Abstract
Background
Abdominal visceral obesity has been reported to be associated with cardiovascular risks than body mass index, waist circumference, and abdominal subcutaneous fat. On the other hand, there is evidence that subcutaneous fat has a beneficial role against cardio-metabolic risks such as diabetes or dyslipidemia. However, little is known regarding the association between high visceral fat with low subcutaneous fat accumulation and the risk for atherosclerosis.
Methods
This study was designed to elucidate whether high visceral fat with low subcutaneous fat accumulation enhances the risk for atherosclerosis in patients with type 2 diabetes. This is a cross-sectional study of 148 patients with type 2 diabetes (mean age 65 ± 12 years; 44.5 % female). Visceral fat area (VFA, cm2) and subcutaneous fat area (SFA, cm2) were assessed by abdominal computed tomography. Carotid intima media thickness (CIMT, mm) measured by ultrasonography was used for the assessment of atherosclerosis. Patients were divided into four groups: SFA < 100 cm2 and VFA < 100 cm2 [S(−)V(−)], SFA ≥ 100 cm2 and VFA < 100 cm2 [S(+)V(−)], SFA < 100 cm2 and VFA ≥ 100 cm2 [S(−)V(+)], and SFA ≥ 100 cm2 and VFA ≥ 100 cm2 [S(+)V(+)]. Linear regression analysis with a stepwise procedure was used for the statistical analyses.
Results
Among the patients examined, 16.3 % were S(−)V(+). Mean (95 % confidence interval) of CIMT adjusting for age and gender were 0.80 (0.69–0.91), 0.86 (0.72–1.01), 1.28 (1.11–1.44) and 0.83 (0.77–0.88) in patients with S(−)V(−), S(+)V(−), S(−)V(+) and S(+)V(+), respectively (p < 0.001). The S(−)V(+) patients exhibited significantly older than S(−)V(−) patients and those with S(+)V(+) and had a highest VFA-SFA ratio (V/S ratio) among the four groups. S(−)V(+) patients were male predominant (100 % male), and S(+)V(−) patients showed female predominance (82 % female). In multivariate linear regression analysis (Adjusted R2 = 0.549), S(−)V(+) was significantly associated with CIMT (Standardized β 0.423, p < 0.001). Notably, S(+)V(+) was inversely associated with CIMT in the multivariate model.
Conclusions
This study provides evidence that high visceral fat with low subcutaneous fat accumulation is an important determinant of carotid atherosclerosis and high subcutaneous fat could be protective against atherosclerosis in patients with type 2 diabetes.
Similar content being viewed by others
Background
Obesity has been reported to be associated with insulin resistance, dyslipidemia, and hypertension, thus increasing the risk for cardiovascular disease (CVD) [1–4]. Regarding body fat distribution, abdominal visceral fat has been more strongly associated with cardiovascular risks than body mass index (BMI), waist circumference, and abdominal subcutaneous fat [5, 6]. Therefore, evaluation and management of visceral fat accumulation is important to reduce cardio-metabolic burdens. Recently, we have reported that increased visceral fat with normal BMI is associated with arterial stiffening in patients with type 2 diabetes [7]. On the other hand, there is evidence that subcutaneous fat has a beneficial role against cardio-metabolic risks such as diabetes or dyslipidemia [8, 9]. These observations suggest the importance of direct evaluation of visceral and subcutaneous fat accumulation for the management of atherosclerosis; therefore it is possible that increased visceral fat with decreased subcutaneous fat accumulation is positively associated with atherosclerosis. Here we investigated the impact of body fat distribution, i.e. increased visceral fat with decreased subcutaneous fat accumulation, on carotid atherosclerosis in Japanese patients with type 2 diabetes.
Methods
Subjects
Patients with type 2 diabetes who regularly visited Tokyo Medical and Dental University Hospital participated in this study. Patients were eligible, if they were aged ≥20 years, and 148 consequential patients who underwent abdominal computed tomography (CT) for the assessment of visceral and subcutaneous fat accumulation were enrolled. Patients with severe renal impairment [estimated glomerular filtration rate (eGFR) <15 mL/min/1.73 m2 or undergoing renal replacement therapy], pregnant women, and those with infectious or malignant diseases were excluded. Type 2 diabetes was diagnosed according to the criteria of the Japan Diabetes Society (JDS) [10]. This study complies with the principles laid by Declaration of Helsinki and has been approved by the ethical committee of Tokyo Medical and Dental University (No. 2103).
Clinical and biochemical analysis
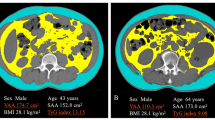
Visceral fat area (VFA) and subcutaneous fat area (SFA) were measured at the level of umbilicus by abdominal CT examination (Aquilion PRIME, Toshiba Medical Systems, Tochigi, Japan). Atherosclerosis was assessed by carotid intima media thickness (CIMT) using an echotomographic system (Aplio XG SSA790A, Toshiba Medical Systems, Tochigi, Japan) with a 7.5-MHz linear transducer, as reported previously [11]. Following the criteria of visceral fat obesity as recommended by the Japan Society for the Study of Obesity [12], we defined visceral and subcutaneous fat accumulation; they were classified into four groups as follows: SFA < 100 cm2 and VFA < 100 cm2 [S(−)V(−)], SFA ≥ 100 cm2 and VFA < 100 cm2 [S(+)V(−)], SFA < 100 cm2 and VFA ≥ 100 cm2 [S(−)V(+)] and SFA ≥ 100 cm2 and VFA ≥ 100 cm2 [S(+)V(+)].
Statistical analysis
Statistical analysis was performed using programs available in the SPSS version 21.0 statistical package (SPSS Inc., Chicago, IL, USA). Data are presented as mean ± SD or geometric mean with 95 % confidence interval (CI) as appropriate according to data distribution. Differences among the four groups were tested with a one-way ANOVA (continuous variables) or Chi square test (categorical variables) followed by Tukey–Kramer methods for the post hoc analyses. Linear regression analysis with a stepwise procedure was used to assess the cross-sectional association of each manifestation of abdominal (VFA) and subcutaneous (SFA) fat accumulation with carotid atherosclerosis. The following covariates were incorporated into the analysis; age, gender, duration of diabetes, smoking status, systolic blood pressure, triglycerides, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, HbA1c, urinary albumin-to-creatinine ratio (ACR), eGFR, and the use of insulin, the use of calcium channel blockers (CCBs), angiotensin-converting enzyme inhibitors, angiotensin receptor blockers (ARBs), statins, and anti-platelet agents. We also underwent a sensitivity analysis to examine the association of VFA and SFA with CIMT, using the cutoff of 100 and 150 cm2 in VFA and SFA, respectively, because the average of SFA in this study was approximately 150 cm2. Differences were considered to be statistically significant at p value less than 0.05.
Results
A total of 148 Japanese patients with type 2 diabetes (mean age 65 ± 12 years; 44.5 % female) were enrolled in this study. Among the participants, 16.3 % (N = 11) were classified as S(−)V(+), and 23.0 % (N = 34), 26.4 % (N = 39) and 43.2 % (N = 64) were classified as S(−)V(−), S(+)V(−), and S(+)V(+), respectively (Fig. 1). As shown in Table 1, S(−)V(+) patients were older than S(−)V(−) patients (p = 0.004) and S(+)V(+) (p = 0.036), and had a significantly higher VFA-SFA ratio (V/S ratio) than S(−)V(−) (p < 0.001), S(+)V(−) (p < 0.001), and S(+)V(+) patients (p < 0.001). Systolic blood pressure in S(−)V(+) patients were significantly higher than S(−)V(−) (p < 0.001) and S(+)V(−) patients (p < 0.001). Interestingly, there were appreciable differences in gender and fat distribution between S(−)V(+) and S(+)V(−) patients, without a significant difference in BMI. In this study, S(−)V(+) patients were male predominant (100 % male), and S(+)V(−) patients showed female predominance (82 % female). Moreover, S(−)V(+) patients had significantly higher uric acid (p < 0.001) and glutamyl transpeptidase (γ-GTP) (p < 0.001) levels than S(+)V(−) patients. The S(−)V(+) patients had reached the maximum BMI at younger age (43 ± 12 years) than S(+)V(−) patients (47 ± 11 years) and S(+)V(+) patients (51 ± 13 years). The maximum BMI in S(−)V(+) patients was significantly lower than that S(+)V(−) and S(+)V(+) patients (data not shown). Medications were listed in Table 2. None of S(−)V(+) patients received biguanides nor statins, although S(−)V(+) patients showed increased visceral fat accumulation. The number of S(+)V(+) patients taking biguanides and statins was greater than those of S(−)V(−), S(+)V(−), and S(+)V(+) patients.
As expected, S(−)V(+) patients had the highest CIMT level among the four groups [vs. S(−)V(−) (p < 0.001), vs. S(+)V(−) (p < 0.001), vs. S(+)V(+) (p < 0.001)] (Table 1). After adjustment for age and gender, mean (95 % CI) of CIMT were 0.80 (0.69–0.91), 0.86 (0.72–1.01), 1.28 (1.11–1.44) and 0.83 (0.77–0.88) in patients with S(−)V(−), S(+)V(−), S(−)V(+) and S(+)V(+), respectively (p < 0.001). On the other hand, CIMT level in S(+)V(+) patients was roughly equivalent to those in S(−)V(−) and S(+)V(−) patients. In the univariate analysis, S(−)V(+) was significantly associated with CIMT (standardized β 0.531, p < 0.001); whereas S(+)V(−) and S(+)V(+) were not associated with CIMT (Table 3). In the multivariate analysis, S(−)V(+) remained to be significantly associated with the risk for CIMT (standardized β 0.423, p < 0.001). Adjusted R2 was 0.549 in the model. Notably, S(+)V(+) was inversely associated with CIMT in the multivariate model. Using V/S ratio as the indicator for balance of visceral and subcutaneous fat accumulation, we also examined whether increased visceral fat relative to subcutaneous fat is continuously associated with CIMT. In this study, V/S ratio showed significantly positive correlations with CIMT in both univariate (Standardized β 0.506, p < 0.001) and multivariate linear regression analyses (Standardized β 0.383, p < 0.001). We finally underwent a sensitivity analysis using the cutoff of 150 cm2 for SFA because the average of SFA in this study was approximately 150 cm2. In the multivariate linear regression analysis, the association between SFA < 150 cm2 and VFA ≥ 100 cm2 and CIMT as compared with SFA < 150 cm2 and VFA < 100 cm2 reached a marginal statistical significance (Standardized β 0.190, p = 0.051); whereas, patients with SFA ≥ 150 cm2 and VFA ≥ 100 cm2 were not significantly increased risk for CIMT.
Discussion
Here, we demonstrate that S(−)V(+) patients are at an significantly increased risk for carotid atherosclerosis among Japanese patients with type 2 diabetes. Moreover, in multivariate analyses, there was a direct relationship between the presence of S(−)V(+) and risk for atherosclerosis and an inverse relationship between the presence of S(+)V(+) and risk for CIMT.
The association between body fat accumulation and atherosclerosis
Visceral adipose tissue has been recently reported to be associated with coronary plaque characteristics in patients without diabetes [13] and visceral adipose tissue is a stronger risk factor of carotid atherosclerosis in Chinese adults [14]. Therefore, our data support the notion that visceral fat accumulation is positively associated with atherosclerosis. By contrast, Ravussin and Smith [15, 16] proposed the possibility that the ability to retain fat in subcutaneous depot is beneficial against cardio-metabolic risks. In addition, a more recent study clearly revealed that subcutaneous adipose thickness assessed by ultrasonography is inversely associated with carotid atherosclerosis in patients with type 2 diabetes [17]. These observations taken together, suggest that body fat distribution should be evaluated with information on visceral and subcutaneous fat accumulation for the assessment of the risks for atherosclerosis.
Possible factors associated with fat distribution and atherosclerosis
In this study, S(−)V(+) patients were elderly men with severe cardio-metabolic profiles, including elevated blood pressure and uric acid, and high V/S ratio. These observations may partly explain the progression of atherosclerosis in S(−)V(+) patients. In addition, S(−)V(+) patients had reached maximum BMI at younger age than S(+)V(−) and S(+)V(+) patients. The maximum BMI in S(−)V(+) patients was low relative to S(+)V(−) and S(+)V(+) patients. It is interesting to speculate that S(−)V(+) patients have lower capacity to store excess energy in subcutaneous fat depot than S(+)V(−) and S(+)V(+) patients. Then, what could affect body fat distribution? A recent large scale cross-sectional study demonstrated that abdominal adiposity is positively associated with a deteriorated cardio-metabolic risk profile in multi-ethnicities and that East Asians have the highest visceral relative to subcutaneous fat accumulation among whites, African Caribbean blacks, Hispanics, East Asians, and Southeast Asians [18]. The Japanese men are likely to have a greater percent body fat than Australian men at any given BMI values [19]. Gender is also an important determinant of body fat distribution. Indeed, a genome-wide association study meta-analysis showed sexual dimorphism in the genetic regulation of fat distribution traits [20]. In this study, there was a clear gender difference in body fat distribution, with male predominance in S(−)V(+) and female predominance in S(+)V(−). It has been observed that high fat stores in ectopic fat compartments including skeletal muscle are present in male patients newly diagnosed with type 2 diabetes and altered lipid partitioning within muscle is independently associated with carotid atherosclerosis [21]. Després has recently proposed the lipid overflow-ectopic fat model [22]. If the extra energy is channeled into insulin-sensitive subcutaneous adipose tissue, the subjects will be protective against the development of the metabolic syndrome; whereas, in cases where the adipose tissue has a limited ability to store the excess energy into subcutaneous adipose tissue, triglycerides surplus will be deposited at undesirable sites such as skeletal muscle and visceral adipose tissue, leading the insulin resistance, atherogenic dyslipidemia, and atherosclerosis. Therefore, it is possible that low capacity of subcutaneous fat accumulation in patients with S(−)V(+) could allow ectopic fat accumulation within muscle as well as visceral fat accumulation, consequently leading to increased risk for carotid atherosclerosis. It remains to be determined whether the association observed between S(−)V(+) and atherosclerosis in Japanese subjects with type 2 diabetes will also be observed in other populations.
Limitations
There are a couple of limitations in this study. First, it is impossible to infer causality because of its cross-sectional design. Second, we evaluated visceral fat and subcutaneous fat accumulation using VFA and SFA at the level of umbilicus; therefore, fat accumulation in other fat depots such as thighs and legs were not evaluated. Third, population in this study was ethnically and socially homogeneous, because this study was hospital-based; therefore, generalization of our findings might be limited. Fourth, we were unable to obtain information on diet and exercise in this study. These lifestyle could affect the distribution of body fat and BMI levels and could be one of the variables that is accounting for this high risk of CIMT in patients with S(−)V(+). Finally, it is important to undergo the sub-analyses to investigate the association of VFA and SFA accumulation with CIMT in different age groups, gender, and metabolic status; however, we could not undergo the analyses due to the relatively small sample size.
Conclusions
It is of primary importance to identify diabetic patients who have advanced atherosclerosis because they are at extremely increased risk for CVD [23, 24]. Our data suggest that imbalance of visceral and subcutaneous fat distribution, i.e. increased visceral fat with decreased subcutaneous fat accumulation, is an important determinant of atherosclerosis, whereas increased subcutaneous fat accumulation could buffer the deleterious effect of visceral fat accumulation in patients with type 2 diabetes.
Abbreviations
- ACEI:
-
angiotensin-converting enzyme inhibitor
- ACR:
-
albumin-to-creatinine ratio
- ALT:
-
alanine aminotransferase
- ARB:
-
angiotensin receptor blocker
- AST:
-
asparatate aminotransferase
- BMI:
-
body mass index
- CCBs:
-
calcium channel blockers
- CI:
-
confidence interval
- CIMT:
-
carotid intima media thickness
- CT:
-
computed tomography
- CVD:
-
cardiovascular disease
- DBP:
-
diastolic blood pressure
- DPP4:
-
dipeptidyl peptidase-4
- eGFR:
-
estimated glomerular filtration rate
- GI:
-
glycosidase inhibitor
- GLP-1:
-
glucagon-like peptide-1
- GTP:
-
glutamyl transpeptidase
- HDL:
-
high-density lipoprotein
- JDS:
-
Japan Diabetes Society
- LDL:
-
low-density lipoprotein
- OHA:
-
oral hypoglycemic agent
- PDR:
-
proliferative diabetic retinopathy
- SBP:
-
systolic blood pressure
- SFA:
-
subcutaneous fat area
- TZD:
-
thiazolidinedione
- UA:
-
uric acid
- VFA:
-
visceral fat area
References
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, Lang CC, Rumboldt Z, Onen CL, Lisheng L, INTERHEART Study Investigators, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–9.
Fujimoto WY, Bergstrom RW, Boyko EJ, Chen KW, Leonetti DL, Newell-Morris L, Shofer JB, Wahl PW. Visceral adiposity and incident coronary heart disease in Japanese-American men. The 10-year follow-up results of the Seattle Japanese-American Community Diabetes Study. Diabetes Care. 1999;22:1808–12.
Britton KA, Massaro JM, Murabito JM, Kreger BE, Hoffmann U, Fox CS. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol. 2013;62:921–5.
Kanai H, Matsuzawa Y, Kotani K, Keno Y, Kobatake T, Nagai Y, Fujioka S, Tokunaga K, Tarui S. Close correlation of intra-abdominal fat accumulation to hypertension in obese women. Hypertension. 1990;16:484–90.
Després JP, Lemieux S, Lamarche B, Prud’homme D, Moorjani S, Brun LD, Gagné C, Lupien PJ. The insulin resistance-dyslipidemic syndrome: contribution of visceral obesity and therapeutic implications. Int J Obes Relat Metab Disord. 1995;19(Suppl 1):S76–86.
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007;116:39–48.
Bouchi R, Minami I, Ohara N, Nakano Y, Nishitani R, Murakami M, Takeuchi T, Akihisa M, Fukuda T, Fujita M, et al. Impact of increased visceral adiposity with normal weight on the progression of arterial stiffness in Japanese patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2015;3:e000081.
Snijder MB, Visser M, Dekker JM, Goodpaster BH, Harris TB, Kritchevsky SB, De Rekeneire N, Kanaya AM, Newman AB, Tylavsky FA, et al. Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. The Health ABC Study. Diabetologia. 2005;48:301–8.
Porter SA, Massaro JM, Hoffmann U, Vasan RS, O’Donnel CJ, Fox CS. Abdominal subcutaneous adipose tissue: a protective fat depot? Diabetes Care. 2009;32:1068–75.
Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Investig. 2010;1:212–28.
Ito H, Komatsu Y, Mifune M, Antoku S, Ishida H, Takeuchi Y, Togane M. The estimated GFR, but not the stage of diabetic nephropathy graded by the urinary albumin excretion, is associated with the carotid intima-media thickness in patients with type 2 diabetes mellitus: a cross-sectional study. Cardiovasc Diabetol. 2010;9:18.
Examination Committee of Criteria for ‘Obesity Disease’ in Japan. Japan Society for the Study of Obesity. Circ J. 2002;66:987–92.
Osawa K, Miyoshi T, Koyama Y, Sato S, Akagi N, Morimitsu Y, Kubo M, Sugiyama H, Nakamura K, Morita H, et al. Differential association of visceral adipose tissue with coronary plaque characteristics in patients with and without diabetes mellitus. Cardiovasc Diabetol. 2014;13:61.
Ren C, Zhang J, Xu Y, Xu B, Sun W, Sun J, Wang T, Xu M, Lu J, Wang W, et al. Association between carotid intima-media thickness and index of central fat distribution in middle-aged and elderly Chinese. Cardiovasc Diabetol. 2014;13:139.
Ravussin E, Smith SR. Increased fat intake, impaired fat oxidation, and failure of fat cell proliferation result in ectopic fat storage, insulin resistance, and type 2 diabetes mellitus. Ann N Y Acad Sci. 2002;967:363–78.
Yang X, Smith U. Adipose tissue distribution and risk of metabolic disease: does thiazolidinedione-induced adipose tissue redistribution provide a clue to the answer? Diabetologia. 2007;50:1127–39.
Jung CH, Kim BY, Kim KJ, Jung SH, Kim CH, Kang SK, Mok JO. Contribution of subcutaneous abdominal fat on ultrasonography to carotid atherosclerosis in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2014;13:67.
Nazare JA, Smith JD, Borel AL, Haffner SM, Balkau B, Ross R, Massien C, Alméras N, Després JP. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/Intra-Abdominal Adiposity. Am J Clin Nutr. 2012;96:714–26.
Kagawa M, Kerr D, Uchida H, Binns CW. Differences in the relationship between BMI and percentage body fat between Japanese and Australian-Caucasian young men. Br J Nutr. 2006;95:1002–7.
Shungin D, Winkler TW, Croteau-Chonka DC, Ferreira T, Locke AE, Mägi R, Strawbridge RJ, Pers TH, Fischer K, Justice AE, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518:187–96.
Kim SK, Park SW, Hwang IJ, Lee YK, Cho YW. High fat stores in ectopic compartments in men with newly diagnosed type 2 diabetes: an anthropometric determinant of carotid atherosclerosis and insulin resistance. Int J Obes (Lond). 2010;34:105–10.
Després JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126:1301–13.
Yamasaki Y, Kodama M, Nishizawa H, Sakamoto K, Matsuhisa M, Kajimoto Y, Kosugi K, Shimizu Y, Kawamori R, Hori M. Carotid intima-media thickness in Japanese type 2 diabetic subjects: predictors of progression and relationship with incident coronary heart disease. Diabetes Care. 2000;23:1310–5.
Bernard S, Sérusclat A, Targe F, Charrière S, Roth O, Beaune J, Berthezène F, Moulin P. Incremental predictive value of carotid ultrasonography in the assessment of coronary risk in a cohort of asymptomatic type 2 diabetic subjects. Diabetes Care. 2005;28:1158–62.
Authors’ contributions
TT, RB and YO designed the study, researched data, and wrote and edited the manuscript. RB, IM, TY, and YO contributed to intellectual discussion and reviewed and edited the manuscript. MA, MF, TF, MM, RN, YN, NO, HI and KH researched data. As the corresponding author and guarantor of this manuscript, RB is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Acknowledgements
This work was supported in part by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan. The authors thank all the staff of Department of Molecular Endocrinology and Metabolism, Tokyo Medical and Dental University and Ochanomizu Surugadai Clinic for their contributions.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ryotaro Bouchi and Takato Takeuchi contributed equally to this work
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bouchi, R., Takeuchi, T., Akihisa, M. et al. High visceral fat with low subcutaneous fat accumulation as a determinant of atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol 14, 136 (2015). https://doi.org/10.1186/s12933-015-0302-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-015-0302-4