Abstract
Although capnography is a standard tool in mechanically ventilated adult and pediatric patients, it has physiological and technical limitations in neonates. Gas exchange differs between small and adult lungs due to the greater impact of small airways on gas exchange, the higher impact of the apparatus dead space on measurements due to lower tidal volume and the occurrence of air leaks in intubated patients. The high respiratory rate and low tidal volume in newborns, especially those with stiff lungs, require main-stream sensors with fast response times and minimal dead-space or low suction flow when using side-stream measurements. If these technical requirements are not fulfilled, the measured end-tidal CO2 (P et CO 2 ), which should reflect the alveolar CO2 and the calculated airway dead spaces, can be misleading. The aim of this survey is to highlight the current limitations of capnography in very young patients to avoid pitfalls associated with the interpretation of capnographic parameters, and to describe further developments.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Acute respiratory disorders in newborns are an important clinical problem, especially in preterm infants [1]. Premature birth interrupts normal in utero lung development, resulting in significant alterations in postnatal lung function with consequences in later life [2, 3]. Clinical interest in postnatal lung function measurements at the end of the 19th century resulted in the development of special mechanical spirometers (Fig. 1) to measure tidal volume (V T ), respiratory rate (RR) and minute ventilation (V’ E ) [4, 5]. These mechanical measuring systems, however, have limitations in newborns, the most important being the high ratio of apparatus dead space (V Dapp ) to tidal volume (V T ), resulting in CO2-rebreathing and a risk of hypercapnia.
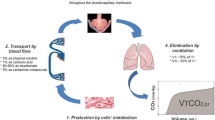
Comprehensive investigations of postnatal lung function, providing insights into neonatal respiratory physiology and pathophysiology, were first performed in the 1950s, after the development of electronic devices suitable for measuring and recording small and fast respiratory signals [6–8]. Besides measuring ventilation, respiratory mechanics and lung volume, the non-invasive measurements of the exhaled carbon dioxide (CO2) was at the beginning in the focus of the pulmonary researcher because its crucial role for the assessment of the alveolar gas exchanges and airway dead spaces (V D ). The measured CO2-signal can be recorded as a function of time (time-based capnography, mostly used for monitoring purposes) or volume (volumetric capnography), which allows calculations of alveolar ventilation (V’A) and airway dead spaces.
Since the 1960s different types of commercial capnographs have been developed for continuous CO2 measurements in adults, and these devices have been adapted for measurements in neonates [9, 10]. The first capnographs were bulky and cumbersome to use, especially when coupled to mass spectrometry [11]. During this time, a new generation of capnographs was developed for measurements in infants, with these instruments resolving many problems associated with earlier capnographs. Lightweight infrared (IR) mainstream sensors with a dead space <1 mL enabled reliable measurements even in preterm infants [12–14]. In addition, special low-flow sidestream capnographs were developed for dead space free measurements in neonates, making long-term monitoring possible [15–17]. Several clinical studies have shown the clinical benefit of the time-based capnography in ventilated infants and children, e.g., for non-invasive monitoring of the arterial pCO2 [18–20], to verify endotracheal tube placement [21–23], and to monitor the integrity of the ventilator circuit including disconnection and accidental extubation [24–26]. In spontaneously breathing infants time-based and volumetric capnography has been used for assessment of functional lung alterations related to bronchopulmonary dysplasia (BPD) [27–29]. Nevertheless the clinical use of capnography in newborns with the equipment available today still has methodological and technical problems which limits its wide adoption as a routine tool in the neonatal intensive care. This survey highlights the current limitations of capnography in these very young patients to avoid pitfalls associated with the interpretation of capnographic parameters which can lead to false clinical decisions, and to describe further developments.
Peculiarities of capnography in small lungs
The lungs and breathing patterns of neonates differ in many respects from those in adults. These differences may alter CO2 measurements as well as the interpretation of time-based and volumetric capnograms and derived parameters [30, 31]. Furthermore, the impact of the patient interface on CO2 measurements in breathed air and on the homogeneity of the alveolar ventilation [32] is much higher in neonates than in adults, as neonates have a much higher ratio of V Dapp to tidal volume [12, 33]. Thus, difficulties in capnographic measurements are greater in smaller infants.
Ventilatory parameters
The measured ranges of the CO2 fraction (FCO 2 ) and the corresponding partial pressure (PCO 2 ) in exhaled air are identical in neonates and adults. However, CO2 production is much lower in neonates (about 15 mL/min) than in adults (about 200 mL/min), and is even lower (9 mL/min) in very low birth weight (VLBW) infants, defined as those with a birth weight <1500 g [34]. The much lower amount of exhaled CO2 makes capnography in neonates more difficult, because there are objective limits in reducing the size of the analyzer chamber to realize fast filling when using a mainstream sensor or in reducing the magnitude of suction flow by side-stream measurements.
The ratio of tidal volume to body weight of a term infant is about 7 mL/kg, nearly the same as in adults. This ratio is slightly lower in preterm infants, 5–6 mL/kg. VLBW infants are at higher risk of having respiratory diseases and needing mechanical respiratory support and may have tidal volumes <10 mL. This low tidal volume limits the accuracy of capnographic measurements in these infants, given that the V Dapp of current mainstream gas analyzers is about 1 mL. Another limitation is the high respiratory rate in these infants. Adults have a breathing rate of 10–12/min, term newborns of 40–45/min and preterm newborns of 55–60/min. Furthermore, preterm infants with respiratory deficiency can have a respiratory rates >60/min with exhalation times of <500 ms [35, 36]. Energetically, this is an optimal breathing strategy for infants with stiff lungs, as it reduces the work of breathing [37]. However, this breathing strategy results in a technical challenge in capnographic measurements using currently available equipment.
Small airways
Both the lungs and airways grow in volume from infancy to adulthood [38], with the upper airways contributing significantly to anatomic dead space visible in volumetric capnograms. Measurements on volumetric capnography can be divided into three phases, as shown in Fig. 2. Phase I represents the CO2 free interval due to anatomic and apparatus dead space; phase II is characterized by a rapid increase in CO2 and represents the transition between airway gas and alveolar gas; and phase III reflects alveolar gas at the alveolar plateau, which is terminated by the most-well known capnographic parameter, the end-tidal CO2 (P et CO 2 ) which is commonly lower than the arterial PCO2 (P a CO 2 ) due to the alveolar dead space ventilation as shown in Fig. 3. In healthy adult lungs, CO2 concentration rapidly increases during phase II because the upper airways contribute negligibly to gas exchange and sophisticated techniques were developed to evaluate and classify time-based and volumetric capnograms [39, 40]. In neonates, airway diameters are much smaller and the ratios of inner surface area and volume per unit length are much higher than in adults, resulting in gas exchange between gas and tissue in the airways. This may result in an exaggerated and not well defined phase II and a reduced or even missing phase III in neonates which hampers the quantitative evaluation. Using volumetric capnography Ream et al. [41] found an inverse relationship between the slope of the alveolar plateau and infant size. Moreover, in a study by Fouzas et al. [5] phase III was found to be likely steeper in infants with than without BPD also due to airway obstruction that occurs in this disease process, suggesting that BPD likely induces a ventilation/perfusion mismatch in the lungs. Thus, in premature infants and infants with respiratory diseases, it is much more difficult to differentiate between phase II and III in the volumetric capnogram and to define an alveolar plateau. This result is supported by modeling studies by Schwardt et al. [42] and Neufeld et al. [43], which demonstrated an association between a morphometric reduction in airway cross-section and increased diffusional resistance within the airways, resulting in an increase in the slope of phase III. As phase III becomes steeper, it becomes more difficult to define an alveolar plateau. The nomenclature of the volumetric capnogram is also used for time-based capnograms, however, the interpretation is not equivalent. An alveolar plateau in a time based capnogram does not give any information if and how much alveolar CO2 was exhaled [31]. Nevertheless a missing or falsified alveolar plateau in the time-based and volumetric capnogram may indicate that the measured P et CO 2 does not reflect the alveolar CO2 pressure, making it problematic to use the measured P et CO 2 to monitor blood gases [44, 45]. Therefore, P et CO 2 measurements are only useful if the shape of the capnogram is considered. Automated measurements of P et CO 2 without monitoring the waveform should be used with caution, as the resulting data can be misleading.
Missing alveolar plateau
In newborns, volumetric capnograms without alveolar plateaus are not uncommon. A clinical study in spontaneously breathing preterm infants by Tirosh et al. [30] showed that the number of capnograms without alveolar plateaus increased significantly with decreasing gestational age. Proquittè et al. [31] investigated the effects of lung stiffness on the incidence of capnograms without alveolar plateaus in 21 ventilated newborn piglets (body weight 560–1435 g) before and after lung lavage with saline. They found that, in healthy lungs, 10 % of capnograms did not show an alveolar plateau, whereas the incidence in surfactant-depleted lungs was about 50 %. Furthermore, the incidence of capnograms without an alveolar plateau increased markedly as exhalation time decreased, with >75 % of capnograms lacking an alveolar plateau when exhalation times were <200 ms. Although the cause remains unclear, they likely result from both the technical limitations of the current technique (primarily, the overly long response time) and the physiological peculiarities of CO2 exchange in small stiff lungs.
Airway dead spaces
In adult lungs, only alveolar ventilation takes part in gas exchange with pulmonary capillary blood, while gas exchange in the physiologic dead space (V Dphys ) is negligible. V Dphys comprised the alveolar dead space (V Dalv ) of non-perfused or under-perfused alveoli, the anatomic dead space (V Dana ) of the conducting airways and the apparatus dead space (V Dapp ) of the face mask, pneumotach and mainstream gas analyzer. As early as the 1960s, Chu et al. [46] used in neonates a rapid capnograph to measure PetCO2 in exhaled air, with the anatomic and physiologic dead space calculated using the Bohr equation:
or the Bohr/Enghoff equation by substituting P a CO 2 for P et CO 2 :
where mean P mean CO 2 is the mean CO2 tension of the mixed expired air. The difference between these dead spaces represents the alveolar dead space:
The measured V Dana includes the dead space of the equipment. The Bohr and Bohr/Enghoff equations use only three measured parameters for dead space calculations, independent of the shape of the capnogram. Fletcher et al. [47] were the first who developed the calculation of different dead spaces from volumetric capnograms shown in Fig. 3. The three dead spaces can be calculated by ratios of the areas X, Y, and Z using Fowler’s classic ‘equal area’ method (p = q) [48].
Fletcher’s method requires a clear subdivision of the capnogram into phases I, II and III. It is, therefore, often difficult to apply this method to measurements in small lungs, in which phases II and III are not well defined. This method was inapplicable in the absence of an alveolar plateau. A clinical study of ventilated infants with a median birth weight of 2658 g showed that Fletcher’s method failed in 67 %, especially in preterm infants, whereas the Bohr/Enghoff equations could be used in all [12]. Therefore, in small infants the Bohr/Enghoff equation has been preferentially used to calculate dead space [44, 49, 50]. However, this advantage may be deceptive, because the extent to which phase III steepness or a missing alveolar plateau leads to errors in calculating dead space has not been determined. The more a capnogram differs from a step function, the more unreliable will be the dead-spaces calculated by Bohr/Enghoff equations.
Endotracheal tube leaks
The time-based capnography is widely used in both the intensive care unit (ICU) and during anesthesia to monitor gas exchange and the integrity of the ventilator circuit [51, 52]. In contrast to adults, newborns are frequently intubated with uncuffed endotracheal tubes (ET) to protect the airways and to avoid subglottic stenosis [53, 54]. Uncuffed ETs, however, have been associated with a risk of inadvertent air leaks [55], which occur in about 70 % of ventilated neonates [56]. In contrast to tidal volume measurements [57, 58], the effects of ET leaks on measurements of exhaled CO2 are much more complex [59]. At the end of expiration, when patient flow is zero, an ET leak can lead to reverse flow through the sample chamber, washing out the exhaled CO2 and resulting in a measured P et CO 2 close to zero. Leak-dependent CO2 measurement errors depend on the shape of the CO2 plateau in exhaled air [59]. As long as the CO2-plateau of exhaled air reaches the sample chamber before reverse flow starts, the peak CO2 will represent the P et CO 2 . Therefore, in contrast to volume measurements [58, 60], it is not possible to determine an upper limit of ET leaks that may be tolerated clinically for capnographic measurements. In mechanically ventilated preterm infants with low compliant, stiff lungs the frequently very short or absent CO2 plateaus may be notably falsified by the leak. If ET leakage occurs, capnographic measurements in these infants should be interpreted with caution, because of the uncertainty of P et CO 2 .
Technical limitations
Apparatus dead space
The apparatus dead space is of particular interest for capnographic measurements because it can lead to rebreathing of exhaled CO2, thereby generating false inspiratory and expiratory CO2 measurements. This was a significant problem using volumetric capnography with serial connections of the CO2 analyzer and pneumotach [61]. Combined sensors with a dead-space of about 1 ml have become available, e.g., neonatal sensor of the NM3, NICO, and CO2SMO+ respiratory monitors (all from Philips-Respironics, Murrysville, PA, USA). Nevertheless, the dead space problem remains, especially in preterm infants with low tidal volumes.
Dead space-free mainstream capnography remains a technical challenge, similar to that of dead space-free ventilatory measurements by the flow-through technique, in which the apparatus dead space is virtually eliminated by a background flow [62]. Evans et al. [63] performed capnographic measurements in 20 one-day old newborns using a bias flow of 3 L/min to wash-out the apparatus dead space of the face mask [63]. However, the bias flow diluted the CO2 concentration of the analyzed breathed gas, causing a loss in the precision of CO2 measurements, depending on the resolution of the capnograph.
Response time
Because the respiratory rate is about 4–5 times higher in neonates than in adults, a capnograph should have a shorter response time in neonates than in adults. The response time of the capnograph, however, must be sufficiently short, so that the magnitude and shape of the CO2 signal pattern are as accurate as possible. The response time of a capnograph has two components, the transit time and the rise time [64]. In sidestream measurements, the transit time is the time taken by the gas sample to travel from the sample port to the CO2 analyzer. This time depends on the suction flow and the length and diameter of the tube, with a numerical correction of the time lag being only approximate. The rise time is the time taken by the CO2 analyzer to increase from 10 to 90 % of the final value. Capnographs used in neonates currently have rise times (T 10–90 % ) of 50–80 ms, depending on the airflow used for testing. This time may be too long for preterm neonates with low expiratory air flow and expiratory times <500 ms. Unfortunately, signal filtering has marginal effects on improving rise times, with improvements limited by the rapid reduction in signal-to-noise ratio [65].
The effects of increased rise time on time-based and volume-based capnograms are shown in Fig. 4. A CO2-signal of a ventilated newborn with a short exhalation time was low pass filtered to simulate an increase in the rise time of the analyzer. The time constant of 36 ms is equivalent to a T10–90 % of 80 ms. Although the errors in P et CO 2 are relatively small, low pass filtering shifts the volumetric capnogram to the right, resulting in overestimates of calculated dead spaces which can lead to misleading clinical interpretations [66]. Thus, dead space measurements in neonates with short exhalation times are much more sensitive to the rise time of the CO2-analyzer than P et CO 2 measurements. Therefore, the results of older studies in newborns, using capnographs developed for adults with much higher rise times, should be interpreted with caution.
Ultrasonic flowmeters that simultaneously measure air flow and the molar mass of breathed gas [67] have very short response times, with no time delays between the two signals (Fig. 5). Although theoretically well suited to dead space measurements, molar mass is a surrogate signal, making it difficult to separate the CO2 signal [68]. Neumann et al. [69] used an ultrasonic flowmeter with an additional V Dapp of 1.1 mL (Exhalyzer D, Ecomedics, Dürnten, Switzerland) for capnographic measurements in mechanically ventilated preterm infants. However the weight and size of currently available ultrasound flow sensors are still too large for widespread clinical use in ventilated neonates.
Sampling rate
In the past capnographs developed for adults have often been shown inappropriate for measurements in neonates. Besides the high suction flow when using sidestream measurements, the long rise time and the large volume of the analyzer chamber, the sampling rates of analogue-to-digital (A/D) converters were often too low for fast respiratory signals [66, 70, 71]. Furthermore, it is crucial that the analogue flow and CO2 signals pass through anti-aliasing filters prior to sampling, in order to satisfy the Shannon sampling theorem and to avoid the potentially insidious problems of aliasing. This requires the specification of appropriate frequency cut-offs, which may differ between adults and newborns [72].
Beside the frequency cut-offs of the anti-aliasing filter the necessary sampling rate depends also on the frequency content of the signals. For acquisition of tidal breathing data, particularly in rapidly breathing infants with low respiratory time constants sampling rates of ≥200 Hz are recommended [72]. The frequency content of the CO2 signal depends on the rise time of CO2 sensor and is still unknown for infants with low respiratory time constant. The rise time of the current infrared CO2 sensors is likely too high to measure correctly the dynamic of CO2 signals in stiff lungs with exhalation times <200 ms (Fig. 4). A sampling rate of 100 Hz has been shown to be normally adequate in mature infants when calculating only V T , P et CO 2 and airway dead spaces by the Bohr/Enghoff equations. Greater time resolution may be required in rapidly breathing infants or intubated infants with stiff lungs, provided that faster CO2 analyzer are available. Furthermore, in contrast to time-based capnograms, the distances between sampling points in volumetric capnograms are not equidistant, reducing the ability to cleanly distinguish among phases I, II, and III of volumetric capnograms. A sufficiently high digital resolution is also necessary for graphical displays of time- and volumetric capnograms, because visual assessment of a capnogram is essential for valid interpretation of capnogram-derived parameters and for calculating interactive dead space by Fletchers method [61].
Further technical developments
The smaller tidal volumes and higher respiratory rates encountered in neonates, compared with those in older infants and adults, result in higher demands on capnograph use in neonates and require further developments [73]:
-
Minimizing the dead-space of main-stream sensors because of low tidal volume,
-
Reducing suction flow of side-stream monitors because of low breathing flow,
-
Reducing the response time of the CO2 analyzer because of the short exhalation times, especially in preterm neonates with stiff lungs,
-
Increasing the sample rate to provide sufficient numerical and graphic resolution of the capnogram, especially in infants with high respiratory rates, and
-
Minimizing the phase shift between CO2 and flow signals to prevent errors in dead space calculations.
Capnography for ventilated neonates will not be widely accepted by neonatologists as long as capnography is not integrated into the neonatal ventilator without increasing of V Dapp by the CO2-analyzer. This requires from the ventilator manufacturers to develop new combined sensors for air flow and CO2 measurements.
Conclusion
Capnography is a fascinating, noninvasive method for collecting information about breathing, alveolar gas exchange and airway dead spaces. In mechanically ventilated infants it is useful for monitoring the integrity of the ventilator circuit for early detection of mishaps, such as accidental tracheal extubation and disconnection of the breathing circuit, before irreversible damage is caused by prolonged hypoxia. Capnography, however, has physiological and technical limitations in neonatal patients, especially in newborns with stiff lungs. The short exhalation times, low tidal volumes and high impact of apparatus dead space hamper its measurements. Dead space calculations developed for adult lungs are often inapplicable to neonates with a prolonged phase II and a reduced or absent phase III. Imaginative physiological concepts are needed to interpret capnograms in these patients.
Despite technological progress, there are still technical limitations in correctly measuring the fast CO2 signals of neonates. These patients require need faster CO2 sensors and low suction flow for side stream measurements. Moreover, when using volumetric capnography, the pneumotach should be integrated with the CO2 sensors to reduce apparatus dead space. Finally, the widespread acceptance of capnography for neonates requires new, well designed bench, animal, and clinical studies to demonstrate its clinical value and various diagnostic possibilities in these patients.
Abbreviations
- A/D:
-
analogue-to-digital
- BPD:
-
bronchopulmonary dysplasia
- ET:
-
endotracheal tube
- FCO 2 :
-
CO2 fraction
- P et CO 2 :
-
end-tidal CO2 partial pressure
- RR :
-
respiratory rate
- T 10–90 % :
-
sensor rise time
- V’(t) :
-
air flow signal
- V(t) :
-
volume signal
- V’ A :
-
alveolar ventilation
- V’E :
-
minute ventilation
- V D :
-
dead space
- V Dalv :
-
alveolar dead space
- V Dana :
-
anatomic dead space
- V Dapp :
-
apparatus dead space
- V Dphys :
-
physiologic dead space
- V T :
-
tidal volume
- VLBW:
-
very low birth weight
References
Altman M, Vanpee M, Cnattingius S, Norman M. Risk factors for acute respiratory morbidity in moderately preterm infants. Paediatr Perinat Epidemiol. 2013;27:172–81.
Fawke J, Lum S, Kirkby J, Hennessy E, Marlow N, Rowell V, et al. Lung function and respiratory symptoms at 11 years in children born extremely preterm: the EPICure study. Am J Respir Crit Care Med. 2010;182:237–45.
Hoo AF, Gupta A, Lum S, Costeloe KL, Huertas-Ceballos A, Marlow N, et al. Impact of ethnicity and extreme prematurity on infant pulmonary function. Pediatr Pulmonol. 2014;49:679–87.
Eckerlein K. Zur Kenntnis des Athmungsmechanismus der Neugeborenen. Z für Geburtshülfe u Gynäkologie. 1890;29:120–73.
Dohrn R. Ueber die Grösse des respiratorischen Luftwechsels in den ersten Lebenstagen. Z für Geburtshülfe u Gynäkologie. 1895;32:25–59.
Karlberg P, Cook CD, O’Brien D, Cherry RB, Smith CA. Studies of respiratory physiology in newborn infants. II. Observations during and after respiratory distress. Acta Paediatr. 1954;43:387–411.
Cook CD, Cherry RB, O’Brien D, Karlberg P, Smith CA. Studies of respiratory physiology in the newborn infant. Observations on normal and full-term infants. J Clin Invest. 1955;34:975–82.
Cook CD, Sutherland JM, Segal S, Cherry RB, Mead J, McIlroy MB, et al. Studies of respiratory physiology in the newborn infant. III. Measurements of mechanics of respiration. J Clin Invest. 1957;36:440–8.
Muranyi L, Osvath P, Uhl K, Osvath P. Continuous registration of the CO2 contents in expired air (capnography) in the inhalative provocation of children. I. Acetylcholine provocation of asthmatic school-age children. Acta Paediatr Acad Sci Hung. 1969;10:133–54.
Steward DJ. Dr M Digby Leigh: his early studies of capnography and their practical application in pediatric cardiac anesthesia. Paediatr Anaesth. 2014;24:214–6.
Meny RG, Bhat AM, Aranas E. Mass spectrometer monitoring of expired carbon dioxide in critically ill neonates. Crit Care Med. 1985;13:1064–6.
Wenzel U, Wauer RR, Schmalisch G. Comparison of different methods for dead space measurements in ventilated newborns using CO2-volume plot. Intensive Care Med. 1999;25:705–13.
Wu CH, Chou HC, Hsieh WS, Chen WK, Huang PY, Tsao PN. Good estimation of arterial carbon dioxide by end-tidal carbon dioxide monitoring in the neonatal intensive care unit. Pediatr Pulmonol. 2003;35:292–5.
Amuchou SS, Singhal N. Dose end-tidal carbon dioxide measurement correlate with arterial carbon dioxide in extremely low birth weight infants in the first week of life? Indian Pediatr. 2006;43:20–5.
Hagerty JJ, Kleinman ME, Zurakowski D, Lyons AC, Krauss B. Accuracy of a new low-flow sidestream capnography technology in newborns: a pilot study. J Perinatol. 2002;22:219–25.
Lopez E, Grabar S, Barbier A, Krauss B, Jarreau PH, Moriette G. Detection of carbon dioxide thresholds using low-flow sidestream capnography in ventilated preterm infants. Intensive Care Med. 2009;35:1942–9.
Kugelman A, Golan A, Riskin A, Shoris I, Ronen M, Qumqam N, et al. Impact of continuous capnography in ventilated neonates: a randomized, multicenter study. J Pediatr. 2016;168:56–61.
McSwain SD, Hamel DS, Smith PB, Gentile MA, Srinivasan S, Meliones JN, et al. End-tidal and arterial carbon dioxide measurements correlate across all levels of physiologic dead space. Respir Care. 2010;55:288–93.
Coates BM, Chaize R, Goodman DM, Rozenfeld RA. Performance of capnometry in non-intubated infants in the pediatric intensive care unit. BMC Pediatr. 2014;14:163.
Kugelman A, Zeiger-Aginsky D, Bader D, Shoris I, Riskin A. A novel method of distal end-tidal CO2 capnography in intubated infants: comparison with arterial CO2 and with proximal mainstream end-tidal CO2. Pediatrics. 2008;122:e1219–24.
Bhende MS, Thompson AE, Cook DR, Saville AL. Validity of a disposable end-tidal CO2 detector in verifying endotracheal tube placement in infants and children. Ann Emerg Med. 1992;21:142–5.
Knapp S, Kofler J, Stoiser B, Thalhammer F, Burgmann H, Posch M, et al. The assessment of four different methods to verify tracheal tube placement in the critical care setting. Anesth Analg. 1999;88:766–70.
Salthe J, Kristiansen SM, Sollid S, Oglaend B, Soreide E. Capnography rapidly confirmed correct endotracheal tube placement during resuscitation of extremely low birthweight babies (<1000 g). Acta Anaesthesiol Scand. 2006;50:1033–6.
Cote CJ, Liu LM, Szyfelbein SK, Firestone S, Goudsouzian NG, Welch JP, et al. Intraoperative events diagnosed by expired carbon dioxide monitoring in children. Can Anaesth Soc J. 1986;33:315–20.
Cheifetz IM, Myers TR. Respiratory therapies in the critical care setting. Should every mechanically ventilated patient be monitored with capnography from intubation to extubation? Respir Care. 2007;52:423–38.
Bhende MS. End-tidal carbon dioxide monitoring in pediatrics—clinical applications. J Postgrad Med. 2001;47:215–8.
Lopez E, Mathlouthi J, Lescure S, Krauss B, Jarreau PH, Moriette G. Capnography in spontaneously breathing preterm infants with bronchopulmonary dysplasia. Pediatr Pulmonol. 2011;46:896–902.
Schmalisch G, Wilitzki S, Roehr CC, Proquitte H, Bührer C. Differential effects of immaturity and neonatal lung disease on the lung function of very low birth weight infants at 48-52 postconceptional weeks. Pediatr Pulmonol. 2013;48:1214–23.
Fouzas S, Hacki C, Latzin P, Proietti E, Schulzke S, Frey U, et al. Volumetric capnography in infants with bronchopulmonary dysplasia. J Pediatr. 2014;164:283–8.
Tirosh E, Bilker A, Bader D, Cohen A. Capnography in spontaneously breathing preterm and term infants. Clin Physiol. 2001;21:150–4.
Proquitte H, Krause S, Rudiger M, Wauer RR, Schmalisch G. Current limitations of volumetric capnography in surfactant-depleted small lungs. Pediatr Crit Care Med. 2004;5:75–80.
Schmalisch G, Wilitzki S, Buhrer C, Fischer HS. The lung clearance index in young infants: impact of tidal volume and dead space. Physiol Meas. 2015;36:1601–13.
Numa AH, Newth CJ. Anatomic dead space in infants and children. J Appl Physiol. 1996;80:1485–9.
Kingdon CC, Mitchell F, Bodamer OA, Williams AF. Measurement of carbon dioxide production in very low birth weight babies. Arch Dis Child Fetal Neonatal Ed. 2000;83:F50–5.
Schmalisch G, Wilitzki S, Wauer RR. Differences in tidal breathing between infants with chronic lung diseases and healthy controls. BMC Pediatr. 2005;5:36.
Latzin P, Roth S, Thamrin C, Hutten GJ, Pramana I, Kuehni CE, et al. Lung volume, breathing pattern and ventilation inhomogeneity in preterm and term infants. PLoS ONE. 2009;4:e4635.
Schmalisch G, Wauer RR, Bohme B. Changes in pulmonary function in preterm infants recovering from RDS following early treatment with ambroxol: results of a randomized trial. Pediatr Pulmonol. 1999;27:104–12.
Menache MG, Hofmann W, Ashgarian B, Miller FJ. Airway geometry models of children’s lungs for use in dosimetry modeling. Inhal Toxicol. 2008;20:101–26.
Herry CL, Townsend D, Green GC, Bravi A, Seely AJ. Segmentation and classification of capnograms: application in respiratory variability analysis. Physiol Meas. 2014;35:2343–58.
Jaffe MB. Using the features of the time and volumetric capnogram for classification and prediction. J Clin Monit Comput. 2016. (Epub ahead of print).
Ream RS, Schreiner MS, Neff JD, McRae KM, Jawad AF, Scherer PW, et al. Volumetric capnography in children. Influence of growth on the alveolar plateau slope. Anesthesiology. 1995;82:64–73.
Schwardt JD, Gobran SR, Neufeld GR, Aukburg SJ, Scherer PW. Sensitivity of CO2 washout to changes in acinar structure in a single-path model of lung airways. Ann Biomed Eng. 1991;19:679–97.
Neufeld GR, Schwardt JD, Gobran SR, Baumgardner JE, Schreiner MS, Aukburg SJ, et al. Modelling steady state pulmonary elimination of He, SF6 and CO2: effect of morphometry. Respir Physiol. 1992;88:257–75.
Rozycki HJ, Sysyn GD, Marshall MK, Malloy R, Wiswell TE. Mainstream end-tidal carbon dioxide monitoring in the neonatal intensive care unit. Pediatrics. 1998;101:648–53.
Tobias JD, Meyer DJ. Noninvasive monitoring of carbon dioxide during respiratory failure in toddlers and infants: end-tidal versus transcutaneous carbon dioxide. Anesth Analg. 1997;85:55–8.
Chu J, Clements JA, Cotton EK, Klaus MH, Sweet AY, Tooley WH, et al. Neonatal pulmonary ischemia. I. Clinical and physiological studies. Pediatrics. 1967;40:709–82.
Fletcher R, Jonson B, Cumming G, Brew J. The concept of deadspace with special reference to the single breath test for carbon dioxide. Br J Anaesth. 1981;53:77–88.
Fowler WS, Cornish ERJ, Kety SS. Lung function studies. VIII. Analysis of alveolar ventilation by pulmonary N2 clearance curves. J Clin Invest. 1952;31:40–50.
Arnold JH, Bower LK, Thompson JE. Respiratory deadspace measurements in neonates with congenital diaphragmatic hernia. Crit Care Med. 1995;23:371–5.
Domsky M, Wilson RF, Heins J. Intraoperative end-tidal carbon dioxide values and derived calculations correlated with outcome: prognosis and capnography. Crit Care Med. 1995;23:1497–503.
Eipe N, Doherty DR. A review of pediatric capnography. J Clin Monit Comput. 2010;24:261–8.
Schmalisch G. Basic principles of respiratory function monitoring in ventilated newborns: a review. Paediatr Respir Rev. 2016. doi:10.1016/j.prrv.2016.01.004 (Epub ahead of print).
Sherman JM, Nelson H. Decreased incidence of subglottic stenosis using an “appropriate-sized” endotracheal tube in neonates. Pediatr Pulmonol. 1989;6:183–5.
Contencin P, Narcy P. Size of endotracheal tube and neonatal acquired subglottic stenosis. Study group for neonatology and pediatric emergencies in the Parisian area. Arch Otolaryngol Head Neck Surg. 1993;119:815–9.
Mahmoud RA, Proquitte H, Fawzy N, Buhrer C, Schmalisch G. Tracheal tube airleak in clinical practice and impact on tidal volume measurement in ventilated neonates. Pediatr Crit Care Med. 2011;12:197–202.
Bernstein G, Knodel E, Heldt GP. Airway leak size in neonates and autocycling of three flow-triggered ventilators. Crit Care Med. 1995;23:1739–44.
Herber-Jonat S, von Bismarck P, Freitag-Wolf S, Nikischin W. Limitation of measurements of expiratory tidal volume and expiratory compliance under conditions of endotracheal tube leaks. Pediatr Crit Care Med. 2008;9:69–75.
Mahmoud RA, Fischer HS, Proquitte H, Shalaby HM, Schmalisch G. Relationship between endotracheal tube leakage and under-reading of tidal volume in neonatal ventilators. Acta Paediatr. 2009;98:1116–22.
Schmalisch G, Al-Gaaf S, Proquitte H, Roehr CC. Effect of endotracheal tube leak on capnographic measurements in a ventilated neonatal lung model. Physiol Meas. 2012;33:1–11.
Main E, Castle R, Stocks J, James I, Hatch D. The influence of endotracheal tube leak on the assessment of respiratory function in ventilated children. Intensive Care Med. 2001;27:1788–97.
Wenzel U, Wauer RR, Wagner MH, Schmalisch G. In vitro and in vivo assessment of the Ventrak 1550/Capnogard 1265 for single breath carbon dioxide analysis in neonates. Br J Anaesth. 1999;83:503–10.
Schmalisch G, Foitzik B, Wauer RR, Stocks J. Effect of apparatus dead space on breathing parameters in newborns: “flow-through” versus conventional techniques. Eur Respir J. 2001;17:108–14.
Evans JM, Hogg MI, Rosen M. Correlation of alveolar PCO2 estimated by infra-red analysis and arterial PCO2 in the human neonate and the rabbit. Br J Anaesth. 1977;49:761–4.
Tang Y, Turner MJ, Baker AB. Effects of lung time constant, gas analyser delay and rise time on measurements of respiratory dead-space. Physiol Meas. 2005;26:1103–14.
Wong L, Hamilton R, Palayiwa E, Hahn C. A real-time algorithm to improve the response time of a clinical multigas analyser. J Clin Monit Comput. 1998;14:441–6.
Hubble CL, Gentile MA, Tripp DS, Craig DM, Meliones JN, Cheifetz IM. Deadspace to tidal volume ratio predicts successful extubation in infants and children. Crit Care Med. 2000;28:2034–40.
Buess C, Pietsch P, Guggenbuhl W, Koller EA. A pulsed diagonal-beam ultrasonic airflow meter. J Appl Physiol. 1986;61:1195–9.
Thamrin C, Latzin P, Sauteur L, Riedel T, Hall GL, Frey U. Deadspace estimation from CO2 versus molar mass measurements in infants. Pediatr Pulmonol. 2007;42:920–7.
Neumann RP, Pillow JJ, Thamrin C, Larcombe AN, Hall GL, Schulzke SM. Influence of gestational age on dead space and alveolar ventilation in preterm infants ventilated with volume guarantee. Neonatology. 2015;107:43–9.
Thibeault DW, Poblete E, Auld PA. Alevolar-arterial O2 and CO2 differences and their relation to lung volume in the newborn. Pediatrics. 1968;41:574–87.
Dumpit FM, Brady JP. A simple technique for measuring alveolar CO2 in infants. J Appl Physiol. 1978;45:648–50.
Bates JH, Schmalisch G, Filbrun D, Stocks J. Tidal breath analysis for infant pulmonary function testing. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. European Respiratory Society/American Thoracic Society. Eur Respir J. 2000;16:1180–92.
Schmalisch G. Time and volumetric capnography in the neonate. In: Gravenstein JS, Jaffe MB, Paulus DA, editors. Capnography, clinical aspects. Cambridge: Cambridge University Press; 2004. p. 81–100.
Acknowledgements
The author thanks Dr. Scott Butler of English Manager Science Editing, Sydney, Australia, for language revision.
Competing interests
The author declares that he has no competing interests. The author has no financial relationship with any commercial entity with an interest in the subject of this manuscript.
Availability of data and supporting materials
There are no additional data available.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Schmalisch, G. Current methodological and technical limitations of time and volumetric capnography in newborns. BioMed Eng OnLine 15, 104 (2016). https://doi.org/10.1186/s12938-016-0228-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12938-016-0228-4