Abstract
Background
Drug resistance remains a major obstacle to malaria treatment and control. It can arise and spread rapidly, and vary substantially even at sub-national level. National malaria programmes require cost-effective and timely ways of characterizing drug-resistance at multiple sites within their countries.
Methods
An improved multiplexed post-PCR ligase detection reaction—fluorescent microsphere assay (LDR-FMA) was used to simultaneously determine the presence of mutations in chloroquine resistance transporter (crt), multidrug resistance 1 (mdr1), dihydrofolate reductase (dhfr) and dihydropteroate synthase (dhps) genes in Plasmodium falciparum (n = 727) and Plasmodium vivax (n = 574) isolates collected in 2006 from cross-sectional community population surveys in two geographically distinct regions (Madang and East Sepik) of Papua New Guinea (PNG) where strong regional differences in in vivo aminoquinoline and antifolate therapeutic efficacy had previously been observed. Data were compared to those of a follow-up survey conducted in 2010.
Results
Despite some very low parasite densities, the assay successfully amplified all P. falciparum and P. vivax loci in 77 and 69 % of samples, respectively. In 2006, prevalences of pfdhfr (59R-108 N) double mutation/wild type pfdhps haplotype, pfcrt SVMNT haplotype (72S-76T double mutation), and 86Y pfmdr1 mutation all exceeded 90 %. For P. vivax, 65 % carried at least two pvdhfr mutations, 97 % the 647P pvdhps mutation and 54 % the 976F pvmdr1 mutation. Prevalence of mutant haplotypes was higher in Madang than East Sepik for pfcrt SVMNT (97.4 vs 83.3 %, p = 0.001), pfdhfr (59R-108 N) (100 vs 90.6 %, p = 0.001), pvdhfr haplotypes (75.8 vs 47.6 %, p = 0.001) and pvmdr1 976F (71.2 vs 26.2 %, p < 0.001). Data from a subsequent Madang survey in 2010 showed that the prevalence of pfdhps mutations increased significantly from <5 % to >30 % (p < 0.001) as did the prevalence of pvdhfr mutant haplotypes (from 75.8 to 97.4 %, p = 0.012).
Conclusions
This LDR-FMA multiplex platform shows feasibility for low-cost, high-throughput, rapid characterization of a broad range of drug-resistance markers in low parasitaemia infections. Significant geographical differences in mutation prevalence correlate with previous genotyping surveys and in vivo trials and may reflect variable drug pressure and differences in health-care access in these two PNG populations.
Similar content being viewed by others
Background
Monitoring the emergence and spread of drug resistance is a key priority for malaria control and elimination efforts in the modern era [1]. The recent emergence of artemisinin resistance in South-east Asia demonstrates that drug resistance can spread rapidly across national borders and how its prevalence can vary substantially even within individual countries [2]. Effective containment strategies will require comprehensive, accurate, real-time estimates of drug resistance status from multiple sites that can identify the potential for treatment failure within small geographic regions.
In vivo evaluations of drug susceptibility are expensive and logistically challenging, requiring a substantial time-commitment from participants and appropriate clinical research infrastructure at each study site. Sample size constraints and the confounding effects of local transmission (risk of re-infection) during follow-up can compromise comparisons between different geographic locations. In vivo evaluations are, therefore, inappropriate for rapid and comprehensive comparisons of drug resistance between distinct sites within a single country or small geographic area.
The recent development of well-characterized molecular markers that correlate strongly with in vivo drug resistance has meant that there are now feasible alternative in vitro methods of characterizing population drug resistance. Resistance to sulfadoxine-pyrimethamine (SP) in Plasmodium falciparum is clearly linked to mutations in the dihydrofolate reductase (pfdhfr) and dihydropteroate synthase (pfdhps) genes with selection thought to occur as a step-wise process leading to highly resistant triple to quintuple mutant parasites [3]. There are orthologs of these genes in P. vivax [4–8], and pvdhfr mutations at codons 57, 58, 61, 117, 173 correlate with SP resistance [9, 10]. P. falciparum 4-aminoquinoline resistance correlates with mutations in pfcrt [11] and pfmdr1. However, the relationship between 4-aminoquinoline resistance and mutations in the P. vivax ortholog (pvmdr1) remains controversial [12–14] even though it seems that a codon 976 mutation is associated with AQ or CQ drug resistance in the Asia–Pacific region [13].
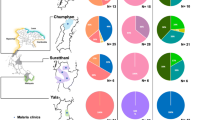
Of the four Plasmodium species present in Papua New Guinea (PNG), P. falciparum and P. vivax predominate [15, 16]. The prevalence of each species differs according to the geography of the country and among age groups [17]. This complex epidemiology makes malaria control in PNG very challenging. Early malaria control efforts in PNG included mass drug administration (MDA) in the 1950s and 1960s [18, 19]. Employed variably throughout the country, some areas received MDA with chloroquine, some with pyrimethamine and others no drug treatment at all [20]. Anti-malarial treatment policy for case management was chloroquine (CQ) for adults or amodiaquine (AQ) for young children until 2000 [21]. However, P. falciparum CQ resistance had started to emerge as early as the 1970s [22] and in vivo resistance rates as high as 47 % were documented in Madang Province by the early 1980s [20]. Resistance in P. vivax emerged much later, with the first well-documented CQ treatment failure described in 1989 [23, 24] and remained at 4.5 % in East Sepik by 2000 [25].
In 2000, PNG treatment policy was changed to incorporate SP as first-line therapy in combination with AQ or CQ. At around that time, P. falciparum PCR-corrected failure rates ranged from 18.2 to 28.6 % for CQ-SP and 10.3 to 21.5 % for AQ-SP in different regions [26]. For P. vivax, estimates of resistance to AQ/CQ-SP ranged from 0 to 7 % in the same provinces [26] whilst uncorrected treatment failure rates of 49 % (28 days) and 87 % (42 days) were documented in Madang and Sepik in 2005–2006 [27]. However, in contrast to P. falciparum, the absence of validated markers to distinguish recrudescence from reinfection have meant that in vivo comparisons of P. vivax therapeutic efficacy between sites with different malaria epidemiology are confounded by both new infections and hypnozoite relapses during follow-up, especially in areas of high transmission [28].
Following observations of heterogeneity of in vivo drug resistance in Madang and East Sepik provinces of PNG [26, 29], the utility of an established ligase detection reaction fluorescence microsphere assay (LDR-FMA) was investigated [29]. A novel primer set was multiplexed to characterize mutations associated with SP and 4-aminoquinoline resistance in both P. falciparum and P. vivax from cross-sectional population surveys conducted in these two provinces. The aim of the study was to demonstrate the feasibility of this high-throughput technology as a practical and cost-effective means of rapidly comparing susceptibility to multiple drugs at numerous geographic sites.
Methods
Study population and blood sample collection
Cross-sectional population-wide surveys were conducted in Maprik, East Sepik Province (2006) and Mugil, Madang Province (2006 and 2010). Following informed consent from adults or children’s guardians, 200 μL of whole blood was collected by fingerprick from participants of all ages. The study was approved by the Medical Research Advisory Committee (#05-20) of PNG and the PNG Institute of Medical Research Institutional Review Board (#06.01).
DNA extraction and molecular diagnosis of Plasmodium species infections
Genomic DNA was extracted from whole blood using the QIAamp 96 DNA blood kit (Qiagen, Valencia, CA) or the 96-well genomic DNA extraction kit (Favorgen, Taiwan) according to the manufacturer instructions. The presence of P. falciparum and P. vivax infections was determined by a post-PCR, ligation detection reaction—fluorescent microsphere assay (LDR-FMA: 2006 surveys) [30] and a qPCR assay (2010 survey) [31, 32].
Detection of mutations in Plasmodium falciparum dhfr, dhps and mdr1 genes
Detection of mutations in pfdhfr, pfdhps, pfmdr1 and pfcrt was achieved by LDR-FMA using an adaptation of the methods of Carnevale et al. [33] and Wong et al. [34]. New primers were designed in order to multiplex the PCR and perform nested PCR. Primer sequences are provided in Additional file 1: Table S1. All PCR-1 reactions were performed in a buffer containing 120 nM of each primer, 67 mM Tris–HCl (pH = 8.8), 6.7 mM MgSO4, 16.6 mM (NH4)2SO4, 10 mM mercaptoethanol, 200 µM (each) dATP, dGTP, dCTP, dTTP, and 2.5 U of thermostable DNA polymerase. Nested PCR-2 reactions were performed with 3 µL of PCR products from the PCR-1 reaction using the same conditions except for the primers (240 nM each). PCR amplification was performed under the following conditions: PCR-1—95 °C for 2 min and 30 cycles at 95 °C for 30 s, 52 °C for 30 s, 72 °C for 80 s, and a final extension at 72 °C for 5 min; PCR-2—95 °C for 2 min and 40 cycles at 95 °C for 30 s, 59 °C for 30 s, 72 °C for 1 min, and a final extension at 72 °C for 5 min. Amplification specificity was evaluated following electrophoresis on 2 % agarose gel. In order to integrate detection of mutations in pfmdr1, new LDR primers were designed (sequences provided in Additional file 2: Table S2). LDR-FMA was performed with 1 μL of PCR-2 product with cycling conditions and fluorescence signal interpretation as described previously [29, 35].
Because a high background signal for the wild type pfmdr 86 allele raised concerns regarding the LDR primer’s specificity in polyclonal infections, a PCR RFLP protocol was used to confirm LDR-FMA genotyping results. PCRs were performed using the same primer sets as the LDR-FMA. RFLP was achieved by mixing 5 μL of PCR products with 15 μL of a mix containing 1 U of ApoI restriction enzyme (New England Biolabs, USA), 1X NE buffer and 1X BSA. The digestion took place at 50 °C for 2 h. Digested products were visualized on 2 % agarose gel.
Detection of mutations in Plasmodium vivax dhfr, dhps and mdr1 genes
Detection of mutations in pvdhfr, pvdhps and pvmdr1 gene was achieved using a LDR-FMA as described previously [29]. Two LDR allele-specific primers were added to the 23 primers already used in the assay in order to integrate two pvdhfr alleles newly identified in PNG by sequencing (Additional file 2: Table S2). Fluorescence signals were interpreted as previously described [28, 35].
Statistics
Chi square and Fisher exact tests (Stata 12) were used to compare the frequency of P. falciparum and P. vivax infections and mutation prevalence between East Sepik and Madang populations.
Results
Study population and Plasmodium infections
As previously detailed [36], a total of 2359 samples, including 1282 (54.3 %) from Madang and 1077 (45.7 %) from East Sepik, were collected in 2006. Of these, 784 (61.1 %) samples from Madang and 416 (38.9 %) from East Sepik had PCR-detected Plasmodium spp (p < 0.001). Plasmodium falciparum was present in 487 (62.1 %) and 240 (57.7 %) (p = 0.14, NS) and P. vivax in 409 (52.2 %) and 165 (39.7 %) of infections (p < 0.001) from Madang and East Sepik, respectively. A further 88 P. falciparum and 89 P. vivax positive samples collected in a 2010 survey in Madang were also selected for drug resistance genotyping.
Drug resistance genotyping reveals geographic heterogeneity of parasite populations
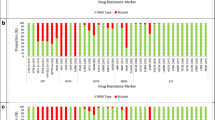
Plasmodium falciparum genotyping
Of 399 randomly-selected 2006 samples, genotyping was successfully performed on the four genes (pfdhfr, pfdhps, pfcrt and pfmdr1) in 307 (76.9. %). An additional 28 samples (7.1 %) yielded results for at least one of the four genes. Mutations in pfdhfr, pfdhps and pfmdr1 were detected individually except for codons 436–437 of pfdhps. Single gene and multigenic haplotypes were only determined in participants displaying a monoclonal infection as determined by the maximum number of alleles (n = 1) detected at pfdhfr, pfdhps, pfcrt and pfmdr1. Genotyping results are displayed in Table 1. Over 95 % of isolates displayed a double mutation at pfdhfr (59R-108N) and a wild type haplotype at pfdhps. A small number (7 samples: 4.8 %) had pfdhps mutations in addition to pfdhfr mutations, and thus carried triple or quadruple mutant pfdhfr/pfdhps haplotypes.
Most isolates (>90 %) displayed the pfcrt SVMNT haplotype (i.e. a double 72S-76T mutations) and a pfmdr1 single mutation (86Y). Only one East Sepik sample carried the triple mutation (74I-75E-76T) at pfcrt (CVIET haplotype). Despite the high overall frequency of pfcrt SVMNT and pfdhfr double mutant haplotypes, their prevalence was significantly higher in Madang than in East Sepik (Table 1: p = 0.001). These results were confirmed when looking at the prevalence of mutations in all samples (monoclonal and polyclonal infections). Wild-type pfdhfr alleles (codons 59 and 108) were more frequent in East Sepik than Madang (p < 0.001; Additional file 3: Table S3) as was wild-type CVMNK pfcrt haplotype (p < 0.001). However pfmdr1 mutations at codons 184 and 1042 were more often observed in East Sepik (p = 0.005 and p = 0.03). Both resistant CVIET and SVMNT alleles were found in East Sepik.
Plasmodium vivax genotyping
Genotyping was successfully performed on the three genes (pvdhfr, pvdhps and pvmdr1) in 398 (69.3 %) of 574 P. vivax LDR-FMA samples and at least one of the three genes in 483 (84.1 %). As described previously [29], mutations in pvdhfr, pvdhps and pvmdr1 were detected either individually (pvdhfr codons 117, 173; pvdhps codons 553, 647; pvmdr1 codon 976), or as a haplotype (pvdhfr codons 57-58-61; pvdhps codons 382–383). For this reason, while it was possible to affirm the presence of triple mutant isolates at pvdhfr codons 57-58-61, it was only possible to confirm the presence of quadruple mutant haplotypes (triple mutant at codons 57-58-61 plus mutant at codon 117) in participants with monoclonal infections. Genotyping results are displayed in Table 2.
Only 38 of 108 monoclonal isolates (35.2 %) displayed a wild type haplotype at pvdhfr with 26 (24.1 %) and 41 (38.0 %) displaying double and quadruple mutant haplotypes, respectively. The vast majority of the isolates (97.2 %) carried the 647P mutation in pvdhps and 58 (53.7 %) the 976F mutation in pvmdr1. The pvmdr1 976 mutation itself was highly significantly associated with the pvdfhr quadruple mutant haplotype (OR = 5.6; CI95 = [2.3;13.6], p < 0.001). The prevalence of mutant pvdhfr haplotypes was significantly higher in Madang than East Sepik (75.8 vs 47.6 %, p = 0.001), with prevalence of the quadruple mutant haplotype reaching 51.5 % in Madang vs 16.7 % in East Sepik. Similarly, pvmdr1 976F mutation prevalence was higher in Madang than East Sepik (71.2 vs 26.2 %, p < 0.001).
These results were confirmed when including all infections (monoclonal and polyclonal) (Additional file 4: Table S4). Two additional mutations were observed but at low frequency: pvdhfr codon 173 (I → L; 0.4 %) and pvdhps codon 647 (A → S; 0.2 %).
Selection of additional mutant genotypes under continuous drug pressure
Genotyping results of P. falciparum and P. vivax isolates collected in 2006 in Madang Province were compared with samples collected at the same site in 2010 (Tables 1, 2). As mutant pfdhfr and pfmdr1 genotypes had already nearly reached fixation in Madang in 2006, no significant change was observed in 2010. The prevalence of the pfcrt K76 wild type allele decreased from 13.6 to 1.2 % (p = 0.002, Additional file 3: Table S3). A dramatic increase in the prevalence of pfdhps mutations was observed. In 2010, 15.9 % of isolates carried a single mutation (437 G, vs 3.5 % in 2006, p = 0.004) and another 15.9 % a double mutation (437G/581G, vs 0 % in 2006, p < 0.001). For P. vivax, while the prevalence of mutant pvdhps and pvmdr1 haplotypes remained stable over time, a significant increase was observed for pvdhfr, (97.4 % in 2010 vs 75.8 % in 2006, p = 0.005).
Discussion
The present study shows that the highly multiplexed LDR-FMA platform performed well in characterizing multiple loci related to 4-aminoquinoline and antifolate drug resistance in both P. falciparum and P. vivax. Through its successful application in low parasite density infections (from cross-sectional population surveys of mostly asymptomatic individuals) and by generating results highly concordant with existing in vivo drug resistance data (reflecting both spatial and temporal differences in population drug resistance profiles), the LDR-FMA platform can be used for rapid, low-cost application at multiple field sites. This makes it an attractive tool for national malaria programmes that require comprehensive local level characterization of drug resistance patterns.
Existing LDR-FMA assays [33, 34] were significantly improved by using new PCR primers designed to allow visualization of the five amplified fragments of pfmdr1, pfcrt, pfdhfr and pfdhps on an agarose gel in a single multiplexed assay. Compared with previously published LDR-FMA protocols, the new assay requires much less total DNA, less technician time and has lower overall assay costs. Even though the assay was performed in samples from mostly asymptomatic individuals who a had much lower parasitaemia than previous studies utilizing samples from patients with symptomatic infections [34], it was only slightly less sensitive for P. vivax and equivalent for P. falciparum [29, 34]. Multiplexing the PCR in a nested PCR protocol did not, therefore, compromise assay performance significantly. A potential problem in the P. falciparum component of the assay related to high background signal for the wild type pfmdr 86 allele (that raised concerns regarding the LDR primer’s specificity in polyclonal infections) was addressed using a PCR RFLP protocol. The P. vivax assay was also improved by designing an allele specific primer targeting a new polymorphism in the pvdhfr codon 57.
The prevalence of the P. falciparum 4-aminoquinoline resistance mutations reported here is very similar to previously published data including a >80 % prevalence of pfmdr1 86Y in 2000–2005 [37–39] and 86–96 % prevalence of pfcrt 76T mutation in the early 2000s in East Sepik and Madang [33, 37–40]. The pfcrt 76T mutation is almost exclusively found as part of the double mutant haplotype SVMNT previously described in PNG and South America [41, 42]. While this mutation has been reaching levels near fixation (96 %) in symptomatic infections from children from the same geographical area (Mugil village, Madang Province) over the last 9 years [43], a similar prevalence is observed here in asymptomatic individuals of all ages.
A recent analysis by Nsanzabana et al. has suggested that strong selection of pfdhfr 59R 108N double mutant parasites occurred in East Sepik in the 3 years following the introduction of SP in the early 2000s, with a 2.5 times increase in double mutant prevalence to 60–70 % over this time [44]. This has progressed with levels approaching fixation in the 2006 surveys and other data from the same provinces in 2005–2007 [34]. By contrast, the frequency of pfdhps mutations remained very low in 2006 suggesting some retention of sulfadoxine activity. However, the emergence of significant rates of single and double mutant pfdhps in the 2010 data (combined prevalence of 31.8 %) suggests that a loss of SP efficacy may be imminent in Madang Province, thus threatening its potential value for intermittent preventive treatment in pregnancy and infants.
Despite the very high overall frequency of many mutations in the present study, at least four mutations (pfcrt, pfdhfr, pvdhfr haplotypes and the pvmdr1 976F) were significantly more prevalent in Madang compared with East Sepik, which is in accord with similar observations of differences in drug resistance mutations between the two areas [37]. One explanation for this phenomenon is that the Madang region has more functional health-care infrastructure and, therefore, its population has better access to anti-malarial drugs than the more remote populations of the East Sepik [44], resulting in a higher selection pressure. Distribution of drugs beyond their expiration date leading to sub optimal dosage could also have contributed to the selection of drug resistant parasites.
The significant differences in pvmdr1 976F mutation prevalence between the two provinces (72 vs 26 % in monoclonal infections) and similar differences observed for pvdhfr mutant genotypes accord well with the observations from in vivo studies of SP + CQ or AQ efficacy of P. vivax infections between 2003 and 2005 that demonstrated no treatment failure in East Sepik but 29 % treatment failures in Madang [26]. Overall, the quadruple pvdhfr genotype was identified in 38.5 % of the P. vivax monoclonal infections. This genotype, when found in combination with a mutation at pvmdr1 976, has previously been associated with AQ-SP treatment failure in a study conducted in PNG children [9]. Apart from the 647P mutation that seems to be fixed in the PNG P. vivax population, mutations in pvdhps were rarely found.
Plasmodium vivax is characterized by early production of gametocytes during its life cycle (prior to the first symptoms of malaria) so that transmission can occur prior to anti-malarial drug exposure, therefore delaying the selection of drug resistant isolates. However, in PNG, the high incidence of mixed P. falciparum/P. vivax infections may result in an early exposure of concurrent P. vivax infections to anti-malarial drugs at the time of treatment of symptomatic malaria caused by P. falciparum. Additionally, P. vivax polyclonal infections are very frequent with up to 75 % of all infected carrying several genotypes [45]. This leads to numerous opportunities for sexual recombination between parasite clones during the mosquito phase of the parasite life cycle and therefore production of meiotic recombinant parasites with drug resistant genotypes. Despite a lower P. vivax prevalence in East Sepik than in Madang, both parasite populations have shown similar levels of genetic diversity [36]. Therefore, as with observations of geographic differences in P. falciparum drug resistance mutants, the higher prevalence of pvmdr1 and pvdhfr mutants in the Madang P. vivax population may reflect greater drug pressure in the Madang area.
Like most malaria-endemic countries, PNG has now adopted WHO recommended artemisinin combination therapy (ACT) as the cornerstone of its anti-malarial case-management strategy. This change to ACT has already been associated with significant reductions in malaria prevalence elsewhere but the emergence and spread of artemisinin resistance in South-East Asia [2], and observations of variable response to partner drugs (such as lumefantrine) [46] suggest the need for ongoing surveillance of drug susceptibility to both components. Recent identification of an association of particular single nucleotide polymorphisms in the kelch-13 gene with artemisinin resistant phenotypes [47] may enable incorporation of markers of artemisinin resistance in combination with those evaluated in this study. As demonstrated here, the LDR-FMA platform is highly flexible and integration of new markers can easily be achieved.
It is also notable that lumefantrine exerts a selective pressure on pfmdr1 N86Y in an opposing direction to that of AQ and CQ [46, 48, 49]. Therefore, reversion to wild-type genotypes following uptake of artemether-lumefantrine may indicate diminishing parasite susceptibility to lumefantrine but may also raise the prospect of resurrecting AQ or CQ as effective treatments.
Conclusion
Significant geographical differences in mutation prevalence in the present study correlate with recent in vivo data obtained from the same regions and may reflect variable drug pressure due to differences in health-care access in the two PNG populations. The high-throughput capacity and relatively low cost of the LDR-FMA assay could make it a valuable tool for rapidly characterizing in a central laboratory the status of resistance to a range of anti-malarial drugs from sites that may not necessarily have the infrastructure required for conducting in vivo evaluations of drug efficacy. This can be achieved by National Malaria Control Programmes and partner organizations using isolates obtained through cross-sectional population sampling.
Abbreviations
- ACT:
-
artemisinin combination therapy
- AQ:
-
amodiaquine
- crt:
-
chloroquine resistance gene
- CQ:
-
chloroquine
- dhfr:
-
dihydrofolate reducatse gene
- dhps:
-
dihydropteroate synthase gene
- LDR-FMA:
-
ligase detection reaction—fluorescent microsphere assay
- MDA:
-
mass drug administration
- mdr1:
-
multidrug resistance 1 gene
- PNG:
-
Papua New Guinea
- SP:
-
sulfadoxine-pyrimethamine
References
Guerin PJ, Bates SJ, Sibley CH. Global resistance surveillance: ensuring antimalarial efficacy in the future. Curr Opin Infect Dis. 2009;22:593–600.
Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014;371:411–23.
Sibley CH, Hyde JE, Sims PF, Plowe CV, Kublin JG, Mberu EK, et al. Pyrimethamine-sulfadoxine resistance in Plasmodium falciparum: what next? Trends Parasitol. 2001;17:582–8.
Brega S, Meslin B, de Monbrison F, Severini C, Gradoni L, Udomsangpetch R, et al. Identification of the Plasmodium vivax mdr-like gene (pvmdr1) and analysis of single-nucleotide polymorphisms among isolates from different areas of endemicity. J Infect Dis. 2005;191:272–7.
de Pecoulas PE, Basco LK, Tahar R, Ouatas T, Mazabraud A. Analysis of the Plasmodium vivax dihydrofolate reductase-thymidylate synthase gene sequence. Gene. 1998;211:177–85.
de Pecoulas PE, Tahar R, Ouatas T, Mazabraud A, Basco LK. Sequence variations in the Plasmodium vivax dihydrofolate reductase-thymidylate synthase gene and their relationship with pyrimethamine resistance. Mol Biochem Parasitol. 1998;92:265–73.
Korsinczky M, Fischer K, Chen N, Baker J, Rieckmann K, Cheng Q. Sulfadoxine resistance in Plasmodium vivax is associated with a specific amino acid in dihydropteroate synthase at the putative sulfadoxine-binding site. Antimicrob Agents Chemother. 2004;48:2214–22.
Sa JM, Nomura T, Neves J, Baird JK, Wellems TE, del Portillo HA. Plasmodium vivax: allele variants of the mdr1 gene do not associate with chloroquine resistance among isolates from Brazil, Papua, and monkey-adapted strains. Exp Parasitol. 2005;109:256–9.
Marfurt J, de Monbrison F, Brega S, Barbollat L, Muller I, Sie A, et al. Molecular markers of in vivo Plasmodium vivax resistance to amodiaquine plus sulfadoxine-pyrimethamine: mutations in pvdhfr and pvmdr1. J Infect Dis. 2008;198:409–17.
Tjitra E, Baker J, Suprianto S, Cheng Q, Anstey NM. Therapeutic efficacies of artesunate-sulfadoxine-pyrimethamine and chloroquine-sulfadoxine-pyrimethamine in vivax malaria pilot studies: relationship to Plasmodium vivax dhfr mutations. Antimicrob Agents Chemother. 2002;46:3947–53.
Sidhu AB, Verdier-Pinard D, Fidock DA. Chloroquine resistance in Plasmodium falciparum malaria parasites conferred by pfcrt mutations. Science. 2002;298:210–3.
Barnadas C, Ratsimbasoa A, Tichit M, Bouchier C, Jahevitra M, Picot S, Menard D. Plasmodium vivax resistance to chloroquine in Madagascar: clinical efficacy and polymorphisms in pvmdr1 and pvcrt-o genes. Antimicrob Agents Chemother. 2008;52:4233–40.
Suwanarusk R, Russell B, Chavchich M, Chalfein F, Kenangalem E, Kosaisavee V, et al. Chloroquine resistant Plasmodium vivax: in vitro characterisation and association with molecular polymorphisms. PLoS One. 2007;2:e1089.
Orjuela-Sanchez P, de Santana Filho, Machado-Lima A, Chehuan YF, Costa MR, Alecrim M, et al. Analysis of single-nucleotide polymorphisms in the crt-o and mdr1 genes of Plasmodium vivax among chloroquine-resistant isolates from the Brazilian Amazon region. Antimicrob Agents Chemother. 2009;53:3561–4.
Mueller I, Widmer S, Michel D, Maraga S, McNamara DT, Kiniboro B, et al. High sensitivity detection of Plasmodium species reveals positive correlations between infections of different species, shifts in age distribution and reduced local variation in Papua New Guinea. Malar J. 2009;8:41.
Mueller I, Genton B, Rare L, Kiniboro B, Kastens W, Zimmerman P, et al. Three different Plasmodium species show similar patterns of clinical tolerance of malaria infection. Malar J. 2009;8:158.
Lin E, Kiniboro B, Gray L, Dobbie S, Robinson L, Laumaea A, et al. Differential patterns of infection and disease with P. falciparum and P. vivax in young Papua New Guinean children. PLoS One. 2010;5:e9047.
Peters W. Studies on the epidemiology of malaria in New Guinea. Part I. Holoendemic malaria–the clinical picture. Trans R Soc Trop Med Hyg. 1960;54:242–9.
Peters W, Standfast HA. Studies on the epidemiology of malaria in New Guinea. Part II. Holoendemic malaria–the entomological picture. Trans R Soc Trop Med Hyg. 1960;54:249–54.
Mueller I, Bockarie M, Alpers M, Smith T. The epidemiology of malaria in Papua New Guinea. Trends Parasitol. 2003;19:253–9.
Health PNGDo. Standard treatment for common illnesses of children in Papua New Guinea. 6th edition. Port Moresby, Papua New Guinea: Department of Health; 1993.
Yung AP, Bennett NM. Chloroquine-resistant falciparum malaria in Papua New Guinea. Med J Aust. 1976;2:320–1.
Rieckmann KH, Davis DR, Hutton DC. Plasmodium vivax resistance to chloroquine? Lancet. 1989;2:1183–4.
Schuurkamp GJ, Spicer PE, Kereu RK, Bulungol PK. A mixed infection of vivax and falciparum malaria apparently resistant to 4-aminoquinoline: a case report. Trans R Soc Trop Med Hyg. 1989;83:607–8.
Genton B, Baea K, Lorry K, Ginny M, Wines B, Alpers MP. Parasitological and clinical efficacy of standard treatment regimens against Plasmodium falciparum, P. vivax and P. malariae in Papua New Guinea. P N G Med J. 2005;48:141–50.
Marfurt J, Mueller I, Sie A, Maku P, Goroti M, Reeder JC, et al. Low efficacy of amodiaquine or chloroquine plus sulfadoxine-pyrimethamine against Plasmodium falciparum and P. vivax malaria in Papua New Guinea. Am J Trop Med Hyg. 2007;77:947–54.
Karunajeewa HA, Mueller I, Senn M, Lin E, Law I, Gomorrai PS, et al. A trial of combination antimalarial therapies in children from Papua New Guinea. N Engl J Med. 2008;359:2545–57.
Barnadas C, Koepfli C, Karunajeewa HA, Siba PM, Davis TM, Mueller I. Characterization of treatment failure in efficacy trials of drugs against Plasmodium vivax by genotyping neutral and drug resistance-associated markers. Antimicrob Agents Chemother. 2011;55:4479–81.
Barnadas C, Kent D, Timinao L, Iga J, Gray LR, Siba P, et al. A new high-throughput method for simultaneous detection of drug resistance associated mutations in Plasmodium vivax dhfr, dhps and mdr1 genes. Malar J. 2011;10:282.
McNamara DT, Thomson JM, Kasehagen LJ, Zimmerman PA. Development of a multiplex PCR-ligase detection reaction assay for diagnosis of infection by the four parasite species causing malaria in humans. J Clin Microbiol. 2004;42:2403–10.
Rosanas-Urgell A, Mueller D, Betuela I, Barnadas C, Iga J, Zimmerman PA, et al. Comparison of diagnostic methods for the detection and quantification of the four sympatric Plasmodium species in field samples from Papua New Guinea. Malar J. 2010;9:361.
Wampfler R, Mwingira F, Javati S, Robinson L, Betuela I, Siba P, et al. Strategies for detection of Plasmodium species gametocytes. PLoS One. 2013;8:e76316.
Carnevale EP, Kouri D, DaRe JT, McNamara DT, Mueller I, Zimmerman PA. A multiplex ligase detection reaction-fluorescent microsphere assay for simultaneous detection of single nucleotide polymorphisms associated with Plasmodium falciparum drug resistance. J Clin Microbiol. 2007;45:752–61.
Wong RP, Karunajeewa H, Mueller I, Siba P, Zimmerman PA, Davis TM. Molecular assessment of Plasmodium falciparum resistance to antimalarial drugs in Papua New Guinea using an extended ligase detection reaction fluorescent microsphere assay. Antimicrob Agents Chemother. 2011;55:798–805.
DaRe JT, Kouri DP, Zimmerman PA, Thomas PJ. Differentiating Plasmodium falciparum alleles by transforming Cartesian X, Y data to polar coordinates. BMC Genet. 2010;11:57.
Arnott A, Barnadas C, Senn N, Siba P, Mueller I, Reeder JC, et al. High genetic diversity of Plasmodium vivax on the North Coast of Papua New Guinea. Am J Trop Med Hyg. 2013;89:188–94.
Casey GJ, Ginny M, Uranoli M, Mueller I, Reeder JC, Genton B, et al. Molecular analysis of Plasmodium falciparum from drug treatment failure patients in Papua New Guinea. Am J Trop Med Hyg. 2004;70:251–5.
Marfurt J, de Monbrison F, Brega S, Barbollat L, Mueller I, Reeder JC, et al. Molecular markers of in vivo Plasmodium vivax resistance to amodiaquine plus sulphadoxine-pyrimethamine: mutations in pvdhfr and pvmdr1. J Infect Dis. 2008;198:409–17.
Mita T, Kaneko A, Hombhanje F, Hwaihwanje I, Takahashi N, Osawa H, et al. Role of pfmdr1 mutations on chloroquine resistance in Plasmodium falciparum isolates with pfcrt K76T from Papua New Guinea. Acta Trop. 2006;98:137–44.
Mehlotra RK, Fujioka H, Roepe PD, Janneh O, Ursos LM, Jacobs-Lorena V, et al. Evolution of a unique Plasmodium falciparum chloroquine-resistance phenotype in association with pfcrt polymorphism in Papua New Guinea and South America. Proc Natl Acad Sci USA. 2001;98:12689–94.
Alifrangis M, Dalgaard MB, Lusingu JP, Vestergaard LS, Staalsoe T, Jensen AT, et al. Occurrence of the Southeast Asian/South American SVMNT haplotype of the chloroquine-resistance transporter gene in Plasmodium falciparum in Tanzania. J Infect Dis. 2006;193:1738–41.
Gbotosho GO, Folarin OA, Bustamante C, da Silva LH, Mesquita E, Sowunmi A. Different patterns of pfcrt and pfmdr1 polymorphisms in P. falciparum isolates from Nigeria and Brazil: the potential role of antimalarial drug selection pressure. Am J Trop Med Hyg. 2012;86:211–3.
Koleala T, Karl S, Laman M, Moore BR, Benjamin J, Barnadas C, et al. Temporal changes in Plasmodium falciparum anti-malarial drug sensitivity in vitro and resistance-associated genetic mutations in isolates from Papua New Guinea. Malar J. 2015;14:37.
Nsanzabana C, Hastings IM, Marfurt J, Muller I, Baea K, Rare L, et al. Quantifying the evolution and impact of antimalarial drug resistance: drug use, spread of resistance, and drug failure over a 12-year period in Papua New Guinea. J Infect Dis. 2010;201:435–43.
Koepfli C, Ross A, Kiniboro B, Smith TA, Zimmerman PA, Siba P, et al. Multiplicity and diversity of Plasmodium vivax infections in a highly endemic region in Papua New Guinea. PLoS Negl Trop Dis. 2011;5:e1424.
Venkatesan M, Gadalla NB, Stepniewska K, Dahal P, Nsanzabana C, Moriera C, et al. Polymorphisms in Plasmodium falciparum chloroquine resistance transporter and multidrug resistance 1 genes: parasite risk factors that affect treatment outcomes for P. falciparum malaria after artemether-lumefantrine and artesunate-amodiaquine. Am J Trop Med Hyg. 2014;91:833–43.
Ariey F, Witkowski B, Amaratunga C, Beghain J, Langlois AC, Khim N, et al. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature. 2014;505:50–5.
Hastings IM, Ward SA. Coartem (artemether-lumefantrine) in Africa: the beginning of the end? J Infect Dis. 2005;192:1303–4 (author reply 1304–1305).
Malmberg M, Ferreira PE, Tarning J, Ursing J, Ngasala B, Bjorkman A, et al. Plasmodium falciparum drug resistance phenotype as assessed by patient antimalarial drug levels and its association with pfmdr1 polymorphisms. J Infect Dis. 2013;207:842–7.
Authors’ contributions
CB, LT were responsible of laboratory work, data analysis and writing up the manuscript. SJ, EM and JI participated in the laboratory work and in editing the manuscript. CK contributed species typing data and in editing the manuscript. LR, NS, BK, LJR contributed to field work and in editing the manuscript. IM, JCR, HK, TMD, PAZ and PMS helped with data analysis and writing up the paper. All authors read and approved the manuscript.
Acknowledgements
We would like to thank all the field team members who helped collect the samples used in this analysis. We thank all the study participants and their guardians. FINANCIAL SUPPORT: This study was supported by grants from Fogarty International Center (TW007872 and TW007377), and the Australian National Health Medical Research Council (#1010203). The Bill & Melinda Gates Foundation funded the original clinical studies under which the samples were collected. TMD was supported by an NHMRC Practitioner Fellowship (#1058260), IM by an NHMRC Senior Research Fellowship (#1043345), HK by an NHMRC Career Development Fellowship (#1064772) and LJR by an NHMRC Early Career Fellowship (#1016443).
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Céline Barnadas and Lincoln Timinao contributed equally to this work
Additional files
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Barnadas, C., Timinao, L., Javati, S. et al. Significant geographical differences in prevalence of mutations associated with Plasmodium falciparum and Plasmodium vivax drug resistance in two regions from Papua New Guinea. Malar J 14, 399 (2015). https://doi.org/10.1186/s12936-015-0879-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-015-0879-9