Abstract
Objective
Metformin is the standard first-line drug for patients with Type 2 diabetes (T2DM). However, the optimal second-line oral anti-diabetic agent (ADA) remains unclear. We investigated the cardiovascular risk of various ADAs used as add-on medication to metformin in T2DM patients from a nationwide cohort.
Methods
T2DM patients using different add-on oral ADAs after an initial metformin therapy of > 90 days were identified from the Taiwan National Health Insurance Database. Five classes of ADAs, including sulphonylureas (SU), glinides, thiazolidinediones (TZD), alpha-glucosidase inhibitors (AGI), and dipeptidyl peptidase-4 inhibitors (DPP-4I) were selected for analysis. The reference group was the SU added to metformin. Patients were excluded if aged < 20 years, had a history of stroke or acute coronary syndrome (ACS), or were receiving insulin treatment. The primary outcomes included any major adverse cardiovascular event (MACE) including ACS, ischemic/hemorrhagic stroke, and death. A Cox regression model was used to estimate the hazard ratio (HR) for MACE.
Results
A total of 26,742 patients receiving their add-on drug to metformin of either SU (n = 24,277), glinides (n = 962), TZD (n = 581), AGI (n = 808), or DPP-4I (n = 114) were analyzed. After a mean follow-up duration of 6.6 ± 3.4 years, a total of 4775 MACEs occurred. Compared with the SU+metformin group (reference), the TZD+metformin (adjusted HR: 0.66; 95% CI 0.50–0.88, p = 0.004) and AGI+metformin (adjusted HR: 0.74; 95% CI 0.59–0.94, p = 0.01) groups showed a significantly lower risk of MACE.
Conclusion
Both TZD and AGI, when used as an add-on drug to metformin were associated with lower MACE risk when compared with SU added to metformin in this retrospective cohort study.
Trial registration CE13152B-3. Registered 7 Mar, 2013, retrospectively registered
Similar content being viewed by others
Introduction
Patients with Type 2 diabetes (T2DM) have an increased risk of cardiovascular disease (CVD), which accounts for half of the causes of mortality in diabetic patients [1]. Given that incidence of T2DM is increasing worldwide, cardiovascular events associated with anti-diabetic therapy have become an important issue [2]. Based upon the beneficial effects of metformin shown in the UK Prospective Diabetes Study (UKPDS) [3, 4], metformin is currently recommended as the standard first-line drug therapy for patients with T2DM in clinical guidelines [5]. As diabetes is a progressive disease associated with a declining beta-cell function, second-line anti-diabetic agents (ADAs) will soon be added to metformin monotherapy in order to achieve the glycemic target [6]. Currently, there is no staunch evidence to correctly identify the most appropriate second-line ADA, particularly in terms of their impact on cardiovascular risk.
Although prospective randomized controlled trials (RCTs) have provided cardiovascular safety data on various ADAs including sulphonylureas (SU) [7], thiazolidinediones (TZD) [8,9,10], alpha-glucosidase inhibitors (AGI) [11, 12], and dipeptidyl peptidase-4 inhibitors (DPP-4I) [13,14,15], these trials were not designed to compare the individual ADAs as the add-on medication to baseline metformin monotherapy [16]. A landmark RCT comparing cardiovascular outcomes of SU, DPP-4I, glucagon-like peptide-1 analogues and insulin as second-line agents to metformin in newly diagnose T2DM patients is expected to be completed in 2020 [17]. Before any convincing clinical evidence becomes available, physicians might require real-world data which can elucidate on the cardiovascular risk associated with different add-on anti-diabetic medication, before they can make a clinical decision.
Several observational studies exploring cardiovascular risk associated with different second-line ADAs have generated diverse results. Ekström et al. reported that TZD and DPP-4I added to metformin was associated with both decreased mortality and cardiovascular events respectively, when compared to SU in a Swedish Diabetic Register Study [18]. In a Korean Health Insurance Review and Assessment Database Study, TZD (pioglitazone) added to metformin was associated with a decreased total CVD risk in patients with T2DM [19]. Another Korean Health Insurance Database Study showed that DPP-4I added to metformin had a lower CVD risk than SU added to metformin in T2DM patients [20]. However, Chang et al. using a Taiwan Diabetic Database, found that there were no differences in cardiovascular risk among several different add-on second-line oral ADAs, in a newly diagnosed diabetic population [21]. These discrepancies may have arisen due to studies of different populations, diverse cardiovascular outcomes employed, and variable observation durations followed. Of importance is that the observation duration for cardiovascular outcomes in these studies was short, ranging from 215 days to 5.6 years [18, 21], suggesting that the long-term cardiovascular risk of the different second-line ADAs added to metformin remains unclear. By using the Taiwan National Health Insurance Database which was implemented in 1995 [22, 23], we were able to investigate the long-term cardiovascular risk associated with different second-line ADAs. We hypothesized that TZD as the add-on medication to metformin decreases the cardiovascular risk when compared to SU. The presence of heart failure (HF) may abolish the cardiovascular benefits of TZD.
Materials and methods
Research database
The Taiwan National Health Insurance program was implemented in 1995. Currently, up to 99% of the Taiwanese population (~ 23 million) is enrolled in this program. The National Health Insurance Research Database includes figures regarding outpatient visits, hospital admissions, prescriptions, and disease records and is managed by the Taiwan National Health Research Institutes (NHRI). A systemic randomized sampling of patients’ data from 2000 to 2011, using a total of 1,000,000 subjects as the study population, was confirmed to be representative of the general Taiwanese population [22, 23]. The patients’ data was provided in an anonymous format, with written informed consents being waived. This study protocol was approved by the Institutional Review Board of Taichung Veterans General Hospital.
Study population
Patients aged ≥ 20 years with a recent diagnosis of T2DM, were identified according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 250 from 1999 to 2010. To avoid misclassification and to validate the diagnosis, T2DM was defined as three or more outpatient visits with a diabetic diagnosis code within a year, or at least one hospitalization with a diagnostic code of diabetes. The diabetic patients who initiated metformin as their first-line of treatment and used metformin monotherapy for a total duration of > 90 days were identified from the outpatient pharmacy prescription database. Metformin initiation was defined as being free of any oral ADAs or insulin injection before the first metformin prescription. According to the 2012 Taiwan Heart Failure Practical Guideline, heart failure (HF, ICD-9-CM code 428) diagnosis was subjectively judged by clinical physicians by the presence of either typical signs and symptoms of HF including fluid retention, weight gain, or objective evidence of cardiac dysfunction, or regular use of HF medications in the medical chart. Because the primary endpoints of the investigation was major adverse cardiovascular events (MACE) including acute coronary syndrome (ACS), ischemic/hemorrhagic stroke, and death, patients were excluded if they possessed a history of MI or stroke. Patients were also excluded if they had received oral ADAs other than metformin as their first-line of therapy, or received combination therapy (metformin plus other oral ADAs) as the first-line of therapy.
Definitions of drug use and comparison groups
Prescribed second-line ADA usage information, including prescribed drug types, dosages, dates of prescription, and total number of pills dispensed, was obtained from an ambulatory and inpatient claims database. Patients were classified into 5 groups based on their second-line oral ADAs added to metformin: SU, glinides, TZD, AGI, and DPP-4I. The reference group was SU added to metformin, which is the most commonly used combination therapy in Taiwan. The date of the above regimen initiation was defined as the index date. During the study period, every person-day was classified into either current use or non-use. Current use was defined as using the second-line medication during the period between the prescription date and the ending date of drug supply. Discontinuation of drug therapy was defined as when no medication was refilled after the end date of the prescription.
Study endpoint
The primary outcome of this study was the occurrence of major adverse cardiovascular events (MACE), which was a composite of all-cause mortality, acute coronary syndrome (ACS, ICD-9-CM: 410), and stroke (included fatal and nonfatal all stroke, ischemic stroke and hemorrhagic strokes; ICD-9-CM: 430–438). The study endpoint was defined as any events which occurred after the patients being added the second-line ADAs during the follow-up period (1999–2011).
Covariate ascertainment
Demographic data including age and gender were recorded. Cardiovascular co-morbidities including hypertension, hyperlipidemia, ischemic heart disease, peripheral vascular disease, valvular heart disease, pulmonary disease, and renal disease were identified by the ICD-9-CM diagnostic code if the patient had at least 1 hospitalization or at least 3 consecutive outpatient visits of the above listed diseases.
Statistical analysis
The data are presented as mean ± standard deviations (SD) for continuous variables, and proportions for categorical variables. Analysis of variance and Chi square tests were used for comparing differences in continuous and categorical variables. The MACE-free survival curves were plotted using the Kaplan–Meier method, and the statistical significance was examined by a log-rank test. Multivariable Cox proportional hazard regression models were used to identify potential confounding factors contributing to MACE occurrence (adjusted for age, gender, co-morbidities, and medications). We also performed stratified analysis to evaluate the cardiovascular outcomes in patients with or without the specific medications. The association between different second-line ADA use and the occurrence of MACE was expressed by the hazard ratio (HR) and a 95% confidence interval (CI). All statistical analyses were carried out using SAS software version 9.2 (SAS Institute, Inc., Cary, NC, USA). A p value of < 0.05 was considered statistically significant.
Results
Baseline characteristics
A total of 26,742 diabetic patients were enrolled in this study. Figure 1 shows the flow chart of the study cohort. Table 1 shows the baseline characteristics of the diabetic patients receiving different second-line ADAs added to metformin. The average age of the study population was 56.4 ± 11.8 years, while 52.7% were male. The diabetic duration (metformin monotherapy duration) was 2.5 ± 2.9 years prior to adding the second-line ADA.
Hypertension (60.0%) was the most prevalent comorbidity, followed by hyperlipidemia (57.8%) and then chronic obstructive pulmonary disease (COPD, 32.3%) in this cohort. The Met+DPP-4I group patients displayed a higher proportion of subjects with COPD (43.0%), CKD (4.4%), hyperlipidemia (74.6%) and HF (8.8%) than other groups. The proportion of patients diagnosed with hypertension was higher in the Met+AGI group (69.7%) than in other groups. Beta-blockers (50.1%) were the most frequently prescribed medications, followed by CCB (48.7%) and ACEIs/ARBSs (44.7%) in this cohort. In the Met+TZD group (n = 581), 227 patients (39.1%) used pioglitazone and 354 patients (60.9%) used rosiglitazone.
Effects of different second-line anti-diabetic agents on cardiovascular outcomes
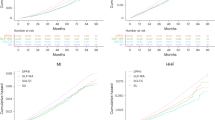
During an average of 6.6 ± 3.4 years’ follow-up, a total of 4775 MACE occurred. Table 2 shows the HRs for MACE and their composite cardiovascular endpoints. Compared to the SU group (29.0/1000 patient-years (PYs)), the incidence of MACE was significantly lower in both the TZD (17.8/1000 PYs, adjusted HR: 0.66, 95% CI 0.50–0.88, p = 0.004) and AGI (18.7/1000 PYs, adjusted HR: 0.74, 95% CI 0.59–0.94, p = 0.01) groups. There was no difference in MACE rate in patients receiving specific medications (i.e., ACEI/ARB or statin) or not among different subgroups (see Additional file 1: Table S1). In the TZD group, both pioglitazone (12.3/1000 PYs, adjusted HR: 0.54, 95% CI 0.30–0.98, p = 0.04) and rosiglitazone (20.3/1000 PYs, adjusted HR: 0.71, 95% CI 0.52–0.97, p = 0.03) groups showed a lower risk for MACE than SU (29.0/1000 PYs) group. (Additional file 1: Table S2) There was no difference in the incidence of ACS between SU and any other groups. The incidence of stroke was lower in both the TZD (56.5/1000 PYs, adjusted HR: 0.41, 95% CI 0.25–0.67, p = 0.0004) and AGI (93.3/1000 PYs, adjusted HR: 0.71, 95% CI 0.51–0.99, p = 0.04) groups than the SU (140/1000 PYs) group. The incidence of ischemic stroke was lower in both the TZD (38.7/1000 PYs, adjusted HR: 0.34, 95% CI 0.19–0.61, p = 0.0003) and AGI (71.7/1000 PYs, adjusted HR: 0.65, 95% CI 0.44–0.95, p = 0.02) groups than in the SU (117/1000 PYs) group. The incidence of hemorrhagic stroke was similar among the study groups. The incidence of all causes of mortality was also shown to be indifferent among the study groups. Figure 2 shows the Kaplan–Meier survival curves on MACE and their composite cardiovascular endpoints among different second-line ADA groups.
Subgroup analysis on cardiovascular outcomes in patients receiving different second-line anti-diabetic agents
Subgroup analysis comparing different second-line ADAs versus SU on the MACE incidence in diabetic patients was shown in Table 3. In patients receiving metformin plus TZD, the incidence of MACE was lower than those in the Met+SU group specifically in male (adjusted HR: 0.61, 95% CI 0.42–0.89, p = 0.01) as opposed to female (adjusted HR: 0.72, 95% CI 0.47–1.10, p = 0.13) patients. The adjusted HR for MACE was lower in both the Met+TZD (adjusted HR: 0.66, 95% CI 0.48–0.90, p = 0.009) and Met+AGI (adjusted HR: 0.77, 95% CI 0.59–1.00, p = 0.04) groups than in the Met+SU group, for patients with hypertension.
In patients without HF, the incidence of MACE was lower in both the Met+TZD (157/1000 PYs, adjusted HR: 0.61, 95% CI 0.45–0.82, p = 0.001) and Met+AGI (171/1000 PYs, adjusted HR: 0.72, 95% CI 0.56–0.93, p = 0.01) groups than in the Met+SU (279/1000 PYs) group. However, in patients with HF, Met+TZD (853/1000 PYs, adjusted HR: 1.43, 95% CI 0.67–3.04) use was associated with an increased MACE incidence when compared to the Met+SU (601/1000 PYs) group, although the statistical significance was not reached (p = 0.36). The interaction between patients with or without HF in the Met+TZD group was significant.
Discussion
There were two main findings in this study: (1) both TZD and AGI as add-on anti-diabetic agents to metformin reduce the risk of cardiovascular events in patients with T2DM. (2) In diabetic patients with a history of HF, add-on TZD or AGI to metformin did not reduce the risk of cardiovascular events.
Second-line add-on anti-diabetic agents and cardiovascular risk
In clinical guidelines, metformin monotherapy is currently the standard first-line anti-diabetic therapy for patients with T2DM [5]. Given the progressive nature of T2DM, adding a second-line ADA to intensify glycemic control is unavoidable for most patients [24]. There are several classes of oral ADAs with different modes of action to control blood sugar level [25]. In addition to their efficacy for glycemic control, their impact on cardiovascular risk is of great concern to clinical physicians. Due to the lack of large RCTs to guide the most appropriate second-line ADAs, observational studies may provide the necessary real-world evidence, thus contributing to an assessment of cardiovascular risk associated with glucose-lowering therapy.
A nationwide Swedish observational study showed that when compared to SU, second-line treatment with TZD and DPP-4I as the add-on medication to metformin was associated with lower risk of mortality and cardiovascular events, respectively [18]. Seong et al. reported that when compared with a DPP-4I, TZD (pioglitazone) as the add-on medication to metformin was associated with decreased cardiovascular and ischemic stroke risk in a Korean Health Insurance Review and Assessment Database [19]. Zghebi et al. found that TZD as an add-on medication to metformin was associated with lower risk of major cardiovascular disease or death, when compared with a SU add-on treatment to metformin in an UK Clinical Practice Research Datalink [26]. Recently, a Korean Health Insurance Service Study showed that TZD as a second-line drug to metformin had relatively lower risk of CVD compared to SU, although these findings did not reach statistical significance [20]. Similar to these previous studies, we observed that both TZD and AGI as the second-line ADAs added to metformin were associated with decreased cardiovascular risk including death, stroke and ACS, although the comparators were different [18, 19, 26]. Taken together, TZD may be the most appropriate second-line medication added to metformin in patients with T2DM. However, Chang et al. in a Taiwan National Health Insurance Database Study found no differences in cardiovascular risk among several add-on second-line oral ADAs, which is contrary to not only our study, but also the above mentioned studies [21]. This discrepancy may be attributed to the differences in the inclusion criteria (metformin monotherapy for 12 months vs 90 days, respectively), diabetic duration (175–238 days vs 2.5 ± 2.9 years, respectively), composite cardiovascular outcomes (MI, heart failure, and ischemic stroke vs ACS, all stroke, and death, respectively), and observational periods (215–305 days vs 6.6 ± 3.4 years, respectively). Since cardiovascular disease was slowly progressive in T2DM patients, a long follow-up period may be essential to observe any significant outcome associated with different ADAs [4]. To the best of our knowledge, this study has undergone the longest observational duration (6.6 ± 3.4 years) among all studies comparing different ADAs as the add-on medication to metformin regarding cardiovascular outcomes.
TZD and AGI on cardiovascular protection
In this study, we observed that both TZD and AGI as the second-line ADAs to baseline metformin reduce the risk of cardiovascular events compared to those patients using SU as their add-on medication. The reduction of MACE associated with TZD and AGI use was driven by the reduction in ischemic stroke. TZD, a potent insulin sensitizer, has favorable effects towards insulin sensitivity, plasma glucose, lipid metabolism, endothelial function, and vascular inflammation [27]. Similar to our finding, Seong et al. found that TZD (pioglitazone) plus metformin was associated with a lower risk of ischemic stroke, but not MI, when compared with the DPP-4I plus metformin group [19]. In a large scale RCT, the IRIS trial, Kernan et al. also reported that in patients with insulin resistance, the risk of stroke or myocardial infarction was lower in those using pioglitazone than a placebo [28]. Although this trial was carried out in non-diabetic patients, it has a much higher evidence level than the rest of other observational studies and proved the cardiovascular benefit for pioglitazone [28]. However, despite the fact that insulin resistance was associated with an increased risk of stroke, improving insulin sensitivity through the use of TZD did not always reduce the risk of stroke [29]. Lu et al. found that TZD (pioglitazone) did not change either cardiovascular or stroke risk when compared to the non-TZD group, among diabetic patients without macro-vascular disease [30]. The reasons why TZD did not reduce the risk of ACS in this study remains unclear. One possibility is that pioglitazone (account for 60.9% of the TZD patients) may reduce the risk of MI, while rosiglitazone (account for 39.1% of the TZD patients) may increase the MI risk in previous studies [31, 32]. Pooling both kinds of TZD users in this study might result in the neutral effect in preventing ACS comparing to SU users.
In the TZD plus metformin group, we observed that the lower incidence of MACE was observed only in male (adjusted HR: 0.61, 95% CI 0.42–0.89) in stratified analysis. This is consistent with the study conducted by Seong et al. showing that the CV risk reduction in the TZD plus metformin group was evident in male, but not female [19]. Estrogen has been shown to improve the lipid profile, increase NO signaling in the vasculature, and reduce atherosclerosis [33]. In animal study, rosiglitazone, a PPAR-γ agonist, can inhibit estrogen receptor (ER) activation and down-regulate ER expression [34]. Whether this anti-estrogen effect of TZD might accounts for the gender difference in reducing MACE by TZD remains to be explored. Further studies are needed in order to investigate the individual role of TZD in reducing the risk of stroke and MACE when it is added on to metformin.
When compared to SU, the use of AGI as the second-line ADA added to metformin decreased the risk of MACE and ischemic stroke in this study. Postprandial hyperglycemia is associated with an increase in oxidative stress, which in turn leads to endothelial dysfunction and subsequent cardiovascular diseases including ischemic stroke [35, 36]. Controlling postprandial hyperglycemia with acarbose might therefore prevent ischemic stroke [37]. The STOP-NIDDM trial showed that acarbose, a commonly used AGI in Taiwan, normalized postprandial hyperglycemia, and was also associated with a reduction in cardiovascular risk for pre-diabetic patients [11]. Consistently, acarbose has been shown to slow the progression of carotid intima-media thickness in patients diagnosed with impaired glucose tolerance, suggesting that acarbose might better prevent ischemic stroke than thrombosis at other arteries (i.e., coronary arteries) [38]. However, the Acarbose Cardiovascular Evaluation (ACE) trial, a large randomized controlled trial that unfortunately showed no cardiovascular benefit for acarbose in patients with coronary heart disease (CHD) and impaired glucose tolerance that contradicts with our result [39]. This discrepancy may be ascribed to the differences in the inclusion criteria (pre-diabetic with established CHD patients in ACE trial vs T2DM patients without CHD in this study), medication used (first-line acarbose add to cardiovascular medication vs second-line acarbose add to metformin, respectively), and composite cardiovascular outcomes (CV death, non-fatal MI, non-fatal stroke, hospital admission for unstable angina, or HF vs ACS, all stroke, and death, respectively). Therefore, the cardiovascular protective effect of acarbose as a second-line ADA to metformin has not been previously reported in diabetic patients. We provided new evidence showing that AGI as the add-on medication to metformin reduces the risk of MACE including ischemic stroke when compared to SU in diabetic patients without CHD history. Whether acarbose as a second-line medication to metformin reduces MACE risk in diabetic patients with established CHD deserved further investigation.
Heart failure and second-line anti-diabetic medication in diabetic patients
HF occurs in 8–20% of patients with T2DM, where up to 50% of diabetic patients may develop HF during the treatment courses [40, 41]. In a national sample of medicare claims database, the mortality rates were 32.7/100 person-years in diabetic patients with HF compared with 3.7/100 person-years in diabetic patients without HF (HR 10.6, 95% CI 10.4–10.9), indicating that HF is associated with 10-times CV risk in diabetic patients [42]. TZDs, including rosiglitazone and pioglitazone, have been reported as a cause of fluid retention, while also increasing the risk of HF [31, 32, 43]. The mechanism of TZD being associated with fluid retention remains unclear, although it has been suggested that peroxisome proliferator activated receptor-gamma activation by TZD may enhance sodium channel activity in the collecting ducts and an increase in both sodium and water re-absorption and retention [44, 45]. In this study, we observed that TZD as the second-line agents was associated with a decreased cardiovascular risk when compared to SU. Subgroup analysis then showed that the cardiovascular benefit of TZD was consistent in patients without HF, indicating that TZD therapy could be favorable in patients without a history of HF. However, in patients with a history of HF, the use of TZD as the second-line agent may increase the risk of MACE (adjusted HR: 1.47, 95% CI 0.69–3.12, p = 0.32) compared to SU.
The 2017 the American Diabetes Association guideline discouraged the use of TZD as the first-line ADA in diabetic patients with HF, due to its concern of worsening HF [25]. In this study, we further found that TZD may not need to be used as a second-line ADA add-on to metformin in patients with pre-existing HF. Whether TZD as the second-line ADA to metformin monotherapy increases cardiovascular risk in diabetic patients with a history of HF deserves further investigation.
Study strength
Previous studies comparing various ADAs added to metformin in cardiovascular outcomes were followed at a short duration [18, 19, 21, 26]. This study offered the longest observational duration (6.6 ± 3.4 years) among all the studies, and will provide robust evidence as a guideline for the appropriate second-line ADA added to metformin.
Limitations
This study had several limitations. First, this was a non-randomized, uncontrolled observational cohort study. We could not be certain whether or not patients complied properly with their prescribed medications and dosages. Secondly, glycemic levels (evaluated by HbA1c), LDL cholesterol concentrations, kidney function (assessed by eGFR), and body mass index were not available in the Taiwan National Health Insurance Database. The degree of glycemic control and the severity of diabetes might together influence the observed CV outcome. Furthermore, low eGFR has been reported to be an independent risk factor for CV and renal events in diabetic patients [46]. Other un-available socio-demographic factors such as smoking status, physical activity, educational level, socioeconomic status, and ethnicity might also confound the CV outcome. Because of the above mentioned shortcomings, translating the study conclusions to clinical recommendations should be with cautions for specific drug therapies. Thirdly, there was a large variation in sample sizes among the different groups. Only the SU group (n = 24,277) has a large number of patients, while other groups consisted of less than 1000 patients each. Interpreting the analytical results involving these groups should be with caution. Fourth, the baseline co-morbidities (i.e., HF) of the patients in each group were not completely matched. In 2007, Nissen and Wolski raised concerns about the cardiovascular safety of rosiglitazone. This information might discourage physicians to use thiazolidinediones, either as a first-line or a second-line therapy, in diabetic patients. On the other hand, previous studies have shown that DPP-4I use was associated with a cardiovascular safety outcome, assuming DPP-4I to be a preferred choice by clinical physicians [47]. These treatment indications, clinical preference, and cost of the various drugs might contribute to the selection bias in baseline characteristics and confounded the result. However, we have adjusted the baseline co-morbidities in the analysis model to minimize this bias, making the result relevant to clinical practice. Finally, this study included mainly East Asian subjects. Whether the results could be applied to Western populations remains unknown.
Perspectives
In recent years, several large RCTs have demonstrated cardiovascular benefits of newer glucose lowering agents not assessed in the Taiwanese cohort. By inhibiting re-absorption of urinary glucose in the proximal tubule, the sodium glucose cotransporter-2 (SGLT-2) inhibitor is a new ADA that carries a low risk for hypoglycemia. The only cardiovascular outcomes trial of SGLT-2 inhibitors to date, the EMPA-REG OUTCOME trial, showed that empagliflozin use was associated with a reduction in the primary composite endpoint of cardiovascular mortality, non-fatal MI, or non-fatal stroke compared with placebo in T2D patients [48].
There are currently 4 FDA-approved DPP-4I sitagliptin, saxagliptin, linagliptin and alogliptin under use in Taiwan. The examination of cardiovascular outcomes with alogliptin versus standard of care in patients with T2D and ACS (EXAMINE), Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus (SAVOR-TIMI 53), and Trial Evaluating Cardiovascular Outcome with Sitagliptin (TECOS) trials have been conducted to evaluate the CV risk [47]. These DPP-4Is are safe in terms of cardiovascular endpoints [49]. However, their effect on the risk of HF remains unclear. Similarly, linagliptin use was not associated with increased cardiovascular risk a large pooled safety analysis [50]. In this study, the number of cases using DPP-4I is, only 114, too small to determine statistical difference. A new RCT comparing cardiovascular outcomes of SU, DPP-4I, glucagon-like peptide-1 analogues and insulin as second-line agents to metformin in T2DM patients is expected to be completed in 2020 [17]. Whether the above mentioned new ADAs as the second-line medication add to metformin is associated with CV safety deserved further investigation.
Conclusion
Both TZD and AGI as add-on ADAs to metformin reduce the risk of cardiovascular events. Thus, adding a TZD or an AGI rather than a SU as a second-line agent to metformin monotherapy might be considered. In diabetic patients with a history of HF, TZD as the add-on medication did not reduce the risk of cardiovascular events.
Abbreviations
- ACS:
-
acute coronary syndrome
- AGI:
-
alpha-glucosidase inhibitor
- CIs:
-
confidence intervals
- COPD:
-
chronic obstructive pulmonary disease
- CVD:
-
cardiovascular disease
- DPP-4I:
-
dipeptidyl peptidase-4 inhibitor
- ER:
-
estrogen receptor
- HF:
-
heart failure
- HR:
-
hazard ratio
- ICD-9-CM:
-
International Classification of Diseases Ninth Revision Clinical Modification
- LHID:
-
Longitudinal Health Insurance Database
- Met:
-
metformin
- NHIRD:
-
National Health Insurance Research Database
- NHRI:
-
National Health Research Institute
- OR:
-
odds ratio
- RCT:
-
randomized controlled trial
- SD:
-
standard deviation
- SU:
-
sulphonylureas
- TZD:
-
thiazolidinediones
References
Rutter MK, Nesto RW. Blood pressure, lipids and glucose in Type 2 diabetes: how low should we go? Re-discovering personalized care. Eur Heart J. 2011;32:2247–55.
Xu J, Rajaratnam R. Cardiovascular safety of non-insulin pharmacotherapy for Type 2 diabetes. Cardiovasc Diabetol. 2017;16:18.
UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with Type 2 diabetes (UKPDS 34). Lancet. 1998;352:854–65.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in Type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in Type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–9.
Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with Type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999;281:2005–12.
Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with Type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Liao HW, Saver JL, Wu YL, Chen TH, Lee M, Ovbiagele B. Pioglitazone and cardiovascular outcomes in patients with insulin resistance, pre-diabetes and Type 2 diabetes: a systematic review and meta-analysis. BMJ Open. 2017;7:e013927.
Dormandy JA, Charbonnel B, Eckland DJ, et al. Secondary prevention of macrovascular events in patients with Type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366:1279–89.
Tian Y, Chen T, Wu Y, et al. Pioglitazone stabilizes atherosclerotic plaque by regulating the Th17/Treg balance in AMPK-dependent mechanisms. Cardiovasc Diabetol. 2017;16:140.
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003;290:486–94.
Shimabukuro M, Tanaka A, Sata M, et al. alpha-Glucosidase inhibitor miglitol attenuates glucose fluctuation, heart rate variability and sympathetic activity in patients with Type 2 diabetes and acute coronary syndrome: a multicenter randomized controlled (MACS) study. Cardiovasc Diabetol. 2017;16:86.
Green JB, Bethel MA, Armstrong PW, et al. Effect of sitagliptin on cardiovascular outcomes in Type 2 diabetes. N Engl J Med. 2015;373:232–42.
Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with Type 2 diabetes mellitus. N Engl J Med. 2013;369:1317–26.
White WB, Cannon CP, Heller SR, et al. Alogliptin after acute coronary syndrome in patients with Type 2 diabetes. N Engl J Med. 2013;369:1327–35.
Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with Type 2 diabetes: a meta-analysis. JAMA. 2016;316:313–24.
Nathan DM, Buse JB, Kahn SE, et al. Rationale and design of the glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE). Diabetes Care. 2013;36:2254–61.
Ekstrom N, Svensson AM, Miftaraj M, et al. Cardiovascular safety of glucose-lowering agents as add-on medication to metformin treatment in Type 2 diabetes: report from the Swedish National Diabetes Register. Diabetes Obes Metab. 2016;18:990–8.
Seong JM, Choi NK, Shin JY, et al. Differential cardiovascular outcomes after dipeptidyl peptidase-4 inhibitor, sulfonylurea, and pioglitazone therapy, all in combination with metformin, for Type 2 diabetes: a population-based cohort study. PLoS ONE. 2015;10:e0124287.
Ha KH, Kim B, Choi H, Kim DJ, Kim HC. Cardiovascular events associated with second-line anti-diabetes treatments: analysis of real-world Korean data. Diabet Med. 2017;34:1235–43.
Chang YC, Chuang LM, Lin JW, Chen ST, Lai MS, Chang CH. Cardiovascular risks associated with second-line oral antidiabetic agents added to metformin in patients with Type 2 diabetes: a nationwide cohort study. Diabet Med. 2015;32:1460–9.
Hung CY, Hsieh YC, Li CH, Huang JL, Lin CH, Wu TJ. Age and CHADS2 score predict the effectiveness of renin-angiotensin system blockers on primary prevention of atrial fibrillation. Sci Rep. 2015;5:11442.
Hsieh YC, Hung CY, Li CH, et al. Angiotensin-receptor blocker, angiotensin-converting enzyme inhibitor, and risks of atrial fibrillation: a nationwide cohort study. Medicine (Baltimore). 2016;95:e3721.
Ekstrom N, Svensson AM, Miftaraj M, et al. Durability of oral hypoglycemic agents in drug naive patients with Type 2 diabetes: report from the Swedish National Diabetes Register (NDR). BMJ Open Diabetes Res Care. 2015;3:e000059.
American Diabetes Association. Pharmacologic approaches to glycemic treatment. Sec. 8. In: Standards of Medical Care in Diabetes—2017. Diabetes Care, Vol. 40; 2017. pp. S64–74.
Zghebi SS, Steinke DT, Rutter MK, Emsley RA, Ashcroft DM. Comparative risk of major cardiovascular events associated with second-line antidiabetic treatments: a retrospective cohort study using UK primary care data linked to hospitalization and mortality records. Diabetes Obes Metab. 2016;18:916–24.
Yki-Jarvinen H. Thiazolidinediones. N Engl J Med. 2004;351:1106–18.
Kernan WN, Viscoli CM, Furie KL, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374:1321–31.
Vaccaro O, Masulli M, Nicolucci A, et al. Effects on the incidence of cardiovascular events of the addition of pioglitazone versus sulfonylureas in patients with Type 2 diabetes inadequately controlled with metformin (TOSCA.IT): a randomised, multicentre trial. Lancet Diabetes Endocrinol. 2017;5:887–97.
Lu CJ, Sun Y, Muo CH, Chen RC, Chen PC, Hsu CY. Risk of stroke with thiazolidinediones: a ten-year nationwide population-based cohort study. Cerebrovasc Dis. 2013;36:145–51.
de Jong M, van der Worp HB, van der Graaf Y, Visseren FLJ, Westerink J. Pioglitazone and the secondary prevention of cardiovascular disease. A meta-analysis of randomized-controlled trials. Cardiovasc Diabetol. 2017;16:134.
Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356:2457–71.
Murphy E. Estrogen signaling and cardiovascular disease. Circ Res. 2011;109:687–96.
Gunin AG, Bitter AD, Demakov AB, Vasilieva EN, Suslonova NV. Effects of peroxisome proliferator activated receptors-alpha and -gamma agonists on estradiol-induced proliferation and hyperplasia formation in the mouse uterus. J Endocrinol. 2004;182:229–39.
El Midaoui A, Wu R, de Champlain J. Prevention of hypertension, hyperglycemia and vascular oxidative stress by aspirin treatment in chronically glucose-fed rats. J Hypertens. 2002;20:1407–12.
Ceriello A, Bortolotti N, Motz E, et al. Meal-generated oxidative stress in Type 2 diabetic patients. Diabetes Care. 1998;21:1529–33.
Hyvarinen M, Qiao Q, Tuomilehto J, et al. Hyperglycemia and stroke mortality: comparison between fasting and 2-h glucose criteria. Diabetes Care. 2009;32:348–54.
Hanefeld M, Chiasson JL, Koehler C, Henkel E, Schaper F, Temelkova-Kurktschiev T. Acarbose slows progression of intima-media thickness of the carotid arteries in subjects with impaired glucose tolerance. Stroke. 2004;35:1073–8.
Holman RR, Coleman RL, Chan JCN, et al. Effects of acarbose on cardiovascular and diabetes outcomes in patients with coronary heart disease and impaired glucose tolerance (ACE): a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2017;5:877–86.
Nesto RW, Bell D, Bonow RO, et al. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. October 7, 2003. Circulation. 2003;108:2941–8.
Kannel WB, Hjortland M, Castelli WP. Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol. 1974;34:29–34.
Bertoni AG, Hundley WG, Massing MW, Bonds DE, Burke GL, Goff DC Jr. Heart failure prevalence, incidence, and mortality in the elderly with diabetes. Diabetes Care. 2004;27:699–703.
Lincoff AM, Wolski K, Nicholls SJ, Nissen SE. Pioglitazone and risk of cardiovascular events in patients with Type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA. 2007;298:1180–8.
Hong G, Lockhart A, Davis B, et al. PPARgamma activation enhances cell surface ENaCalpha via up-regulation of SGK1 in human collecting duct cells. FASEB J. 2003;17:1966–8.
Yokoyama H, Araki S, Kawai K, et al. Pioglitazone treatment and cardiovascular event and death in subjects with Type 2 diabetes without established cardiovascular disease (JDDM 36). Diabetes Res Clin Pract. 2015;109:485–92.
Ninomiya T, Perkovic V, de Galan BE, et al. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol. 2009;20:1813–21.
Bae JC. Diabetes drugs and cardiovascular safety. Endocrinol Metab (Seoul). 2016;31:239–44.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Ou HT, Chang KC, Li CY, Wu JS. Risks of cardiovascular diseases associated with dipeptidyl peptidase-4 inhibitors and other antidiabetic drugs in patients with Type 2 diabetes: a nation-wide longitudinal study. Cardiovasc Diabetol. 2016;15:41.
Rosenstock J, Marx N, Neubacher D, et al. Cardiovascular safety of linagliptin in Type 2 diabetes: a comprehensive patient-level pooled analysis of prospectively adjudicated cardiovascular events. Cardiovasc Diabetol. 2015;14:57.
Authors’ contributions
YCH, JLH, CHL and TJW conceived and designed the study. CLY, JCL, CYH, and CHL performed data collection. YCL, CCL, and CPL performed the statistical analysis. YCH and CWC wrote the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank the Healthcare Service Research Center of Taichung Veterans General Hospital for assisting with the statistical analyses.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Consent for publication
If the manuscript is accepted, we approve it for publication in Cardiovascular Diabetology.
Ethics approval and consent to participate
The patients’ data was provided in an anonymous format, with written informed consents being waived. This study protocol was approved by the Institutional Review Board of Taichung Veterans General Hospital.
Funding
This study was supported in part by grants from Taichung Veterans General Hospital, Taiwan (TCVGH-NHRI10603, TCVGH-1067310C, TCVGH-FCU1068205, TCVGH-YM1060201, TCVGH-VTA106PREM1, TCVGH-1033103C, TCVGH-1033105C, TCVGH-1043109C, TCVGH-1053108C, TCVGH-VHCY1068606) and the National Science Council, Taiwan (102-2314-B-075A-009-MY2, 104-2314-B-367-001, 105-2314-B-367-001-MY3).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
12933_2018_663_MOESM1_ESM.docx
Additional file 1: Table S1. Hazard ratios of MACE in patients receiving different 2nd-line anti-diabetic agents with or without ACEI/ARBs and statins. Table S2. Hazard ratios of MACE in patients receiving pioglitazone and rosiglitazone as the 2nd-line anti-diabetic agents compared to SU.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chan, CW., Yu, CL., Lin, JC. et al. Glitazones and alpha-glucosidase inhibitors as the second-line oral anti-diabetic agents added to metformin reduce cardiovascular risk in Type 2 diabetes patients: a nationwide cohort observational study. Cardiovasc Diabetol 17, 20 (2018). https://doi.org/10.1186/s12933-018-0663-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-018-0663-6