008, The Cochrane Collaboration, CD003054-3
Priebe M, van Binsbergen J, de Vos R, Vonk RJ: Whole grain foods for the prevention of type 2 diabetes mellitus (Review). Cochrane Database of Systematic Reviews. 2008, The Cochrane Collaboration, CD006061-1
Hussain A, Claussen B, Ramachandran A, Williams R: Prevention of type 2 diabetes: A review. Diabetes Research and Clinical Practice. 2007, 76: 317-326. 10.1016/j.diabres.2006.09.020.
Nield L, Summerbell CD, Hooper L, Whittaker V, Moore H: Dietary advice for the prevention of type 2 diabetes mellitus in adults. Cochrane Database of Systematic Reviews. 2008, The Cochrane Collaboration, CD005102-3
Schulze MB, Hu FB: Primary prevention of diabetes: what can be done and how much can be prevented?. Annu Rev Public Health. 2005, 26: 445-467. 10.1146/annurev.publhealth.26.021304.144532.
Gillies CL, Abrams KR, Lambert PC, Cooper MJ, Sutton AJ, Hsu RT, Khunti K: Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007, 334: 299-302. 10.1136/bmj.39063.689375.55.
Abuissa H, Bell DH, O'Keefe JH: Strategies to prevent type 2 diabetes. Curr Med Res Opin. 2005, 21 (7): 1107-1114. 10.1185/030079905X50606.
Schwellnus MP, Patel DN, Nossel C, Dreyer M, Whitesman S, Derman EW: Healthy lifestyle interventions in general practice. Part 4: Lifestyle and Diabetes Mellitus. South African Family Practice. 2009, 51 (1): 19-25.
Satterfield DW, Volansky M, Caspersen CJ, Engelgau MM, Bowman BA, Gregg EW, Geiss LS, Hosey GW, May J, Vinicor F: Community-Based Lifestyle Interventions to Prevent Type 2 Diabetes. Diabetes Care. 2003, 26 (9): 2643-2652. 10.2337/diacare.26.9.2643.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB: Meta-analysis of Observational Studies in Epidemiology: A Proposal for Reporting- for the Meta-analysis Of Observational Studies in Epidemiology, Group. JAMA. 2000, 283 (15): 2008-2012. 10.1001/jama.283.15.2008.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, STROBE Initiative: The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Preventive Medicine. 2007, 45 (4): 247-251. 10.1016/j.ypmed.2007.08.012.
Boutron I, Moher D, Tugwell P, Giraudeau B, Poiraudeau S, Nizard R, Ravaud P: A checklist to evaluate a report of a nonpharmacological trial (CLEAR NPT) was developed using consensus. Journal of Clinical Epidemiology. 2005, 58 (12): 1233-1240. 10.1016/j.jclinepi.2005.05.004.
Kelley K, Clark B, Brown V, Sitzia J: Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003, 15 (3): 261-266. 10.1093/intqhc/mzg031.
Des Jarlais DC, Lyles C, Crepaz N, the TREND Group: Improving the Reporting Quality of Nonrandomized Evaluations of Behavioral and Public Health Interventions: The TREND Statement. Am J Public Health. 2004, 94 (3): 361-366. 10.2105/AJPH.94.3.361.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Deveraux PJ, Kleijnen J, Moher D: The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. Public Library of Science Med. 2009, 6: 7-
Oldroyd JC, Unwin NC, White M, Mathers C, ALberti KGMM: Randomised controlled trial evaluating lifestyle interventions in people with with impaired glucose tolerance. Diabetes Research and Clinical Practice. 2006, 72: 117-127. 10.1016/j.diabres.2005.09.018.
Bo S, Ciccone G, Baldi C, Benini L, Dusio F, Forastiere G, Lucia C, Nuti C, Durazzo M, Cassader M, et al: Effectiveness of a lifestyle intervention on metabolic syndrome. A randomized controlled trial. Journal of General Internal Medicine. 2007, 22 (12): 1695-1703. 10.1007/s11606-007-0399-6.
Kosaka K, Nodaa M, Kuzuya T: Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Research and Clinical Practice. 2005, 67: 152-162. 10.1016/j.diabres.2004.06.010.
Dyson PA, Hammersley MS, Morris RJ, Holman RR, Turner RC, Fasting Hyperglycaemia Study Group: The Fasting Hyperglycaemia Study: II. Randomized Controlled Trial of Reinforced Healthy-Living Advice in Subjects With Increased But Not Diabetic Fasting Plasma Glucose. Metabolism. 1997, 46 (Suppl 1): 50-55. 10.1016/S0026-0495(97)90318-8. (December)(12)
NCSS Statistical and power analysis software Trial version 7.1.1.9. NCSS. NCSS, LLC. Kaysville, Utah, [http://www.ncss.com]
Seidel MC, Powell RO, Zgibor JC, Siminerio LM, Piatt GA: Translating the Diabetes Prevention Program Into an Urban Medically Underserved Community: A nonrandomized prospective intervention study. Diabetes Care. 2008, 31 (4): 684-689. 10.2337/dc07-1869.
Swinburn BA, Metcalf PA, Ley SJ: Long-Term (5-Year) Effects of a Reduced-Fat Diet Intervention in Individuals With Glucose Intolerance. Diabetes Care. 2001, 24 (4): 619-624. 10.2337/diacare.24.4.619.
Davis-Smith YM, Boltri JM, Seale JP, Shellenberger STB, Tobin B: Implementing a Diabetes Prevention Program in a Rural African-American Church. JAMA. 2007, 99 (4): 440-446.
Ackermann RT, Marrero DG: Adapting the Diabetes Prevention Program lifestyle intervention for delivery in the community- The YMCA model. The Diabetes Educator. 2007, 33 (1): 73-78. 10.1177/0145721706297743.
Williams K, Prevost AT, Griffin S, Hardeman W, Hollingwort W, Spiegelhalter D, Sutton S, Ekelund U, Wareham N, Kinmonth AL: The ProActive trial protocol - a randomised controlled trial of the efficacy of a family-based, domiciliary intervention programme to increase physical activity among individuals at high risk of diabetes [ISRCTN61323766]. BMC Public Health. 2004, 4: 48-10.1186/1471-2458-4-48.
Simmons D, Fleming C, Voyle J, Fou F, Feo S, Gatland B: A Pilot Urban Church-based Programme to Reduce Risk Factors for Diabetes Among Western Samoans in New Zealand. Diabetic Medicine. 1998, 15: 136-142. 10.1002/(SICI)1096-9136(199802)15:2<136::AID-DIA530>3.0.CO;2-P.
Coppell KJ, Tipene-Leach DC, Pahau HLR, Williams SM, Abel S, Iles M, Hindmarsh JM, Mann JI: Two-year results from a community-wide diabetes prevention intervention in a high-risk indigenous community: The Ngaty and Healthy project. Diabetes Research and Clinical Practice. 2009, 13: 220-227. 10.1016/j.diabres.2009.05.009.
Payne WR, Walsh KJ, Harvey JT, Livy MF, McKenzie KJ, Donaldson A, Atkinson MG, Keogh JB, Moss RS, Dunstan DW, et al: Effect of a low-resource-intensive lifestyle modification program incorporating gymnasium-based and home-based resistance training on type 2 diabetes risk in Australian adults. Diabetes Care. 2008, 31 (2): 2244-2250. 10.2337/dc08-0152.
Liao D, Asberry PJ, Shofer JB, Callahan H, Matthys C, Boyko EJ, Leonetti D, Kahn S, Austin M, Newell L, et al: Improvement of BMI, Body Composition, and Body Fat Distribution With Lifestyle Modification in Japanese Americans With Impaired Glucose Tolerance. Diabetes Care. 2002, 25: 1504-1510. 10.2337/diacare.25.9.1504.
Aldana S, Greenlow R, Diehl HA, Salberg A, Merril RM, Ohmine S, Thomas C: Effects of an intensive diet and physical activity modification program on the health risks of adults. Journal of the American Dietetic Association. 2005, 105: 3-10.1016/j.jada.2004.12.007.
Mensink M, Feskens EJM, Saris WHM, de Bruin TWA, Blaak EE: Study on Lifestyle Intervention and Impaired Glucose Tolerance Maastricht (SLIM): preliminary results after one year. International Journal of Obesity. 2003, 27: 377-384. 10.1038/sj.ijo.0802249.
Page RC, Harnden KE, Cook JT, Turner RC: Can life-styles of subjects with impaired glucose tolerance be changed? A feasibility study. Diabet Med. 1992, 9 (6): 562-566. 10.1111/j.1464-5491.1992.tb01839.x.
Wing RR, Venditti E, Jakicic JM, Polley BA, Lang W: Lifestyle intervention in overweight individual with a family history of diabetes. Diabetes Care. 1998, 21 (3): 350-359. 10.2337/diacare.21.3.350.
Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, Hesson LA, Osei SY, Kaplan R, Stunkard AJ: Randomized Trial of Lifestyle Modification and Pharmacotherapy for Obesity. N Engl J Med. 2005, 353 (20): 2111-2120. 10.1056/NEJMoa050156.
Stevens VJ, Glasgow RE, Toobert DJ, Karanja N, Smith S: One-year results from a brief, computer-assisted intervention to decrease consumption of fat and increase consumption of fruits and vegetables. Preventive Medicine. 2003, 36: 594-600. 10.1016/S0091-7435(03)00019-7.
van Sluijs EMF, van Poppel MNM, Twisk JWR, Chin AP, Marijke J, Calfas KJ, van Mechelen W: Effect of a Tailored Physical Activity Intervention Delivered in General Practice Settings: Results of a Randomized Controlled Trial. Am J Public Health. 2005, 95 (10): 1825-1831. 10.2105/AJPH.2004.044537.
Universitaire de Sherbrooke: Diabetes Prevention in Estrie. Clinical Trials.gov identifier NCT00991549 (unpublished results). 2009, Accessd August 2009, [http://clinicaltrials.gov/ct2/show/NCT00991549?term=diabetes&cond=prevention&intr=lifestyle&lup_s=10%2F07%2F2009&rank=2]
University of Pittsburgh: Evaluation of Group Lifestyle Balance DVD in Primary Care Practice (STEP UP). Clinical Trials database. 2008, [http://clinicaltrials.gov/ct2/show/NCT00480779?term=group+lifestyle+balance+DVD+in+primary+care&rank=1]
Finnish Diabetes Association: Development Programme for the Prevention and Care of Diabetes in Finland DEHKO 2000 - 2010. 2009, Webpage, [http://www.diabetes.fi/en/finnish_diabetes_association/diabetes_programme_dehko]
Delahanty LM, Nathan DM: Implications of the Diabetes Prevention Program and Look AHEAD clinical trials for lifestyle interventions. Journal of the American Dietetic Association. 2008, 108: S66-S72. 10.1016/j.jada.2008.01.026.
Aldana SG, Greenlaw RL, Diehl HA, Salberg A, Merrill RMOS, Thomas C: The behavioral and clinical effects of therapeutic lifestyle change on middle-aged adults. Prev Chronic Dis [serial online]. 2006, 3 (1): 1-16.
Watanabe M, Yamaoka K, Yokotsuka M, Tango T: Randomized Controlled Trial of a New Dietary Education Program to Prevent Type 2 Diabetes in a High-Risk Group of Japanese Male Workers. Diabetes Care. 2003, 26 (12): 3209-3214. 10.2337/diacare.26.12.3209.
Kolt GS, Schofield GM, Kerse N, Garrett N, Oliver M: Effect of telephone counselling on physical activity for low-active older people in primary care: a randomized controlled trial. J Am Geriatr Soc. 2007, 55: 986-992. 10.1111/j.1532-5415.2007.01203.x.
Kilkkinen A, Heistaro S, Laatikainen T, Janus E, Chapman A, Absetz P, Dunbar J: Prevention of type 2 diabetes in a primary health care setting. Interim results from the Greater Green triangle (GGT) Diabetes Prevention Project. Diabetes Research and Clinical Practice. 2007, 76: 460-462. 10.1016/j.diabres.2006.09.027.
Venditti EM, Bray GA, Carrion-Petersen ML, Delahanty LM, Eldestein SL, Hamman RF, Hoskin MA, Knowler WC, Ma Y: First versus repeat treatment with a lifestyle itnervention program: attendance and weight loss outcomes. International Journal of Obesity. 2008, 32: 1537-1544. 10.1038/ijo.2008.134.
Absetz P, Oldenburg B, Hankonen N, Valve R, Heinonen H, Nissinen A, Fogelholm M, Talja M, Uutella A: Type 2 diabetes prevention in the real world. Three-year results of the GOAL lifestyle implementation trial. Diabetes Care. 2009, 32 (8): 1418-1420. 10.2337/dc09-0039.
Whittemore R, Melikus G, Wagner J, Dziura J, Northrup V, Grey M: Translating the Diabetes Prevention Program to primary care- A pilot study. Nursing Research. 2009, 58 (1): 2-12. 10.1097/NNR.0b013e31818fcef3.
Eriksson KF, Lindgiirde E: Prevention of Type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise The 6-year Malmo feasibility study. Diabetologia. 1991, 34: 891-898. 10.1007/BF00400196.
Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L: XENical in the Prevention of Diabetes in Obese Subjects (XENDOS) Study A randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004, 27: 155-161. 10.2337/diacare.27.1.155.
Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, Hämäläinen H, Härkönen P, Keinänen-Kiukaanniemi S, Laakso M, et al: Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. The Lancet. 2006, 368 (9548): 1673-1679. 10.1016/S0140-6736(06)69701-8.
Absetz P, Valve R, Oldenburg B, Heinonen H, Nissinen A, Fogelholm M, Ilvesmaki V, Talja M, Uutella A: Type 2 diabetes prevention in the "real world". One-year results of the GOAL Implementation Trial. Diabetes care. 2007, 30 (10): 2465-2470. 10.2337/dc07-0171.
Laatikainen T, Dunbar JA, Chapman A, Kilkinen A, Vartiainen E, Heistaro S, Philpot B, Absetz P, Bunker S, O'Neil A, et al: Prevention of type 2 diabetes by lifestyle intervention in an Australian primary health care setting: Greater Green Triangle (GGT) Diabetes Prevention Project. BioMed Central Public Health. 2007, 7: 249-
McTigue KM, Conroy MB, Bigi L, Murphy C, McNeill M: Weight loss through living well. Translating an effective lifestyle intervention into clinical practice. The Diabetes Educator. 2009, 35 (2): 199-208. 10.1177/0145721709332815.
Ulijaszek SJ, Kerr DA: Anthropometric measurement error and the assessment of nutritional status. Br J Nutr. 1999, 82 (3): 165-177. 10.1017/S0007114599001348.
Greaves CJ, Middlebrooke A, O'Loughlin L, Holland S, Piper J, Steele A, Gale T, Hammerton F, Daly M: Motivational interviewing for modifying diabetes risk: a randomised controlled trial. British Journal of General Practice. 2008, 58: 535-540. 10.3399/bjgp08X319648.
Barclay C, Procter KL, Glendenning R, Marsh P, Freemen J, Mathers N: Can type 2 diabetes be prevented in UK general practice? A lifestyle-change feasibility study (ISAIAH). Br J Gen Pract. 2008, 58 (553): 541-547. 10.3399/bjgp08X319701.
Lenz M, Steckelberg A, Richter B, Mühlhauser I: Meta-analysis does not allow appraisal of complex interventions in diabetes and hypertension self-management: a methodological review. Diabetologia. 2007, 50 (7): 1375-1383. 10.1007/s00125-007-0679-z.
Schwarz PE, Lindström J, Kissimova-Scarbeck K, Szybinski Z, Barengo NC, Peltonen M, Tuomilehto J, DE-PLAN project: The European perspective of type 2 diabetes prevention: diabetes in Europe--prevention using lifestyle, physical activity and nutritional intervention (DE-PLAN) project. Exp Clin Endocrinol Diabetes. 2008, 116 (3): 167-172. 10.1055/s-2007-992115.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/10/653/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MC-M, conceived the study, designed the quality and bias assessment tools, conducted database searches and quality assessments, wrote the first draft of the manuscript and incorporated changes suggested by others. MC-M coordinated database searches by LR and AB; LR, SM and PTE conducted bias assessments; AB and LR assisted in the design of the study; MC-M and SM performed the statistical analyses. SM, AB and LR helped to comment on and refined the manuscript. All authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cardona-Morrell, M., Rychetnik, L., Morrell, S.L. et al. Reduction of diabetes risk in routine clinical practice: are physical activity and nutrition interventions feasible and are the outcomes from reference trials replicable? A systematic review and meta-analysis. BMC Public Health 10, 653 (2010). https://doi.org/10.1186/1471-2458-10-653
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-10-653