Background
Type 1 diabetes is associated with increased cardiovascular disease (CVD). Decreased endothelial progenitor cells (EPCs) number plays a pivotal role in reduced endothelial repair and development of CVD. We aimed to determine if cardioprotective effect of metformin is mediated by increasing circulating endothelial progenitor cells (cEPCs), pro-angiogenic cells (PACs) and decreasing circulating endothelial cells (cECs) count whilst maintaining unchanged glycemic control.
Methods
This study was an open label and parallel standard treatment study. Twenty-three type 1 diabetes patients without overt CVD were treated with metformin for 8 weeks (treatment group-TG). They were matched with nine type 1 diabetes patients on standard treatment (SG) and 23 age- and sex-matched healthy volunteers (HC). Insulin dose was adjusted to keep unchanged glycaemic control. cEPCs and cECs counts were determined by flow cytometry using surface markers CD45dimCD34+VEGFR-2+ and CD45dimCD133−CD34+CD144+ respectively. Peripheral blood mononuclear cells were cultured to assess changes in PACs number, function and colony forming units (CFU-Hill’s colonies).
Results
At baseline TG had lower cEPCs, PACs, CFU-Hills’ colonies and PACs adhesion versus HC (p < 0.001-all variables) and higher cECs versus HC (p = 0.03). Metformin improved cEPCs, PACs, CFU-Hill’s colonies number, cECs and PACs adhesion (p < 0.05-all variables) to levels seen in HC whilst HbA1c (one-way ANOVA p = 0.78) and glucose variability (average glucose, blood glucose standard deviation, mean amplitude of glycaemic excursion, continuous overall net glycaemic action and area under curve) remained unchanged. No changes were seen in any variables in SG. There was an inverse correlation between CFU-Hill’s colonies with cECs.
Conclusions
Metformin has potential cardio-protective effect through improving cEPCs, CFU-Hill’s colonies, cECs, PACs count and function independently of hypoglycaemic effect. This finding needs to be confirmed by long term cardiovascular outcome studies in type 1 diabetes.
Trial registration ISRCTN26092132
Similar content being viewed by others
Background
Type 1 diabetes mellitus is characterised by an increased risk of cardiovascular disease (CVD) compared with the non-diabetic population [1, 2]. The life expectancy of adults at age of 20 with type 1 diabetes is reduced by up to 13 years with CVD being the leading cause of premature death [3]. Even with good glycaemic control the CVD risk remains more than twice that of non-diabetic individuals [4, 5]. Despite current use of statins and ACE-inhibitors, CVD risk in type 1 diabetes remains higher than non-diabetic population. Patients with type 1 diabetes mellitus without overt CVD or diabetes-related complications have been shown to have features of endothelial dysfunction [6]. There is a need to explore newer treatment options to improve endothelial dysfunction and reduce CVD risk. Endothelial dysfunction itself results from imbalance between vascular damage and vascular repair.
Vascular damage results in the release of circulating endothelial cells (cECs) from the vascular intima. cECs are mature endothelial cells characterised by presence of endothelial cell surface markers like CD144 and absence of heamatopoetic (e.g. CD45) and progenitor cell markers (e.g. CD133). CD144 is important for maintaining endothelium integrity through cell to cell adhesion [7].
cECs are formed through detachment from vascular intima due to irreversible loss of integrity as a response to endothelial activation by mechanical stress, inflammatory cytokines, growth factors, infectious agents, lipoprotein, and oxidative stress [7, 8]. Furthermore, cECs are elevated in type 1 and type 2 diabetes [9, 10], and are a predictor of CVD events in similar high risk populations [11]. cECs count (a marker of vascular damage) is directly related to HbA1c in type 1 diabetes [9].
In response to vascular damage, vascular repair is promoted by local endothelial cells and bone-marrow derived cells, called endothelial progenitor cells (EPCs). EPCs were first described in 1997 [12]. These cells have the ability to home to the site of vascular injury, proliferate and contribute to endothelial repair [13], thereby maintaining endothelial health.
Circulating endothelial progenitor cells (cEPCs) are a heterogenous population of cells characterised by the expression of surface antigen CD34+, VEGFR-2+ and/or CD133+ identified by flow cytometry. CD34+ and CD133+ are hematopoietic stem cell markers [14, 15]. VEGFR-2 is a surface marker of endothelial lineage. Progenitor cells undergo various stages of maturation. CD133 marker is lost as cEPCs mature. Thus, more mature cEPCs are positive for CD34 and VEGFR-2 [16]. VEGFR-2 plays an important role in angiogenesis by promoting endothelial cell growth and cell permeability [17]. cEPCs predict microvascular complication in type 2 diabetes [18] and future CVD events in patients with CVD [19]. In addition cEPCs count is inversely related to HbA1c [20].
Proangiogenic cells (PACs), previously known as early EPCs are the cultured peripheral blood mononuclear cells (PBMNC) whereas colonies derived from replated PBMNC are known as colony forming units (CFU-Hill’s colonies) [21]. PACs and CFU-Hill’s colonies are reduced in both type 1 and type 2 diabetes and CFU-Hill’s colonies have been shown to predict CVD events [20–24]. PAC count is inversely related to HbA1c and much more suppressed in the presence of diabetes-related complications [23–25]. In addition, the functional capacity of cultured PACs is impaired in patients with diabetes [23].
As the outcome of CVD management using the same therapies is worse in diabetic versus nondiabetic patients [26], there is a need to identify additional treatment options and study the mechanism of action behind the cardio-protective properties. Metformin has been shown to have cardio-protective properties in type 2 diabetes, [27, 28]. In the UKPD trial [27] the incidence of myocardial infarction was reduced after a median follow-up of 10 years. Furthermore, metformin also reduced cardiac infarct size and improved endothelial function in diabetes [29, 30]. It has been shown that metformin under diabetic environment protects ECs regardless of its glycaemic effects [31]. In nondiabetic patients however, there were mixed findings regarding metformin’s cardio-protective effect. Metformin had no effect on reducing left ventricular dysfunction and re-perfusion cardiac injury in non-diabetic patients following an acute myocardial infarction and coronary arterial bypass graft [32, 33].
Thus, the data are in keeping with a cardio-protective effect of metformin in diabetes, although the underlying mechanism is unclear. Since metformin has been shown to improve endothelial function in type 1 diabetes, we hypothesised that metformin modulates cEPCs and cECs count and this cardio-protective effect is mediated beyond improving glycaemic control.
Thus the primary aim of our trial was to study if metformin improved cEPCs number in type 1 diabetes whilst, maintaining unchanged diabetic control. Secondary aims were to determine if metformin also improved cECs number, PACs number and function and CFU-Hill’s colonies.
Methods
We recruited 23 patients with type 1 diabetes with inclusion criteria of HbA1c <8.5 % (69 mmol/mmol), absence of macrovascular disease or stage 3b renal impairment (eGFR <45 ml/min/1.73 m2) or active proliferative retinopathy, as the ‘treatment group’ (TG). Nine matched type 1 diabetes patients were recruited as a standard group (SG). Both, TG and SG did not have any new intervention during the trial except for metformin in TG. Patients with suspected hypoglycemia unawareness were excluded. The study protocol (Fig. 1) included a run-in phase of 6 weeks to ensure stable glucose control. Following this period metformin was given for 8 weeks to TG with a dose titrated up to a maximum of 1 g twice a day over 2–3 weeks or to highest tolerated dose. The SG underwent similar follow-up except for metformin treatment. Furthermore, the TG was compared with 23 age- and gender-matched non-diabetic healthy controls (HC). All subjects gave their written informed consent and the Local Ethics Committee approved the study. Patients with type 1 diabetes were recruited either from, Queen Elizabeth Hospital, Gateshead or Royal Victoria Infirmary, Newcastle, UK. Healthy controls were recruited from the staff from the above or students from Newcastle University, UK.
Routine laboratory investigations (full blood count, U&Es, liver function test, thyroid function test, and HbA1c), 12-lead ECG, blood pressure, weight, height and BMI were performed at baseline and at the end of the study.
We aimed for unchanged glycaemic control during the study, which was assessed by HbA1c (four times points over 14 weeks) and continuous glucose monitoring (CGM) (Ipro2- Medtronic) (minimum of 48 h) was performed in those receiving metformin to ensure unchanged glycemic control. EasyGV Version 8.8.2. R2 was used to calculate glucose variability index [34].
Peripheral EDTA blood samples were collected before and after the study from TG and SG and at baseline from HC.
Endothelial progenitor cells
Flow cytometric evaluation of circulating endothelial progenitor cells (cEPCs) and circulating endothelial cells (cECs)
100 µl of whole blood [6] was incubated with 5 µl of V500 CD45 (B.D Bioscience), 20 µl of PerCP-Cy5.5 CD34 (BD Bioscience), 5 µl of PE VEGFR-2+ (R&D), 5 µl APC CD133 (Miltenyi Biotec USA), 10 µl of FITC CD144 for 30 min. Subsequently, 2 mls of pharmlyse (BD Bioscience) was used to lyse the red cells. The sample was then analysed by flow cytometry on BD FACS Canto™ II system and results by using BD FACSDiva™ software. On average 450,000 events were counted. cEPCs were defined as CD45dimCD34+VEGFR-2+ cells and cECs as CD45dim, CD133−, CD34+, and CD144+ events. cEPC count was expressed as % leukocytes (Intra-assay variation <8 %) and cECs as per ml of blood.
In-vitro assays
Methods for each of in vitro assay are described in details in Additional file 1. Assays described are: (1) enumeration of proangiogenic cells (PACs); (2) Colony forming units (CFU-Hills’ colonies; and (3) PAC function: fibronectin adhesion assay.
Statistical analysis
The results are expressed as mean ± SD unless stated otherwise. Within group (treatment or standard) comparison was evaluated by paired Student t test or Wilcoxon Signed Rank test depending on the distribution. Between-groups, comparison was by unpaired Student t test or the Mann–Whitney test. Correlation between different parameters were calculated by Pearson correlation or Spearman’s rho analysis. Multivariate regression analysis of delta changes in parameters were used to determine if independent metabolic variables predicted an improvement in cEPCs, PACs, CFU-Hill’s colonies, cECs and PACs function. One-way ANOVA was used to analyse the difference between HbA1c values. Adjustment for multiple comparisons was made by using the Bonferroni correction. Statistical significance was accepted at p < 0.05 (two-tailed significance).
As the aim of the study was to assess the effect of metformin on cEPCs in type 1 diabetes, therefore, statistical power calculation was undertaken only for the TG. Based on our pilot work and in order to reduce CVD risk in patients with type 1 diabetes, we aimed to detect a difference of 0.0021 in cEPCs (% leukocytes) in the treatment group (before and after metformin treatment), with α = 0.05 and a power of 90 %, a minimum of 20 patients were required. SPSS v21.0 (SPSS Inc, Ill) was used to perform statistical analysis.
Results
Clinical characteristics
Baseline characteristics of three groups are shown in Table 1. All groups were well matched for age, gender and blood pressure. TG and SG had a similar duration of diabetes (DOD), HbA1c, baseline insulin dose, lipid profile and creatinine. BMI was lower in SG in comparison to TG.
In TG, at recruitment twelve patients took aspirin and/or ACE inhibitor and/or statins in addition to insulin. No new medication other than metformin was started during the trial (except for metformin in the TG). No medication dosage was changed other than the dose of insulin and metformin. HC took no aspirin, ACE inhibitors and/or statins. Five patients in the SG took aspirin or/and ACE inhibitor and/or statins in addition to insulin. There was no difference in medication between TG and SG.
After treatment with metformin, BMI, total cholesterol, triglyceride, blood pressure and HbA1c remained unchanged. Over 14 weeks HbA1c values were as follows −6 week (56.4 ± 8.3 mmol/mol, 7.3 ± 3 %), 0 week (56.85 ± 10.5 mmol/mol, 7.3 ± 0.9 %), +6 week (56.8 ± 8.5 mmol/mol, 7.3 ± 0.8 %) and +8 week (56 ± 0.8 mmol/mol, 7.3 ± 0.8 %); one-way ANOVA, p = 0.78). The coefficient of variation of HbA1c over 14 weeks was 4.8 %. Furthermore, continuous glucose monitoring confirmed unchanged glucose control and variability (Average glucose CGM mmol/l: 9 ± 3 vs 8 ± 2.3, p = 0.17; blood glucose standard deviation: 3.3 ± 1.1 vs 3 ± 1.2, p = 0.3; mean amplitude of glycaemic excursion; 7 ± 2.7 vs 6 ± 3, p = 0.3; continuous overall net glycaemic action: 7.7 ± 2 vs 7.3 ± 2.2, p = 0.4; Total area under curve (AUC) (calculated): 12341 ± 2900 vs 11500 ± 3182, p = 0.3; AUC above limit-7.8 (CGM): 1.86 vs 1.97, p = 0.7. Insulin dose, HDL cholesterol and creatinine were significantly reduced in the TG treatment group after metformin treatment. There were no changes in any variables in SG.
Side effects
None of the volunteers in the study suffered any side effects requiring discontinuation of metformin. Fifteen patients took the full recommended dose of metformin (1000 mg BD). One patient took 500 mg BD due to low low eGFR (46 ml/min/1.73 m2). Five patients had gastrointestinal side effects that required dose reduction (two patients took 500 mg TDS; two took 500 mg BD, and one took 500 mg OD). No patient suffered any major or severe episode of hypoglycaemia. Major episode of hypoglycaemia was defined as any episode of low blood sugar requiring intervention of another person to resolve the event. Severe hypoglycaemia was defined as any episode of hypoglycaemia resulting in loss of consciousness. There was no significant effect of metformin on minor hypoglycaemic events (% ≤3.9 mmol/l and area under curve 3.9 mmol/l on CGMS: 8.6 % vs 13.3 %; p = 0.2 and 0.08 vs 0.1; p = 0.5 respectively).
Study biomarkers
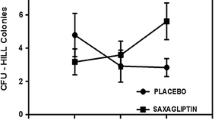
Figure 2 provides a comparison of cEPCs while Table 2 provides a comparison of cECs, PACs, CFU-Hill’s colonies and PACs adhesion function between the TG, SG and HC.
Circulating endothelial progenitor cells CD45dimCD34+ VEGFR-2+. Results given as per 100 leukocytes. TG V1 treatment group pre-metformin, TG V2 treatment group post-metformin, SG V1 standard group pre observation, SG V2 standard group post 8 weeks observation. Line denotes in each box as median and + in each box denotes mean value
Circulating endothelial progenitor cells
cEPCs count was similar in TG and the SG at baseline (p = 0.4). cEPCs (CD45dimCD34+VEGFR-2+) were significantly lower (60 %) in TG versus HC [Treatment group pre-metformin (TG V1 vs HC); median intraquartile range (IQ): 0.0028 (0.0016–0.006) vs 0.0068 (0.006–0.009) % leukocytes; p < 0.0005)]. Eight weeks metformin treatment significantly increased cEPCs in TG by more than 75 % and normalised the levels of cEPCs count when compared to HC [TG V1 vs TG V2 (Treatment group post metformin); median (IQ): 0.0028 (0.0016–0.006) vs 0.005 (0.0035–0.0085) % leukocytes; p = 0.002]. In SG 8 weeks of standard follow-up did not result in any change in cEPCs count [SG V1 vs SG V2: median (IQ): 0.0032 (0.002–0.004) vs 0.0035 (0.003–0.005) % leukocytes; p = 0.6]. Figure 3 provides before and after treatment plots for cEPC in TG.
Circulating endothelial cells
cECs number was similar in TG and SG at baseline. However, cECs were significantly higher (74 %) in TG versus HC. Metformin treatment led to a significantly reduction of cECs (36 %) in TG. Furthermore, metformin treatment normalised cECs numbers versus HC. cECs numbers did not change after eight-week follow-up in the SG.
Culture Assay for PACs and CFU-Hill’s colonies
PACs and CFU-Hill’s colonies numbers were similar in TG and the SG at baseline. PACs and CFU-Hill’s colonies counts were significantly lower (59 and 60 % respectively) in TG compared with HC. Eight weeks metformin treatment significantly increased PACs and CFU-Hill’s colonies in TG by 71 and 66 % respectively. Metformin treatment seemed to bring PACs and CFU-Hill’s colonies count closer to HC levels. After 8 weeks of follow-up in SG, the PACs and CFU-Hill’s colonies numbers remained unchanged.
PACs adhesion to fibronectin
The adhesion of PACs was similar in TG and SG at baseline. The adhesion of PACs in TG was 60 % lower when compared to HC. Metformin led to a significant increase (127 %), in PACs adhesion in TG and to the level seen in HC.
The PACs number remained unchanged after eight weeks of follow-up in SG.
Correlation
Univariate analysis in TG
In univariate analysis in TG, there was no correlation between changes in HbA1c, BMI, insulin dosage, total cholesterol, HDL cholesterol, LDL cholesterol, cEPCs, PACs, CFU-Hill’s colonies levels and PACs adhesion. There was an inverse correlation between changes in CFU-Hill’s colonies and cECs number (r = −0.6; p = 0.003) in TG. There was an inverse correlation between changes in PACs number and triglycerides (r = −0.6; p = 0.001) in TG.
Multivariate regression in TG
In multivariate regression analysis none of independent variables (changes in HbA1c, BMI, insulin dosage, LDL cholesterol) predicted changes in cEPCs, PACs number and function, CFU-Hill’s colonies and cECs.
Univariate and multivariate regression analysis are given in Additional file 1: Tables S1 and S2 respectively.
Discussion
In this study, we have demonstrated for the first time that in patients with relatively well controlled type 1 diabetes mellitus (mean HbA1c 7.3 or 56.4 mmol/mol), metformin therapy improved markers of vascular damage (cECs) and repair (cEPCs). We believe that this study may have positive clinical implication for patients with increased CVD risk by rebalancing the emphasis in their management from limiting damage alone to also improving vascular repair. Further evidence that our patients might benefit from metformin comes from the fact that CFU-Hill’s colonies, PACs number and adhesion properties improved significantly. It is well established that CFU-Hill's colonies number are inversely related to Framingham risk score. Therefore, CFU-Hill’s colonies are yet another predictor of CVD [21]. In addition, PACs adhesion function is an important factor in cEPCs homing, cell-cell contact and transmigration events for neovascularisation and vascular repair [35]. Metformin not only improved the level of cEPCs but also brought PACs number/adhesion and CFU-Hill’s colonies closer to the HC levels.
In addition, for the first time we have shown that in TG there was an inverse correlation between changes in cECs and CFU-Hills’ colonies. This shows that changes in markers of vascular/endothelial damage are linked inversely with a marker of CVD risk (CFU-Hill’s colonies).
The additional benefit suggested by our study for patients with type 1 diabetes is that the vascular health/repair may be improved in already well-controlled patients and without a need for further improvement in glycaemic control. Patients with type 1 diabetes are currently advised to achieve HbA1c <7 % or <54 mmol/mol in order to reduce CVD events. However, this is associated with inherent risk of experiencing hypoglycaemia. The recent work by the EURODIAB Prospective Complications Study has demonstrated a U shaped association between all-cause mortality and HbA1c. That is, all-cause mortality is highest at low (5.6 %; 37.7 mmol/l) and high (11.8 %; 105.5 mmol/mol) HbA1c [36]. Thus, an additional advantage of using metformin in type 1 diabetes suggested by our study is that markers of vascular health and repair may be improved without lowering blood glucose concentrations to a tightly control HbA1c level.
Metformin has been shown to improve cEPCs in type 2 diabetes [37]. However, there was a significant improvement in HbA1c. Thus, the change in cEPCs number could have been attributed to improved diabetic control. We have shown that the effect of metformin on all vascular biomarkers studied was beyond improving diabetic control. Indeed, HbA1c and glycaemic variability remained unchanged after 8 weeks of therapy. The glucose independent mechanism behind the metformin cardio-protective effect is of particular interest as this drug has some beneficial cardiac properties in non-diabetic animals [38]. When used in non-diabetic animals, metformin improved the outcome and revascularization following surgically induced myocardial infarction and hindlimb ischemia [38, 39]. Insulin dosage was reduced significantly, but it was not correlated with changes in cEPCs number or PACs adhesion. This is interesting, as insulin has been shown to improve cEPCs number [40, 41] and function in type 2 diabetes [42, 43]. However, the improvement in cEPCs number in Fadini et al. [41] could be attributed to improvement in HbA1c. This is in contrast with Humpert et al. [40], who showed that effect of insulin on the cEPCs number is independent of HbA1c. If the former was likely, given the reduction in insulin dosage in our study, cEPCs, PACs and CFU-Hill’s colonies number and PACs adhesion should have decreased, but this is not the case. This suggests that the insulin dose reduction did not have any effect on improving cEPCs or PACs function. Reduction in insulin dose had no effect on any variable including cEPCs in univariate or multivariate analysis.
cECs are recognised markers of vascular damage. Our study showed that metformin therapy improved the cECs count in type 1 diabetes and brought it closer to the matched HC. Even though cECs improved significantly, we believe that our study did not show the full effect of metformin on cECs, as some of our patients were using cardio-protective drugs already: statins and ACE inhibitors. Indeed, in TG subjects on ACE inhibitors and or statins less reduction of cECs was observed.
Eight weeks of metformin treatment did not result in any significant change or BMI. This is in contrast with a recent study which showed that 6 months of metformin in people with type 1 diabetes resulted in the loss of nearly 2.5 kg weight when compared to placebo [30]. However, we requested that patient would not aim to improve their diabetic control whilst in the study, so it is possible explanation for the lack of weight loss. Surprisingly, HDL cholesterol levels were reduced after metformin therapy, though, were similar to the control group and remained well within the normal range. However, there was no correlation between changes in cEPCs with BMI nor HDL cholesterol in univariate analysis. Thus, in our study it seems that BMI and HDL cholesterol are not responsible for metformin’s effect on the cEPCs number. This is in contrast with available evidence where HDL cholesterol has been shown to play a role in number EPCs and ischemia induced endothelial repair [44–46]. Furthermore, the multivariate analysis also showed that change in BMI was not a predictor of cEPCs either.
Our work can be supplemented further by understanding the mechanism through which metformin improves cEPC and cECs numbers. It is established that EPC differentiation and mobilization is impaired in diabetes mellitus patients [47]. Hyperglycaemia induces endothelial cell death via suppression of SIRT1. In-vitro work has shown metformin’s effect on improved cell survival (at physiological levels) although in mouse cells in high glucose levels (40 mM) by reducing premature senescence and apoptosis via increased SIRT expression/activity [48]. Metformin has been shown to promote SIRT 1 activity via AMPK pathway. This reduced the oxidative stress caused by hyperglycaemia in a dose-dependent manner [49]. Thus, we speculate that observed effect of metformin on cEPCs in our study may be due to improved cell survival, decreased senescence and/or increased recruitment from the bone marrow. Other beneficial effects of metformin have been achieved, although at very high unphysiological metformin levels only, such as activation of AMPK-mTOR and AMPK-eNOS-NO pathway [50].
EPC mobilisation can be increased via activation of eNOS pathway in diabetes mellitus [51]. Thereby, we can infer that activation of eNOS pathway can increase EPC mobilisation. However, this speculative and needs confirmation using metformin at physiological concentration. For that purpose, we have constructed an angiogenic model to study the mechanism of metformin at physiological concentration. In this experiment, metformin improved angiogenesis through increased angiogenic signal. It not only increased VEGF-A levels but also downregulated angiogenic inhibitors; CXCL-10 and TIMP-1 [52].
Our work can be meaningfully extended by addressing the limitations of our study. Although, there was a small number of patients in this study it was adequately powered. Our type 1 diabetes cohort was heterogeneous with a wide range of diabetes duration and age. This may seem to be a limitation but can also be seen as an advantage to improve generalisability of the results of our study. CGMS was done at the beginning and middle of the study and not at the end of the study. However, CGMS in the middle of the treatment phase was done at the maximum dose of tolerated metformin. Therefore, it is representative of metformin effect on blood glucose levels. We did not use randomised design nor long intervention (8 weeks only). As this research was designed as a proof of concept study exploring the effect of metformin on cEPCs and cECs, data generated from our work can be used to design randomised trials of longer duration in order to repurpose this widely used type 2 diabetes drug, for patients with type 1 diabetes [53]. Our work can be supplemented by exploring the effect of metformin treatment on endothelial function, inflammatory and adhesion markers.
Conclusions
In summary, our study has shown for the first time that metformin treatment may result in cardiovascular benefit by increasing markers of vascular repair or health (cEPCs, CFU-Hill's colonies, and PACs) and reducing markers of vascular damage (cECs). In a pivotal study by Werner et al. [19], higher levels of cEPCs lead to reduced CVD events. It appears that a 75 % rise in cEPCs number in type 1 diabetes patients as seen in our study might equate to the reclassification of our patients into a lower CVD risk group with approximate Hazard Ratio for CVD death of 0.77 thus 23 % reduction [19]. However, this needs to be confirmed by large randomised controlled trial examining cardiovascular events.
References
Soedamah-Muthu SS, Fuller JH, Mulnier HE, Raleigh VS, Lawrenson RA, Colhoun HM. High risk of cardiovascular disease in patients with type 1 diabetes in the U.K.: a cohort study using the general practice research database. Diabetes Care. 2006;29:798–804.
Livingstone SJ, Looker HC, Hothersall EJ, Wild SH, Lindsay RS, Chalmers J, Cleland S, Leese GP, McKnight J, Morris AD, et al. Risk of cardiovascular disease and total mortality in adults with type 1 diabetes: Scottish registry linkage study. PLoS Med. 2012;9:e1001321.
Livingstone SJ, Levin D, Looker HC, Lindsay RS, Wild SH, Joss N, Leese G, Leslie P, McCrimmon RJ, Metcalfe W, et al. Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008–2010. JAMA. 2015;313:37–44.
Snell-Bergeon JK, Maahs DM. Diabetes: Elevated risk of mortality in type 1 diabetes mellitus. Nat Rev Endocrinol. 2015;11:136–8.
Lind M, Svensson A-M, Kosiborod M, Gudbjörnsdottir S, Pivodic A, Wedel H, Dahlqvist S, Clements M, Rosengren A. Glycemic control and excess mortality in type 1 diabetes. New Engl J Med. 2014;371:1972–82.
Sibal L, Aldibbiat A, Agarwal SC, Mitchell G, Oates C, Razvi S, Weaver JU, Shaw JA, Home PD. Circulating endothelial progenitor cells, endothelial function, carotid intima-media thickness and circulating markers of endothelial dysfunction in people with type 1 diabetes without macrovascular disease or microalbuminuria. Diabetologia. 2009;52:1464–73.
Goon PK, Lip GY, Boos CJ, Stonelake PS, Blann AD. Circulating endothelial cells, endothelial progenitor cells, and endothelial microparticles in cancer. Neoplasia. 2006;8:79–88.
Burger D, Touyz RM. Cellular biomarkers of endothelial health: microparticles, endothelial progenitor cells, and circulating endothelial cells. J Am Soc Hypertens. 2012;6:85–99.
Asicioglu E. Gogas Yavuz D, Koc M, Ozben B, Yazici D, Deyneli O, Akalin S: Circulating endothelial cells are elevated in patients with type 1 diabetes mellitus. Eur J Endocrinol. 2010;162:711–7.
McClung JA, Naseer N, Saleem M, Rossi GP, Weiss MB, Abraham NG, Kappas A. Circulating endothelial cells are elevated in patients with type 2 diabetes mellitus independently of HbA(1)c. Diabetologia. 2005;48:345–50.
Koc M, Richards HB, Bihorac A, Ross EA, Schold JD, Segal MS. Circulating endothelial cells are associated with future vascular events in hemodialysis patients. Kidney Int. 2005;67:1078–83.
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–7.
Urbich C, Dimmeler S. Endothelial progenitor cells functional characterization. Trends Cardiovasc Med. 2004;14:318–22.
Timmermans F, Plum J, Yöder MC, Ingram DA, Vandekerckhove B, Case J. Endothelial progenitor cells: identity defined? J Cell Mol Med. 2009;13:87–102.
Yoder MC. Human endothelial progenitor cells. In: Cold Spring Harb Perspect Med, vol. 2; 2012.
Hristov M, Erl W, Weber PC. Endothelial progenitor cells: mobilization, differentiation, and homing. Arterioscler Thromb Vasc Biol. 2003;23:1185–9.
Collet G, Lamerant-Fayel N, Tertil M, El Hafny-Rahbi B, Stepniewski J, Guichard A, Foucault-Collet A, Klimkiewicz K, Petoud S, Matejuk A, et al. Hypoxia-regulated overexpression of soluble VEGFR2 controls angiogenesis and inhibits tumor growth. Mol Cancer Ther. 2014;13:165–78.
Rigato M, Bittante C, Albiero M, Avogaro A, Fadini GP. Circulating progenitor cell count predicts microvascular outcomes in type 2 diabetic patients. J Clin Endocrinol Metab. 2015;100:2666–72.
Werner N, Kosiol S, Schiegl T, Ahlers P, Walenta K, Link A, Bohm M, Nickenig G. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005;353:999–1007.
Hörtenhuber T, Rami-Mehar B, Satler M, Nagl K, Höbaus C, Höllerl F, Koppensteiner R, Schernthaner G, Schober E, Schernthaner G-H. Endothelial progenitor cells are related to glycemic control in children with type 1 diabetes over time. Diabetes Care. 2013;36:1647–53.
Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, Finkel T. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348:593–600.
Tepper OM, Galiano RD, Capla JM, Kalka C, Gagne PJ, Jacobowitz GR, Levine JP, Gurtner GC. Human endothelial progenitor cells from type II diabetics exhibit impaired proliferation, adhesion, and incorporation into vascular structures. Circulation. 2002;106:2781–6.
Loomans CJ, de Koning EJ, Staal FJ, Rookmaaker MB, Verseyden C, de Boer HC, Verhaar MC, Braam B, Rabelink TJ, van Zonneveld AJ. Endothelial progenitor cell dysfunction: a novel concept in the pathogenesis of vascular complications of type 1 diabetes. Diabetes. 2004;53:195–9.
Fadini GP, Miorin M, Facco M, Bonamico S, Baesso I, Grego F, Menegolo M, de Kreutzenberg SV, Tiengo A, Agostini C, Avogaro A. Circulating endothelial progenitor cells are reduced in peripheral vascular complications of type 2 diabetes mellitus. J Am Coll Cardiol. 2005;45:1449–57.
Dessapt C, Karalliedde J, Hernandez-Fuentes M, Prieto PM, Maltese G, Dattani N, Atkar R, Viberti G, Gnudi L. Circulating vascular progenitor cells in patients with type 1 diabetes and microalbuminuria. Diabetes Care. 2010;33:875–7.
Nauta ST, Deckers JW, Akkerhuis KM, van Domburg RT. Short- and long-term mortality after myocardial infarction in patients with and without diabetes: changes from 1985 to 2008. Diabetes Care. 2012;35:2043–7.
Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998; 352:854–865.
Fung CS, Wan EY, Wong CK, Jiao F, Chan AK. Effect of metformin monotherapy on cardiovascular diseases and mortality: a retrospective cohort study on Chinese type 2 diabetes mellitus patients. Cardiovasc Diabetol. 2015;14:137.
Lexis CH, Wieringa W, Hiemstra B, van Deursen V, Lipsic E, van der Harst P, van Veldhuisen D, van der Horst IC. Chronic metformin treatment is associated with reduced myocardial infarct size in diabetic patients with st-segment elevation myocardial infarction. Cardiovasc Drugs Ther. 2014;28:163–71.
Pitocco D, Zaccardi F, Tarzia P, Milo M, Scavone G, Rizzo P, Pagliaccia F, Nerla R, Di Franco A, Manto A, et al. Metformin improves endothelial function in type 1 diabetic subjects: a pilot, placebo-controlled randomized study. Diabetes Obes Metab. 2013;15:427–31.
Eriksson L, Nyström T. Activation of AMP-activated protein kinase by metformin protects human coronary artery endothelial cells against diabetic lipoapoptosis. Cardiovasc Diabetol. 2014;13:152.
Lexis CH, van der Horst IC, Lipsic E, et al. Effect of metformin on left ventricular function after acute myocardial infarction in patients without diabetes: the gips-iii randomized clinical trial. JAMA. 2014;311:1526–35.
Elmessaoudi S, Nederlof R, Zuurbier CJ, van Swieten HA, Pickkers P, Noyez L, Dieker HJ, Coenen MJ, Donders ART, Vos A, et al. Effect of metformin pretreatment on myocardial injury during coronary artery bypass surgery in patients without diabetes (MetCAB): a double-blind, randomised controlled trial. Lancet Diabetes Endocrinol. 2014;3:615–23.
Hill NR, Oliver NS, Choudhary P, Levy JC, Hindmarsh P, Matthews DR. Normal reference range for mean tissue glucose and glycemic variability derived from continuous glucose monitoring for subjects without diabetes in different ethnic groups. Diabetes Technol Ther. 2011;13:921–8.
Urbich C, Dimmeler S. Endothelial progenitor cells: characterization and role in vascular biology. Circ Res. 2004;95:343–53.
Schoenaker DAJM, Simon D, Chaturvedi N, Fuller JH, Soedamah-Muthu SS. Glycemic control and all-cause mortality risk in type 1 diabetes patients: the EURODIAB prospective complications study. J Clin Endocrinol Metab. 2014;99:800–7.
Chen LL, Liao YF, Zeng TS, Yu F, Li HQ, Feng Y. Effects of metformin plus gliclazide compared with metformin alone on circulating endothelial progenitor cell in type 2 diabetic patients. Endocrine. 2010;38:266–75.
Gundewar S, Calvert JW, Jha S, Toedt-Pingel I, Ji SY, Nunez D, Ramachandran A, Anaya-Cisneros M, Tian R, Lefer DJ. Activation of AMP-activated protein kinase by metformin improves left ventricular function and survival in heart failure. Circ Res. 2009;104:403–11.
Takahashi N, Shibata R, Ouchi N, Sugimoto M, Murohara T, Komori K. Metformin stimulates ischemia-induced revascularization through an eNOS dependent pathway in the ischemic hindlimb mice model. J Vasc Surg. 2015;61:489–96.
Humpert PM, Neuwirth R, Battista MJ, Voronko O, von Eynatten M, Konrade I, Rudofsky G, Wendt T, Hamann A, Morcos M, et al. SDF-1 genotype influences insulin-dependent mobilization of adult progenitor cells in type 2 diabetes. Diabetes Care. 2005;28:934–6.
Fadini GP, de Kreutzenberg SV, Mariano V, Boscaro E, Bertolini F, Mancuso P, Quarna J, Marescotti M, Agostini C, Tiengo A, Avogaro A. Optimized glycaemic control achieved with add-on basal insulin therapy improves indexes of endothelial damage and regeneration in type 2 diabetic patients with macroangiopathy: a randomized crossover trial comparing detemir versus glargine. Diabetes Obes Metab. 2011;13:718–25.
Humpert PM, Djuric Z, Zeuge U, Oikonomou D, Seregin Y, Laine K, Eckstein V, Nawroth PP, Bierhaus A. Insulin Stimulates the Clonogenic Potential of Angiogenic Endothelial Progenitor Cells by IGF-1 Receptor-Dependent Signaling. Mol Med. 2008;14:301–8.
Oikonomou D, Kopf S, von Bauer R, Djuric Z, Cebola R, Sander A, Englert S, Vittas S, Hidmark A, Morcos M, et al. Influence of insulin and glargine on outgrowth and number of circulating endothelial progenitor cells in type 2 diabetes patients: a partially double-blind, randomized, three-arm unicenter study. Cardiovasc Diabetol. 2014;13:137.
OvO Verhaar, Nieuwdorp M, Westerweel PE, Hoefer IE, Basser P, Stroes ESG. Reconstituted HDL increases circulating endothelial progenitor cells in patients with type 2 diabetes. Arterioscler Thromb Vasc Biol. 2007;27:1864.
Nagai MS, Masataka S, Shin-ichiro M, Kerry-Anne R, Naoki T, Yuji K, Katsuhiko Y, Takao O, Keijiro S. Ryozo: Reconstituted high-density lipoprotein stimulates differentiation of endothelial progenitor cells and enhances ischemia-induced angiogenesis. Arterioscler Thromb Vasc Biol. 2007;27:813.
Rossi F, Bertone C, Montanile F, Miglietta F, Lubrano C, Gandini L, Santiemma V. HDL cholesterol is a strong determinant of endothelial progenitor cells in hypercholesterolemic subjects. Microvasc Res. 2010;80:274–9.
Avogaro GPF, Mattia A, Saulavigilide K, Elisa B, Roberta C, Mariacristina M, Nicol P, Carlo A. Diabetes impairs stem cell and proangiogenic cell mobilization in humans. Diabetes Care. 2013;36:943.
Arunachalam G, Samuel SM, Marei I, Ding H, Triggle CR. Metformin modulates hyperglycaemia-induced endothelial senescence and apoptosis through SIRT1. Br J Pharmacol. 2014;171:523–35.
Xu ZZ, Haibing C, Jun L, Tao L, Bingqing Z, Ying Z, Huiyi J, Ying H, Qing G. Sirtuin 1-mediated cellular metabolic memory of high glucose via the LKB1/AMPK/ROS pathway and therapeutic effects of metformin. Diabetes. 2012;61:217.
Li WD, Du XL, Qian AM, Hu N, Kong LS, Wei S, Li CL, Li XQ. Metformin regulates differentiation of bone marrow-derived endothelial progenitor cells via multiple mechanisms. Biochem Biophys Res Commun. 2015;465:803–9.
Lu A, Wang L, Qian L. The role of eNOS in the migration and proliferation of bone-marrow derived endothelial progenitor cells and in vitro angiogenesis. Cell Biol Int. 2015;39:484–90.
Bakhashab S, Ahmed FW, Schulten H-J, Bashir A, Karim S, Al-Malki AL, Gari MA, Abuzenadah AM, Chaudhary AG, Alqahtani MH, et al. Metformin improves the angiogenic potential of human CD34+ cells co-incident with downregulating CXCL10 and TIMP1 gene expression and increasing VEGFA under hyperglycemia and hypoxia within a therapeutic window for myocardial infarction. Cardiovasc Diabetol. 2016;15:1–12.
Bromage DI, Yellon DM. The pleiotropic effects of metformin: time for prospective studies. Cardiovasc Diabetol. 2015;14:109.
Authors’ contributions
FWA recruitment and follow up of patients, laboratory experiments, acquisition of data, analysis and interpretation of the data and drafting of manuscript. RR follow up of patients and advising patients on adjusting insulin therapy. MG support in laboratory experiment. SR recruitment of patients and drafting of manuscript. KN recruitment of patients and drafting of manuscript. JUW conception and design of the study, securing the funding, recruitment of patients, laboratory experiments, acquisition of data, analysis and interpretation of the data and drafting of manuscript. JUW is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Acknowledgements
We thank Professor I Spyridopoulos for helpful discussions at the conception of the study, Medtronic Diabetes UK for providing Ipro2 for continuous glucose monitoring. We thank Clinical Research Facility and its staff in Royal Victoria Infirmary, Newcastle for use of the facility.
Competing interests
The authors declare that they have no competing interests.
Ethics approval
NRES Committee North East—Sunderland: REC reference number: 12/NE/0044.
Funding
Diabetes Research and Wellness Foundation and Diabetes Research Fund in Gateshead.
Author information
Authors and Affiliations
Corresponding author
Additional file
12933_2016_413_MOESM1_ESM.docx
Additional file 1: Table S1. Correlation matrix of associations between the changes in cEPCs, PACs, PAC adhesion, CFU-Hill colonies and CECs in treatment group. Table S2. The univariate and multivariate relationship between changes in cEPC, PACs, CFU-Hill Colonies, CECs and PAC adhesion to changes in other metabolic markers.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ahmed, F.W., Rider, R., Glanville, M. et al. Metformin improves circulating endothelial cells and endothelial progenitor cells in type 1 diabetes: MERIT study. Cardiovasc Diabetol 15, 116 (2016). https://doi.org/10.1186/s12933-016-0413-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-016-0413-6