Abstract
Background
Plasmodium vivax malaria is a major public health problem in India. Control of vivax malaria is challenging due to various factors including relapse which increase the burden significantly. There is no well studied marker to differentiate relapse from reinfection. This creates hindrance in search for anti-relapse medicines. The genomic study of minisatellite can help in characterization of relapse and new infection of vivax malaria.
Methods
Eighty-eight samples of P. vivax were collected from malaria clinic. All the 14 chromosomes of P. vivax were scanned for minisatellite marker by Tandem Repeat Finder software Version 4.07b. Minisatellite marker CH1T1M13779 from chromosome one was applied for genotyping in 88 samples of P. vivax including 2 recurrence cases.
Results
Whole genome of P. vivax was scanned and found to have one hundred minisatellite markers. CH1T1M13779 minisatellite marker from chromosome-1 was used for amplification in 88 samples of P. vivax. Of 66 amplified samples, 14 alleles were found with varied allele frequency. The base size of 280 (13.63 %) 320 bp (13.63 %) and 300 bp (16.66 %) showed the predominant allele in the P. vivax population. Genotyping of two paired samples (day 0 and day relapse) could demonstrate the presence of relapse and reinfection.
Conclusion
The CH1T1M13779 can be potential minisatellite marker which can be used to differentiate between relapse and new infection of P. vivax strain.
Similar content being viewed by others
Background
Malaria is a major global public health problem [1]. Plasmodium vivax is the most prevalent malaria parasite in Asia [2]. Relapsing nature of P. vivax poses a challenge for malaria elimination. Relapse rates of 5–40 % have been reported from India [3]. Relapses are known to occur at different time intervals, ranged from 1 month to 1 year. The long-term relapsing malaria has been reported from India [3–5]. It is difficult to differentiate relapse from reinfection and the existing methods have limitations.
Attempts have been made by using polymorphic markers and techniques for phylogenetic analyses in P. vivax like VNTR analysis [6], PCR–RFLP of msp3 [7, 8], msp1 [9, 10]. csp [9], pvrbp-2 [11], andgam-1 [12, 13]. Sequencing technique was also used for polymorphism analysis in genes of msp1 [14], msp-3α [15], msp-3β [16], msp5 [15, 17], dpb [18] and vama1 [19]. Microsatellite markers were used for polymorphism analysis by GeneMapper [4, 20, 21].
An attempt was made to evaluate the utility of a newly designed minisatellite marker for differentiating relapse from reinfection.
Methods
Sample collection
The blood samples from confirmed vivax malaria patients were collected by finger prick method aseptically from malaria clinic of National Institute of Malaria Research, New Delhi (Fig. 1). The diagnosis of malaria species was confirmed by microscopic method. Two to three drops of blood were also collected on 3 mm filter paper (Whatman International Ltd., Maidstone, UK) for DNA isolation. Altogether, 88 samples of P. vivax were collected. Patients were treated as per National Drug Policy of India [22]. Of 88 P. vivax cases, two reported back to malaria clinic after a lapse of nine and 11 months, while two patients from same family (father and son) reported on the same date. The ethics committee of National Institute of Malaria Research approved this study and written informed consent was obtained from the patients/guardians.
Identification of minisatellite markers
All the 14 chromosomes of P. vivax were downloaded from National Center for Biotechnology (NCBI) and chromosome wise scanning for minisatellite markers was performed by Tandem Repeat Finder (TRF) software Version 4.07b [23]. One hundred minisatellite markers were identified by applying the parameters like period size (8–20), copy number (10–20), percent matches (90–100) and percent indels (0–2). Thirteen minisatellite markers were identified in the chromosome number one, of which three minisatellite marker’s primer sets were synthesized. Of three minisatellite markers, one minisatellite CH1T1M13779 which showed highly polymorphic nature was applied for amplification of 242 bp in 88 samples of P. vivax.
DNA isolation and PCR amplification
The genomic DNA of P. vivax was extracted from the blood samples collected on the filter paper using QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany) as per manufacturer’s instructions. PCR amplification of CH1T1M13779 was carried out in the final volume of 25 µl reaction contained 1× Buffer (50 mM KCl, 10 mM Tris, pH 8.3) 1.5 mM MgCl2, 0.2 mM dNTPs, 10 pmol of each primer forward (F-5′-GCATCATAATGGGTAAAG-3′) and reverse (R-5′-TCTCAATCACTGCAACAA-3′), 0.2 µM of dNTPs, 0.75 U of Taq DNA polymerase and 2 µl of genomic DNA. The thermal cycler parameter: initial denaturation at 94 °C for 5 min followed by 45 cycles denaturation at 94 °C for 1 min, annealing at 46 °C for 1 min, extension at 72 °C for 1.30 min and final extension at 72 °C for 10 min. The amplified PCR products and control were resolved on 2 % of metaphore agarose gel. The gel was stained with ethidium bromide and visualised under the UV light.
Results
Genome scanning for minisatellite marker and validation in clinical samples of Plasmodium vivax
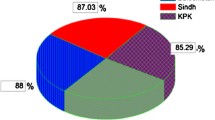
One hundred minisatellite markers were identified in the whole genome sequence of P. vivax. Of 88 samples, 66 were amplified and showed 14 alleles with varied allele frequency (Fig. 2). Period size 13 (AGCAAAGGTAGGC) and copy number 10.5 showed 14 alleles in the 66 samples. The allelic frequencies were 165 bp in 3.03 %, 170 bp in 1.51, 235 bp in 1.51, 240 bp in 10.60, 250 bp in 4.54, 260 bp in 10.60, 265 bp in 3.03, 280 bp in 13.63, 290 bp in 1.51, 300 bp in 16.66, 320 bp in 13.63, 340 bp in 1.51, 350 bp in 12.12 and 360 bp in 6.00 % of the P. vivax population (Fig. 3). The base size of 280 bp in 13.63 %, 320 bp in 13.63 % and 300 bp in 16.66 % showed the predominant allele in P. vivax population (Table 1).
Validation of minisatellite in case control study
Minisatellite marker CH1T1M13779 was used for case study in relapse, new infection and transmission pattern of P. vivax. Genotyping of two samples collected on day 0 and after 9 months from one patient from Dwarka region showed the identical genotype (Fig. 4, Lane 1 and 2). Both the samples from this patient showed same strain of P. vivax which caused the relapse after 9 months (Table 2).
Genotyping of another patient based on samples collected on day 0 and after a lapse of 11 months from Vijay Enclave showed two different genotypes (Fig. 4, Lane 3 and 4). Different genotype from same patient showed new infection due to different strain of P. vivax (Table 2). Genotyping of two patients from same family (father and son) who reported at the clinic on same day from Shahabad showed identical genotype (Fig. 4, Lane 5 and 6). The identical genotype of both the patients showed transmission of one P. vivax strain in the family (Table 2).
Discussion
The control and elimination of P. vivax is a major challenge due to the relapses. Relapses need to be differentiated from reinfection for knowing true efficacy of anti-relapse medicines during clinical trials. Current techniques to differentiate relapse from reinfections have limitations. The technique PCR–RFLP is used for allelic discrimination and polymorphism analysis in the genes such as Pvmsp3α, msp1 [24, 25], sequencing of microsatellite [4], capillary electrophoresis-based heteroduplex tracking assay [25, 26]. Recently, deep sequencing technique has been used for differentiation of relapse and reinfection [27].
These techniques are time consuming, expensive and need well established molecular laboratory. In the present study, whole genome of P. vivax was scanned and designed the simple, rapid, cost effective technique for differentiation of relapse and reinfection. The newly designed minisatellite marker CH1T1M13779 is highly polymorphic in nature and showed 14 alleles with varied allele frequency. The base size of 280 bp (13.63 %), 320 bp (13.63 %) and 300 bp (16.66 %) were predominant allele in P. vivax population.
The paired samples from one patient (day 0 and day recurrence at nine months) were analysed by minisatellite marker CH1T1M13779. Samples from another patient collected on day 0 and 11 months showed two different genotypes demonstrating that it was new infection due to different strain of P. vivax. Thus, this minisatellite marker could help to differentiate the relapse from new infection of P. vivax. Genotyping data of P. vivax by minisatellite marker supports the hypothesis of Kim et al. [10] and Koepfli et al. [28].
Genetic diversity of P. vivax has significant impact on malaria transmission [29]. The identical genotype of P. vivax in a father and son showed that transmission occurred due to same strain. Thus, the marker may also be helpful in identifying the origin and transmission of parasite in family or locality. Genotyping by the minisatellite marker can also help to differentiate P. vivax relapse from reinfection and thus help to determine efficacy of antirelapse medicines. This preliminary data shows that there is need to further strengthen data using more number of minisatellite markers in more paired P. vivax sample for statistical conclusions. This technique is rapid and cost effective as compared to the PCR–RFLP, sequencing, gene scanning and heteroduplex tracking assay.
Further, the study of polyclonal infections of P. vivax by the capillary electrophoresis-based heteroduplex tracking assay [25] and deep sequencing for detection of genetic signatures can generate important data that could be useful in developing antirelapse medicine trials.
Conclusion
Study provided preliminary evidence of identifying the relapse and new infection by newly designed minisatellite marker CH1T1M13779. Further studies are needed to validate the same.
References
WHO. Guidelines for the treatment of malaria, second edition. Geneva, World Health Organization, 2010. http://www.who.int/malaria/publication/atos/978941547925/enindex.html.
Hay SI, Guerra CA, Tatem AJ, Noor AM, Snow RW. The global distribution and population at risk of malaria: past, present and future. Lancet Infect Dis. 2004;4:327–36.
Adak T, Valecha N, Sharma VP. Plasmodium vivax polymorphism in a clinical drug trial. Clin Diagn Lab Immunol. 2001;8:891–4.
Imwong M, Snounou G, Pukrittayakamee S, Tanomsing N, Kim JR, Nandy A, et al. Relapses of Plasmodium vivax infection usually result from activation of heterologous hypnozoites. J Infect Dis. 2007;195:927–33.
Nicholas JW. Determinants of relapse periodicity in Plasmodium vivax malaria. Malar J. 2011;10(297):135. doi:10.1186/1475-2875-10-297.
Prajapati SK, Joshi M, Shalini S, Patarroyo MA, Suwanarusk R, Kumar A, et al. Plasmodium vivax lineages: geographical distribution, tandem repeat polymorphism, and phylogenetic relationship. Malar J. 2011;10:374.
Zakeri S, Barjesteh H, Djadid ND. Merozoite surface protein-3alpha is a reliable marker for population genetic analysis of Plasmodium vivax. Malar J. 2006;5:53.
Prajapati SK, Joshi H, Valecha N. Plasmodium vivax merozoite surface protein-3a: a high resolution marker for genetic diversity studies. J Vector Borne Dis. 2010;47:85–90.
Imwong M, Pukrittayakamee S, Grüner AC, Rénia L, Letourneur F, Looareesuwan S, et al. Practical PCR genotyping protocols for Plasmodium vivax using Pvcs and Pvmsp1. Malar J. 2005;4:20.
Kim JR, Imwong M, Nandy A, Chotivanich K, Nontprasert A, Tonomsing N, et al. Genetic diversity of Plasmodium vivax in Kolkata. India. Malar J. 2006;5:71.
Prajapati SK, Kumari P, Singh OP. Molecular analysis of reticulocyte binding protein-2 gene in Plasmodium vivax isolates from India. BMC Microbiol. 2012;12:243. doi:10.1186/1471-2180-12-243.
Imwong M, Pukrittakayamee S, Looareesuwan S, Poirriez J, Pasvol G, White NJ, et al. Plasmodium vivax: polymerase chain reaction amplification artifacts limit the suitability of pvgam1 as a genetic marker. Exp Parasitol. 2001;99:175–9.
Prajapati SK, Verma A, Adak T, Yadav RS, Kumar A, Eapen A, et al. Allelic dimorphism of Plasmodium vivax gam-1 in the Indian subcontinent. Malar J. 2006;5:90.
Putaporntip C, Jongwutiwes S, Sakihama N, Ferreira MU, Kho WG, Kaneoko A, et al. Mosaic organization and heterogeneity in frequency of allelic recombination of the Plasmodium vivax merozoite surface protein-1 locus. Proc Natl Acad Sci USA. 2002;99:16348–53.
Rayner JC, Huber CS, Feldman D, Ingravallo P, Galinski MR, Barnwell JW. Plasmodium vivax merozoite surface protein PvMSP-3 beta is radically polymorphic through mutation and large insertions and deletions. Infect Genet Evol. 2004;4:309–19.
Yang Z, Miao J, Huang Y, Li X, Putaporntip C, Jongwutiwes S, et al. Genetic structures of geographically distinct Plasmodium vivax populations assessed by PCR/RFLP analysis of the merozoite surface protein 3beta gene. Acta Trop. 2006;100:205–12.
Gomez A, Suarez CF, Martinez P, Saravia C, Patarroyo MA. High polymorphism in Plasmodium vivax merozoite surface protein-5 (MSP5). Parasitology. 2006;133:661–72.
Sousa TN, Ceravolo IP, Fernandes FCJ, Couto A, Carvalho LH, Brito CF. The pattern of major polymorphisms in the Duffy binding protein ligand domain among Plasmodium vivax isolates from the Brazilian Amazon area. Mol Biochem Parasitol. 2006;146:251–4.
Han ET, Park JH, Shin EH, Choi MH, Oh MD, Chai JY. Apical membrane antigen-1 (AMA-1) gene sequences of re-emerging Plasmodium vivax in South Korea. Korean J Parasitol. 2002;40:157–62.
Prajapati SK, Joshi H, Carlton JM, Rizvi MA. Neutral polymorphisms in putative housekeeping genes and tandem repeats unravels the population genetics and evolutionary history of Plasmodium vivax in India. PLoS Negl Trop Dis. 2013;7:e2425. doi:10.1371/journal.pntd.0002425.
McCollum AM, Valeria S, Salas CJ, Santolalla ML, Udhayakumar V, Escalante AA, et al. Genetic variation and recurrent parasitaemia in Peruvian Plasmodium vivax populations. Malar J. 2014;13:67.
NVBDCP: National drug policy on malaria, Ministry of Health and Family Welfare/Directorate of National Vector Borne Disease Control Programme, Govt. of India. 2010. http://www.nvbdcp.gov.in.
Benson G. Tandem repeats finder: a program to analyze DNA sequences. Nucleic Acids Res. 1999;27:573–80.
Lin JT, Juliano JJ, Kharabora O, Sem R, Lin FC, Muth S, et al. Individual Plasmodium vivax msp1 variants within polyclonal P. vivax infections display different propensities for relapse. J Clin Microbiol. 2012;50:1449–51.
Andrianaranjaka V, Lin JT, Golden C, Juliano JJ, Randrianarivelojosia M. Activation of minority-variant Plasmodium vivax hypnozoites following artesunate + amodiaquine treatment in a 23-year old manwith relapsing malaria in Antananarivo. Madagascar. Malar J. 2013;12:177.
Givens MB, Lin JT, Lon C, Gosi P, Char MC, Lanter CA, et al. Development of a capillary electrophoresis-cased heteroduplex tracking assay to measure in host genetic diversity of initial and recurrent Plasmodium vivax infections in Cambodia. J Clin Microbiol. 2014;52:298–301.
Lin JT, Hathaway NJ, Saunders DL, Lon C, Balasubramanian S, Kharabora O, et al. Using amplicon deep sequencing to detect genetic signatures of Plasmodium vivax relapse. J Infect Dis. 2015;212:999–1008. doi:10.1093/infdis/jiv142.
Koepfli C, Mueller I, Marfurt J, Goroti M, Sie A, et al. Evaluation of Plasmodium vivax genotyping markers for molecular monitoring in clinical trials. J Infect Dis. 2009;199:1074–80.
Cui L, Escalante AA, Imwong M, Snounou G. The genetic diversity of Plasmodium vivax populations. Trends Parasitol. 2003;19:220–6.
Author contributions
NV, RD designed the research, DS, RD collected the samples, RD performed experiment and analysed the results, RD, ARA, RCD wrote the paper. All authors were involved in edited the manuscript and approved the manuscript.
Acknowledgements
We would like to acknowledge Indian Council of Medical Research (ICMR), New Delhi, India for financial supports (No. ICMR/REC NO ECD/ad-hoc/38).
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Das, R., Dhiman, R.C., Savargaonkar, D. et al. Genotyping of Plasmodium vivax by minisatellite marker and its application in differentiating relapse and new infection. Malar J 15, 115 (2016). https://doi.org/10.1186/s12936-016-1139-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-016-1139-3