Abstract
Background
As a strong platelet agonist on the one hand and key molecule in plasmatic coagulation on the other hand, thrombin connects primary and secondary hemostasis. Thrombin generation potential reflects the individual capacity to generate thrombin, and has been associated with the occurrence of thromboembolic events. In the current study, we sought to identify predictors of thrombin generation potential in patients undergoing angioplasty and stenting for atherosclerotic cardiovascular disease.
Methods
Peak thrombin generation potential and area under the curve (AUC) of thrombin generation potential were determined with a commercially available assay in 315 patients on dual antiplatelet therapy 1 day after percutaneous intervention, and in 100 healthy individuals without cardiovascular disease.
Results
Median (interquartile range) peak thrombin generation potential and AUC of thrombin generation potential in the study cohort (n = 315) were significantly higher than in healthy individuals (n = 100) without cardiovascular disease (peak thrombin generation potential: 445.4 nM [354.5–551.8 nM] vs. 174.5 nM [141.2–261.2 nM]; AUC of thrombin generation potential: 5262.7 nM thrombin [4806.6–5756.9 nM thrombin] vs. 3405.2 nM thrombin [3043.6–3747.3 nM thrombin]; both p < 0.001). In patients undergoing angioplasty and stenting, hemoglobin A1c (HbA1c) was the only variable that was independently associated with both, peak thrombin generation potential and AUC of thrombin generation potential (both p ≤ 0.007). In contrast, platelet count and high-sensitivity C-reactive protein were only associated with peak thrombin generation potential, and body mass index and serum creatinine were only associated with AUC of thrombin generation potential after adjustment for covariates by multivariate linear regression analyses (all p < 0.05). Patients with HbA1c ≥ 6% had significantly higher peak thrombin generation potential and AUC of thrombin generation potential than patients with HbA1c < 6% (peak thrombin generation potential: 476.9 nM [385.8–577.9 nM] vs. 423.9 nM [335.8–529.5 nM], p = 0.002; AUC of thrombin generation potential: 5371.8 nM thrombin [4903 – 5899 nM thrombin] vs. 5172.5 nM thrombin [4731.8–5664.7 nM thrombin], p = 0.01). HbA1c ≥ 6% remained independently associated with both parameters of thrombin generation potential after multivariate linear regression analyses (both p ≤ 0.02).
Conclusions
Impaired glucose metabolism is associated with increased thrombin generation potential in patients undergoing angioplasty and stenting for cardiovascular disease.
Similar content being viewed by others
Introduction
Patients with atherosclerotic cardiovascular disease are at an increased risk of ischemic events such as myocardial infarction and stroke, which are the main causes of death in high income countries. Previous studies by others and us revealed higher in vivo expression of platelet surface P-selectin and activated glycoprotein IIb/IIIa as well as increased levels of monocyte-platelet aggregates in these patients compared to healthy individuals [1,2,3]. P-selectin and activated glycoprotein IIb/IIIa are expressed on the surface of activated platelets and can be measured by flow cytometry [4, 5]. Monocyte-platelet aggregates are mainly formed via the interaction of platelet surface P-selectin with its counterreceptor P-selectin glycoprotein ligand-1 on leukocytes [6], and were shown to be an even more sensitive indicator of ongoing platelet activation than P-selectin in several pathophysiological circumstances including myocardial infarction [7]. Besides these cellular markers, various soluble parameters of platelet activation are elevated in patients with cardiovascular disease [8, 9]. In particular soluble P-selectin deriving from platelet α-granules and endothelial Weibel-Palade bodies [6, 10], is increased in advanced atherosclerosis [8], and has been linked to the occurrence of ischemic outcomes [11]. Altogether, the above-mentioned findings point towards a smoldering prothrombotic state in cardiovascular disease.
In this environment, the exposure of subendothelial structures of the vessel wall due to the rupture of an atherosclerotic plaque leads to immediate platelet adhesion to collagen fibers [12]. Platelets become activated, release the content of their granules and trigger the recruitment of further platelets and the activation of the hemostatic system, which entails local thrombin generation [6, 12, 13]. As a strong platelet agonist on the one hand and key molecule in plasmatic coagulation on the other hand, thrombin connects primary and secondary hemostasis. Thus, it plays a pivotal role in the processes resulting in intravascular thrombus formation with narrowing or even occlusion of the affected artery and subsequent end organ ischemia [14]. In detail, thrombin rapidly activates human platelets via protease-activated receptors (PAR)-1 and PAR-4 even in the presence of state-of-the art antiplatelet therapy [15, 16]. It propagates platelet adhesion and aggregation, and thereby the formation of a first platelet plug [6]. As a serine protease, thrombin subsequently converts fibrinogen to fibrin resulting in the stabilization of the thrombus [14]. Recent data suggest that the formation of denser fibrin clots displaying an impaired lysability may be associated with worse clinical outcomes in patients with acute ischemic stroke [17]. Besides its role in thrombosis and hemostasis, thrombin serves as a signalling molecule and activates cell complexes involved in the development and progression of atherosclerosis [18].
Thrombin generation potential reflects the individual capacity to generate thrombin, and can be quantified by a commercially available assay [19]. Measuring thrombin generation potential may offer a way to identify patients with a hyper- or hypocoagulable phenotype [20]. Indeed, it has been shown that increased thrombin generation potential is associated with the occurrence of venous thromboembolism (VTE) in cancer patients and with recurrence of VTE after a first unprovoked thromboembolic event [21, 22]. Attanasio et al. found thrombin generation potential to predict cardiovascular death after acute coronary syndromes [23]. Furthermore, previous studies revealed higher thrombin generation potential in patients with lupus anticoagulant, protein C and S deficiencies, factor V Leiden mutation, and elevated coagulation factors VIII, IX and XI, as well as in women taking oral contraceptives or hormone replacement therapy [24].
Given the previous reports on thrombin generation potential as risk factor for adverse cardiovascular outcomes [20,21,22,23], we sought to identify predictors of thrombin generation potential in patients undergoing angioplasty and stenting for atherosclerotic cardiovascular disease.
Methods
Study population
The study population consisted of 315 patients on dual antiplatelet therapy after percutaneous intervention with endovascular stent implantation. All patients received daily aspirin (100 mg/days) and clopidogrel therapy (75 mg/days). Moreover, thrombin generation potential was determined in 100 healthy controls without cardiovascular disease (65 men, 35 women; median age 47 years [39–55]).
Exclusion criteria were a known aspirin or clopidogrel intolerance (allergic reactions, gastrointestinal bleeding), a therapy with vitamin K antagonists (warfarin, phenprocoumon, acenocoumarol) or novel oral anticoagulants (rivaroxaban, apixaban, dabigatran, edoxaban), treatment with ticlopidine, dipyridamole or nonsteroidal antiinflammatory drugs, a family or personal history of bleeding disorders, malignant paraproteinemias, myeloproliferative disorders or heparin-induced thrombocytopenia, severe hepatic failure, known qualitative defects in thrombocyte function, a major surgical procedure within 1 week before enrollment, a platelet count < 100,000 or > 450,000/µl and a hematocrit < 30%.
The study protocol was approved by the Ethics Committee of the Medical University of Vienna in accordance with the Declaration of Helsinki and written informed consent was obtained from all study participants.
Blood sampling
Blood was drawn by aseptic venipuncture from an antecubital vein using a 21-gauge butterfly needle (0.8 × 19 mm; Greiner Bio-One, Kremsmünster, Austria) 1 day after the percutaneous intervention. To avoid procedural deviations all blood samples were taken by the same physician applying a light tourniquet, which was immediately released and the samples were mixed adequately by gently inverting the tubes. After the initial 3 ml of blood had been discarded to reduce procedurally-induced platelet activation, blood was drawn into 3.8% sodium citrate Vacuette tubes (Greiner Bio-One; 9 parts of whole blood, 1 part of sodium citrate 0.129 M/l) for the measurement of thrombin generation potential.
Thrombin generation assay
Thrombin generation was measured with a commercially available assay (Technothrombin TGA kit, Techonoclone, Vienna, Austria) on a fully automated, computer-controlled microplate reader (Bio-Tek, FL X800) and a specially adapted software (Technothrombin TGA, Vienna, Austria) using the fluorogenic substrate Z-Gly-Gly-Arg-AMC (Bachem, Bubendorf, Switzerland) according to the manufacturer’s instructions as previously described [25]. The reaction was triggered with the TGA RC low reagent, which contained 71.6 pM recombinant human tissue factor lipidated in 3.2 μmol/l phospholipid micelles (phosphatidylcholine [2.56 μmol/l] and phosphatidylserine [0.64 μmol/l]). In this assay, thrombin activity is registered in a thrombin generation curve. From this curve, the parameters peak thrombin generation potential (the maximum concentration of thrombin generation) and area under the curve (AUC) of thrombin generation potential were used. All assay kits were from the same batch and all samples were tested within the same run by the same operator. The lower limit of detection with this assay is 0 for peak thrombin generation potential and the AUC of thrombin generation potential. The intra-assay coefficients of variation were 12% and 5.5% for peak thrombin generation potential and the AUC of thrombin generation potential, respectively (n = 21). Thrombin generation potential was available for all patients.
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (IBM SPSS version 24, Armonk, New York, USA). Median and interquartile range of continuous variables are shown. Categorical variables are given as number (%). To detect differences in continuous variables, we performed t-tests or Mann–Whitney U tests, as appropriate. Differences in categorical variables were assessed by the Chi square test. The Kolmogorov–Smirnov test was used to test for normal distribution, and variables with skewed distribution were log-transformed for regression analyses. Covariates for multivariate regression analyses were selected on the basis of univariate analyses (p ≤ 0.1), including age, sex, body mass index, hypertension, hyperlipidemia, active smoking, hematocrit, white blood cell count (WBC), platelet count, serum creatinine, high-sensitivity C-reactive protein (hsCRP), and hemoglobin A1c (HbA1c). Two-sided p-values < 0.05 were considered statistically significant.
Results
Clinical, laboratory, and procedural characteristics of the overall study population, of patients with HbA1c < 6% and of patients with HbA1c ≥ 6% are shown in Table 1.
Median (interquartile range) peak thrombin generation potential and AUC of thrombin generation potential in the study cohort (n = 315) were significantly higher than in healthy individuals (n = 100) without cardiovascular disease (peak thrombin generation potential: 445.4 nM [354.5–551.8 nM] vs. 174.5 nM [141.2–261.2 nM]; AUC of thrombin generation potential: 5262.7 nM thrombin [4806.6–5756.9 nM thrombin] vs. 3405.2 nM thrombin [3043.6–3747.3 nM thrombin]; both p < 0.001).
In patients undergoing angioplasty and stenting, active smoking as well as increasing WBC, platelet count, hsCRP and HbA1c were associated with higher peak thrombin generation potential in univariate analyses (all p < 0.05). In contrast, increasing serum creatinine was linked to lower peak thrombin generation potential (p = 0.03). In multivariate linear regression analysis, platelet count, hsCRP and HbA1c remained independently associated with peak thrombin generation potential (Table 2).
Using the AUC as parameter of thrombin generation potential, increasing BMI, platelet count and HbA1c were associated with higher levels of thrombin generation potential, whereas increasing serum creatinine was linked to lower AUC values in univariate analyses (all p < 0.05). In multivariate linear regression analysis, BMI, serum creatinine and HbA1c remained independently associated with the AUC of thrombin generation potential (Table 3).
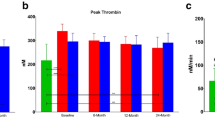
In a second step, we stratified the study population in patients with normal (< 6%) and elevated (≥ 6%) HbA1c levels according to a common definition of prediabetes [26, 27]. Those with elevated HbA1c were considered as patients with impaired glucose metabolism [28]. HbA1c was available for 301 patients (95.6%) of the study population, and with use of the above-mentioned cut-off value, normal and elevated HbA1c levels were seen in 156 (51.8%) and 145 (48.2%) patients, respectively. As expected, patients with HbA1c ≥ 6% had a higher BMI than patients with HbA1c < 6% (Table 1). Patients with elevated HbA1c had significantly higher peak thrombin generation potential and AUC of thrombin generation potential than patients with normal HbA1c (peak thrombin generation potential: 476.9 nM [385.8–577.9 nM] vs. 423.9 nM [335.8–529.5 nM], p = 0.002; AUC of thrombin generation potential: 5371.8 nM thrombin [4903–5899 nM thrombin] vs. 5172.5 nM thrombin [4731.8–5664.7 nM thrombin], p = 0.01; Fig. 1a, b). In multivariate linear regression analyses, elevated HbA1c remained independently associated with increased peak thrombin generation potential and AUC of thrombin generation potential (Tables 4, 5).
a Peak thrombin generation potential (peak thrombin) and b area under the curve of thrombin generation potential (AUC) in patients with normal (< 6%) and elevated (≥ 6%) hemoglobin A1c (HbA1c). The boundaries of the box show the lower and upper quartile of data, the line inside the box represents the median. Whiskers are drawn from the edge of the box to the highest and lowest values that are outside the box but within 1.5 times the box length
Prothrombin time, activated partial thromboplastin time, fibrinogen and D-dimer levels were similar in patients without and with elevated HbA1c (Table 6; all p ≥ 0.1).
Discussion
To the best of our knowledge, our study is the first to investigate predictors of thrombin generation potential in patients with atherosclerotic cardiovascular disease undergoing angioplasty and stenting. HbA1c was the only variable that was independently associated with both, peak thrombin generation potential and AUC of thrombin generation potential. In contrast, platelet count and hsCRP were only associated with peak thrombin generation potential, and BMI and serum creatinine were only associated with AUC of thrombin generation potential after adjustment for covariates by multivariate linear regression analyses. Patients with HbA1c ≥ 6% had significantly higher peak thrombin generation potential and AUC of thrombin generation potential than patients with HbA1c < 6%.
Association of thrombin generation potential with impaired glucose metabolism
Beijers et al. assessed thrombin generation potential with a different assay in 744 individuals from a cohort study on glucose metabolism in the general population [29]. In line with our results, they reported higher peak thrombin generation potential and increased endogenous thrombin generation potential in those with impaired glucose metabolism. Tripodi et al. analyzed blood samples from 60 patients with type 2 diabetes and found a significantly increased peak thrombin generation potential compared to 60 age- and gender-matched healthy controls [30]. Based on these previous observations and our findings, it may be speculated that increased thrombin generation potential at least in part contributes to the higher risk of ischemic events in diabetics undergoing angioplasty and stenting [31, 32]. However, clinical data linking thrombin generation potential with adverse cardiovascular outcomes in diabetics are missing, so far. Moreover, it remains to be established if antidiabetic therapy besides lowering blood glucose levels also affects thrombin generation potential. In our study, 11 patients with type 2 diabetes had HbA1c levels < 6% due to antidiabetic therapy (Table 1). These patients had numerically lower peak thrombin generation potential and AUC of thrombin generation potential than patients with HbA1c ≥ 6% (peak thrombin generation potential: 450.2 nM [397–522.5 nM] vs. 476.9 nM [385.8–577.9 nM]; AUC of thrombin generation potential: 5266.3 nM thrombin [4309–5658.8 nM thrombin] vs. 5371.8 nM thrombin [4903–5899 nM thrombin]; both p > 0.05).
Previous studies showed that subclinical and advanced atherosclerosis is associated with increased thrombin generation potential [33,34,35]. In line with these data, we found significantly higher peak thrombin generation potential and AUC of thrombin generation potential in patients undergoing angioplasty and stenting compared to 100 healthy individuals. Due to overall increased thrombin generation potential, the presence of macrovascular disease may abrogate the differences of thrombin generation potential between patients without and with impaired glucose metabolism. However, our findings of increased thrombin generation potential in patients with HbA1c ≥ 6% within a study population undergoing angioplasty and stenting, suggest that impaired glucose metabolism remains associated with thrombin generation potential even in advanced atherosclerotic cardiovascular disease.
Potential underlying mechanisms
The detailed mechanisms leading to increased thrombin generation potential in patients with impaired glucose metabolism remain unclear. Since pronounced thrombin generation has been reported in obesity [36], the higher BMI in patients with elevated HbA1c in our study may partially explain their increased thrombin generation potential compared to those with normal HbA1c levels [29]. Moreover, it has previously been suggested that low-grade inflammation may enhance thrombin generation potential [29]. Indeed, hsCRP was independently associated with peak thrombin generation potential in our cohort. However, after adjusting for BMI and hsCRP in multivariate linear regression analyses, HbA1c ≥ 6% was still significantly associated with both parameters of thrombin generation potential thereby indicating that additional factors might play a role. Indeed, Rusak et al. recently showed that the incubation of platelets with glucose results in an increased mean platelet volume, more pronounced collagen-induced platelet aggregation, secretion, platelet-dependent thrombin generation and phosphatidylserine expression, thereby suggesting that hyperglycemia itself exerts procoagulatory effects [37]. In line with these findings, Soma et al. reported a higher expression of platelet surface receptors and enhanced platelet activation in type 2 diabetics compared to healthy individuals [38]. Besides hyperglycemia and increased endogenous thrombin generation, insulin receptor substrate-1 polymorphisms may be responsible for high on-treatment platelet reactivity in diabetes. In detail, carriage of the G allele of rs13431554 in the insulin receptor substrate-1 gene was associated with a hyperreactive platelet phenotype in diabetics with coronary artery disease [39]. Pretorius et al. revealed that the clotting of plasma from patients with type 2 diabetes is amyloid in nature and potentially induced by bacterial lipopolysaccharides [40]. Their findings suggest a microbial component in the development of type 2 diabetes. If so, lipopolysaccharide-binding protein might become a treatment option for diabetes and a way to prevent the associated coagulopathy.
Association of thrombin generation potential with chronic kidney disease, inflammation and obesity
Interestingly, we observed decreasing peak thrombin generation potential and AUC of thrombin generation potential with increasing serum creatinine in univariate analyses. Furthermore, the association between AUC of thrombin generation potential and serum creatinine remained significant after adjustment for covariates in multivariate regression analysis, suggesting that thrombin generation potential decreases with worsening renal function. Thus, the increased bleeding risk in chronic kidney disease may be partially due to impaired thrombin generation [41, 42].
Our observation that platelet count and hsCRP were only associated with peak thrombin generation potential, and BMI and serum creatinine were only associated with AUC of thrombin generation potential after multivariate linear regression analyses may be explained by the underlying conditions: While platelet count and hsCRP can be considered as acute phase parameters reflecting inflammation, obesity and renal insufficiency are chronic comorbidities.
Limitations
A limitation of our study is the lack of clinical outcome data. Moreover, we did not include matched patients without percutaneous intervention and we did not assess thrombin generation potential prior to angioplasty and stenting. Therefore, we cannot exclude an influence of the angioplasty procedure on thrombin generation potential. However, since angioplasty was performed in all patients and thrombin generation potential was assessed 1 day after the percutaneous intervention in all patients, it is unlikely that the angioplasty procedure affected the association between impaired glucose metabolism and thrombin generation potential.
Conclusion
Impaired glucose metabolism is associated with increased thrombin generation potential in patients undergoing angioplasty and stenting for cardiovascular disease. Further studies are warranted to reveal potential clinical implications of these findings and to investigate if antidiabetic therapy decreases thrombin generation potential.
Abbreviations
- AUC:
-
area under the curve
- HbA1c:
-
hemoglobin A1c
- hsCRP:
-
high-sensitivity C-reactive protein
- VTE:
-
venous thromboembolism
- WBC:
-
white blood cell count
References
Gremmel T, Michelson AD, Frelinger AL 3rd. In vivo and protease-activated receptor-1-mediated platelet activation in patients presenting for cardiac catheterization. Platelets. 2016;27(4):308–16.
Furman MI, Barnard MR, Krueger LA, Fox ML, Shilale EA, Lessard DM, Marchese P, Frelinger AL 3rd, Goldberg RJ, Michelson AD. Circulating monocyte-platelet aggregates are an early marker of acute myocardial infarction. J Am Coll Cardiol. 2001;38(4):1002–6.
Furman MI, Benoit SE, Barnard MR, Valeri CR, Borbone ML, Becker RC, Hechtman HB, Michelson AD. Increased platelet reactivity and circulating monocyte-platelet aggregates in patients with stable coronary artery disease. J Am Coll Cardiol. 1998;31(2):352–8.
Shattil SJ, Hoxie JA, Cunningham M, Brass LF. Changes in the platelet membrane glycoprotein IIb.IIIa complex during platelet activation. J Biol Chem. 1985;260(20):11107–14.
Michelson AD. Flow cytometry: a clinical test of platelet function. Blood. 1996;87(12):4925–36.
Gremmel T, Frelinger AL 3rd, Michelson AD. Platelet physiology. Semin Thromb Hemost. 2016;42(3):191–204.
Michelson AD, Barnard MR, Krueger LA, Valeri CR, Furman MI. Circulating monocyte-platelet aggregates are a more sensitive marker of in vivo platelet activation than platelet surface P-selectin: studies in baboons, human coronary intervention, and human acute myocardial infarction. Circulation. 2001;104(13):1533–7.
Blann AD, Faragher EB, McCollum CN. Increased soluble P-selectin following myocardial infarction: a new marker for the progression of atherosclerosis. Blood Coagul Fibrinolysis. 1997;8(7):383–90.
Blann AD, Tan KT, Tayebjee MH, Davagnanam I, Moss M, Lip GY. Soluble CD40L in peripheral artery disease. Relationship with disease severity, platelet markers and the effects of angioplasty. Thromb Haemost. 2005;93(3):578–83.
Fijnheer R, Frijns CJ, Korteweg J, Rommes H, Peters JH, Sixma JJ, Nieuwenhuis HK. The origin of P-selectin as a circulating plasma protein. Thromb Haemost. 1997;77(6):1081–5.
Ridker PM, Buring JE, Rifai N. Soluble P-selectin and the risk of future cardiovascular events. Circulation. 2001;103(4):491–5.
Davi G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med. 2007;357(24):2482–94.
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–95.
Siller-Matula JM, Schwameis M, Blann A, Mannhalter C, Jilma B. Thrombin as a multi-functional enzyme. Focus on in vitro and in vivo effects. Thromb Haemost. 2011;106(6):1020–33.
Kahn ML, Nakanishi-Matsui M, Shapiro MJ, Ishihara H, Coughlin SR. Protease-activated receptors 1 and 4 mediate activation of human platelets by thrombin. J Clin Invest. 1999;103(6):879–87.
Badr Eslam R, Lang IM, Koppensteiner R, Calatzis A, Panzer S, Gremmel T. Residual platelet activation through protease-activated receptors (PAR)-1 and -4 in patients on P2Y12 inhibitors. Int J Cardiol. 2013;168(1):403–6.
Bembenek JP, Niewada M, Siudut J, Plens K, Czlonkowska A, Undas A. Fibrin clot characteristics in acute ischaemic stroke patients treated with thrombolysis: the impact on clinical outcome. Thromb Haemost. 2017;117(7):1440–7.
Loeffen R, Spronk HM, ten Cate H. The impact of blood coagulability on atherosclerosis and cardiovascular disease. J Thromb Haemost. 2012;10(7):1207–16.
van Veen JJ, Gatt A, Makris M. Thrombin generation testing in routine clinical practice: are we there yet? Br J Haematol. 2008;142(6):889–903.
Hron G, Kollars M, Binder BR, Eichinger S, Kyrle PA. Identification of patients at low risk for recurrent venous thromboembolism by measuring thrombin generation. JAMA. 2006;296(4):397–402.
Ay C, Dunkler D, Simanek R, Thaler J, Koder S, Marosi C, Zielinski C, Pabinger I. Prediction of venous thromboembolism in patients with cancer by measuring thrombin generation: results from the Vienna Cancer and Thrombosis Study. J Clin Oncol. 2011;29(15):2099–103.
Eichinger S, Hron G, Kollars M, Kyrle PA. Prediction of recurrent venous thromboembolism by endogenous thrombin potential and d-dimer. Clin Chem. 2008;54(12):2042–8.
Attanasio M, Marcucci R, Gori AM, Paniccia R, Valente S, Balzi D, Barchielli A, Carrabba N, Valenti R, Antoniucci D, et al. Residual thrombin potential predicts cardiovascular death in acute coronary syndrome patients undergoing percutaneous coronary intervention. Thromb Res. 2016;147:52–7.
Pabinger I, Ay C. Biomarkers and venous thromboembolism. Arterioscler Thromb Vasc Biol. 2009;29(3):332–6.
Gremmel T, Panzer S, Steiner S, Seidinger D, Koppensteiner R, Pabinger I, Kopp CW, Ay C. Response to antiplatelet therapy is independent of endogenous thrombin generation potential. Thromb Res. 2013;132(1):e24–30.
Rosella LC, Lebenbaum M, Fitzpatrick T, Zuk A, Booth GL. Prevalence of prediabetes and undiagnosed diabetes in Canada (2007–2011) according to fasting plasma glucose and Hba1c screening criteria. Diabetes Care. 2015;38(7):1299–305.
Morris DH, Khunti K, Achana F, Srinivasan B, Gray LJ, Davies MJ, Webb D. Progression rates from HbA1c 6.0–6.4% and other prediabetes definitions to type 2 diabetes: a meta-analysis. Diabetologia. 2013;56(7):1489–93.
Zhang X, Gregg EW, Williamson DF, Barker LE, Thomas W, Bullard KM, Imperatore G, Williams DE, Albright AL. A1C level and future risk of diabetes: a systematic review. Diabetes Care. 2010;33(7):1665–73.
Beijers HJ, Ferreira I, Spronk HM, Bravenboer B, Dekker JM, Nijpels G, ten Cate H, Stehouwer CD. Impaired glucose metabolism and type 2 diabetes are associated with hypercoagulability: potential role of central adiposity and low-grade inflammation—the Hoorn Study. Thromb Res. 2012;129(5):557–62.
Tripodi A, Branchi A, Chantarangkul V, Clerici M, Merati G, Artoni A, Mannucci PM. Hypercoagulability in patients with type 2 diabetes mellitus detected by a thrombin generation assay. J Thromb Thrombolysis. 2011;31(2):165–72.
Mathew V, Gersh BJ, Williams BA, Laskey WK, Willerson JT, Tilbury RT, Davis BR, Holmes DR Jr. Outcomes in patients with diabetes mellitus undergoing percutaneous coronary intervention in the current era: a report from the Prevention of REStenosis with Tranilast and its Outcomes (PRESTO) trial. Circulation. 2004;109(4):476–80.
De Luca G, Malek LA, Maciejewski P, Wasek W, Niewada M, Kaminski B, Drze wieck J, Kosmider M, Kubica J, Ruzyllo W, et al. Impact of diabetes on survival in patients with ST-segment elevation myocardial infarction treated by primary angioplasty: insights from the POLISH STEMI registry. Atherosclerosis. 2010;210(2):516–20.
Bernhard H, Wipfler P, Leschnik B, Novak M, Kraus J, Pilz G, Ladurner G, Muntean W. Relationship between thrombin generation and carotid intima-media thickness. Hamostaseologie. 2010;30(Suppl 1):S168–71.
Smid M, Dielis AW, Spronk HM, Rumley A, van Oerle R, Woodward M, ten Cate H, Lowe G. Thrombin generation in the Glasgow Myocardial Infarction Study. PLoS ONE. 2013;8(6):e66977.
Kalz J, ten Cate H, Spronk HM. Thrombin generation and atherosclerosis. J Thromb Thrombolysis. 2014;37(1):45–55.
Ay L, Kopp HP, Brix JM, Ay C, Quehenberger P, Schernthaner GH, Pabinger I, Schernthaner G. Thrombin generation in morbid obesity: significant reduction after weight loss. J Thromb Haemost. 2010;8(4):759–65.
Rusak T, Misztal T, Rusak M, Branska-Januszewska J, Tomasiak M. Involvement of hyperglycemia in the development of platelet procoagulant response: the role of aldose reductase and platelet swelling. Blood Coagul Fibrinolysis. 2017;28(6):443–51.
Soma P, Swanepoel AC, du Plooy JN, Mqoco T, Pretorius E. Flow cytometric analysis of platelets type 2 diabetes mellitus reveals ‘angry’ platelets. Cardiovasc Diabetol. 2016;15:52.
Zhang D, Zhang X, Liu D, Liu T, Cai W, Yan C, Han Y. Association between insulin receptor substrate-1 polymorphisms and high platelet reactivity with clopidogrel therapy in coronary artery disease patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2016;15:50.
Pretorius E, Page MJ, Engelbrecht L, Ellis GC, Kell DB. Substantial fibrin amyloidogenesis in type 2 diabetes assessed using amyloid-selective fluorescent stains. Cardiovasc Diabetol. 2017;16(1):141.
Ocak G, Rookmaaker MB, Algra A, de Borst GJ, Doevendans PA, Kappelle LJ, Verhaar MC, Visseren FL, Group SS. Chronic kidney disease and bleeding risk in patients at high cardiovascular risk: a cohort study. J Thromb Haemost. 2018;16(1):65–73.
Acedillo RR, Shah M, Devereaux PJ, Li L, Iansavichus AV, Walsh M, Garg AX. The risk of perioperative bleeding in patients with chronic kidney disease: a systematic review and meta-analysis. Ann Surg. 2013;258(6):901–13.
Authors’ contributions
SL: data analysis, writing the manuscript. CA: study design, critical revision and final approval of the manuscript. SP: critical revision and final approval of the manuscript. CWK: critical revision and final approval of the manuscript. TG: study design, patient recruitment, data analysis, writing the manuscript, final approval of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated in the current study are available from the corresponding author upon request.
Consent for publication
All authors have declared their consent for this publication.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the Medical University of Vienna in accordance with the Declaration of Helsinki and written informed consent was obtained from all study participants.
Funding
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lee, S., Ay, C., Kopp, C.W. et al. Impaired glucose metabolism is associated with increased thrombin generation potential in patients undergoing angioplasty and stenting. Cardiovasc Diabetol 17, 131 (2018). https://doi.org/10.1186/s12933-018-0774-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-018-0774-0