Abstract
Background
Most of the objective and quantitative methods proposed for spasticity measurement are not suitable for clinical application, and methods for surface electromyography (sEMG) signal processing are mainly limited to the time-domain. This study aims to quantify muscle activity in the time–frequency domain, and develop a practical clinical method for the objective and reliable evaluation of the spasticity based on the Hilbert–Huang transform marginal spectrum entropy (HMSEN) and the root mean square (RMS) of sEMG signals.
Methods
Twenty-six stroke patients with elbow flexor spasticity participated in the study. The subjects were tested at sitting position with the upper limb stretched towards the ground. The HMSEN of the sEMG signals obtained from the biceps brachii was employed to facilitate the stretch reflex onset (SRO) detection. Then, the difference between the RMS of a fixed-length sEMG signal obtained after the SRO and the RMS of a baseline sEMG signal, denoted as the RMS difference (RMSD), was employed to evaluate the spasticity level. The relations between Modified Ashworth Scale (MAS) scores and RMSD were investigated by Ordinal Logistic Regression (OLR). Goodness-of-fit of the OLR was obtained with Hosmer–Lemeshow test.
Results
The HMSEN based method can precisely detect the SRO, and the RMSD scores and the MAS scores were fairly well related (test: χ2 = 8.8060, p = 0.2669; retest: χ2 = 1.9094, p = 0.9647). The prediction accuracies were 85% (test) and 77% (retest) when using RMSD for predicting MAS scores. In addition, the test–retest reliability was high, with an interclass correlation coefficient of 0.914 and a standard error of measurement of 1.137. Bland–Altman plots also indicated a small bias.
Conclusions
The proposed method is manually operated and easy to use, and the HMSEN based method is robust in detecting SRO in clinical settings. Hence, the method is applicable to clinical practice. The RMSD can assess spasticity in a quantitative way and provide greater resolution of spasticity levels compared to the MAS in clinical settings. These results demonstrate that the proposed method could be clinically more useful for the accurate and reliable assessment of spasticity and may be an alternative clinical measure to the MAS.
Similar content being viewed by others
Background
Spasticity is a serious and potentially disabling complication of stroke [1]. In the commonly accepted definition, spasticity is characterized by an increase in muscle tension during passive stretching, which is velocity-dependent and results from the hyperexcitability of the stretch reflex [2, 3]. Accurate and reliable assessment of spasticity is crucial for designing optimal treatment plans or evaluating potential effects of treatment interventions [4, 5].
At present, the dominant clinical method for assessing spasticity is the Modified Ashworth Scale (MAS), which provides for great simplicity in clinical assessment, but nonetheless represents a semi-quantitative method that depends on subjective physiotherapists evaluations based on experience [6,7,8,9,10,11]. Moreover, the method provides ambiguous descriptions such as “more marked (MAS 2), slight increase (MAS 1 and MAS 1+) in muscle tone”, which leads to equally ambiguous and imprecise results such as “1 to 1+” or “1+ to 2” [5].
The subjective and imprecise assessments of spasticity are not sensitive enough to slight changes of patient’s status [12]. They may misestimate the rehabilitation state of patients and lead to an inaccurate understanding of the characteristics of spasticity, thereby affecting the longitudinal follow-up of patients. They may also undermine the evaluation of the performance of therapeutic resources and misjudge the efficacy of an intervention in the clinical management of spasticity, thereby affecting the interventions, such as dose adjustment of anti-spasticity drugs or design of physiotherapy options.
Many studies have reported on the inaccurate and unreliable results obtained in the clinical assessment of spasticity, demonstrating the need to improve assessment accuracy and reliability [13,14,15,16]. However, most of these proposed methods have been criticized for being too cumbersome and inconvenient to apply in clinical settings [17,18,19,20].
Among the proposed methods, the tonic stretch reflex threshold (TSRT) seems to be the most promising approach [21]. The stretch reflex threshold (SRT) refers to the joint angle at which motoneurons and respective muscles begin to be recruited, and this onset of muscle recruitment is referred to as the stretch reflex onset (SRO), which can be detected based on surface electromyography (sEMG) activity [22, 23]. The TSRT represents the angle at which the SRO is detected when the muscle is at rest (i.e., at zero stretch velocity).
However, no consensus has yet been attained regarding the detection of the SRO [23]. In clinical settings, current approaches for detection of the SRO are mainly based on visual interpretation (VI) or time-domain signal analysis methods [24, 25]. These methods readily result in the erroneous detection of the SRO because sEMG signals are weak and vulnerable to interference. Additionally, the estimation of TSRT relies on a number of preliminary measurements with different stretching velocities that must be carefully undertaken in advance [26]. Finally, spasticity assessment based on the TSRT requires measurement of the joint angle and sEMG signal synchronously. It is quite difficult to realize ideal synchronous sampling in an actual testing environment because synchronization errors for separately sampled values always exist. In summary, spasticity assessment methods based on the TSRT are not practicable for clinical settings.
The nature of sEMG signals presents numerous processing challenges. sEMG signal is sparsely distributed in the time–frequency domain, and current detection approaches only expand signal in the time domain. The more detailed information in each frequency component is absent [25]. As such, a time–frequency representation is required to facilitate the SRO detection [25]. Moreover, sEMG signals seem to be nonlinear or even chaotic in nature. Therefore, nonlinear time series analysis methods, for example, entropy, may achieve improved performance over the methods relying on time domain parameter [27, 28]. Hence, a signal processing method that combines nonlinear dynamics and time–frequency analysis is more suitable for sEMG signal processing.
The Hilbert–Huang transform (HHT) is a relatively new time–frequency analysis approach, which is well suited for processing non-linear, non-stationary signals such as sEMG signals [29]. HHT marginal spectrum entropy (HMSEN) analysis is based on HHT and entropy, and the method of HMSEN has been used and acquired good performance in non-linear and non-stationary signal processing [30].
This study proposes a new practical clinical assessment method based on the HMSEN and the root mean square (RMS) of sEMG signals. The method detects the SRO based on the HMSEN of sEMG signals, and directly assesses spasticity quantitatively based on the difference between the RMS of a fixed-length sEMG signal obtained after the SRO and the RMS of a baseline sEMG signal.
The objectives of this study are to determine (1) the ability of the HMSEN to detect the SRO, (2) the relationship between the spasticity levels obtained clinically based on the MAS and the RMS difference measured from sEMG signals, (3) the test–retest reliability of the proposed method between days, and finally to (4) develop a clinical practical method of spasticity assessment, which is simple to operate and could provide greater resolution of spasticity level and better treatment and rehabilitation programs in clinical settings.
Methods
Subjects
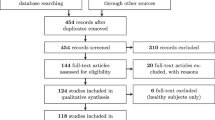
Twenty-six patients (19 males and 7 females) with stroke participated in the study (mean age 53.85 ± 15.39, range 21–80 years). All the subjects were from Anhui Provincial Hospital. The study was approved by the ethics committee of Anhui Provincial Hospital. All subjects gave written informed consent approved by Anhui Provincial Hospital. For assuring confidentiality, the subjects were identified through the use of an Arabic numeral code, and no identifying information was recorded (i.e., no names, addresses, or contact information).
Subjects were included if they had (a) sustained a stroke; (b) elbow flexor spasticity; (c) at least a 90° passive range of motion in the elbow joint; (d) good awareness and no serious cognitive, visual, or auditory disorders.
Subjects were excluded if they had (a) other concurrent central nervous system disorders that may lead to myodystonia, e.g., Parkinson’s syndrome or multiple sclerosis; (b) other concurrent diseases that may compromise movement of the upper limb elbow joints, e.g., upper limb fracture or pain.
Each subject’s eligibility was carefully reviewed by an attending physician. The clinical characteristics of the 26 participants are listed in Table 1.
Sensing system
Acquisition of the sEMG signal from the biceps brachii was accomplished using three electrodes via a three-point differential input. The patient’s skin at the points of electrode application was first wiped with an alcohol-soaked cotton swab to remove surface grease and dander. Two electrodes corresponding to the sEMG differential input were placed over the motor point of the biceps brachii muscles along the direction of the muscle fibers. The centers of the two electrodes were separated by 20 mm. The remaining electrode was designed as a reference point and was placed over the skin without any muscle activity.
The acquired sEMG signals were first filtered and amplified. The sEMG acquisition system consisted of a 10 Hz notch filter and a 500 Hz low-pass filter to remove the noise of the sEMG signals, and the filtered signals were amplified by a factor of 1000. The sEMG signals were then converted via a 12-bit analog to digital converter (ADC) (ADS1198, Texas Instruments, Dallas, TX, USA) at a sampling rate of 1 kHz, and transferred to a personal computer via USB ports. To store and analyze the data obtained during the study, data acquisition software were developed using Microsoft Foundation Classes (MFC). The trace of sEMG signals was continuously displayed on a monitor, and simultaneously stored on the computer. The data were employed to detect the SRO for each subject tested and investigate the correlation between the RMSD and MAS scores.
Experimental protocol
Each subject was tested in a seated position with the upper limb stretched toward the ground. Prior to assessment, a professional physiotherapist manually stretched the upper limb of each subject to assist the subject in adapting to the extension activity to avoid inaccuracy of spasticity assessment due to sudden extension. Subsequently, the physiotherapist performed a standard MAS scoring for each subject at a proper stretch velocity based on his professional experience. Here, we define elbow extension as a motion from full flexion, which represents the maximum flexion allowed by the upper arm and forearm without making contact between them, to full extension, representing the maximum extension allowed by the arm and the forearm. An MAS testing session consisted of a single elbow extension (Fig. 1). For purposes of statistical coding, ‘1+’ on the MAS was assigned a value of 1.5 in this study. Spasticity was evaluated in two sessions, denoted as test and retest, separated by an interval of 3–5 days. To minimize the influence of environmental and stress factors on spasticity assessment, all assessments were performed by the same physiotherapist, at approximately the same time of day, at the same location, and at a room temperature of 25 °C.
SRO
Patients with spasticity have suffered damage to their upper motor neurons. The central lesion disrupts the balance of supraspinal inhibitory and excitatory inputs directed to the spinal cord, leading to a state of disinhibition of the stretch reflex. Decreased postsynaptic inhibition is involved in the hyperexcitability of the stretch reflex, which ultimately changes the electrophysiological output, manifesting as an increased complexity of sEMG signals in the time and frequency domain [31, 32]. This feature allows for the determination of the SRO using the HMSEN.
HHT marginal spectral entropy
The fundamental component of HHT [29] is the empirical mode decomposition (EMD) method and the Hilbert transform. Application of EMD to an original time-based signal x(t) provides n intrinsic mode functions (IMFs) ci(t) and a residue signal rn(t) as follows:
For any ci(t), its Hilbert transform H(ci(t)) is defined as:
To construct the analytic signal:
where ai(t) and φi(t) are the amplitude and instantaneous phase, which are respectively given as
Correspondingly, x(t) can be expressed as
where fi(t) is the instantaneous frequency, which is defined as
The Hilbert–Huang spectrum is then defined to represent the frequency–time distribution of the amplitude:
Then, Eq. (8) is subjected to an integration over t to generate the Hilbert marginal spectrum of the signal:
The marginal spectrum offers a measure of total amplitude (or energy) contribution from each frequency value. Equation (9) can be rewritten to generate h(i) for discrete frequency points f = iΔf:
where n represents the number of discrete frequency points within each analytic frequency band.
Correspondingly, the HMSEN is expressed according to the definition of information entropy as
where pi = h(i)/∑h(i), and pi is the probability of occurrence of an event and here it refers the probability density of the spectrum and the occurrence probability of amplitude corresponding to the i th frequency.
The HMSEN values are then normalized in the range [0, 1], yielding the new HMSEN as follows:
where N represents the sequence length of h(i).
SRO detection algorithm
The HMSEN of sEMG signals obtained from the biceps brachii of patients was employed to detect the SRO according to the following procedure as shown in Fig. 2. First, the sEMG signal was framed by a sliding window of fix-length (k points) with a frame shift of m points. The HMSEN of each signal frame was calculated and denoted as MsEn. Subsequently, an adaptive threshold Th was set according to minimum and maximum values of MsEn [i.e., min(MsEn) and max(MsEn), respectively] as follows:
where λ is the sensitivity factor of Th. Here, the MsEn values were adjusted according to Th, where MsEn values less than Th were reassigned as 0, and MsEn values greater than Th were retained. The adjusted MsEn values are denoted as En. If, at a given point in time, an En value was greater than 0 and all n consecutive En values afterward were greater than 0, that point in time was determined to be the SRO. Considering a reasonable tradeoff between the computational burden and the desired level of accuracy, the values of these parameters were set as k = 90, m = 3, n = 50, and λ = 0.3 or 0.35.
The detection algorithm is outlined in Fig. 2, and was implemented in MATLAB (version 8.3, R2014a).
Activity bursts of short duration (25–40 ms) are considered to have little effect on the resulting kinetic output [33]. Therefore, the present study employed an interval [t0 − 50, t0 + 50] to obtain the recognition rate of the algorithm. The recognition rate is defined as
where TD and FD represent the number of true detection and false detection, respectively. A classification is counted as TD if the detected onset time is within the interval [t0 − 50, t0 + 50], and classifications are counted as FD if the detected onset time is outside the interval [t0 − 50, t0 + 50]. Here, t0 is the onset time obtained by the physiotherapist using VI.
The most cited method proposed by Calota A to measure TSRT [22], in which SRO was defined as the point at which the EMG signal increased 2 (standard deviation) SDs above the mean baseline EMG was selected for our performance comparison tests. Baseline EMG was the EMG activity while the subject was at rest before beginning the evaluation session. This method will be referred to as “SD detection” from now on.
The performance of the proposed method was evaluated using semi-synthetic sEMG signals where the onset time was artificially set. To construct the semi-synthetic sEMG signals employed for testing, we collected actual sEMG signals of the biceps brachii of elbow flexor spasticity patients, and two types of experimental signals were first identified. The first type represents quiescent baselines obtained during passive stretching. The second type represents clear sEMG signals where SRO occurred during passive stretching. The duration of each segment was 1000 ms.
Spasticity assessment based on the RMSD
The SRO is accompanied by an excessive reflex activation of α-motoneurons, and the number of excitatory motoneurons and the electric activity are both increased. As a result, the RMS values of the sEMG signals increase with increasing muscle tension [34]. Hence, the spasticity level can be quantified using the RMS of the sEMG signals. However, some studies found that the sEMG signal showed differences in power spectrum even it was obtained when same action was performed by different individuals, and the differences still existed when the same individual performed the same action at different time [35]. Significant differences in signal amplitudes were also found in the baseline sEMG signals of the same subject. Hence, to eliminate the effects of individual differences of sEMG signals to the lowest, the difference between the RMS of sEMG signals obtained after the SRO and the RMS of baseline sEMG signals, henceforth defined as the RMSD, was employed to assess the spasticity level quantitatively. In consideration of the fact that the muscle continues contracting if the stretch is maintained (stretch velocity = 0) according to sEMG recordings [31], a fixed signal length of 1000 ms was adopted for assessing spasticity by this method. For short time-series, a fixed signal length of 500 ms was adopted.
The RMS is as follow:
where Xi is the i th sampling value of sEMG signals.
Statistical analysis
The relations between MAS scores and RMSD are investigated by Ordinal Logistic Regression (OLR) using R software. The quality of the RMSD in spasticity assessment was evaluated by how well the classes of the MAS test were predicted by the RMSD based on confusion matrix. Goodness-of-fit of the OLR was assessed with Hosmer–Lemeshow test with the R package generalhoslem [36]. The test–retest reliability was examined using (1) the interclass correlation coefficient (ICC) one-way random effects model for single measures [37], implemented using SPSS Statistics (IBM, Version 21.0), (2) Bland–Altman 95% limits of agreement (LOA) [38], implemented using MedCalc statistical software (version 15.8), and (3) standard errors of measurement (SEM) [39]. We employed ICC and SEM together because ICC is a relative measure of reliability that reflects the ability of the measurements to differentiate between participants, while SEM is an absolute measure. A one way ANOVA and post hoc test were used to compare the RMSDs among all subjects [20]. All statistical tests were conducted at a significance level of p = 0.05.
Results
SRO detection
The data processing results based on the developed detection algorithm for subjects 1, 2, 7, and 19 with varying MAS levels are shown in Figs. 3, 4, 5 and 6, respectively. In the experimental results of subject 1 with an MAS score of 2 (Fig. 3), the HMSEN is approximately 0.25 prior to the SRO and approximately 0.5 after the SRO, which represents a significant difference before and after the SRO. Likewise, the experimental results of subject 2 with MAS 1+ (Fig. 4), subject 7 with MAS 1 (Fig. 5) and subject 19 with MAS 1+ (Fig. 6) demonstrate significant differences in their HMSEN values before and after the SRO as well, indicating that the HMSEN based method can reliably identify the SRO. According to Eq. (14), the results demonstrate that the HMSEN based method obtained a high SRO recognition rate of 96.3%.
Performance comparison
Figure 7 presents the performance comparison result. The vertical dashed lines indicate the SROs, which are detected by the SD detection method using different baselines. Visual inspection of the figure shows that a slight change in the baseline EMG signals may lead to a substantial change in the detection result (max error: 991 ms) when using SD detection. However, the SROs detected by the proposed approach, which are indicated by the vertical solid lines, show a smaller error (max error: 69 ms) and a better stability. Hence, the HMSEN based method appears to be more accurate and more robust than the SD detection method for SRO detection.
Performance comparison result: the vertical dashed line indicates SRO detected by SD detection, and the vertical solid line indicates SRO detected by our approach. The numbers next to the dashed line indicate the SD of the baseline sEMG signals. The solid lines from left to right indicate the SRO detection results when the sensitivity factor of Th is 0.3, 0.35 and 0.45
Spasticity assessments
The RMSD of each subject is listed in Table 2. The scatter plot below shows the distribution of the RMSD of test (Fig. 8) and the RMSD of retest (Fig. 9) according to the MAS classification of the patients. The distribution of RMSD shows less variability than the RMSD of retest: except for three scores, the RMSD are monotonically related to the MAS classification. For the retest, the monotonic relation is less clear.
An OLR was performed with the three levels of the MAS score as outcome measure and RMSD test as a predictor. The Hosmer–Lemeshow test (Table 3) shows significant goodness of fit and that the RMSD scores and the MAS scores are fairly well related (χ2 = 8.8060, p = 0.2669). Regarding the retest, the RMSD scores and the MAS scores are also fairly well related (χ2 = 1.9094, p = 0.9647), which demonstrates that the RMSD can quantitatively assess the level of upper limb spasticity.
The confusion matrix (Table 4) shows how the MAS scores predicted with the RMSD (test) correspond to the observed MAS scores of the patients. The six patients who were classified with a MAS score of 2, all have a predicted score of 2 based on their RMSD scores. Not all patients are correctly classified: two patients were classified with MAS score of 1, but the predicted score based on RMSD is 1+, and for another two patients exactly the opposite occurs: observed MAS score is 1+, predicted based on RMSD is equal to 1. Overall the accuracy of the test is good: 0.85, 95% CI = (0.65, 0.96), which means that 85% of the patients were correctly classified. The confusion matrix of retest (Table 5) shows that the patients are less well classified based on the RMSD of retest: overall accuracy of the retest is equal to 0.77, 95% CI = (0.56, 0.91), which means that 78% of the patients were correctly classified.
However, the goodness-of-fit of the OLR when considering only the RMS of sEMG signals after the SRO are (test: χ2 = 7.3070, p = 0.3976; retest: χ2 = 3.8367, p = 0.7984), and overall accuracy of the test and retest are 0.77 and 0.62 predicted predicting MAS scores with the RMSD respectively. These results mean the RMSD can achieve improved performance over the RMS in spasticity assessment, and decrease the individual difference effect to some degree.
Test–retest reliability
The results of the test–retest reliability study are listed in Table 6. In addition, a Bland–Altman plot showing the mean RMSD over a period of two test days (X-axis), the difference in the RMSD values between the test days (Y-axis), and the 95% LOA (dashed lines), is presented in Fig. 10. We note from Table 6 that the ICC scores indicate good agreement between the two tests with an ICC of 0.914. The SEM value is very small (1.137). Finally, the Bland–Altman 95% LOA results also suggest a small bias with 92.3% (24/26) of the data points lying within the LOA.
Spasticity level discrimination performance of the MAS
Through a post hoc analysis by means of the Bonferroni test, it was found that the differences between the RMSD values of the MAS 1 group and that of the MAS 1+ group (retest: p = 0.089) were not significant.
Discussion
The objective of this study was to evaluate the level of spasticity easily, accurately, and reliable by combining the characteristics of both the MAS and sEMG signals. One advantage of the proposed approach is that the elbow flexors are manually stretched by the rater, instead of by isokinetic-dynamometer-like devices which may make the spasticity assessment more complicated. Another advantage is that it measures the RMS of sEMG signals after the SRO, rather than the TSRT, and the strict synchronous acquisition of the sEMG signals and the joint angle is no longer needed. Hence, the proposed method is more practical in clinical practice due to its compactness and portability. It is not clear whether it is absolutely necessary to apply constant velocity when measuring spastic joint stiffness [40]. Therefore, our manual methods and device might be a better measure of spasticity than those used in current practice and play an important role in further studies for spasticity measurement in clinical settings. Additionally, a novel approach for detecting SRO was presented based on time–frequency analysis and nonlinear dynamics, which is robust in detecting the SRO in clinical settings.
Patient selection
Patients with MAS score 0, 3 and 4 are excluded from this experiment because the instructions of MAS score 0 and score 4 are obvious: either no resistance felt (score 0) or no movement possible (score 4) [41]. Therefore, the evaluation of spasticity levels of patients with MAS 0 and MAS 4 is simple and clear, and the chances of misdiagnosis barely exist. What’s more, the ROM of patients with MAS score 3 is very small, the chances of misdiagnosis barely exist as well. However, the descriptions of MAS score 1, 1+ and 2, such as “more marked (MAS 2), or slight increase (MAS 1 or 1+) in muscle tone”, as we discussed in Background, are qualitative and ambiguous Therefore, we only recruited patients with MAS score 1, 1+ and 2. Patients with these scores comprise the majority, and physiotherapists are tending to make mistakes when assessing the spasticity levels of patients with these scores in a clinical setting. Furthermore, the distribution of our dataset is similar to many studies [42,43,44], which indicate that only a small percentage of individuals with chronic stroke exhibit scores at the upper two levels of the MAS under passive extension of the elbow.
Results analysis
We note that the recognition rate of 96.3% obtained by the HMSEN is considerably greater than the recognition rate of 87.5% correspondence with VI using the Teager-Kaiser Energy Operator method [23]. Hence, the HMSEN based method achieved improved performance over the methods relying on conventional SD detection and the Teager Kaiser Energy domain. The HMSEN also presents definite advantages relative to the sample entropy of sEMG signals, which currently has been employed for detecting the onset of muscle activity [45]. Despite the significant performance of the standard sample entropy in physiological signals processing, it does require more various parameters, such as the dimension and the tolerance, first be empirically established to obtain accurate results [46]. However, the HMSEN approach needs less parameter settings, resulting in enhanced practicability for clinicians. Overall, the HMSEN approach for SRO detection is more suitable for clinical settings.
While this study provides some evidence for the good test–retest reliability of the system, Rankin and Stokes [47] have recommended that a large sample size of at least 50 is required for an accurate evaluation of the 95% LOA. As such, our sample size of 26 subjects does not provide for an accurate calculation of the Bland–Altman LOA, which limits the credibility of our test–retest reliability study. Additionally, unlike the ICC, the SEM provides an absolute index of reliability [39], which is of greater usefulness to clinicians. In this study, the RMSD varies from 1.0797 to 16.3307, so an SEM of 1.137 may have little effect on the spasticity level measured by the RMSD. However, the SEM value obtained was slightly greater for patients with MAS 1 than that obtained for other spasticity levels, and we preliminarily hypothesize that this may be the result of the small sample size. Thus, better test–retest reliability data can be expected for a larger sample size.
No significant differences of the average RMSDs between the MAS1 and MAS1+ groups were detected (retest: p = 0.089). Hence, this supports the questionability of the MAS due to its subjectivity and the equivocal descriptions employed, where the rate of change in passive resistance and the joint angle at the onset of stretching are what physiotherapists actually examine based on their experience [48]. In this sense, spasticity assessment based on RMSD is aligned with the study of Damiano DL in [48]. Additionally, the MAS grades spasticity through only 6 levels, but the RMSD varies from 1.0797 to 16.3077. Therefore, our manual method might be more reasonable for providing an accurate, reliable, detailed, and discriminative evaluation of spasticity once its reliability and validity are established further.
Study limitations
Considerable work is required before the proposed system can be adopted as a practical clinical tool. Firstly, we note that examiners typically did not take the velocity-dependent character of spasticity into account during MAS evaluation, and the elbow extension of the patients was conducted according to their experience and visual feedback. As such, the RMSD must also be considered at different stretch velocities. Thus, we plan to investigate the impact of the stretch velocity on the experimental results in a future study, as well as to develop a clinically simple method of eliminating the influence of different stretch velocities.
Secondly, we acknowledge that the subjects in this study all came from one rehabilitation centre and that the sample is thus relatively small. Therefore, this system should be applied to a larger number of spasticity patients with a greater variation in spasticity levels, particularly patients with MAS 1+ and 2 levels. Besides, we will need to apply our system to patients with various upper motor-neuron disorders, in order to demonstrate its feasibility.
Thirdly, spasticity level was determined by means of the MAS by one physiotherapist, following routine clinical test procedures. However, the MAS has been criticized for inaccuracy and unreliability [7], which may have impact on results. Hence, the inter-rater reliability should be considered in the future. In addition, the value of other clinical scales, for example, Modified Tardieu Scale, as an indicator for the level of spasticity should be further explored. Besides, the SRO detection results may be biased by the length of the sliding window and the interval which is set based on the onset time detected using VI. The assessment of spasticity levels may be biased by the length of sEMG signals for the calculation of RMSD. How to set the optimal parameters for more precise detection of the SRO and more accurate assessment for spasticity should be future studied.
A final limitation of this study is that we only use one single clinical parameter (RMSD) to assess the spasticity levels of patients. In a future study, we plan to equip our device with extra force sensors and use multiple parameters to assess spasticity level, such as the mean power–frequency of sEMG signal, the joint resistance and the SRT.
Clinical implications
A quantitative method to measure spasticity may provide physiotherapists with accurate understanding of spasticity and optimal treatment plans for patients. The proposed method takes the advantages of the MAS and portable manual system and is easy to operate. Hence, the proposed method permits physiotherapists to assess the level of spasticity reliably, easily and unrestrictedly. Compared with the clinical scales for spasticity assessment, which are not sensitive enough to status changes of patients, it can provide clinicians with a greater resolution of spasticity level. Another advantage is that RMSD values can also provide clinicians with insight into the etiology of spasticity in the future, for it mainly demonstrates the neural response to the muscle stretch [49]. From a therapeutical point of view, the proposed method can provide better treatment program. For patients, the proposed method assesses their spasticity level manually, which avoid the uncomfortable muscle stretches, which are forcibly made by locking up the extremity in an instrument [20, 44]. From the view of rehabilitation, it is likely to derive a standardized clinical evaluation protocol for patients with different spasticity levels. It can provide a more refined classification of spasticity grades, which may lead to better healthcare services and better therapeutic intervention for patients, and facilitate the rehabilitation of patients in clinical practice.
Conclusions
This report presented a novel framework for upper limb spasticity assessment based on the analysis of sEMG signals for detecting the SRO and for the direct quantitative assessment of spasticity. Experimental results demonstrated that the HMSEN based method could precisely detect the SRO. The statistical analysis results demonstrated a strong correlation between the RMSD and the MAS scores obtained for spasticity patients, and good test–retest reliability. This method is manually operated and easy to use, so it can make quantitative spasticity assessment readily available in clinical practice, and therefore enhancing diagnostic and recovery of patients. The preliminary results suggest that the proposed method could potentially provide useful clinical information, and may be viewed as an alternative clinical measure to the MAS in clinical settings.
Change history
20 March 2019
After the publication of the original article work [1], it was highlighted that the circuit information and the A/D converter used for acquiring sEMG signal were not correctly reported in the Methods section. The circuit included a 10 Hz high-pass filter instead of 10 Hz notch filter as stated in the original article. The A/D converter was ADS7818, instead of ADS1198 as stated in the original paper. The authors apologize to the readers for the inconvenience.
Abbreviations
- sEMG:
-
surface electromyography
- HHT:
-
Hilbert–Huang transform
- HMSEN:
-
Hilbert–Huang transform marginal spectrum entropy
- RMS:
-
root mean square
- SRO:
-
stretch reflex onset
- RMSD:
-
RMS difference
- MAS:
-
Modified Ashworth Scale
- OLR:
-
Ordinal Logistic Regression
- TSRT:
-
tonic stretch reflex threshold
- SRT:
-
stretch reflex threshold
- VI:
-
visual interpretation
- M:
-
male
- F:
-
female
- R:
-
right
- L:
-
left
- ADC:
-
analog to digital converter
- MFC:
-
Microsoft Foundation Classes
- EMD:
-
empirical mode decomposition
- IMF:
-
intrinsic mode functions
- TD:
-
true detection
- FD:
-
false detection
- SD:
-
standard deviation
- ICC:
-
interclass correlation coefficient
- LOA:
-
limits of agreement
- SEM:
-
standard errors of measurement
References
McCrory P, Turner-Stokes L, Baguley IJ, De Graaff S, Katrak P, Sandanam J, Davies L, Munns M, Hughes A. Botulinum toxin A for treatment of upper limb spasticity following stroke: a multi-centre randomized placebo-controlled study of the effects on quality of life and other person-centred outcomes. J Rehabil Med. 2009;41:536–44.
Dietz V, Sinkjaer T. Spastic movement disorder: impaired reflex function and altered muscle mechanics. Lancet Neurol. 2007;6:725–33.
Pandyan AD, Gregoric M, Barnes MP, Wood D, Van Wijck F, Burridge J, Hermens H, Johnson GR. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil. 2005;27:2–6.
Brashear A, Gordon MF, Elovic E, Kassicieh VD, Marciniak C, Do M, Lee CH, Jenkins S, Turkel C. Intramuscular injection of botulinum toxin for the treatment of wrist and finger spasticity after a stroke. N Engl J Med. 2002;347:395–400.
Park HS, Kim J, Damiano DL. Development of a haptic elbow spasticity simulator (HESS) for improving accuracy and reliability of clinical assessment of spasticity. IEEE Trans Neur Syst Rehabil Eng. 2012;20:361–70.
Pandyan AD, Johnson GR, Price CIM, Curless RH, Barnes MP, Rodgers H. A review of the properties and limitations of the Ashworth and modified Ashoworth scales as a measure of spasticity. Clin Rehabil. 1999;13:373–83.
Fleuren JF, Voerman GE, Erren-Wolters CV, Snoek GJ, Rietman JS, Hermens HJ, Nene AV. Stop using the Ashworth Scale for the assessment of spasticity. J Neurol Neurosur Psychiatry. 2010;81:46–52.
Yam WK, Leung MS. Interrater reliability of Modified Ashworth Scale and modified Tardieu Scale in children with spastic cerebral palsy. J Child Neurol. 2006;21:1031–5.
Klingels K, De Cock P, Molenaers G, Desloovere K, Huenaerts C, Jaspers E, Feys H. Upper limb motor and sensory impairments in children with hemiplegic cerebral palsy. Can they be measured reliably? Disabil Rehabil. 2010;32:409–16.
Mehrholz J, Major Y, Meissner D, Sandi-Gahun S, Koch R, Pohl M. The influence of contractures and variation in measurement stretching velocity on the reliability of the Modified Ashworth Scale in patients with severe brain injury. Clin Rehabil. 2005;19:63–72.
Bhimani RH, Peden-McAlpine C, Gaugler J, Anderson LC. Spasticity over time during acute rehabilitation: a study of patient and clinician scores. Appl Nurs Res. 2016;30:16–23.
Szczerbik E, Kalinowska M, Graff K, Olczak-kowalczyk D, Dąbrowska-Gontarczyk A, Jelonek E, Syczewska M. Use of instrumented spasticity tests in clinical applications. Preliminary results. Biomed Hum Kinet. 2015;7:23–8.
Kim J, Park HS, Damiano DL. Accuracy and reliability of haptic spasticity assessment using HESS (Haptic Elbow Spasticity Simulator). In: Proceedings of the IEEE 2011 annual international conference of the IEEE engineering in medicine and biology society (EMBS), August 30–September 3, Boston. 2011. p. 8527–30. https://doi.org/10.1109/IEMBS.2011.6092104.
Takhashi Y, Komeda T, Koyama H, Yamamoto S, Arimatsu T, Kawakami Y, Inoue K, Ito Y. Development of an upper limb patient simulator for physical therapy exercise. In: Proceedings of the 2011 IEEE international conference on rehabilitation robotics (ICORR), June 29–July 1, Zurich. 2011. https://doi.org/10.1109/ICORR.2011.5975510.
Kikuchi T, Oda K, Furusho J. Leg-robot for demonstration of spastic movements of brain-injured patients with compact magnetorheological fluid clutch. Adv Robotics. 2010;24:671–86.
Grow DI, Wu M, Locastro MJ, Arora SK, Bastian AJ, Okamura AM. Haptic simulation of elbow joint spasticity. In: Proceedings of the 2008 symposium on haptic interfaces for virtual environment and teleoperator systems, March 13–14, Reno. 2008. p. 475–6. http://doi.org/10.1109/HAPTICS.2008.4479997.
Ju MS, Chen JJ, Lee HM, Lin TS, Lin CC, Huang YZ. Time-course analysis of stretch reflexes in hemiparetic subjects using an on-line spasticity measurement system. J Electromyogr Kinesiol. 2000;10:1–14.
Abdollahi I, Taghizadeh A, Shakeri H, Eivazi M, Jaberzadeh S. The relationship between isokinetic muscle strength and spasticity in the lower limbs of stroke patients. J Bodyw Mov Ther. 2015;19:284–90.
Bar-On L, Aertbeliën E, Wambacq H, Severijns D, Lambrecht K, Dan B, Huenaerts C, Bruyninckx H, Janssens L, Van Gestel L, Jaspers E, Molenaers G, Desloovere K. A clinical measurement to quantify spasticity in children with cerebral palsy by integration of multidimensional signals. Gait Posture. 2013;38:141–7.
Kim KS, Seo JH, Song CG. Portable measurement system for the objective evaluation of the spasticity of hemiplegic patients based on the tonic stretch reflex threshold. Med Eng Phys. 2011;33:62–9.
Germanotta M, Taborri J, Rossi S, Frascarelli F, Palermo E, Cappa P, Castelli E, Petrarca M. Spasticity measurement based on tonic stretch reflex threshold in children with cerebral palsy using the PediAnklebot. Front Hum Neurosci. 2017;11:1–11.
Calota A, Feldman AG, Levin MF. Spasticity measurement based on tonic stretch reflex threshold in stroke using a portable device. Clin Neurophysiol. 2008;119:2329–37.
Malone A, Meldrum D, Gleeson J, Bolger C. Reliability of surface electromyography timing parameters in gait in cervical spondylotic myelopathy. J Electromyogr Kinesiol. 2011;21:1004–10.
Cheng J, Chen X, Peng H. An onset detection method for action surface electromyography based on sample entropy. Acta Electronica Sinica. 2016;44:479–84.
Liu J, Ying D, Rymer WZ. EMG burst presence probability: a joint time–frequency representation of muscle activity and its application to onset detection. J Biomech. 2015;48:1193–7.
Silva MB, Silva AN, Naves EL, Palomari ET, Soares AB. An improved approach for measuring the tonic stretch reflex response of spastic muscles. Comput Biol Med. 2017;80:166–74.
Swie YW, Sakamoto K, Shimizu Y. Chaotic analysis of electromyography signal at low back and lower limb muscles during forward bending posture. Electromyogr Clin Neurophysiol. 2005;45:329–42.
Barnum H, Barrett J, Clark LO, Leifer M, Spekkens R, Stepanik N, Wilce A, Wilke R. Entropy and information causality in general probabilistic theories. New J Phys. 2010;12:1–32.
Huang NE, Zheng S, Long SR, Wu MC, Shih HH, Zheng Q, Yen NC, Tung CC, Liu HH. The empirical mode decomposition and the Hilbert spectrum for non-linear and non-stationary time series analysis. Proc R Soc Lond A. 1998;454:903–95.
Fu K, Qu J, Chai Y, Zou T. Hilbert marginal spectrum analysis for automatic seizure detection in EEG signals. Biomed Signal Proces. 2015;18:179–85.
Trompetto C, Marinelli L, Mori L, Pelosin E, Currà A, Molfetta L, Abbruzzese G. Pathophysiology of spasticity: implications for neurorehabilitation. Biomed Res Int. 2014. https://doi.org/10.1155/2014/354906.
Edgerton VR, Roy RR. Spasticity: a switch from inhibition to excitation. Nat Med. 2010;16:270–1.
Bogey RA, Barnes LA, Perry J. Computer algorithms to characterize individual subject EMG profiles during gait. Arch Phys Med Rehabil. 1992;73:835–41.
Zhu W, Zheng G, Gu Y, Chen X, Jin Y, Zhang G, Huang J, Shen J. Clinical efficacy and sEMG analysis of a new traditional Chinese medicine therapy in the treatment of spasticity following apoplectic hemiparalysis. Acta Neurol Belg. 2014;114:125–9.
Luo ZZ, Wang RC. Hand movement pattern recognition based on surface electromyography. Chin J Sci Instrum. 2006;27:996–9.
Fagerland MW, Hosmer DW. Tests for goodness of fit in ordinal logistic regression models. J Stat Comput Sim. 2016;86:1–21.
Shrout P, Fleiss J. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19:231–40.
Burridge JH, Wood DE, Hermens HJ, Voerman GE, Johnson GR, van Wijck F, Platz T, Gregoric M, Hitchcock R, Pandyan AD. Theoretical and methodological considerations in the measurement of spasticity. Disabil Rehabil. 2005;27:69–80.
Bohannon RW, Smith MB. Interrater reliability of a Modified Ashworth Scale of muscle spasticity. Phys Ther. 1987;67:206–7.
Watkins CL, Leathley MJ, Gregson JM, Moore AP, Smith TL, Sharma AK. Prevalence of spasticity post stroke. Clin Rehabil. 2002;16:515–22.
Johnson GR. Outcome measures of spasticity. Eur J Neurol. 2002;9:10–6.
McCrea PH, Eng JJ, Hodgson AJ. Linear spring-damper model of the hypertonic elbow: reliability and validity. J Neurosci Methods. 2003;128:121–8.
Zhang X, Zhou P. Sample entropy analysis of surface EMG for improved muscle activity onset detection against spurious background spikes. J Electromyogr Kinesiol. 2012;22:901–7.
Alcaraz R, Rieta JJ. A review on sample entropy applications for the non-invasive analysis of atrial fibrillation electrocardiograms. Biomed Signal Proces. 2010;5:1–14.
Rankin G, Stokes M. Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clin Rehabil. 1998;12:187–99.
Damiano DL, Quinlivan JM, Owen BF, Payne P, Nelson KC, Abel MF. What does the Ashworth scale really measure and are instrumented measures more valid and precise? Dev Med Child Neurol. 2002;44:112–8.
Ewoldt JK, Lazzaro EC, Roth EJ, Suresh NL. Quantification of a single score (1+) in the Modified Ashworth Scale (MAS), a clinical assessment of spasticity. In: Proceedings of the 38th annual international conference of the IEEE engineering in medicine and biology society (EMBC), August 16–20, Orlando. 2016. p. 1737–40. https://doi.org/10.1109/EMBC.2016.7591052.
Authors’ contributions
HBH and ZXF implemented the algorithm, analyzed the data and interpreted the results. HBH wrote the first draft of the manuscript. HBH and WY designed the study and performed all stages of the study including data collection, analysis, interpretation, and substantial revision of the manuscript. MJS performed the experiments of spasticity assessment. MJS and WM gave valuable comments about rehabilitation medicine. All authors read and approved the final manuscript.
Acknowledgements
The authors are very grateful to the participants and staff who participated in this project.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Consent for publication of individual data has been obtained from all the participants of the study.
Data availability statements
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request, without breaching participant confidentiality.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Anhui Provincial Hospital (Approval Number: 2015-Ethical Approval-08) and all the participants gave their informed consent.
Funding
This work is supported in part by the National Natural Science Foundations of China (Nos. 41076061 and 51279044) and in part by the Wuhu Municipal Science and Technology Project (2015cy04).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hu, B., Zhang, X., Mu, J. et al. Spasticity assessment based on the Hilbert–Huang transform marginal spectrum entropy and the root mean square of surface electromyography signals: a preliminary study. BioMed Eng OnLine 17, 27 (2018). https://doi.org/10.1186/s12938-018-0460-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12938-018-0460-1