Abstract
Docosahexaenoic acid (DHA) is an omega-3 (ω-3) long-chain polyunsaturated fatty acid (LCPUFA) relevant for brain function. It has largely been explored as a potential candidate to treat Alzheimer’s disease (AD). Clinical evidence favors a role for DHA in the improvement of cognition in very early stages of the AD. In response to stress or damage, DHA generates oxygenated derivatives called docosanoids that can activate the peroxisome proliferator-activated receptor γ (PPARγ). In conjunction with activated retinoid X receptors (RXR), PPARγ modulates inflammation, cell survival, and lipid metabolism. As an early event in AD, inflammation is associated with an excess of amyloid β peptide (Aβ) that contributes to neural insult. Glial cells are recognized to be actively involved during AD, and their dysfunction is associated with the early appearance of this pathology. These cells give support to neurons, remove amyloid β peptides from the brain, and modulate inflammation. Since DHA can modulate glial cell activity, the present work reviews the evidence about this modulation as well as the effect of docosanoids on neuroinflammation and in some AD models. The evidence supports PPARγ as a preferred target for gene modulation. The effective use of DHA and/or its derivatives in a subgroup of people at risk of developing AD is discussed.
Similar content being viewed by others
Background
Docosahexaenoic acid (DHA), an omega-3 (ω-3) long-chain polyunsaturated fatty acid (LCPUFA), is involved in a wide range of cellular processes in mammalian cells. It serves as a structural component and as a precursor for bioactive compounds that modulate cell signaling and gene expression [1]. Humans lack Δ15-desaturase and Δ12-desaturase, and they do not produce αLNA de novo, and it is from this compound that eicosapentaenoic acid (EPA) and ultimately DHA are produced [2, 3]. Consequently, humans need to acquire DHA or its precursors, α-linolenic acid (αLNA) and EPA, from food in order to fulfill bodily requirements [2, 4]. DHA and its precursors are present in oils from macroalgae [3] and cold water fish, from the latter in relatively large quantities [1]. Alternatively, DHA can be synthesized from its precursor αLNA, which is found in oils from seeds and green leafy vegetables [1, 3, 5].
DHA absorption and synthesis from αLNA and EPA
During fetal life and breast feeding, DHA is obtained from the mother. After weaning, DHA derives from animal food, especially fish [1, 5, 6]. In nature, ω-3 fatty acids are mainly esterified as triacylglycerol (TAG) and phospholipids (PLs) [2, 7]. TAG is hydrolyzed in the digestive tract by lingual, pancreatic, and gastric lipases to yield monoacylglycerols and free LCPUFAs [2, 7]. PLs are hydrolyzed in the small intestine by calcium-independent phospholipase A2 (iPLA2) and other lipases [7]. The products of TAG and PL hydrolysis are then absorbed by enterocytes and reassembled into TAG and PLs, which are then integrated into chylomicrons, high-density lipoproteins, and very low-density lipoproteins, finally reaching the liver via the lymphatic system and the blood stream [2, 7].
Alternatively, DHA can be obtained from αLNA or EPA through chain elongation and desaturation processes in the liver, involving Δ6-desaturase (Δ6D), elongase complex activity, Δ5-desaturase, and β-oxidation of tetracosahexaenoic acid to form DHA in the peroxisomes [8, 9]. Although αLNA is considered a poor source for DHA production [4, 10, 11], a diet containing only αLNA can give adequate amounts of DHA in human and rat livers [12, 13]. Nevertheless, higher levels of αLNA and linoleic acid (LA) can potentially inhibit Δ6D and DHA production through β-oxidation [14]. After DHA is synthesized in the liver, it is esterified into PLs, assembled into lipoproteins, and secreted into the blood where it is hydrolyzed again by endothelial lipases and taken up by tissues [7, 15].
DHA entrance into the brain by crossing the blood-brain barrier
The central nervous system (CNS) has the second greatest amount of lipids of the body and ~35 % are polyunsaturated fatty acids (PUFA), being DHA and arachidonic acid (AA), the two major PUFA [16, 17]. DHA is the most predominant fatty acid (FA) found at the sn-2 position in PLs on neuronal and synaptic membranes [18].
Most of the DHA that constitutes the brain before birth and during breast feeding is supplied from the mother [19]. After weaning, DHA is supplied mainly by the liver, where it can be synthesized from its precursors, αLNA, and EPA [19]. DHA is incorporated into the brain from the blood [20]. It has been shown that unesterified DHA can diffuse through the blood-brain barrier (BBB) and readily enter the brain [21]. However, DHA in the blood is bound to serum albumin (SA), either as an unesterified FA or esterified as DHA-lysophosphatidylcholine (DHA-LPC) [22]. After being released from SA, DHA is able to cross the BBB, mainly in the form of DHA-LPC [22]. Although passive diffusion of DHA has been shown, PUFA 18 and 20 carbons long can enter the brain through FA transporter proteins (FATP) and FA binding proteins (FABP), as shown in human brain microvessel endothelial cells [23]. Specially, FATP4, FABP5, and fatty acid translocase/CD36 mediate PUFA transport [23]. In the hippocampus of primates, FABP5 is expressed in neurons while FABP7 is found in astrocytes [24], suggesting a possible mechanism for DHA transport. Also, a previously identified orphan sodium-dependent LPC symporter, Mfsd2a, has been implicated in the transport of DHA-LPC but not free DHA across BBB microvessels [25]. In this sense, it has been shown that DHA-LPC esterified at the sn-2 position is captured by the brain more efficiently than free DHA in rats [26, 27].
In the rat brain, there is evidence that astrocytes are capable of synthesizing DHA continuously [28, 29] and that endothelial cells from microvasculature, astrocytes, and neurons synthesize DHA and cooperate for DHA accretion in the brain [30]. Interestingly, DHA accretion decreases slightly after the administration of a high concentration of DHA in the mouse brain [21] and in cultured astrocytes [29], suggesting that some mechanisms regulate DHA entrance and synthesis when DHA levels increase. However, in these experiments, DHA levels were not affected importantly [21, 29]. Finally, it has been suggested that DHA conservation mechanisms might exist in the brain, as has been shown in retinal pigment epithelium [31], suggesting that DHA entrance and production in the brain are sensed and regulated.
DHA and DHA derivatives are involved in neuroprotection through peroxisome proliferator-activated receptors
DHA in the brain of humans and other vertebrates participates in normal growth, development, and function [32], acting as a neurotrophic factor [33] and modulating synaptic activity [34]. Interestingly, DHA-oxygenated derivatives are known to be produced during strokes in the murine brain [35] and to prevent leukocyte infiltration in ischemic murine models [36], thus modulating inflammation in the brain.
DHA derivatives are produced from the DHA contained in the acyl chains of PLs of cellular membranes. In the cellular membrane, DHA is cut by the action of iPLA2 [37, 38]. Subsequently, lipoxygenases (LOX) [36, 37, 39, 40] and/or cyclooxygenase 2 (COX2, induced by stress stimuli) [35, 41] produce di- and trihydroxylated DHA derivatives, called resolvins or protectins (docosanoids) [36, 37, 39–41]. The first DHA derivatives described were called resolvins, due to their anti-inflammatory activity in murine brain exudates [41]. In particular, the 7S,8R,17S-trihydroxy-docosa-4Z,9E,11E,13Z,15E,19Z-hexaenoic acid called resolvin D1 (RvD1) has been shown to participate in resolution of inflammation [41, 42]. Another studied DHA derivative that acts as a neuro-protector is the 10R,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic acid, called neuroprotectin or protectin D1 (NPD1) [36, 40], shown to halt the inflammatory response by decreasing the number of cytotoxic T cells and their migration, as well as the production of pro-inflammatory mediators [36].
DHA is an endogenous ligand for retinoid X receptors (RXR), which form heterodimers with peroxisome proliferator-activated receptors (PPARs) to produce nuclear transcription factors RXR/PPAR, and these can modulate gene expression in different cell types [38, 43]. Additionally, NPD1, but not DHA, activates the PPAR-γ isoform (PPARγ) in human neuronal and glial cells [37]. DHA-oxygenated synthetic derivatives are also potent activators of PPARγ [44], and PPARs lead in the murine model to the control of differentiation or neurons and astrocytes [45, 46]. Furthermore, PPARs modulate COX2 activity in the murine brain [47], suggesting a feedback loop in DHA signaling because COX2 participates in DHA oxygenation [35, 41]. Thus, DHA and DHA derivatives can exert gene modulation through RXR/PPARγ activation, dimerization, and translocation to the nucleus (Fig. 1).
DHA modulation of gene transcription through the action of RXR/PPARγ transcription factors heterodimers. DHA is cut from PLs in cellular membranes by the action of iPLA2. DHA is oxygenated by the action of LOX, or alternatively by the action of COX2. The products of DHA oxygenation are docosanoids, such as NPD1 and RvD1. DHA is a ligand for RXR and NPD1 for PPARγ. Activation of RXR and PPARγ leads to the formation of RXR/PPARγ, which binds to a PPAR response element, in the promoter region of target genes [38], thus modulating inflammation, lipid metabolism, and cellular differentiation. DHA docosahexaenoic acid, PL phospholipids, iPLA 2 independent phospholipase A2, LOX lipoxygenases, COX2 cyclooxygenase 2, NPD1 neuroprotectin D1, RvD1 resolvin D1, RXR retinoid X receptor, PPARγ peroxisome proliferator-activated receptors gamma, RXR/PPARγ heterodimers of nuclear transcription factors RXR and PPARγ. Activation is indicated by black arrows and modulation by the black gaped arrow
DHA modulates the inflammatory response in AD
Alzheimer’s disease (AD) is a neurodegenerative disease that leads to dementia. It is characterized histologically by amyloid deposits, constituted by aggregates of amyloid β peptide (Aβ) and neurofibrillary tangles, conformed by aggregates of microtubule-associated tau protein and cell loss [48, 49]. Aβ is the cleavage product of amyloid β protein precursor (APP) by the β site cleavage enzyme 1 (BACE1) and the γ-secretase complex. Overproduction or inefficient removal of Aβ is thought to trigger early damage in AD [48, 49]. Aβ can be aggregated into oligomeric soluble species, fibrils, and finally amyloid plaques or deposits, leading to glia activation and the induction of an inflammatory response [50, 51].
Participation of glial cells in AD
Glial cells, astrocytes, and microglia, the main supportive cells of neurons, are encountered near Aβ plaques [52, 53]. Nevertheless, the role of glial cells in the pathology of AD is not clear. Whereas inactivated or dysfunctional glial cells increase the amyloid burden and AD pathology, activation of glial cell leads to the production of cytotoxic molecules like nitric oxide (NO), thus contributing to inflammatory damage [50–53].
Astrocytes
Astrocytes are part of the BBB, providing protection to neurons by secreting neurotrophic factors. They nurture neurons and release neurotransmitters that sustain neuronal synaptic transmission [51–54]. In AD, astrocytes are associated with the amyloid pathology and an inflammatory environment, and when activated, they acquire a greater size and express higher levels of glial acid fibrillary protein (GFAP) [52]. In addition, astrocytes can become dysfunctional by Aβ, especially by toxic oligomeric species that lead to calcium dyshomeostasis and finally disrupt astrocytic support of neuronal synaptic function (reviewed in [55]). Astrocytes are structural components of the BBB, and cerebral-vascular deficiencies increase the influx and buildup of Aβ in the brain. This further contributes to the sustained activation of glia (microglia and astrocytes) and to the secretion of two pro-inflammatory molecules, tumor necrosis factor-α (TNF-α), and interleukin-1β (IL-1β), which in turn disrupts glutamatergic transmission [55]. In addition, astrocytes express proteins that are involved in the clearance of Aβ. The failure of neprilysin, insulin-degrading enzyme, and matrix metalloproteinase 9 (proteolytic enzymes) to degrade Aβ promotes the buildup of Aβ in the brain parenchyma, the activation of glial cells, and even a greater Aβ secretion by astrocytes (reviewed in [56]). Moreover, apolipoprotein E (APOE) is needed for Aβ clearance by astrocytes, and bearing APOE ε4 allele decreases Aβ clearance and increases Aβ deposition [57]. The sustained activation of astrocytes increases the production of cytotoxic mediators, such as NO, complement protein, and reactive oxygen species (ROS) [57]. For example, increased production of the complement factor 3 protein in the presence of Aβ and the activation of the nuclear transcription factor kappa-light-chain-enhancer of activated B cells (NF-κB) has been suggested to impair the synaptic function of neurons and the behavior of mice in a model of AD [58]. However, these results are controversial, and the rational of the experimental methods has been debated [59]. Finally, activated astrocytes lead to the release of chemokines such the C-X-C motif ligand 10 (CXCL10), which in turn attracts microglia to Aβ sites through the C-X-C chemokine receptor 3 (CXCR3) [52, 53] (Fig. 2).
Participation of glial cells in AD. 1 Aβ is secreted by the action of BACE1 and γ-secretase, thus forming aggregates of Aβ (oligomers, insoluble fibrillary aggregates and plaques), 2 microglia (M2- like phenotype) and astrocytes capture and degrade Aβ peptides, 3 Aβ aggregates can activate or harm microglia and astrocytes, promoting the production of pro-inflammatory cytokines and mediators, 4 dysfunction of microglia and astrocytes allows Aβ deposition, increasing cellular damage and inflammation, BACE1 β site cleavage enzyme 1, Aβ amyloid β peptide, M1 pro-inflammatory microglia, M2 anti-inflammatory microglia, green arrows anti-inflammatory and clearing action, red arrows pro-inflammatory actions, black arrows interaction
Microglia
Microglial cells are the immune-competent cells of the CNS and the primary phagocytic cell responding to Aβ. When isolated and exposed to Aβ, microglia from AD brain tissue shows elevated expression of interleukin 1 (IL-1), TNF-α, interleukin 6 (IL-6), and interleukin 12 (IL-12). This strongly suggests that either Aβ or amyloid plaques can initiate the activation of microglia and the subsequent release pro-inflammatory molecules in the AD brain [52, 53]. Depending on their activation state, microglia may contribute to the toxic milieu in AD. Like macrophages, microglia exhibit the pro-inflammatory (M1) phenotype, characterized by the expression of cytotoxic genes TNF-α, IL-1, IL-6, IL-12, and interleukin 18 (IL-18), as well as impaired phagocytic capacity [57]. The anti-inflammatory (M2) phenotype, on the other hand, is characterized by expression of anti-inflammatory molecules interleukin 4 (IL-4), interleukin 10 (IL-10), interleukin 13 (IL-13), and transforming growth factor β (TGF-β), as well as by increased phagocytic capacity without production of the toxic NO [57]. However, these two states of activation are assumed to be the extremes of a variety of activation states, and all can contribute differently to AD progression [57]. In addition, aging can enhance microglia’s sensitivity, exacerbating the inflammatory response [53, 57], thus favoring the M1 phenotype by decreasing the phagocytic ability of microglia. Nevertheless, microglia are activated and migrate to amyloid deposits early in the pathogenesis of a mouse model of AD [60]. In old AD patients, microglia from the hippocampus is the prominent proliferating cell population surrounding amyloid deposits [61]. Also, an increased number of activated microglia are detected in the dentate gyrus of hippocampus in the triple transgenic mouse model of AD (3xTg-AD) before overt plaque deposition [62], suggesting that microglia respond early in the pathology of AD and become more active than astrocytes. It is unclear whether this contributes to the pathology or is a mechanism to contain Aβ damage. Additionally, microglia are more effective than astrocytes for phagocyting fibrillar Aβ, except when the latter are associated to APOE, apolipoprotein J (APOJ), α1-antichymotrypsin, or serum amyloid P-complement C1q protein, which are present in amyloid plaques. Furthermore, the same proteins impair phagocytosis of oligomeric Aβ by astrocytes [63]. Thus, the data suggests that both microglia and astrocytes may have differential roles in inflammation during the pathology of AD and that their dysfunction may contribute to the damage in AD (Fig. 2).
DHA and its derivatives as modulators of glial cell activity
A large amount of evidence, in cellular and animal models under neurotoxic stimuli, has suggested that DHA can prevent inflammation by modulating glial cell activity [64–67]. In vitro, DHA diminishes the activation of microglia, the production of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6, and the production of the chemokines C-C motif ligand 2 (CCL2), C-C motif ligand 3 (CCL3), and CXCL10 [67]. In microglia derived from mice, DHA decreases the release of NO that is induced by lipopolysaccharide (LPS) or interferon γ (IFN-γ) and myelin [68]. DHA reduces production of the pro-inflammatory cytokines and NO induced through toll-like receptors type 3 and 4 (TLR3 and TLR4) [69]. This is explained in part by DHA incorporation in the cellular membrane phospholipids that impairs the presentation of antigens, including LPS by TLR4 and its associated receptor CD14 molecule (CD14), thus preventing NF-κB activation and synthesis of IL-1β and TNF-α [70]. On the other hand, DHA inhibits p38 mitogen-activated protein kinase (p38 MAPK) phosphorylation [67, 71], thus inhibiting the expression of inflammatory molecules, and promotes the activation of PPARγ [71], which modulates lipid and glucose metabolism. In microglia exposed to LPS, DHA inhibits the pro-inflammatory characteristics of microglia, including enlarged lipid bodies (lipid droplets, composed of neutral lipids, mainly phospholipids, sterols, triacylglycerols, sterol esters, and proteins) [72], involved in the production of inflammatory mediators [73] and NO. Hence, this mechanism of DHA lessens dendritic damage associated with inflammation in hippocampal slices of mice [74].
In vitro and in vivo, microglia pro-inflammatory activity is associated with an ameboid-like phenotype and the expression of pro-inflammatory cytokines and chemokines related to the M1 macrophage phenotype. DHA treatment reduces ameboid morphology in Müller’s glia (microglia) in the retina [75] and leads to a phenotype with extended branches and the expression of molecules of the M2 macrophage phenotype, related to termination of inflammation [68]. Nevertheless, it is also possible that DHA inhibits the synthesis of pro-inflammatory mediators without inducing a change in phenotype of microglia, despite prompting the inhibition of p38 MAPK phosphorylation and the activation of PPARγ, related to anti-inflammatory action [71]. Furthermore, DHA anti-inflammatory effects are accompanied by an increase in the phagocytic activity of microglial cells [68]. In a human microglial cell line (CHME3), DHA stimulates Aβ phagocytosis and promotes an anti-inflammatory profile [76]. Apart from its anti-inflammatory action, DHA promotes antioxidant activity in BV-2 microglia, by up-regulation of heme oxygenase-1 (HO-1) and protein kinase B (AKT) activation [77]. In addition, increased total glutathione levels have been found in microglia cells under DHA administration [69], supporting DHA role in antioxidant activity in these cells, which could protect them against the oxidative damage associated with AD.
Supplementation of DHA in rodents and humans demonstrates anti-inflammatory action and tissue protection in microglia. DHA enhanced photoreceptor survival and converted activated microglia into a quiescent phenotype in retinal sections of retinoschisin (Rs1h)-deficient mice [78], resembling that of phagocytic non-inflammatory microglia. After induction of cerebral ischemia, DHA reduces central macrophage/microglia activation, leukocyte infiltration, peripheral leukocyte activation, and expression of TNF-α, IL-1β, IL-6, monocyte chemotactic protein-1 (MCP-1), and the CCL2 receptor (CCR2). Also, post-stroke oxidative stress decreases with DHA supplementation, as demonstrated by low c-Jun N-terminal kinase (JNK) phosphorylation, as well as activation of c-Jun phosphorylation and activating protein-1 (AP-1), and an elevated expression of NF-E2-related factor-2 (Nrf2) and HO-1 [79]. In rats with injured sciatic nerve, DHA treatment significantly reduces neurogenic pain and neuronal damage by reducing allograft inflammatory factor 1 (AIF, also known as induction of brown adipocytes, iba-1), positive satellite cells (macrophages or microglia) and expression of the pro-apoptotic p53 protein in the dorsal root ganglia (DRG) [66]. The review of Hjorth and Freund-Levi deals with DHA and EPA action on microglial cells [80].
DHA modulation of astrocytes also demonstrates fine tuning of neuronal activity through inhibition of pro-inflammatory mediators and an important regulation of astrocytic activity. Astrocytes cultured from the rat brain and pre-incubated with DHA prevent the cytotoxic effects of excessive unconjugated bilirubin (UCB) and increase the activity of superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx), therefore contributing to the antioxidant defense [81]. DHA-treated astrocytes also decrease the production of TNF-α and IL-6 while attenuating the phosphorylation of both p38 and p42/44 MAKP, suggesting modulation of TLR4 [82]. Following in vitro ischemia, DHA prevents calcium dyshomeostasis and endoplasmic reticulum stress (ERS) in astrocytes by acting on inositol 1,4,5-triphosphate receptors, attenuating the phosphorylation of eukaryotic initiation factor 2α (EIF2α) and activating transcription factor-4 (ATF-4) following in vitro ischemia [83]. Importantly, DHA modulates glutamate transmission by regulating glutamate transport in astroglia [84] and thus can potentially alleviate the dysregulation of calcium homeostasis and glutamatergic transporters associated with AD [55]. The importance of DHA levels in glutamate recycling by astrocytes has been explored by Latour and collaborators, showing that low levels of DHA in rats are associated with increased astroglial expression of GFAP and decreased uptake of glutamate by astrocytes [85].
Like DHA, the docosanoid NPD1 promotes a ramified, non-inflammatory microglial phenotype and attenuation of choroidal neo-vascularization when administered topically in the eye of mice [86]. The NPD1 isomer 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic acid (DiHDoHE) has similar effects as DHA on calcium dyshomeostasis and ERS in astrocytes [83].
RvD1 inhibits LPS and IFN-γ-induced TNF-α release in astrocyte cultures by inhibition of the extracellular-regulated mitogen-activated protein kinase (ERK) [87]. In peripheral blood mononuclear cells (PBMC) from AD patients, incubated with Aβ, RvD1 promotes the phagocytosis of Aβ in vitro, inhibits apoptosis through the chemokine receptor G protein-coupled receptor 32 (GPR32), and promotes anti-inflammatory profiles by up-regulation of the interleukin 1 receptor antagonist (IL1RN), the integrin B 2 protein (ITGB2), and NF-κB expression, along with the down-regulation of pro-inflammatory cytokines, such as IL-1 and IL-6 [88]. In summary, DHA and its derivatives down-regulate the expression of pro-inflammatory mediators related to cytotoxic cell damage, while up-regulating the expression of anti-inflammatory mediators. This profile prevents the recruitment of resident or incoming immune cells and promotes phagocytic and antioxidant activity. The effects of DHA and its derivatives are summarized in Table 1.
Activation of PPARγ is involved in the modulation of glia by docosanoids
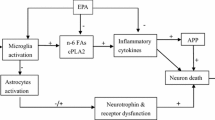
Although there is no clear evidence that DHA is a direct ligand of PPARγ, in silico and in vitro analysis suggests that carboxyl group of DHA can form hydrogen bonds with four of the five amino acids in the ligand-binding pocket of the PPARγ molecule [44]. Furthermore, synthetic-oxygenated derivatives of DHA, such as 5E-4-hydroxydocosahexaenoic acid (4-HDHA) and 5E-4-oxodocosahexaenoic acid (4-oxoDHA), bind and activate PPARγ even more potent than pioglitazone [44]. RvD1 promotes the expression of markers in microglia associated with tissue remodeling and healing activity. In this sense, RvD1 enhances IL-4 as well as the activation of the signal transducer and activator of transcription 6 (STAT6) and the PPARγ transcriptional factors [64]. Additionally, NPD1 activates PPARγ in human neurons and glial cell co-cultures. Despite the important decrease in Aβ secretion caused by NPD1, its inflammatory response has not been evaluated [37]. Moreover, activation of heterodimeric PPARγ/RXRα results in increased phagocytosis of Aβ by microglia [89]. In this sense, PPAR-α isoform agonists diminish the inflammatory response of microglia [65], thus making PPARs or PPARγ potential modulation targets of docosanoids. Nevertheless, it is necessary to establish methods for delivering a particular docosanoid in humans (Fig. 3).
DHA and docosanoids modulate the activation of microglia. DHA and/or docosanoids activate RXR/PPARγ heterodimers that promote transcription of anti-inflammatory cytokines and acquisition of M2 anti-inflammatory profile [74–78]. IL-1 interleukin 1, IL1RN interleukin 1 receptor antagonist, ITGB2 integrin B 2 protein, IL-4 interleukin 4, IL-6 interleukin 6, NF-κB nuclear factor kappa-light-chain-enhancer of activated B cells, Aβ amyloid β peptide, DHA docosahexaenoic acid, NPD1 neuroprotectin D1, RvD1 resolvin D1, RXR/PPARγ heterodimers of nuclear transcription factors RXR and PPARγ, M1 pro-inflammatory microglia, M2 anti-inflammatory microglia, green arrows anti-inflammatory and clearance action
DHA and its derivatives modulate the cellular lipidic environment and amyloid production
DHA modulation of the lipid composition and organization of cellular membranes has been greatly studied. Particularly, it is well known that cholesterol levels are modulated by DHA [90–92]. DHA acyl chains incorporate directly into the lipid raft micro-domains and exclude cholesterol, thus changing protein organization, clustering activity, and signaling [33, 91, 92]. Alternatively, DHA halts cholesterol synthesis and reduces the γ-secretase contents in lipid rafts and activity of BACE1 [93]. Thus, the effects of DHA on the lipidic composition of cellular membranes are of particular interest, because in the brains of AD patients, highly ordered membrane lipid rafts have been found with increased levels of cholesterol, which in turn contain increased levels of BACE1 that suggests increased amyloidogenic processing of APP [94].
In the same sense, DHA administration to transgenic APPswe/PS1dE9 mice, which overproduce Aβ, has proven to lessen Aβ production while decreasing the ratio of omega-6/omega-3 [95]. Additionally, DHA stimulates the production of the soluble amyloid precursor protein α (sAPPα), the alternative non-toxic product of the APP cleavage, and decreases Aβ secretion [96]. The DHA derivative 2-hydroxydocosahexaenoic acid (2OHDHA) shows similar effects on amyloidosis [97], and NPD1 decreases Aβ secretion and protects a primary co-culture of human neurons and glia by increasing sAPPα, which further increases NPD1 production [98]. In addition, NPD1 down-regulates BACE1 expression and activity through the activation of PPARγ [37], a known target of docosanoids [44]. Thus, apart from altering the lipidic profile of cellular membranes, DHA can also modulate the enzymes involved in APP processing and Aβ production.
DHA prevents Aβ toxicity by directly interacting with Aβ monomers or oligomers, thus preventing fibril formation, and lipid peroxidation, as well as increasing the viability of neuronal cells in vitro [99]. Additionally, 2OHDHA acid, a DHA derivative, promotes Aβ monomer insertion into the cellular membrane (rather than the oligomeric or fibrillar Aβ species), thus suggesting the prevention of Aβ oligomerization and derived toxicity [97]. Furthermore, it has been observed that Aβ short species (25–35) form annular structures that solubilize artificial lipid membranes. Increasing DHA levels in the cellular membrane prevents its solubilization and promotes the disruption of Aβ annular structures [100].
DHA treatment in AD: from research to clinical evidence
Since cognitive deficits are the clinical hallmark of AD, any prospective treatment has to be able to ameliorate cognitive deficiencies in animal models and finally in humans. In this regard, DHA has proven to be protective against cognitive deficits in transgenic and non-transgenic murine models of AD by restoring dendritic spine molecular functionality [101, 102], reducing Aβ load, helping against Aβ toxicity [103–106], decreasing tau pathology [107], and increasing cerebral blood volume [108]. Furthermore, administration of 2OHDHA in the 5XFAD transgenic mouse model of AD improved memory and restored cell proliferation in the dentate gyrus without changing the content of Aβ plaques, suggesting that cell proliferation is a major component of memory recovery in mice [109].
In patients with AD (from the OmegaAD study), DHA supplementation increased DHA levels in cerebral spinal fluid and directly correlated with soluble interleukin-1 receptor type II, an inhibitor of IL-1, and the modulation of genes involved in the inflammatory response [110, 111]. This suggests an anti-inflammatory effect of DHA in humans. However, DHA has proven to be ineffective in improving cognition in AD patients with mild to moderate dementia, although some data demonstrate effectiveness in treating patients with mild cognitive impairment (MCI, a prodrome to AD) and participants with memory complaints [112].
What could explain DHA ineffectiveness, despite all the data pointing to DHA benefits? APOE ε4 is a risk factor for developing AD and has been shown to further reduce the effectiveness of DHA treatment. A clinical study conducted in conjunction with the Alzheimer’s Disease Cooperative Study (ADCS) showed that 2 g/day of DHA had no effect on the cognitive state or brain atrophy of AD patients. Nevertheless, AD patients negative for APOE ε4 showed mild though not significant effectiveness of this treatment [113]. In this sense, influence of the APOE ε4 allele on DHA metabolism has been studied in healthy individuals, showing lower levels of DHA in plasma and a lower half-life of DHA in the body [114]. Also, when comparing mice carrying the APOE ε4 allele with those having the APOE ε2 allele, the former show lower brain uptake of DHA [115]. APOE proteins are found on the surface of chylomicron particles after lipid consumption and serve as ligands for low-density lipoprotein receptors, thus regulating the transport of FA. The APOE genotype (ε2, ε3, or ε4) modifies the rate of clearance of ω-3 FA, and APOE ε4 accelerates the clearance of ω-3 FA, increasing β-oxidation of DHA [116] and potentially disrupting lipid metabolism [117]. However, the authors suggest that results on DHA metabolism are inconclusive and that the analysis need to be improved [116, 117]. Interestingly, astrocytes from an AD mice model treated with liver X receptor (LXR) agonists express APOE. Moreover, conditioned medium of primary astrocytes from AD mice increased Aβ phagocytosis that relies on APOE and LXR expression [118]. DHA in combination with the LXR agonist bexarotene increases APOE expression, which in turn increases phagocytosis and reduces inflammatory mediators in astrocytes [119]. Interestingly, bexarotene also induces APOE ε4 lipidation, which increases the generation of APOE ε4–Aβ complexes and reduces Aβ pathology as well as synaptic damage in a mouse model expressing human APOE [120], suggesting a potential role of bexarotene for treating AD pathology and defective APOE ε4; however, bexarotene safety must be guaranteed [120].
There is evidence of DHA deficiency in the plasma from patients diagnosed with AD [121–124]. However, there is controversy concerning DHA levels between AD patients and cognitive normal subjects [125]. Epidemiological studies associate scarce DHA consumption with an increased risk of AD [113]. In a similar sense, mouse models evidence reduced DHA during the aggravation AD pathology [126]. DHA is the major ω-3 PUFA in synaptic membranes. A decreased level of DHA in hippocampus synapses is characterized by altered synaptic transmission and glutamate release by neurons [127], deficient uptake of glutamate by astrocytes, and altered extracellular levels of glutamate [85]. However, restoration of DHA levels by ω-3 supplementation improves altered synaptic transmission and glutamate release [127].
In light of these findings in humans, DHA metabolism in AD patients with APOE ε4 may be especially disrupted, and the effectiveness of DHA treatment might be compromised. This suggests a possible subgroup for DHA administration: those at risk for developing AD with no overt cognitive deterioration and without bearing the APOE ε4 allele.
In this respect, effectiveness of fish oil or DHA-enriched fish oil has been proved in recent studies. DHA-enriched fish oil supplementation in MCI has been observed in a double-blind Malayan study. Subjects over 60 years old received DHA-enriched fish oil during a year, a treatment that improved memory and attention [128]. Other supplements containing ω-3, including DHA, have also shown stabilization of the cognitive state in MCI, but as found in previous studies, neither improvement nor stabilization was observed in AD patients [129]. Finally, a recent published retrospective study evaluated the effect of fish oil consumption on cognition and brain volume in normal individuals as well as MCI and AD patients. By using a generalized estimating equation (GEE) model to analyze incomplete longitudinal data on the Alzheimer’s Disease Neuroimaging Initiative (ADNI) from inception to August 2010, it was found that in all cases, fish oil consumption was associated with increased brain volume and a better cognitive performance, except in APOEε4 carriers as observed in former studies [130].
However, the efficacy of DHA alone has to be reevaluated as it may be more effective in combination with other nutrients including vitamin B [131], or compounds such as bexarotene [119]. Alternative treatments may include the activation of PPARs with agonists or DHA derivatives [132]. Overall, a reevaluation of ω-3 and especially DHA may provide valuable information about DHA effectiveness on MCI.
Conclusions
DHA is a natural compound that can easily be obtained from animal sources, especially cold-water fish. DHA can easily cross the BBB, especially in the form of the DHA-LPC, and therefore, it is suitable as a therapeutic agent for neurological disorders. DHA, free or bound in to PLs, is incorporated into cellular membranes, where it is released and transformed into docosanoids (oxygenated derivatives) to exert its function within the cells via RXR and PPARγ. Although DHA has been associated with protection, based on the modification of cellular membrane fluidity, increasing data suggest that DHA’s action can be attributable to a signaling cascade in which docosanoids exert their action by regulating gene expression of anti-inflammatory and other protective pathways. The neurodegenerative disease of Alzheimer has a complex etiology in which the deposition of Aβ plays an important role. Inflammation is an early event in AD that contributes to increased neuronal damage, especially due to the dysfunction of glial cells. This dysfunction leads to the lack of clearance of Aβ, which further increases the over-activation of glial cells. Overall, a harmful environment is created, withdrawing support to neurons and favoring plaque formation.
In animal models and in vitro, DHA and its derivatives have proven to regulate gene expression of inflammatory mediators, as well as enzymes involved in lipid metabolism and Aβ processing. Activation of PPARγ has been shown to mediate some of the effects promoted by DHA and its derivatives in neurons and glial cells. Therefore, based on the current evidence, DHA or its derivatives can help to prevent or retard inflammatory aspects of the pathology of AD. This aspect of the disease has been considered to be an important player in the determination of the outcome of AD. On the other hand, patients carrying the APOE ε4 allele show disrupted metabolism of DHA. Further evaluation of this trait is needed. New longitudinal studies considering early symptoms of cognitive deterioration associated to AD, including MCI, DHA metabolism in APOE ε4 participants, and inflammatory status, might help to conclude whether people at risk of developing AD can potentially be treated with DHA.
Abbreviations
- 2OHDHA:
-
2-hydroxydocosahexaenoic acid
- 3xTg-AD:
-
triple transgenic mouse model of AD
- 4-HDHA:
-
5E-4-hydroxydocosahexaenoic acid
- 4-oxoDHA:
-
5E-4-oxodocosahexaenoic acid
- AA:
-
arachidonic acid
- AD:
-
Alzheimer’s disease
- ADCS:
-
Alzheimer’s Disease Cooperative Study
- ADNI:
-
Alzheimer’s Disease Neuroimaging Initiative
- AIF:
-
allograft inflammatory factor 1, also known as induction of brown adipocytes, iba-1
- AP-1:
-
activating protein-1
- APOE:
-
apolipoprotein E
- APOJ:
-
apolipoprotein J
- APP:
-
amyloid β precursor protein
- ATF-4:
-
activating transcription factor-4
- Aβ:
-
amyloid β peptide
- BACE1:
-
β site cleavage enzyme 1
- BBB:
-
blood-brain barrier
- CAT:
-
catalase
- CCL2:
-
C-C motif ligand 2
- CCL3:
-
C-C motif ligand 3
- CCR2:
-
CCL2 receptor
- CD11b:
-
integrin subunit alpha M (ITGAM)
- CD14:
-
CD14 molecule
- CD45:
-
protein tyrosine phosphatase, receptor type C
- CLN6NCLFmouse:
-
a mouse with natural occurring neuronal ceroid lipofuscinoses (NCLF) and alterations in the ceroid-lipofuscinosis, neuronal 6 (CLN6) gene
- CNS:
-
central nervous system
- COX2:
-
cyclooxygenase 2
- CXCL10:
-
C-X-C motif ligand 10
- CXCR3:
-
C-X-C chemokine receptor 3
- DHA:
-
docosahexaenoic acid
- DiHDoHE:
-
10S,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic acid
- DRG:
-
dorsal root ganglia
- EIF2α:
-
eukaryotic initiation factor 2α
- EPA:
-
eicosapentaenoic acid
- ERK:
-
extracellular-regulated mitogen-activated protein kinase
- ERS:
-
endoplasmic reticulum stress
- FA:
-
fatty acid(s)
- FABP:
-
FA binding protein(s)
- FATP:
-
FA transporter protein(s)
- GFAP:
-
glial acid fibrillary protein
- GPR32:
-
G protein-coupled receptor 32
- GPx:
-
glutathione peroxidase
- HO-1:
-
heme oxygenase-1
- IFN-γ:
-
interferon γ
- IL-1:
-
interleukin 1
- IL-10:
-
interleukin 10
- IL-12:
-
interleukin 12
- IL-13:
-
interleukin 13
- IL-18:
-
interleukin 18
- IL1RN:
-
interleukin 1 receptor antagonist
- IL-1β:
-
interleukin 1β
- IL-4:
-
interleukin 4
- IL-6:
-
interleukin 6
- iPLA2 :
-
independent phospholipase A2
- ITGB2:
-
integrin B 2 protein
- JNK:
-
c-Jun N-terminal kinase
- AKT:
-
protein kinase B
- LA:
-
linoleic acid
- LCPUFA:
-
long-chain polyunsaturated fatty acid
- LOX:
-
lipoxygenases
- LPC:
-
lysophosphatidylcholine
- LPS:
-
lipopolysaccharide
- LXR:
-
liver X receptor
- M1:
-
pro-inflammatory microglia
- M2:
-
anti-inflammatory microglia
- MAPK:
-
mitogen activated protein kinase
- MCI:
-
mild cognitive impairment
- MCP-1:
-
monocyte chemotactic protein-1
- NF-κB:
-
nuclear factor kappa-light-chain-enhancer of activated B cells
- NO:
-
nitric oxide
- NPD1:
-
neuroprotectin D1 or protectin D1
- Nrf2:
-
NF-E2-related factor-2
- p38 MAPK:
-
p38 mitogen-activated protein kinase
- PBMC:
-
peripheral blood mononuclear cells
- PLs:
-
phospholipids
- PPARs:
-
peroxisome-proliferator activated receptors
- PPARγ:
-
PPAR-γ isoform
- PUFA:
-
polyunsaturated fatty acid(s)
- ROS:
-
reactive oxygen species
- RvD1:
-
resolvin D1
- RXR:
-
retinoid X receptors
- SA:
-
serum albumin
- sAPPα:
-
soluble amyloid precursor protein α
- SOD:
-
superoxide dismutase
- STAT6:
-
signal transducer and active tor of transcription 6
- TAG:
-
triacylglycerol
- TGF-β:
-
transforming growth factor β
- TLR3:
-
toll-like receptor type 3
- TLR4:
-
toll-like receptor type 4
- TNF-α:
-
tumor necrosis factor-α
- UCB:
-
unconjugated bilirubin
- αLNA:
-
α-linolenic acid
- Δ6D:
-
Δ6-desaturase
- ω-3:
-
omega-3
References
Calder PC. Mechanisms of action of (n-3) fatty acids. J Nutr. 2012;142:592S–9.
SanGiovanni JP, Chew EY. The role of omega-3 long-chain polyunsaturated fatty acids in health and disease of the retina. Prog Retin Eye Res. 2005;24:87–138.
Pereira H, Barreira L, Figueiredo F, Custódio L, Vizetto-Duarte C, Polo C, et al. Polyunsaturated fatty acids of marine macroalgae: potential for nutritional and pharmaceutical applications. Mar Drugs. 2012;10:1920–35.
Williams CM, Burdge G. Long-chain n-3 PUFA: plant v. marine sources. Proc Nutr Soc. 2006;65:42–50.
Morse NL. Benefits of docosahexaenoic acid, folic acid, vitamin D and iodine on foetal and infant brain development and function following maternal supplementation during pregnancy and lactation. Nutrients. 2012;4:799–840.
Carlson SE. Docosahexaenoic acid and arachidonic acid in infant development. Semin Neonatol. 2001;6:437–49.
Burri L, Hoem N, Banni S, Berge K. Marine omega-3 phospholipids: metabolism and biological activities. Int J Mol Sci. 2012;13:15401–19.
Kihara A. Very long-chain fatty acids: elongation, physiology and related disorders. J Biochem. 2012;152:387–95.
Sprecher H, Luthria DL, Mohammed BS, Baykousheva SP. Reevaluation of the pathways for the biosynthesis of polyunsaturated fatty acids. J Lipid Res. 1995;36:2471–7.
Huffman SL, Harika RK, Eilander A, Osendarp SJ. Essential fats: how do they affect growth and development of infants and young children in developing countries? A literature review. Matern Child Nutr. 2011;Suppl 3:44–65.
Arterburn LM, Hall EB, Oken H. Distribution, interconversion, and dose response of n-3 fatty acids in humans. Am J Clin Nutr. 2006;83:1467S–76.
Rapoport SI, Rao JS, Igarashi M. Brain metabolism of nutritionally essential polyunsaturated fatty acids depends on both the diet and the liver. Prostaglandins Leukot Essent Fatty Acids. 2007;77:251–61.
Rapoport SI, Igarashi M. Can the rat liver maintain normal brain DHA metabolism in the absence of dietary DHA? Prostaglandins Leukot Essent Fatty Acids. 2009;81:119–23.
Gibson RA, Neumann MA, Lien EL, Boyd KA, Tu WC. Docosahexaenoic acid synthesis from alpha-linolenic acid is inhibited by diets high in polyunsaturated fatty acids. Prostaglandins Leukot Essent Fatty Acids. 2013;88:139–46.
Bazan NG. Neuroprotectin D1-mediated anti-inflammatory and survival signaling in stroke, retinal degenerations, and Alzheimer’s disease. J Lipid Res. 2009;50 Suppl:S400–5.
Lauritzen L, Hansen HS, Jørgensen MH, Michaelsen KF. The essentiality of long chain n-3 fatty acids in relation to development and function of the brain and retina. Prog Lipid Res. 2001;40:1–94.
Rapoport SI, Ramadan E, Basselin M. Docosahexaenoic acid (DHA) incorporation into the brain from plasma as an in vivo biomarker of brain DHA metabolism and neurotransmission. Prostaglandins Other Lipid Mediat. 2011;96:109–13.
Glomset JA. Role of docosahexaenoic acid in neuronal plasma membranes. Sci STKE. 2006;2006:pe6.
Guesnet P, Alessandri JM. Docosahexaenoic acid (DHA) and the developing central nervous system (CNS)—implications for dietary recommendations. Biochimie. 2011;93:7–12.
Guest J, Garg M, Bilgin A, Grant R. Relationship between central and peripheral fatty acids in humans. Lipids Health Dis. 2013;2:79.
Ouellet M, Emond V, Chen CT, Julien C, Bourasset F, Oddo S, et al. Diffusion of docosahexaenoic and eicosapentaenoic acids through the blood-brain barrier: an in situ cerebral perfusion study. Neurochem Int. 2009;55:476–82.
Brossard N, Croset M, Normand S, Pousin J, Lecerf J, Laville M, et al. Human plasma albumin transports [13C] docosahexaenoic acid in two lipid forms to blood cells. J Lipid Res. 1997;38:1571–82.
Mitchell RW, On NH, Del Bigio MR, Miller DW, Hatch GM. Fatty acid transport protein expression in human brain and potential role in fatty acid transport across human brain microvessel endothelial cells. J Neurochem. 2011;117:735–46.
Ma D, Zhang M, Mori Y, Yao C, Larsen CP, Yamashima T, et al. Cellular localization of epidermal-type and brain-type fatty acid-binding proteins in adult hippocampus and their response to cerebral ischemia. Hippocampus. 2010;20:811–9.
Nguyen LN, Ma D, Shui G, Wong P, Cazenave-Gassiot A, Zhang X, et al. Mfsd2a is a transporter for the essential omega-3 fatty acid docosahexaenoic acid. Nature. 2014;509:503–6.
Thies F, Pillon C, Moliere P, Lagarde M, Lecerf J. Preferential incorporation of sn-2 lysoPC DHA over unesterified DHA in the young rat brain. Am J Physiol. 1994;267:R1273–9.
Chen S, Subbaiah PV. Regioisomers of phosphatidylcholine containing DHA and their potential to deliver DHA to the brain: role of phospholipase specificities. Lipids. 2013;48:675–86.
Moore SA, Yoder E, Murphy S, Dutton GR, Spector AA. Astrocytes, not neurons, produce docosahexaenoic acid (22:6 omega-3) and arachidonic acid (20:4 omega-6). J Neurochem. 1991;56:518–24.
Williard DE, Harmon SD, Kaduce TL, Preuss M, Moore SA, Robbins ME, et al. Docosahexaenoic acid synthesis from n-3 polyunsaturated fatty acids in differentiated rat brain astrocytes. J Lipid Res. 2001;42:1368–76.
Moore SA. Polyunsaturated fatty acid synthesis and release by brain-derived cells in vitro. J Mol Neurosci. 2001;16(2-3):195–200.
Bazan NG. Cellular and molecular events mediated by docosahexaenoic acid-derived neuroprotectin D1 signaling in photoreceptor cell survival and brain protection. Prostaglandins Leukot Essent Fatty Acids. 2009;81:205–11.
Tu WC, Cook-Johnson RJ, James MJ, Mühlhäusler BS, Stone DA, Gibson RA. Barramundi (Lates calcarifer) desaturase with Δ6/Δ8 dual activities. Biotechnol Lett. 2012;34:1283–96.
Kim HY, Akbar M, Kim YS. Phosphatidylserine-dependent neuroprotective signaling promoted by docosahexaenoic acid. Prostaglandins Leukot Essent Fatty Acids. 2010;82:165–72.
Cao D, Kevala K, Kim J, Moon HS, Jun SB, Lovinger D, et al. Docosahexaenoic acid promotes hippocampal neuronal development and synaptic function. J Neurochem. 2009;111:510–21.
Hong S, Lu Y, Yang R, Gotlinger KH, Petasis NA, Serhan CN. Resolvin D1, protectin D1, and related docosahexaenoic acid-derived products: analysis via electrospray/low energy tandem mass spectrometry based on spectra and fragmentation mechanisms. J Am Soc Mass Spectrom. 2007;18:128–44.
Ariel A, Li PL, Wang W, Tang WX, Fredman G, Hong S, et al. The docosatriene protectin D1 is produced by TH2 skewing and promotes human T cell apoptosis via lipid raft clustering. J Biol Chem. 2005;280:43079–86.
Zhao Y, Calon F, Julien C, Winkler JW, Petasis NA, Lukiw WJ, et al. Docosahexaenoic acid-derived neuroprotectin D1 induces neuronal survival via secretase- and PPARγ-mediated mechanisms in Alzheimer’s disease models. PLoS One. 2011;6:e15816.
Bordoni A, Di Nunzio M, Danesi F, Biagi PL. Polyunsaturated fatty acids: from diet to binding to PPARs and other nuclear receptors. Genes Nutr. 2006;1:95–106.
Picq M, Chen P, Perez M, Michaud M, Véricel E, Guichardant M, et al. DHA metabolism: targeting the brain and lipoxygenation. Mol Neurobiol. 2010;42:48–51.
Chen P, Véricel E, Lagarde M, Guichardant M. Poxytrins, a class of oxygenated products from polyunsaturated fatty acids, potently inhibit blood platelet aggregation. FASEB J. 2011;25:382–8.
Serhan CN, Hong S, Gronert K, Colgan SP, Devchand PR, Mirick G, et al. Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter proinflammation signals. J Exp Med. 2002;196:1025–37.
Dalli J, Colas RA, Serhan CN. Novel n-3 immunoresolvents: structures and actions. Sci Rep. 2013;3:1940.
Dyall SC, Michael GJ, Michael-Titus AT. Omega-3 fatty acids reverse age-related decreases in nuclear receptors and increase neurogenesis in old rats. J Neurosci Res. 2010;88:2091–102.
Itoh T, Yamamoto K. Peroxisome proliferator activated receptor gamma and oxidized docosahexaenoic acids as new class of ligand. Naunyn Schmiedebergs Arch Pharmacol. 2008;377:541–7.
Cimini A, Benedetti E, Cristiano L, Sebastiani P, D'Amico MA, D'Angelo B, et al. Expression of peroxisome proliferator-activated receptors (PPARs) and retinoic acid receptors (RXRs) in rat cortical neurons. Neuroscience. 2005;130:325–37.
Cristiano L, Cimini A, Moreno S, Ragnelli AM, Paola CM. Peroxisome proliferator-activated receptors (PPARs) and related transcription factors in differentiating astrocyte cultures. Neuroscience. 2005;131:577–87.
Aleshin S, Grabeklis S, Hanck T, Sergeeva M, Reiser G. Peroxisome proliferator-activated receptor (PPAR)-gamma positively controls and PPARalpha negatively controls cyclooxygenase-2 expression in rat brain astrocytes through a convergence on PPARbeta/delta via mutual control of PPAR expression levels. Mol Pharmacol. 2009;76:414–24.
Holtzman DM, Morris JC, Goate AM. Alzheimer’s disease: the challenge of the second century. Sci Transl Med. 2011;3:77sr1.
Blennow K, de Leon MJ, Zetterberg H. Alzheimer’s disease. Lancet. 2006;368:387–403.
Heppner FL, Ransohoff RM, Becher B. Immune attack: the role of inflammation in Alzheimer disease. Nat Rev Neurosci. 2015;16:358–72.
Lucin KM, Wyss-Coray T. Immune activation in brain aging and neurodegeneration: too much or too little? Neuron. 2009;64:110–22.
Farfara D, Lifshitz V, Frenkel D. Neuroprotective and neurotoxic properties of glial cells in the pathogenesis of Alzheimer’s disease. J Cell Mol Med. 2008;12:762–80.
Weitz TM, Town T. Microglia in Alzheimer’s disease: it’s all about context. Int J Alzheimers Dis. 2012;2012:314185.
Lee KM, MacLean AG. New advances on glial activation in health and disease. World J Virol. 2015;4:42–55.
Rossi D. Astrocyte physiopathology: at the crossroads of intercellular networking, inflammation and cell death. Prog Neurobiol. 2015;130:86–120.
Avila-Muñoz E, Arias C. When astrocytes become harmful: functional and inflammatory responses that contribute to Alzheimer’s disease. Ageing Res Rev. 2014;18:29–40.
Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, Feinstein DL, et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015;14:388–405.
Lian H, Yang L, Cole A, Sun L, Chiang AC, Fowler SW, et al. NFκB-activated astroglial release of complement C3 compromises neuronal morphology and function associated with Alzheimer’s disease. Neuron. 2015;85:101–15.
Woodruff TM, Tenner AJ. A commentary on: NFκB-activated astroglial release of complement C3 compromises neuronal morphology and function associated with Alzheimer’s disease. A cautionary note regarding C3aR. Front Immunol. 2015;6:220.
Meyer-Luehmann M, Spires-Jones TL, Prada C, Garcia-Alloza M, de Calignon A, Rozkalne A, et al. Rapid appearance and local toxicity of amyloid-beta plaques in a mouse model of Alzheimer’s disease. Nature. 2008;451:720–4.
Marlatt MW, Bauer J, Aronica E, van Haastert ES, Hoozemans JJ, Joels M, et al. Proliferation in the Alzheimer hippocampus is due to microglia, not astroglia, and occurs at sites of amyloid deposition. Neural Plast. 2014;2014:693851.
Rodríguez JJ, Noristanic HN, Hilditchd T, Olabarriad M, Yehd CY, Wittone J, et al. Increased densities of resting and activated microglia in the dentate gyrus follow senile plaque formation in the CA1 subfield of the hippocampus in the triple transgenic model of Alzheimer’s disease. Neurosci Lett. 2013;552:129–34.
Mulder SD, Nielsen HM, Blankenstein MA, Eikelenboom P, Veerhuis R. Apolipoproteins E and J interfere with amyloid-beta uptake by primary human astrocytes and microglia in vitro. Glia. 2014;62:493–503.
Li L, Wu Y, Wang Y, Wu J, Song L, Xian W, et al. Resolvin D1 promotes the interleukin-4-induced alternative activation in BV-2 microglial cells. J Neuroinflammation. 2014;11:72.
Xu J, Storer PD, Chavis JA, Racke MK, Drew PD. Agonists for the peroxisome proliferator-activated receptor-alpha and the retinoid X receptor inhibit inflammatory responses of microglia. J Neurosci Res. 2005;81:403–11.
Manzhulo IV, Ogurtsova OS, Lamash NE, Latyshev NA, Kasyanov SP, Dyuizen IV. Analgetic effect of docosahexaenoic acid is mediated by modulating the microglia activity in the dorsal root ganglia in a rat model of neuropathic pain. Acta Histochem. 2015;117:659–66.
Lu Y, Zhao LX, Cao DL, Gao YJ. Spinal injection of docosahexaenoic acid attenuates carrageenan-induced inflammatory pain through inhibition of microglia-mediated neuroinflammation in the spinal cord. Neuroscience. 2013;241:22–31.
Chen S, Zhang H, Pu H, Wang G, Li W, Leak RK, et al. n-3 PUFA supplementation benefits microglial responses to myelin pathology. Sci Rep. 2014;4:7458.
Pettit LK, Varsanyi C, Tadros J, Vassiliou E. Modulating the inflammatory properties of activated microglia with docosahexaenoic acid and aspirin. Lipids Health Dis. 2013;12:16.
De Smedt-Peyrusse V, Sargueil F, Moranis A, Harizi H, Mongrand S, Layé S. Docosahexaenoic acid prevents lipopolysaccharide-induced cytokine production in microglial cells by inhibiting lipopolysaccharide receptor presentation but not its membrane subdomain localization. J Neurochem. 2008;105:296–307.
Antonietta Ajmone-Cat M, Lavinia Salvatori M, De Simone R, Mancini M, Biagioni S, Bernardo A, et al. Docosahexaenoic acid modulates inflammatory and antineurogenic functions of activated microglial cells. J Neurosci Res. 2012;90:575–87.
Farese RV, Walther TC. Lipid droplets finally get a little R-E-S-P-E-C-T. Cell. 2009;139:855–60.
Saka HA, Valdivia R. Emerging roles for lipid droplets in immunity and host-pathogen interactions. Annu Rev Cell Dev Biol. 2012;28:411–37.
Chang PK, Khatchadourian A, McKinney RA, Maysinger D. Docosahexaenoic acid (DHA): a modulator of microglia activity and dendritic spine morphology. J Neuroinflammation. 2015;12:34.
Mirza M, Volz C, Karlstetter M, Langiu M, Somogyi A, Ruonala MO, et al. Progressive retinal degeneration and glial activation in the CLN6 (nclf) mouse model of neuronal ceroid lipofuscinosis: a beneficial effect of DHA and curcumin supplementation. PLoS One. 2013;8:e75963.
Hjorth E, Zhu M, Toro VC, Vedin I, Palmblad J, Cederholm T, et al. Omega-3 fatty acids enhance phagocytosis of Alzheimer’s disease-related amyloid-β42 by human microglia and decrease inflammatory markers. J Alzheimers Dis. 2013;35:697–713.
Lu DY, Tsao YY, Leung YM, Su KP. Docosahexaenoic acid suppresses neuroinflammatory responses and induces heme oxygenase-1 expression in BV-2 microglia: implications of antidepressant effects for ω-3 fatty acids. Neuropsychopharmacology. 2010;35:2238–48.
Ebert S, Weigelt K, Walczak Y, Drobnik W, Mauerer R, Hume DA, et al. Docosahexaenoic acid attenuates microglial activation and delays early retinal degeneration. Neurochem. 2009;110:1863–75.
Chang CY, Kuan YH, Li JR, Chen WY, Ou YC, Pan HC, et al. Docosahexaenoic acid reduces cellular inflammatory response following permanent focal cerebral ischemia in rats. J Nutr Biochem. 2013;24:2127–37.
Hjorth E, Freund-Levi Y. Immunomodulation of microglia by docosahexaenoic acid and eicosapentaenoic acid. Curr Opin Clin Nutr Metab Care. 2012;15:134–43.
Becerir C, Kılıç İ, Sahin Ö, Özdemir Ö, Tokgün O, Özdemir B, et al. The protective effect of docosahexaenoic acid on the bilirubin neurotoxicity. J Enzyme Inhib Med Chem. 2013;28:801–7.
Gupta S, Knight AG, Gupta S, Keller JN, Bruce-Keller AJ. Saturated long-chain fatty acids activate inflammatory signaling in astrocytes. J Neurochem. 2012;120:1060–71.
Begum G, Kintner D, Liu Y, Cramer SW, Sun D. DHA inhibits ER Ca2+ release and ER stress in astrocytes following in vitro ischemia. J Neurochem. 2012;120:622–30.
Grintal B, Champeil-Potokar G, Lavialle M, Vancassel S, Breton S, Denis I. Inhibition of astroglial glutamate transport by polyunsaturated fatty acids: evidence for a signalling role of docosahexaenoic acid. Neurochem Int. 2009;54:535–43.
Latour A, Grintal B, Champeil-Potokar G, Hennebelle M, Lavialle M, Dutar P, et al. Omega-3 fatty acids deficiency aggravates glutamatergic synapse and astroglial aging in the rat hippocampal CA1. Aging Cell. 2013;12:76–84.
Sheets KG, Jun B, Zhou Y, Zhu M, Petasis NA, Gordon WC, et al. Microglial ramification and redistribution concomitant with the attenuation of choroidal neovascularization by neuroprotectin D1. Mol Vis. 2013;19:1747–59.
Abdelmoaty S, Wigerblad G, Bas DB, Codeluppi S, Fernandez-Zafra T, El-Awady e-S, et al. Spinal actions of lipoxin A4 and 17(R)-resolvin D1 attenuate inflammation-induced mechanical hypersensitivity and spinal TNF release. PLoS One. 2013;8:e75543.
Mizwicki MT, Liu G, Fiala M, Magpantay L, Sayre J, Siani A, et al. 1α, 25-dihydroxyvitamin D3 and resolvin D1 retune the balance between amyloid-β phagocytosis and inflammation in Alzheimer’s disease patients. J Alzheimers Dis. 2013;34:155–70.
Yamanaka M, Ishikawa T, Griep A, Axt D, Kummer MP, Heneka MT. PPARγ/RXRα-induced and CD36-mediated microglial amyloid-β phagocytosis results in cognitive improvement in amyloid precursor protein/presenilin 1 mice. J Neurosci. 2012;32:17321–31.
Bahety P, Tan YM, Hong Y, Zhang L, Chan EC, Ee PL. Metabotyping of docosahexaenoic acid-treated Alzheimer’s disease cell model. PLoS One. 2014;9:e90123.
Seo J, Barhoumi R, Johnson AE, Lupton JR, Chapkin RS. Docosahexaenoic acid selectively inhibits plasma membrane targeting of lipidated proteins. FASEB J. 2006;20:770–2.
Raza Shaikh S, Brown DA. Models of plasma membrane organization can be applied to mitochondrial membranes to target human health and disease with polyunsaturated fatty acids. Prostaglandins Leukot Essent Fatty Acids. 2013;88:21–5.
Grimm MO, Kuchenbecker J, Grösgen S, Burg VK, Hundsdörfer B, Rothhaar TL, et al. Docosahexaenoic acid reduces amyloid beta production via multiple pleiotropic mechanisms. J Biol Chem. 2011;286:14028–39.
Fabelo N, Martín V, Marín R, Moreno D, Ferrer I, Díaz M. Altered lipid composition in cortical lipid rafts occurs at early stages of sporadic Alzheimer’s disease and facilitates APP/BACE1 interactions. Neurobiol Aging. 2014;35:1801–12.
Oksman M, Iivonen H, Hogyes E, Amtul Z, Penke B, Leenders I, et al. Impact of different saturated fatty acid, polyunsaturated fatty acid and cholesterol containing diets on beta-amyloid accumulation in APP/PS1 transgenic mice. Neurobiol Dis. 2006;23:563–72.
Eckert GP, Chang S, Eckmann J, Copanaki E, Hagl S, Hener U, et al. Liposome-incorporated DHA increases neuronal survival by enhancing non-amyloidogenic APP processing. Biochim Biophys Acta. 1808;2011:236–43.
Torres M, Price SL, Fiol-Deroque MA, Marcilla-Etxenike A, Ahyayauch H, Barceló-Coblijn G, et al. Membrane lipid modifications and therapeutic effects mediated by hydroxydocosahexaenoic acid on Alzheimer’s disease. Biochim Biophys Acta. 1838;2014:1680–92.
Zhang C, Bazan NG. Lipid-mediated cell signaling protects against injury and neurodegeneration. J Nutr. 2010;140:858–63.
Hashimoto M, Katakura M, Hossain S, Rahman A, Shimada T, Shido O. Docosahexaenoic acid withstands the Aβ (25-35)-induced neurotoxicity in SH-SY5Y cells. J Nutr Biochem. 2011;22:22–9.
Sublimi Saponetti M, Grimaldi M, Scrima M, Albonetti C, Nori SL, Cucolo A. Aggregation of Aβ (25-35) on DOPC and DOPC/DHA bilayers: an atomic force microscopy study. PLoS One. 2014;9:e115780.
Calon F, Lim GP, Yang F, Morihara T, Teter B, Ubeda O, et al. Docosahexaenoic acid protects from dendritic pathology in an Alzheimer’s disease mouse model. Neuron. 2004;43:633–45.
Calon F, Cole G. Neuroprotective action of omega-3 polyunsaturated fatty acids against neurodegenerative diseases: evidence from animal studies. Prostaglandins Leukot Essent Fat Acids. 2007;77:287–93.
Lim GP, Calon F, Morihara T, Yang F, Teter B, Ubeda O, et al. A diet enriched with the omega-3 fatty acid docosahexaenoic acid reduces amyloid burden in an aged Alzheimer mouse model. J Neurosci. 2005;25:3032–40.
Arsenault D, Julien C, Tremblay C, Calon F. DHA improves cognition and prevents dysfunction of entorhinal cortex neurons in 3xTg-AD mice. PLoS One. 2011;6:e17397.
Perez SE, Berg BM, Moore KA, He B, Counts SE, Fritz JJ, et al. DHA diet reduces AD pathology in young APPswe/PS1 delta E9 transgenic mice: possible gender effects. J Neurosci Res. 2010;88:1026–40.
Hashimoto M, Tozawa R, Katakura M, Shahdat H, Haque AM, Tanabe Y, et al. Protective effects of prescription n-3 fatty acids against impairment of spatial cognitive learning ability in amyloid β-infused rats. Food Funct. 2011;2:386–94.
Green KN, Martinez-Coria H, Khashwji H, Hall EB, Yurko-Mauro KA, Ellis L, et al. Dietary docosahexaenoic acid and docosapentaenoic acid ameliorate amyloid-beta and tau pathology via a mechanism involving presenilin 1 levels. J Neurosci. 2007;27:4385–95.
Hooijmans CR, Rutters F, Dederen PJ, Gambarota G, Veltien A, van Groen T, et al. Changes in cerebral blood volume and amyloid pathology in aged Alzheimer APP/PS1 mice on a docosahexaenoic acid (DHA) diet or cholesterol enriched typical western diet (TWD). Neurobiol Dis. 2007;28:16–29.
Fiol-deRoque MA, Gutierrez-Lanza R, Terés S, Torres M, Barceló P, Rial RV, et al. Cognitive recovery and restoration of cell proliferation in the dentate gyrus in the 5XFAD transgenic mice model of Alzheimer’s disease following 2-hydroxy-DHA treatment. Biogerontology. 2013;14:763–75.
Vedin I, Cederholm T, Freund-Levi Y, Basun H, Garlind A, Irving GF, et al. Effects of DHA-rich n-3 fatty acid supplementation on gene expression in blood mononuclear leukocytes: the OmegAD study. PLoS One. 2012;7:e35425.
Freund Levi Y, Vedin I, Cederholm T, Basun H, Faxén Irving G, Eriksdotter M, et al. Transfer of omega-3 fatty acids across the blood-brain barrier after dietary supplementation with a docosahexaenoic acid-rich omega-3 fatty acid preparation in patients with Alzheimer’s disease: the OmegAD study. J Intern Med. 2014;275:428–36.
Cederholm T, Salem Jr N, Palmblad J. ω-3 fatty acids in the prevention of cognitive decline in humans. Adv Nutr. 2013;4:672–6.
Quinn JF, Raman R, Thomas RG, Yurko-Mauro K, Nelson EB, Van Dyck C, et al. Docosahexaenoic acid supplementation and cognitive decline in Alzheimer disease: a randomized trial. JAMA. 2010;304:1903–11.
Chouinard-Watkins R, Rioux-Perreault C, Fortier M, Tremblay-Mercier J, Zhang Y, et al. Disturbance in uniformly 13C-labelled DHA metabolism in elderly human subjects carrying the apoE ε4 allele. Br J Nutr. 2013;110:1751–9.
Vandal M, Alata W, Tremblay C, Rioux-Perreault C, Salem Jr N, Calon F, et al. Reduction in DHA transport to the brain of mice expressing human APOE4 compared to APOE2. J Neurochem. 2014;129:516–26.
Conway V, Allard MJ, Minihane AM, Jackson KG, Lovegrove JA, Plourde M. Postprandial enrichment of triacylglycerol-rich lipoproteins with omega-3 fatty acids: lack of an interaction with apolipoprotein E genotype? Lipids Health Dis. 2014;13:148.
Dang TM, Conway V, Plourde M. Disrupted fatty acid distribution in HDL and LDL according to apolipoprotein E allele. Nutrition. 2015;31:807–12.
Terwel D, Steffensen KR, Verghese PB, Kummer MP, Gustafsson JÅ, Holtzman DM, et al. Critical role of astroglial apolipoprotein E and liver X receptor-α expression for microglial Aβ phagocytosis. J Neurosci. 2011;31:7049–59.
Casali BT, Corona AW, Mariani MM, Karlo JC, Ghosal K, Landreth GE. Omega-3 fatty acids augment the actions of nuclear receptor agonists in a mouse model of Alzheimer’s disease. J Neurosci. 2015;35:9173–81.
Tai LM, Koster KP, Luo J, Lee SH, Wang YT, Collins NC, et al. Amyloid-β pathology and APOE genotype modulate retinoid X receptor agonist activity in vivo. J Biol Chem. 2014;289:30538–55.
Conquer JA, Tierney MC, Zecevic J, Bettger WJ, Fisher RH. Fatty acid analysis of blood plasma of patients with Alzheimer’s disease, other types of dementia, and cognitive impairment. Lipids. 2000;35:1305–12.
Tully AM, Roche HM, Doyle R, Fallon C, Bruce I, Lawlor B, et al. Low serum cholesteryl ester-docosahexaenoic acid levels in Alzheimer’s disease: a case-control study. Br J Nutr. 2003;89:483–9.
Wang W, Shinto L, Connor WE, Quinn JF. Nutritional biomarkers in Alzheimer’s disease: the association between carotenoids, n-3 fatty acids, and dementia severity. J Alzheimers Dis. 2008;13:31–8.
Astarita G, Jung KM, Berchtold NC, Nguyen VQ, Gillen DL, Head E, et al. Deficient liver biosynthesis of docosahexaenoic acid correlates with cognitive impairment in Alzheimer’s disease. PLoS One. 2010;5:e12538.
Plourde M, Fortier M, Vandal M, Tremblay-Mercier J, Freemantle E, Bégin M, et al. Unresolved issues in the link between docosahexaenoic acid and Alzheimer’s disease. Prostaglandins Leukot Essent Fatty Acids. 2007;77:301–8.
Cole GM, Frautschy SA. Docosahexaenoic acid protects from amyloid and dendritic pathology in an Alzheimer’s disease mouse model. Nutr Health. 2006;18:249–59.
McGahon BM, Martin DS, Horrobin DF, Lynch MA. Age-related changes in synaptic function: analysis of the effect of dietary supplementation with ω-3 fatty acids. Neuroscience. 1999;94:305–14.
Lee LK, Shahar S, Chin AV, Yusoff NA. Docosahexaenoic acid-concentrated fish oil supplementation in subjects with mild cognitive impairment (MCI): a 12-month randomised, double-blind, placebo-controlled trial. Psychopharmacology (Berl). 2013;225:605–12.
Fiala M, Halder RC, Sagong B, Ross O, Sayre J, Porter V, et al. ω-3 supplementation increases amyloid-β phagocytosis and resolvin D1 in patients with minor cognitive impairment. FASEB J. 2015;29:2681–9.
Daiello LA, Gongvatana A, Dunsiger S, Cohen RA, Ott BR, Alzheimer’s Disease Neuroimaging Initiative. Association of fish oil supplement use with preservation of brain volume and cognitive function. Alzheimers Dement. 2015;11:226–35.
Jernerén F, Elshorbagy AK, Oulhaj A, Smith SM, Refsum H, Smith AD. Brain atrophy in cognitively impaired elderly: the importance of long-chain ω-3 fatty acids and B vitamin status in a randomized controlled trial. Am J Clin Nutr. 2015;102:215–21.
van Neerven S, Kampmann E, Mey J. RAR/RXR and PPAR/RXR signaling in neurological and psychiatric diseases. Prog Neurobiol. 2008;85:433–51.
Acknowledgements
David Heras-Sandoval is supported by a postdoctoral grant from Dirección General de Asuntos de Personal Académico (DGAPA) of the Universidad Nacional Autónoma de México (UNAM).
Jazmin M Pérez-Rojas is supported by a research grant 178946 from Mexican Council of Science and Technology (CONACYT).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DHS carried out the writing and illustrations of the study and JMPR and JPC contributed to the revision and edition of the study. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Heras-Sandoval, D., Pedraza-Chaverri, J. & Pérez-Rojas, J.M. Role of docosahexaenoic acid in the modulation of glial cells in Alzheimer’s disease. J Neuroinflammation 13, 61 (2016). https://doi.org/10.1186/s12974-016-0525-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-016-0525-7