Abstract
Background
It is not clear which glucose measure is more useful in the assessment of atherosclerosis. We investigated the associations of hemoglobin A1c (HbA1c), glycated albumin (GA), 1,5-anhydroglucitol (1,5-AG), fasting plasma glucose (FPG), and 2-hour postload glucose (PG) with carotid intima-media thickness (IMT) in community-dwelling Japanese subjects.
Methods
A total of 2702 subjects aged 40–79 years underwent a 75-g oral glucose tolerance test and measurements of HbA1c, GA, 1,5-AG, and carotid IMT by ultrasonography in 2007–2008. Carotid wall thickening was defined as a maximum IMT of >1.0 mm. The crude and multivariable-adjusted linear and logistic regression models were used to analyze cross-sectional associations between levels of glycemic measures and carotid IMT.
Results
The crude average of the maximum IMT increased significantly with rising quartiles of HbA1c, GA, FPG, and 2-hour PG levels in subjects with and without glucose intolerance (GI), while no clear association was observed for 1,5-AG. After adjustment for other confounding factors, positive trends for HbA1c, GA, and FPG (all p for trend < 0.05), but not 2-hour PG (p = 0.07) remained robust in subjects with GI, but no such associations were found in those without GI. When estimating multivariable-adjusted β values for the associations of 1 SD change in glycemic measures with the maximum IMT in subjects with GI, the magnitude of the influence of HbA1c (β = 0.021), GA (β = 0.024), and FPG (β = 0.024) was larger than that of 2-hour PG (β = 0.014) and 1,5-AG (β = 0.003). The multivariable-adjusted odds ratios for the presence of carotid wall thickening increased significantly with elevating HbA1c, GA, and FPG levels only in subjects with GI (all p for trend < 0.001). Among subjects with GI, the area under the receiver operating characteristic curve significantly increased by adding HbA1c (p = 0.04) or GA (p = 0.04), but not 1,5-AG, FPG, or 2-hour PG, to the model including other cardiovascular risk factors.
Conclusions
In community-dwelling Japanese subjects with GI, elevated HbA1c, GA, and FPG levels were significantly associated with increased carotid IMT, and HbA1c and GA provided superior discrimination for carotid wall thickening compared to 1,5-AG, FPG, and 2-hour PG, suggesting that HbA1c and GA are useful for assessing carotid atherosclerosis.
Similar content being viewed by others
Background
It has been well established that hemoglobin A1c (HbA1c) levels, which have been used widely as a measure of chronic hyperglycemia, are closely associated with the risk of microvascular complications, such as diabetic retinopathy, and this fact has led to the adoption of HbA1c as a diagnostic tool for diabetes by the International Expert Committee [1]. The question has now arisen as to whether HbA1c measurement is useful in the assessment of macrovascular complications. Several population-based epidemiological studies in Asian populations [2–5] as well as in Western populations [6–13] have focused on the association between HbA1c levels and intima-media thickness (IMT) of carotid arteries, which is generally accepted as a marker of the early stage of atherosclerosis. However, this issue has not been assessed sufficiently in a general Japanese population [5].
Glycated albumin (GA) and 1,5-anhydroglucitol (1,5-AG) levels, which are serum markers of short-term glycemic status, have also been shown to be intimately related to microvascular complications in recent epidemiological studies, including our previous report [14–16], and there has been a growing interest in GA and 1,5-AG as alternative markers of hyperglycemia [17]. Although several studies have examined the associations of GA [15, 18–25] and 1,5-AG [26, 27] levels with atherosclerosis among patients on dialysis and those with diabetes or hypertension, very few studies have been conducted to clarify this association in general populations [5, 28]. In addition, to our knowledge, there are no data comparing HbA1c, GA, 1,5-AG, fasting plasma glucose (FPG), and 2-hour postload glucose (PG) measurements as a tool for the assessment of atherosclerosis.
To investigate which glucose measure is more useful in the assessment of atherosclerosis, we examined the associations of HbA1c, GA, 1,5-AG, FPG, and 2-hour PG levels with carotid IMT in a community-dwelling Japanese population stratified by glucose tolerance status, and compared the magnitude of the influence of these five glycemic measures on the ability to discriminate carotid wall thickening.
Methods
Study population
A population-based prospective study of cardiovascular disease (CVD) and its risk factors has been underway since 1961 in the town of Hisayama, a suburb of the Fukuoka metropolitan area on Japan’s Kyushu Island. The population of the town has been stable for 50 years and was approximately 8400 in 2010. The age and occupational distributions, and nutritional intake of the population were similar to those of Japan as a whole based on data from the national census and nutrition survey [29]. In 2007 and 2008, a cross-sectional survey for the present study was performed in the town. A detailed description of this survey was published previously [16, 30]. Among a total of 3835 residents aged 40–79 years based on the town registry, 2957 (77.1 %) took part in a comprehensive assessment, including a 75-g oral glucose tolerance test (OGTT), the measurement of HbA1c, and a carotid ultrasound examination. We excluded eight subjects who did not consent to participate in the study, 46 who had already had breakfast, 35 who did not undergo the OGTT due to receiving insulin therapy, and 156 who refused the OGTT, leaving a total of 2712 subjects who completed the OGTT, HbA1c measurement, and carotid ultrasound. Among these, 10 subjects without measurement of GA or 1,5-AG were excluded, and the remaining 2702 subjects (1198 men and 1504 women) were enrolled in the present study.
Clinical evaluation and laboratory measurements
The study subjects underwent the OGTT between 8:00 and 10:30 A.M. after an overnight fast of at least 12 h. Blood for the glucose assay was obtained by venipuncture into tubes containing sodium fluoride at fasting and at 2-hour postload, and was separated into plasma and blood cells within 20 min. Plasma glucose concentrations were determined by the hexokinase method. Glucose tolerance status was classified as normal glucose tolerance (NGT) and glucose intolerance (GI) according to the 1998 World Health Organization criteria [31]; namely, for NGT, FPG <6.1 mmol/L and 2-hour PG <7.8 mmol/L; for GI, FPG ≥6.1 mmol/L, 2-hour PG ≥7.8 mmol/L, or the use of antidiabetic medications. Diabetes was defined as FPG ≥7.0 mmol/L, 2-hour PG ≥11.1 mmol/L, or the use of antidiabetic medications. HbA1c levels were measured by latex aggregation immunoassay (Determiner HbA1C; Kyowa Medex, Tokyo, Japan). The values for HbA1c were estimated as a National Glycohemoglobin Standardization Program (NGSP) equivalent value calculated with the formula: HbA1c (%) = 1.02 × HbA1c (Japan Diabetes Society) (%) + 0.25 % [32]. A portion of each serum specimen was stored at -80 °C for 5 years until it was used for measurement of GA and 1,5-AG in 2012. Serum GA levels were determined by an enzymatic method using an albumin-specific proteinase, ketoamine oxidase, and an albumin assay reagent (Lucica GA-L; Asahi Kasei Pharma, Tokyo, Japan). Serum 1,5-AG concentrations were measured enzymatically (Lana 1,5AG Auto Liquid; Nippon Kayaku, Tokyo, Japan). The intra- and interassay coefficients of variation were 0.6–1.1 % and 1.4–3.4 % for HbA1c, 0.5–3.2 % and 1.3 % for GA, 1.1–2.0 % and 2.5–2.8 % for 1,5-AG, and 0.4–1.3 % and 1.9–3.0 % for plasma glucose, respectively. Serum insulin values were measured by a chemiluminescent enzyme immunoassay. The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated with the formula: FPG (mmol/L) × fasting serum insulin (μU/mL) / 22.5 [33], and subjects in the highest quartile of HOMA-IR distribution in our study population (HOMA-IR ≥2.07) were defined as having insulin resistance [31]. Serum total, low-density lipoprotein (LDL), and high-density lipoprotein (HDL) cholesterols and triglycerides were all determined enzymatically. Hyper-LDL cholesterolemia was defined as LDL cholesterol levels ≥3.62 mmol/L or the use of lipid-lowering medications [34]. Freshly voided urine samples were tested by the dipstick method. Proteinuria was defined as 1+ or more. Serum creatinine concentrations were measured enzymatically, and estimated glomerular filtration rate (eGFR) (mL/min/1.73 m2) was calculated using the following modified equations of the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) for Japanese [35]: for men with a serum creatinine level >0.9 mg/dL, eGFR = 141 × (serum creatinine/0.9)-1.209 × 0.993Age × 0.813; for men with a serum creatinine level ≤0.9 mg/dL, eGFR = 141 × (serum creatinine/0.9)-0.411 × 0.993Age × 0.813; for women with a serum creatinine level >0.7 mg/dL, eGFR = 144 × (serum creatinine/0.7)-1.209 × 0.993Age × 0.813; for women with a serum creatinine level ≤0.7 mg/dL, eGFR = 144 × (serum creatinine/0.7)-0.329 × 0.993Age × 0.813. Chronic kidney disease (CKD) was defined as either an eGFR <60 mL/min/1.73 m2 or the presence of proteinuria [36].
The height and weight were measured with the subject in light clothes without shoes, and the body mass index (BMI) (kg/m2) was calculated. Blood pressure was obtained three times using an automated sphygmomanometer (BP-203 RVIIIB; Omron Healthcare Co., Ltd., Kyoto, Japan) with the subject in a sitting position after rest for at least 5 min; the average values were used in the analyses. Hypertension was defined as a systolic blood pressure ≥140 mmHg, a diastolic blood pressure ≥90 mmHg, or current treatment with antihypertensive agents.
Each participant completed a self-administered questionnaire covering medical history, antidiabetic, antihypertensive, and lipid-lowering treatments, alcohol intake, smoking habits, and physical activity. Alcohol intake and smoking habits were classified as either current use or not. Current smoking was defined as when the subject smoked at least 1 cigarette per day. Current drinking was defined as when the subject consumed at least 1 alcohol beverage per month. Subjects engaging in sports at least three times per week during their leisure time were defined as the regular exercise group. History of CVD was defined as any preexisting events of stroke or coronary heart disease, including myocardial infarction and coronary intervention. All cardiovascular events were adjudicated on the basis of physical examinations and a review of all available clinical information including medical records and imaging.
Carotid ultrasonography
Carotid ultrasound was performed in a supine position using a real-time, B-mode ultrasound imaging unit (Toshiba Sonolayer SSA-250A; Toshiba, Tokyo, Japan) with a 7.5-MHz annular array probe. The ultrasound examination was carried out by specially trained laboratory technicians using a standardized technique. The technicians were blinded to the medical history, and clinical and laboratory data of each participant. The IMT was measured using the long-axis view of each common carotid artery. An image was obtained in the region 20 mm proximal to the origin of the bulb at the far wall of each common carotid artery. The IMT values at 250 computer-based points in the region were measured on each side using a computer-assisted measurement system (Intimascope; Media Cross Co., Ltd., Tokyo, Japan) [37]. The maximum IMT was defined as the largest IMT value in either the left or right common carotid artery, and carotid wall thickening was defined as a maximum IMT of >1.0 mm according to the Japan Academy of Neurosonology and the Japan Society of Ultrasonics in Medicine’s guidelines [38, 39].
Statistical analysis
The SAS software package version 9.3 (SAS Institute, Cary, NC) was used to perform all statistical analyses. The differences in the mean values or frequencies of risk factors between glucose tolerance categories were assessed using the linear or logistic regression model, respectively. HbA1c, GA, 1,5-AG, FPG, and 2-hour PG levels were divided into quartiles by the presence or absence of GI. The values of IMT, fasting insulin, HOMA-IR, and triglycerides were transformed into logarithms to improve the skewed distribution, and geometric means were reported by back transformation. The linear regression model was used to examine the associations of 1 SD change in glycemic measures with the maximum IMT. The adjusted average values of the maximum IMT were calculated using the analysis of covariance method, and their trends across the quartiles of glycemic measures were tested by the linear regression model. The crude and multivariable-adjusted odds ratios (ORs) and their 95 % confidence intervals (CIs) for the presence of carotid wall thickening were estimated using the logistic regression model. Because serum 1,5-AG levels are decreased in the presence of hyperglycemia, the highest quartile was used as the reference group for 1,5-AG, while the lowest quartile was defined as the reference category for other glycemic measures. The heterogeneity in the influence of each glycemic measure on carotid wall thickening between subjects with and without other cardiovascular risk factors was assessed by adding an interaction term to the relevant statistical model. To compare the discrimination for the presence of carotid wall thickening between the models adjusted for known cardiovascular risk factors with and without continuous values of each glycemic measure, the difference in the area under the receiver operator characteristic curve (AUC) among models was estimated using the method of DeLong et al. [40]. A value of p < 0.05 was considered statistically significant in all analyses.
Ethical considerations
This study was conducted with the approval of the Kyushu University Institutional Review Board for Clinical Research, and written informed consent was obtained from all the participants.
Results
Of the study participants, there were 1603 (59.3 %) with NGT and 1099 (40.7 %) with GI. Among subjects with GI, 145 (13.2 %) had isolated fasting hyperglycemia (FPG ≥6.1 mmol/L and 2-hour PG <7.8 mmol/L), 457 (41.6 %) had isolated 2-hour postload hyperglycemia (FPG <6.1 mmol/L and 2-hour PG ≥7.8 mmol/L), and 497 (45.2 %) had both fasting and 2-hour postload hyperglycemia (FPG ≥6.1 mmol/L and 2-hour PG ≥7.8 mmol/L). The clinical characteristics of subjects are shown by GI status in Table 1. The mean values of age, maximum IMT, HbA1c, GA, FPG, 2-hour PG, fasting insulin, HOMA-IR, systolic and diastolic blood pressures, BMI, LDL cholesterol, and triglycerides, and the frequencies of men, insulin resistance, hypertension, antihypertensive and lipid-lowering medications, hyper-LDL cholesterolemia, proteinuria, CKD, and history of CVD were significantly higher in subjects with GI than in those with NGT, and subjects with GI had significantly lower 1,5-AG, HDL cholesterol, and eGFR values. The mean values of total cholesterol and the frequencies of alcohol intake, smoking habits, and regular exercise did not differ between the groups.
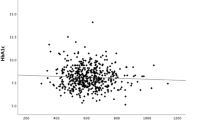
We estimated the crude and multivariable-adjusted geometric average of the maximum IMT according to the quartiles of each glycemic measure in subjects with GI. The crude geometric average of the maximum IMT increased significantly with rising HbA1c, GA, FPG, and 2-hour PG levels (all p for trend <0.001), but no clear association was observed for 1,5-AG levels (p for trend = 0.30). Similar associations were also observed in subjects with NGT (p for trend <0.05 for HbA1c, GA, FPG, and 2-hour PG; p for trend = 0.32 for 1,5-AG). Among subjects with GI, positive trends for HbA1c (p for trend = 0.048), GA (p for trend <0.001), and FPG (p for trend <0.001), but not 2-hour PG (p for trend = 0.07), remained significant even after adjustment for cardiovascular risk factors; namely, age, sex, hypertension, LDL cholesterol, HDL cholesterol, BMI, alcohol intake, smoking habits, regular exercise, and lipid-lowering medication (Fig. 1). Meanwhile, in those with NGT, the significant associations between levels of any glycemic measures and the maximum IMT disappeared after adjustment for the above-mentioned confounding factors (Additional file 1: Figure S1).
Multivariable-adjusted geometric average of maximum intima-media thickness according to quartiles of each glycemic measure in subjects with glucose intolerance. IMT: intima-media thickness; HbA1c: hemoglobin A1c; GA: glycated albumin; 1,5-AG: 1,5-anhydroglucitol; FPG: fasting plasma glucose; 2-hour PG: 2-hour postload glucose. * p < 0.01 vs Quartile 1, † p for trend <0.05. Multivariable adjustment was made for age, sex, hypertension, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, body mass index, alcohol intake, smoking habits, regular exercise, and lipid-lowering medication. HbA1c: Q1, <5.4 (36); Q2, 5.4–5.6 (36–38); Q3, 5.7–6.2 (39–44); Q4, ≥6.3 % (45 mmol/mol); GA: Q1, <14.3; Q2, 14.3–15.3; Q3, 15.4–17.1; Q4, ≥17.2 %; 1,5-AG: Q1, <11.0; Q2, 11.0–16.9; Q3, 17.0–22.9; Q4, ≥23.0 μg/mL; FPG: Q1, <5.7; Q2, 5.7–6.1; Q3, 6.2–6.8; Q4, ≥6.9 mmol/L; 2-hour PG: Q1, <8.0; Q2, 8.0–9.1; Q3, 9.2–12.3; Q4, ≥12.4 mmol/L
In subjects with GI, when continuous variables of glycemic measures were used instead of quartile categories, HbA1c, GA, FPG, and 2-hour PG levels were significantly and positively associated with the maximum IMT even after adjustment for other cardiovascular factors, but no such association was seen for 1,5-AG (Table 2). The magnitude of the influence of 1 SD increment in HbA1c (β = 0.021, p < 0.001), GA (β = 0.024, p < 0.001), and FPG (β = 0.024, p < 0.001) was larger than that of 2-hour PG (β = 0.014, p = 0.03). In those with NGT, no significant associations were found for all five glycemic measures after adjustment for other confounding factors (Additional file 1: Table S1).
The crude and multivariable-adjusted ORs and their 95 % CIs for the presence of carotid wall thickening according to the quartiles of each glycemic measure in subjects with GI are shown in Table 3. The crude ORs for the presence of carotid wall thickening significantly increased with elevating HbA1c, GA, FPG, and 2-hour PG levels, while lower 1,5-AG levels were significantly associated with prevalent carotid wall thickening. These associations remained robust even after adjustment for other confounding factors for HbA1c, GA, and FPG (all p for trend <0.001), but not for 1,5-AG (p = 0.09) and 2-hour PG (p = 0.14). In subjects with NGT, although the crude OR for carotid wall thickening did not increase with decreasing 1,5-AG levels, HbA1c, GA, FPG, and 2-hour PG levels were significantly and positively associated with the presence of carotid wall thickening (Additional file 1: Table S2). However, these upward trends were markedly attenuated and no longer significant after multivariable adjustment.
We next performed stratified analyses to examine whether the associations of glycemic measures with the presence of carotid wall thickening differed between groups with and without other cardiovascular risk factors in subjects with GI (Additional file 1: Figure S2A and S2B). Overall, there were no statistically significant differences in the multivariable-adjusted ORs for the prevalent carotid wall thickening per 1 SD increment in HbA1c, GA, FPG, and 2-hour PG, and 1 SD decrement in 1,5-AG according to levels of other risk factors: sex, age (<65 and ≥65 years), smoking habits, insulin resistance, hypertension, and hyper-LDL cholesterolemia (all p for heterogeneity >0.05).
To evaluate the improvement in discriminative ability for detecting the presence of carotid wall thickening by addition of continuous values of each glycemic measure to the model including potential cardiovascular risk factors, we compared the AUC between the models with and without each glycemic measure among subjects with GI (Table 4). The AUC increased significantly by adding HbA1c (0.729, p = 0.04) or GA (0.728, p = 0.04) values to the model including the potential cardiovascular risk factors mentioned above (0.719). When 1,5-AG (0.721, p = 0.27), FPG (0.724, p = 0.19), and 2-hour PG (0.721, p = 0.39) values were added, the AUC did not increase significantly.
We also performed sensitivity analyses excluding subjects with history of CVD and found that the findings were not substantially altered (data not shown).
Discussion
Using data from a cross-sectional survey in a Japanese community, we demonstrated that in subjects with GI, elevated levels of HbA1c, GA, and FPG were more strongly associated with increased maximum IMT compared to 1,5-AG and 2-hour PG, independent of other cardiovascular risk factors. Similar results were obtained from analysis of the associations between glycemic measures and the presence of carotid wall thickening. There were no clear differences in the influence of each glycemic measure between subjects with and without other cardiovascular risk factors. Furthermore, adding HbA1c or GA to a model including known cardiovascular risk factors significantly improved the assessment of the likelihood of prevalent carotid wall thickening in those with GI. These findings suggest that HbA1c and GA provide superior discrimination for the presence of carotid wall thickening, which is an early stage of atherosclerosis, compared to other glycemic measures in community-dwelling Japanese subjects with GI.
In the present study, increased HbA1c levels were significantly and positively associated with the presence of carotid wall thickening in individuals with GI, independently of other cardiovascular risk factors. Other Asian population studies have also shown that higher HbA1c levels were significantly and independently related to increased carotid IMT in Chinese populations [2, 3] and an Asian Indian population [4]. Similar findings were observed in most studies in Western populations [6, 8–10, 13]. With regard to clinical CVD events, although some cohort studies in the U.S. have demonstrated that HbA1c levels were not independently predictive of CVD incidence and mortality [41, 42], our previous study revealed that elevated HbA1c levels were significantly associated with increased risk of the development of CVD [43]. Other prospective studies in Western populations have also shown significant positive associations between HbA1c levels and the risk of CVD [9, 44]. These findings suggest that a higher HbA1c level is a risk factor for subclinical and clinical CVD in Asian populations including Japanese as well as in Western populations.
Epidemiological studies of community-dwelling persons which investigated the association between GA levels and atherosclerosis have been scarce. Only a Japanese community-based study has reported that maximum carotid IMT increased in subjects with higher GA levels, although it did not fully take confounding factors into consideration [5]. In our study, the likelihood of carotid wall thickening increased linearly with elevating GA levels among individuals with GI, and this association remained robust even after controlling for other cardiovascular risk factors. With regard to clinical studies, a recent case-cohort study in subjects with type 1 diabetes failed to demonstrate a significant influence of GA levels on CVD incidence and death [15]. Another study of patients with type 1 diabetes has also reported no significant association between GA/HbA1c ratio and carotid IMT [25]. However, other studies of patients on dialysis and those with type 2 diabetes have shown that higher GA levels were associated with the presence and progression of carotid atherosclerosis [20, 22, 24], the presence of coronary artery disease [18], impaired coronary collateral growth [23], and future CVD mortality [21] or hospitalization [19]. These findings, when taken together with our present results, indicate a close association between GA levels and the risk of atherosclerosis.
The present analysis demonstrated no clear association of 1,5-AG levels with maximum carotid IMT even in the crude analysis. Prior clinical studies also did not reveal significant differences in mean or maximum carotid IMT across 1,5-AG levels in patients with diabetes or hypertension [26, 27]. These findings imply that a weak association exists between 1,5-AG levels and carotid atherosclerosis. One of the possible reasons for this phenomenon is that the 1,5-AG level depends on the magnitude of glycosuria rather than plasma glucose levels [17], while other glycemic measures, including HbA1c, GA, FPG and 2-hour PG, directly reflect the degree of hyperglycemia. Another reason may be that 1,5-AG levels were affected by individual differences in the renal thresholds for glucose [45]. These explanations may account for the relatively weak association between 1,5-AG levels and carotid atherosclerosis in our study. On the other hand, with regard to clinical CVD events, one population-based cohort study in Japan has shown that lower 1,5-AG levels significantly increased the risk of developing CVD in men [28]. Since few studies have investigated the associations between 1,5-AG levels and the risk of CVD, further research is needed to clarify this issue.
In our study, higher FPG levels were independently related to carotid wall thickening in subjects with GI, but 2-hour PG levels were not. There have been conflicting data regarding the association between 2-hour PG levels and carotid atherosclerosis. At least 4 studies have shown that higher 2-hour PG levels were not a relevant factor for carotid atherosclerosis [3, 7, 11, 46], although others have found that elevated 2-hour PG levels were associated with increased carotid IMT [6, 47, 48]. Our previous prospective study showed that increased 2-hour PG levels were an independent risk factor for the occurrence of clinical CVD [49]. Thus, 2-hour PG levels might be more associated with the advanced stages of atherosclerosis than the early stages. Further investigation is necessary to validate this hypothesis.
In the present study, adding HbA1c or GA to a model including known cardiovascular risk factors significantly increased the AUCs for the presence of carotid wall thickening in subjects with GI, while the addition of 1,5-AG, FPG, and 2-hour PG did not substantially increase them. These results suggest that HbA1c and GA provide greater improvement in discriminative ability for detecting carotid atherosclerosis than other glycemic measures. Advanced glycation end products (AGEs) are recognized as one of the important contributors to the pathogenesis of atherosclerosis in hyperglycemia [50]. It is also known that HbA1c and GA are non-enzymatically glycated proteins, and these two measures are regarded as precursors of AGEs [51, 52]. Thus, it is speculated that HbA1c and GA values are correlated with the amount of AGEs. These findings raise the possibility that AGEs may play a key role in the early stages of atherosclerosis. Furthermore, it has been reported that HbA1c had a strong correlation with elevated FPG levels, which are mainly caused by insulin resistance, while GA was closely related to higher postprandial glucose levels, which are attributed to reduced insulin secretion [53]. Considering this finding, higher HbA1c levels may indicate insulin resistance, while elevated GA levels are likely to reflect decreased insulin secretion, resulting in postprandial glucose excursion. Since insulin resistance [54], abdominal obesity [55, 56], and glucose excursion [57] were also found to play important roles in the pathogenesis of atherosclerosis, higher HbA1c and GA levels may contribute to increased carotid IMT through insulin resistance, glucose excursion as well as AGEs, and this might be the reason why measurements of HbA1c and GA improve the discriminative ability for the presence of carotid wall thickening. In addition, because HbA1c and GA measurements can be done without fasting or timed samples, these two measures are convenient and suitable for use in general practice. This advantage has implications for the identification and management of atherosclerosis in its early stages, and thus measurements of HbA1c and GA suggest to be useful in the assessment of atherosclerosis.
In our subjects with NGT, the crude ORs for the presence of carotid wall thickening increased with rising HbA1c, GA, FPG, and 2-hour PG levels, but these associations were markedly attenuated after adjustment for other covariates. These findings suggest that higher glucose levels within normal range may not contribute independently to increased carotid IMT. Since other known cardiovascular risk factors, such as aging, hypertension, and dyslipidemia, tended to accumulate at the higher levels of HbA1c, GA, FPG, and 2-hour PG in our subjects with NGT (data not shown), individuals with elevations of these glycemic measures would seem to have higher carotid IMT through the mediation of other coexisting risk factors.
The strengths of our study include the population-based design and high participation rate. We also made a comparison of the five glycemic measures, which was not done in prior studies. However, some limitations should be mentioned. First, the cross-sectional study design limits the interpretation of causality between levels of glycemic measures and carotid atherosclerosis. Since the usefulness of glycemic measures in the assessment of atherosclerosis would ideally be evaluated in studies that examine the association between measures of glycemia and incident atherosclerotic disease, further prospective investigation is expected. Second, each glycemic measure was based on a single measurement, as was the case in most other epidemiological studies. This limitation may have resulted in misclassification of study subjects into different categories, and such misclassification could have weakened the association found in our study, biasing the results toward the null hypothesis. Third, the serum GA and 1,5-AG levels were measured after being stored at -80 °C for 5 years. In this context, however, we should note that the stability of GA and 1,5-AG measurements in frozen stored serum sample has been confirmed [58, 59]. Fourth, several laboratory technicians took ultrasound images of carotid artery without assessment of inter-observer variability. However, they were specially trained to use a standardized technique, and the IMT was measured automatically using a computer-assisted measurement system. Thus, we believe that this limitation is not likely to invalidate the findings observed in the present study. Fifth, CKD may cause a change in 1,5-AG levels through alterations in renal hemodynamics. However, the sensitivity analyses excluding subjects with CKD did not make any material difference in the findings on the association between 1,5-AG levels and carotid IMT (data not shown). Lastly, sample size of our study was relatively small to perform analyses separately in subjects with diabetes and prediabetes. Further studies with larger sample size are required to elucidate this issue.
Conclusions
The present analysis showed that, in a Japanese population with GI, elevated HbA1c, GA, and FPG levels were significantly associated with increased carotid IMT, and that the ability of HbA1c and GA to detect carotid wall thickening was superior to that of 1,5-AG, FPG, and 2-hour PG, suggesting that measurements of HbA1c and GA are useful as markers of early atherosclerosis. Further prospective studies are needed to verify these findings.
Abbreviations
- HbA1c :
-
Hemoglobin A1c
- IMT:
-
Intima-media thickness
- GA:
-
Glycated albumin
- 1,5-AG:
-
1,5-anhydroglucitol
- FPG:
-
Fasting plasma glucose
- PG:
-
Postload glucose
- CVD:
-
Cardiovascular disease
- OGTT:
-
Oral glucose tolerance test
- NGT:
-
Normal glucose tolerance
- GI:
-
Glucose intolerance
- NGSP:
-
National Glycohemoglobin Standardization Program
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- eGFR:
-
Estimated glomerular filtration rate
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- CKD:
-
Chronic kidney disease
- BMI:
-
Body mass index
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- AUC:
-
Area under the receiver operating characteristic curve
- AGE:
-
Advanced glycation end product
References
International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327–34.
Hung CS, Lee PC, Li HY, Ma WY, Lin MS, Wei JN, et al. Haemoglobin A1c is associated with carotid intima-media thickness in a Chinese population. Clin Endocrinol. 2011;75:780–5.
Huang Y, Bi Y, Wang W, Xu M, Xu Y, Li M, et al. Glycated hemoglobin A1c, fasting plasma glucose, and two-hour postchallenge plasma glucose levels in relation to carotid intima-media thickness in Chinese with normal glucose tolerance. J Clin Endocrinol Metab. 2011;96:E1461–5.
Venkataraman V, Amutha A, Anbalagan VP, Deepa M, Anjana RM, Unnikrishnan R, et al. Association of glycated hemoglobin with carotid intimal medial thickness in Asian Indians with normal glucose tolerance. J Diabetes Complications. 2012;26:526–30.
Furusyo N, Koga T, Ai M, Otokozawa S, Kohzuma T, Ikezaki H, et al. Plasma glycated albumin level and atherosclerosis: results from the Kyushu and Okinawa Population Study (KOPS). Int J Cardiol. 2013;167:2066–72.
Beks PH, Mackaay AJ, de Vries H, de Neeling JN, Bouter LM, Heine RJ. Carotid artery stenosis is related to blood glucose level in an elderly Caucasian population: the Hoorn Study. Diabetologia. 1997;40:290–8.
Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Bonadonna R, et al. Plasma glucose within the normal range is not associated with carotid atherosclerosis: prospective results in subjects with normal glucose tolerance from the Bruneck Study. Diabetes Care. 1999;22:1339–46.
Jørgensen L, Jenssen T, Joakimsen O, Heuch I, Ingebretsen OC, Jacobsen BK. Glycated hemoglobin level is strongly related to the prevalence of carotid artery plaques with high echogenicity in nondiabetic individuals: the Tromsø Study. Circulation. 2004;110:466–70.
Sander D, Schulze-Horn C, Bickel H, Gnahn H, Bartels E, Conrad B. Combined effects of hemoglobin A1c and C-reactive protein on the progression of subclinical carotid atherosclerosis: the INVADE Study. Stroke. 2006;37:351–7.
McNeely MJ, McClelland RL, Bild DE, Jacobs Jr DR, Tracy RP, Cushman M, et al. The association between A1C and subclinical cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. Diabetes Care. 2009;32:1727–33.
Kowall B, Ebert N, Then C, Thiery J, Koenig W, Meisinger C, et al. Associations between blood glucose and carotid intima-media thickness disappear after adjustment for shared risk factors: the KORA F4 study. PLoS ONE. 2012;7, e52590.
Zieman SJ, Kamineni A, Ix JH, Barzilay J, Djousse L, Kizer JR, et al. Hemoglobin A1c and arterial and ventricular stiffness in older adults. PLoS ONE. 2012;7:e47941.
Haring R, Baumeister SE, Lieb W, von Sarnowski B, Volzke H, Felix SB, et al. Glycated hemoglobin as a marker of subclinical atherosclerosis and cardiac remodeling among non-diabetic adults from the general population. Diabetes Res Clin Pract. 2014;105:416–23.
Selvin E, Francis LM, Ballantyne CM, Hoogeveen RC, Coresh J, Brancati FL, et al. Nontraditional markers of glycemia: associations with microvascular conditions. Diabetes Care. 2011;34:960–7.
Nathan DM, McGee P, Steffes MW, Lachin JM. Relationship of glycated albumin to blood glucose and HbA1c values and to retinopathy, nephropathy, and cardiovascular outcomes in the DCCT/EDIC Study. Diabetes. 2014;63:282–90.
Mukai N, Yasuda M, Ninomiya T, Hata J, Hirakawa Y, Ikeda F, et al. Thresholds of various glycemic measures for diagnosing diabetes based on prevalence of retinopathy in community-dwelling Japanese subjects: the Hisayama Study. Cardiovasc Diabetol. 2014;13:45.
Parrinello CM, Selvin E. Beyond HbA1c and glucose: the role of nontraditional glycemic markers in diabetes diagnosis, prognosis, and management. Curr Diab Rep. 2014;14:548.
Pu LJ, Lu L, Shen WF, Zhang Q, Zhang RY, Zhang JS, et al. Increased serum glycated albumin level is associated with the presence and severity of coronary artery disease in type 2 diabetic patients. Circ J. 2007;71:1067–73.
Murea M, Moran T, Russell GB, Shihabi ZK, Byers JR, Andries L, et al. Glycated albumin, not hemoglobin A1c, predicts cardiovascular hospitalization and length of stay in diabetic patients on dialysis. Am J Nephrol. 2012;36:488–96.
Song SO, Kim KJ, Lee BW, Kang ES, Cha BS, Lee HC. Serum glycated albumin predicts the progression of carotid arterial atherosclerosis. Atherosclerosis. 2012;225:450–5.
Shafi T, Sozio SM, Plantinga LC, Jaar BG, Kim ET, Parekh RS, et al. Serum fructosamine and glycated albumin and risk of mortality and clinical outcomes in hemodialysis patients. Diabetes Care. 2013;36:1522–33.
Sato Y, Nagao M, Asai A, Nakajima Y, Takaya M, Takeichi N, et al. Association of glycated albumin with the presence of carotid plaque in patients with type 2 diabetes. J Diabetes Invest. 2013;4:634–9.
Shen Y, Lu L, Ding FH, Sun Z, Zhang RY, Zhang Q, et al. Association of increased serum glycated albumin levels with low coronary collateralization in type 2 diabetic patients with stable angina and chronic total occlusion. Cardiovasc Diabetol. 2013;12:165.
Moon JH, Chae MK, Kim KJ, Kim HM, Cha BS, Lee HC, et al. Decreased endothelial progenitor cells and increased serum glycated albumin are independently correlated with plaque-forming carotid artery atherosclerosis in type 2 diabetes patients without documented ischemic disease. Circ J. 2012;76:2273–9.
Kim W, Kim KJ, Lee BW, Kang ES, Cha BS, Lee HC. The glycated albumin to glycated hemoglobin ratio might not be associated with carotid atherosclerosis in patients with type 1 diabetes. Diabetes Metab J. 2014;38:456–63.
Karrei K, Koehler C, Hanefeld M, Temelkova-Kurktschiev T, Del Prato S. Fluctuations in glycaemia in clinical diabetes mellitus type 2 are not associated with carotid intima-media thickening. Diab Vasc Dis Res. 2004;1:51–2.
Watanabe K, Suzuki T, Ouchi M, Suzuki K, Ohara M, Hashimoto M, et al. Relationship between postprandial glucose level and carotid artery stiffness in patients without diabetes or cardiovascular disease. BMC Cardiovasc Disord. 2013;13:11.
Watanabe M, Kokubo Y, Higashiyama A, Ono Y, Miyamoto Y, Okamura T. Serum 1,5-anhydro-D-glucitol levels predict first-ever cardiovascular disease: an 11-year population-based cohort study in Japan, the Suita study. Atherosclerosis. 2011;216:477–83.
Hata J, Ninomiya T, Hirakawa Y, Nagata M, Mukai N, Gotoh S, et al. Secular trends in cardiovascular disease and its risk factors in Japanese: half century data from the Hisayama Study, 1961–2009. Circulation. 2013;128:1198–205.
Fukuhara M, Arima H, Ninomiya T, Hata J, Hirakawa Y, Doi Y, et al. White-coat and masked hypertension are associated with carotid atherosclerosis in a general population: the Hisayama Study. Stroke. 2013;44:1512–7.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53.
Committee on the standardization of diabetes mellitus-related laboratory testing of Japan Diabetes Society. International clinical harmonization of glycated hemoglobin in Japan: from Japan Diabetes Society to National Glycohemoglobin Standardization Program values. J Diabetes Invest. 2012;3:39–40.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Committee for Epidemiology and Clinical Management of Atherosclerosis. Executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan-2012 version. J Atheroscler Thromb. 2013;20:517–23.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Modification of the CKD Epidemiology Collaboration (CKD-EPI) equation for Japanese: accuracy and use for population estimates. Am J Kidney Dis. 2010;56:32–8.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Yanase T, Nasu S, Mukuta Y, Shimizu Y, Nishihara T, Okabe T, et al. Evaluation of a new carotid intima-media thickness measurement by B-mode ultrasonography using an innovative measurement software. Intimascope Am J Hypertens. 2006;19:1206–12.
The Joint Committee of ‘The Japan Academy of Neurosonology’ and ‘The Japan Society of Embolus Detection and Treatment’ on guideline for Neurosonology. Carotid ultrasound examination. Neurosonology. 2006;19:49–69. in Japanese.
Terminology and Diagnostic Criteria Committee, Japan Society of Ultrasonics in Medicine. Standard method for ultrasound evaluation of carotid artery lesions. J Med Ultrasonics. 2009;36:219–26.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Pradhan AD, Rifai N, Buring JE, Ridker PM. Hemoglobin A1c predicts diabetes but not cardiovascular disease in nondiabetic women. Am J Med. 2007;120:720–7.
Chonchol M, Katz R, Fried LF, Sarnak MJ, Siscovick DS, Newman AB, et al. Glycosylated hemoglobin and the risk of death and cardiovascular mortality in the elderly. Nutr Metab Cardiovasc Dis. 2010;20:15–21.
Ikeda F, Doi Y, Ninomiya T, Hirakawa Y, Mukai N, Hata J, et al. Haemoglobin A1c even within non-diabetic level is a predictor of cardiovascular disease in a general Japanese population: the Hisayama Study. Cardiovasc Diabetol. 2013;12:164.
Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362:800–11.
Kilpatrick ES, Keevilt BG, Richmond KL, Newland P, Addison GM. Plasma 1,5-anhydroglucitol concentrations are influenced by variations in the renal threshold for glucose. Diabet Med. 1999;16:496–9.
Bobbert T, Mai K, Fischer-Rosinský A, Pfeiffer AF, Spranger J. A1C is associated with intima-media thickness in individuals with normal glucose tolerance. Diabetes Care. 2010;33:203–4.
Temelkova-Kurktschiev TS, Koehler C, Henkel E, Leonhardt W, Fuecker K, Hanefeld M. Postchallenge plasma glucose and glycemic spikes are more strongly associated with atherosclerosis than fasting glucose or HbA1c level. Diabetes Care. 2000;23:1830–4.
Kato K, Otsuka T, Kobayashi N, Kon Y, Kawada T. Two-hour post-load plasma glucose levels are associated with carotid intima-media thickness in subjects with normal glucose tolerance. Diabet Med. 2014;31:76–83.
Doi Y, Ninomiya T, Hata J, Fukuhara M, Yonemoto K, Iwase M, et al. Impact of glucose tolerance status on development of ischemic stroke and coronary heart disease in a general Japanese population: the Hisayama Study. Stroke. 2010;41:203–9.
Goldin A, Beckman JA, Schmidt AM, Creager MA. Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation. 2006;114:597–605.
Makita Z, Vlassara H, Rayfield E, Cartwright K, Friedman E, Rodby R, et al. Hemoglobin-AGE: a circulating marker of advanced glycosylation. Science. 1992;258:651–3.
Kim KJ, Lee BW. The roles of glycated albumin as intermediate glycation index and pathogenic protein. Diabetes Metab J. 2012;36:98–107.
Sakuma N, Omura M, Oda E, Saito T. Converse contributions of fasting and postprandial glucose to HbA1c and glycated albumin. Diabetol Int. 2011;2:162–71.
Gotoh S, Doi Y, Hata J, Ninomiya T, Mukai N, Fukuhara M, et al. Insulin resistance and the development of cardiovascular disease in a Japanese community: the Hisayama Study. J Atheroscler Thromb. 2012;19:977–85.
Dahlén EM, Bjarnegård N, Länne T, Nystrom FH, Östgren CJ. Sagittal abdominal diameter is a more independent measure compared with waist circumference to predict arterial stiffness in subjects with type 2 diabetes - a prospective observational cohort study. Cardiovasc Diabetol. 2013;12:55.
Ren C, Zhang J, Xu Y, Xu B, Sun W, Sun J, et al. Association between carotid intima-media thickness and index of central fat distribution in middle-aged and elderly Chinese. Cardiovasc Diabetol. 2014;13:139.
Mo Y, Zhou J, Li M, Wang Y, Bao Y, Ma X, et al. Glycemic variability is associated with subclinical atherosclerosis in Chinese type 2 diabetic patients. Cardiovasc Diabetol. 2013;12:15.
Nowatzke W, Sarno MJ, Birch NC, Stickle DF, Eden T, Cole TG. Evaluation of an assay for serum 1,5-anhydroglucitol (GlycoMarkTM) and determination of reference intervals on the Hitachi 917 analyzer. Clin Chim Acta. 2004;350:201–9.
Nathan DM, Steffes MW, Sun W, Rynders GP, Lachin JM. Determining stability of stored samples retrospectively: the validation of glycated albumin. Clin Chem. 2011;57:286–90.
Acknowledgments
The authors thank the staff of the Division of Health and Welfare of Hisayama for their cooperation in this study.
This study was supported in part by Grants-in-Aid for Scientific Research (A) (25253048) and (C) (25460758, 26350895, 26460748, 15 K09267, 15 K08738, and 15 K09835) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; by Core Research for Evolutionary Science and Technology (CREST) (13417915) from Japan Science and Technology Agency; by Health and Labour Sciences Research Grants of the Ministry of Health, Labour and Welfare of Japan (H25-Junkankitou [Seishuu]-Sitei-022, H26-Junkankitou [Seisaku]-Ippan-001, and H27-Shokuhin-Sitei-017); by the Japan Agency for Medical Research and Development (AMED) (15dk0207003h0003, 15ek0210001h0003, 15ek0210004h0002, 15dk0207009h0002, and 15gm0610007h0203 (CREST)); and by a research grant from the Japan Diabetes Society.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
NM contributed to the study concept and design, data collection, data analysis, data interpretation, and drafting of the manuscript. TN, JH, YH, FI, and MF contributed to the data collection and data interpretation. TH and DK measured the samples and contributed to the data interpretation. MK, UN, and TK contributed to the data interpretation and reviewed/edited the manuscript. YK contributed to the data collection, data interpretation, drafting of the manuscript, obtained funding, and study supervision. All authors provided critical review of the draft and approved the final version.
Additional file
Additional file 1: Figure S1.
Multivariable-adjusted geometric average of maximum intima-media thickness according to quartiles of each glycemic measure in subjects with normal glucose tolerance. Table S1: The associations of 1 SD increment in HbA1c, GA, FPG, and 2-hour PG, and 1 SD decrement in 1,5-AG with the maximum intima-media thickness in subjects with normal glucose tolerance. Table S2: Crude and multivariable-adjusted odds ratios and 95 % confidence intervals for the presence of carotid wall thickening according to quartiles of glycemic measures in subjects with normal glucose tolerance. Figure S2A and S2B: Multivariable-adjusted odds ratios and their 95 % confidence intervals for the presence of carotid wall thickening per 1 SD increment in HbA1c, GA, FPG, and 2-hour PG, and 1 SD decrement in 1,5-AG according to the subgroups of sex, age, smoking habits, insulin resistance, hypertension, and hyper-LDL cholesterolemia in subjects with glucose intolerance.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mukai, N., Ninomiya, T., Hata, J. et al. Association of hemoglobin A1c and glycated albumin with carotid atherosclerosis in community-dwelling Japanese subjects: the Hisayama Study. Cardiovasc Diabetol 14, 84 (2015). https://doi.org/10.1186/s12933-015-0247-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-015-0247-7