Abstract
Background
A high mortality rate has always been observed in patients with severe community-acquired pneumonia (SCAP) admitted to the intensive care unit (ICU); however, there are few reported predictive models regarding the prognosis of this group of patients. This study aimed to screen for risk factors and assign a useful nomogram to predict mortality in these patients.
Methods
As a developmental cohort, we used 455 patients with SCAP admitted to ICU. Logistic regression analyses were used to identify independent risk factors for death. A mortality prediction model was built based on statistically significant risk factors. Furthermore, the model was visualized using a nomogram. As a validation cohort, we used 88 patients with SCAP admitted to ICU of another hospital. The performance of the nomogram was evaluated by analysis of the area under the receiver operating characteristic (ROC) curve (AUC), calibration curve analysis, and decision curve analysis (DCA).
Results
Lymphocytes, PaO2/FiO2, shock, and APACHE II score were independent risk factors for in-hospital mortality in the development cohort. External validation results showed a C-index of 0.903 (95% CI 0.838–0.968). The AUC of model for the development cohort was 0.85, which was better than APACHE II score 0.795 and SOFA score 0.69. The AUC for the validation cohort was 0.893, which was better than APACHE II score 0.746 and SOFA score 0.742. Calibration curves for both cohorts showed agreement between predicted and actual probabilities. The results of the DCA curves for both cohorts indicated that the model had a high clinical application in comparison to APACHE II and SOFA scoring systems.
Conclusions
We developed a predictive model based on lymphocytes, PaO2/FiO2, shock, and APACHE II scores to predict in-hospital mortality in patients with SCAP admitted to the ICU. The model has the potential to help physicians assess the prognosis of this group of patients.
Similar content being viewed by others
Introduction
Pneumonia is an acute respiratory infection classified into community-acquired pneumonia (CAP) and hospital-acquired pneumonia (HAP) [1]. CAP is an acute disease caused by a pulmonary parenchymal infection acquired outside the hospital. More than 1.5 million adults in the United States are hospitalized yearly for CAP, with high hospitalization costs [2]. Patients with mild to moderate CAP are admitted to the outpatient clinic, ward, or intensive care unit (ICU) for treatment, depending on severity. Severe CAP (SCAP) or CAP requiring ICU hospitalization has a significantly worse prognosis [3,4,5,6,7]. A secondary analysis of a population-based cohort study of hospitalized SCAP patients in the United States by Cavallazzi et al. found that 23% of patients required ICU admission and that the risk for SCAP patients admitted to the ICU was 17% in-hospital mortality and nearly 50% 1-year mortality [2].
In previous studies on the prognosis of SCAP, either the study population was outside the ICU [8,9,10], the risk factors for mortality were not readily available clinically [9, 10], no relevant predictive model was developed [11], or the model developed was not externally validated [10, 12]. Generally, only a few comprehensive and accurate evaluation systems can adequately assess the prognosis of patients with SCAP admitted to the ICU at this stage. Therefore, developing a mortality prediction model for such patients is necessary to identify the risk factors for death at an early stage. In addition, ICU physicians can improve patient management and make better decisions with the help of a reasonable model.
In our study, we analyzed clinical data of patients with SCAP admitted to the ICU retrospectively, developed a mortality risk prediction model using easily accessible variables, and performed external validation to identify patients with high mortality risk as early as possible. We anticipate that the results of this study will assist ICU physicians in their efforts to improve the prognosis of patients with SCAPs.
Methods
Study design
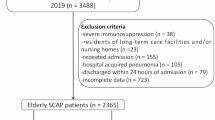
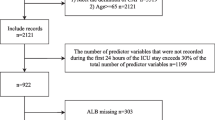
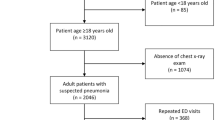
We conducted a two-center retrospective observational cohort study. The development cohort included 455 patients with SCAP from the Department of Critical Care Medicine of The First Affiliated Hospital of Anhui Medical University of China between June 2019 and October 2022. The validation cohort included 88 patients with SCAP admitted to the Department of Respiratory ICU at Anhui Chest Hospital, China, between July 2021 and November 2022. We retrospectively analyzed the clinical data of patients from these two cohorts. We established a mortality prediction model based on the development cohort. Model visualization was done using a nomogram. The validation cohort was substituted in the model for external verification.
Informed consent
of patients was waived by the First Affiliated Hospital Ethics Committee of Anhui Medical University because this study was retrospective. This study was approved by the First Affiliated Hospital Ethics Committee of Anhui Medical University. We conducted the study in strict compliance with the Declaration of Helsinki.
Patients
The inclusion criterion for this study was ICU inpatients who met the diagnostic criteria for SCAP. Following the guidelines of the Infectious Diseases Society of America/American Thoracic Society, SCAP was defined as the fulfillment of 1 main diagnostic criterion or ≥ 3 minor diagnostic criteria [13, 14]. The main diagnostic criteria included the following: (1) respiratory failure requiring invasive mechanical ventilation and (2) septic shock requiring vasopressors even after fluid resuscitation. The minor diagnostic criteria included the following: (1) Respiratory rate > 30 breaths/min, (2) PaO2/FiO2 < 250 mmHg, (3) multilobar infiltration, (4) consciousness impairment and/or orientation disorders, (5) blood urea nitrogen > 20 mg/dL, (6) count of white blood cell < 4 × 109 cells/L, (7) count of platelet < 100 × 109 platelets/L, (8) central body temperature < 36 °C, (9) hypotension (Systolic blood pressure < 90 mmHg, requiring active fluid resuscitation). The exclusion criteria were as follows: (1) patients with considerable missing clinical information, (2) diagnosis of hospital-acquired pneumonia, and (3) uncertain outcomes.
Data collection
The following clinical data were collected from the critical care electronic data mart within 48 h of admission to ICU: (1) demographic characteristics: sex, age; (2) chronic underlying disease comorbidities: hypertension, diabetes, tumors; (3) laboratory examinations: C-reactive protein (CRP), procalcitonin (PCT), neutrophils, lymphocytes, fibrinogen, D-dimer, blood urea nitrogen, total bilirubin, albumin, blood glucose, blood lactate, PaCO2, PaO2/FiO2; (4) severity of disease: whether combined with shock, APACHE II score, SOFA score; (5) clinical interventions: days of invasive mechanical ventilation, use of glucocorticoids. Patients admitted to the ICU with SCAP were divided into survival and death groups according to the in-hospital outcomes.
Statistical analysis
We excluded the variables with missing values greater than 20%, and the remaining variables were supplemented based on the multiple imputation method. Thereafter, we performed descriptive statistics for both cohorts and compared the differences between them. The mean ± standard deviation or median (interquartile range) was used for continuous variables, while frequencies and proportions were used as the descriptive statistics for categorical variables. The normal distribution of each variable was examined using the Kolmogorov–Smirnov test. Continuous variables were compared using the Student’s t-test or Mann–Whitney U-test. Categorical variables were analyzed using either Fisher’s exact test or Pearson’s χ2 test.
The developmental cohort was divided into survival and death groups based on the occurrence of death during hospitalization as the outcome variable. Potential variables with P < 0.05 in the univariate logistic regression analysis were added to the multivariate analysis to identify the independent risk factors for hospital morbidity. Odds ratios (ORs) and 95% confidence intervals (CIs) were used to present the results.
A nomogram was developed based on these independent risk factors in the development cohort to predict the probability of death. The model of the nomogram was evaluated using the consistency index (C-index) for the validation cohort. In the development and validation cohorts, predictive models were assessed using the area under the receiver operating characteristic (ROC) curve (AUC), calibration curve analysis, and decision curve analysis (DCA).
Statistical analysis was performed using SPSS version 26.0 and R version 4.12. P < 0.05 for both bilaterals was considered statistically significant.
Results
Basic demographic characteristics
Descriptions of the clinical data of the development and validation cohorts are provided in Table 1. The development cohort was composed of 455 patients with SCAP, of which 295 (64.84%) were male, and 160 (35.16%) were female, with an average age of (61.93 ± 17.77) years. They were divided into 358 patients in the survival group and 97 patients in the death group according to their prognosis, with a mortality rate of 21.32%. The validation cohort included 88 patients with SCAP, there were 70 males (79.55%) and 18 females (20.45%) among them, and the average age was (67.49 ± 14.02) years. According to their prognosis, the validation cohort was divided into 68 patients in the survival group and 20 cases in the death group, with a mortality rate of 22.73%. There were no significant differences between the development and validation cohorts with respect to the mortality rate (P > 0.05).
Construction of the predictive model
The results of the univariate regression analysis and the multivariate regression analyses for the development cohort are summarized in Table 2, which provides a detailed summary of the ORs and 95% CIs. It was observed that 23 variables were filtered using univariate logistic regression analysis to identify 12 statistically significant variables. These included CRP, PCT, lymphocyte, D-dimer, urea nitrogen, total bilirubin, blood glucose, PaCO2, PaO2/FiO2, Shock, APACHE II score, and SOFA score. Further multivariate regression analysis of these 12 variables showed that lymphocyte count, PaO2/FiO2, shock, and APACHE II score were independent risk factors for death in patients with SCAP admitted to the ICU in the development cohort. A one-unit lymphocyte increase within 48 h of admission was associated with approximately two-fold in-hospital mortality (OR: 1.996). A high APACHE II score was also a risk factor for in-hospital mortality (OR: 1.135). Shock can increase the risk of in-hospital death by approximately four-fold with a one-unit increase (OR: 4.093). PO2/FiO2 was a significant protective factor against in-hospital mortality because the OR was < 1 (OR : 0.997).
These variables were used to build a predictive model. A nomogram (Fig. 1) was constructed to predict the in-hospital mortality of patients admitted to the ICU with SCAP. The points corresponding to each variable were summed to obtain the total score and generate predicted mortality probability.
Evaluation of the predictive model
The clinical data of the validation cohort, which included 88 patients with SCAP from another hospital, were incorporated into the prediction model for external validation. The external validation results showed that the C index of the validation cohort was 0.903 (95% CI 0.838–0.968). We used ROC curves to compare the model with two classical scoring systems (APACHE II and SOFA). Figure 2 showed the ROC curve for the development cohort, the AUC of our predictive model was 0.850 (95% CI 0.813–0.881), APACHE II score 0.795 (95% CI 0.755–0.832), and SOFA score 0.69 (95% CI 0.645–0.732). The ROC curve for the validation cohort was shown in Fig. 3, the AUC of the predictive model was 0.893 (95% CI 0.809–0.949), APACHE II score 0.746 (95% CI 0.642–0.833), and SOFA score 0.742 (95% CI 0.638–0.829). The results indicated that the model had well-predicted power and accuracy for SCAP mortality. Meanwhile, it outperformed the traditional APACHE II and SOFA scoring systems.
Figures 4 and 5 showed the calibration curves for the development and validation cohorts, respectively, suggesting that the model’s predicted probabilities were close to the observed actual probabilities. The DCA curves for both cohorts were shown in Figs. 6 and 7, with significant net gains for most of the threshold probabilities. Moreover, our prediction model had a higher clinical application compared to APACHE II score and SOFA score.
Discussion
SCAP is the highest life-threatening type of CAP. The number of patients admitted to the ICU has increased significantly in recent decades, especially among older adults, individuals with comorbidities, and immunocompromised patients, with a high ICU in-hospital mortality rate [15, 16]. Miquel Ferrer et al. reported a 30-day mortality rate of 33% for patients with SCAP on invasive mechanical ventilation in the ICU [17]. The study by Cavallazzi et al. reported an in-hospital mortality rate of 17% in patients with SCAP in the ICU [2]. In our study, the mortality rates of patients with SCAP in the ICU were 21.32% and 22.73% at the two study centers, respectively. This finding is consistent with those of other studies. The high morbidity rate associated with SCAP in patients admitted to the ICU remains a global concern.
Therefore, it was necessary to develop a valuable evaluation system to predict the prognosis in this group. Ideally, such a system would be based on readily available variables in clinical practice. Our study analyzed 455 patients with SCAP admitted to the ICU as the developmental cohort. The final multivariate logistic regression analysis revealed lymphocyte count, PaO2/FiO2, shock, and APACHE II score as independent risk factors, used to establish the mortality prediction model.
As innate immune cells with adaptive immune functions, innate lymphoid cells (ILCs) constitute the body’s intrinsic immune system [18]. ILCs can be classified into ILC1, ILC2, and ILC3 at the molecular level [19]. They are involved in the early inflammatory and immune responses in patients with pulmonary infections, which is manifested as an increase in their numbers [20,21,22,23]. In addition, most patients with SCAP admitted to the ICU suffer from respiratory or circulatory failure; therefore, their condition is often complicated by sepsis. It is known that the pathophysiology of sepsis is characterized by an immune cytokine storm in the early stage and immune cell depletion in the late stage [24, 25]. The lymphocytes collected in our study were obtained within 48 h of admission to the ICU, which is just during the cytokine storm phase of sepsis. At this time, the lymphocytes are activated, and later an unfavorable prognosis occurs after a phase of immune cell depletion.
As one of the minor criteria for diagnosing SCAP, PaO2/FiO2 reflects the severity of respiratory failure in SCAP [13]. It has been suggested that the deterioration of PaO2/FiO2 can predict chest X-ray (CXR) abnormalities [26], whereas widespread severe CXR abnormalities are independent factors related to high mortality in patients with CAP [27, 28]. An observational study by Roberto et al. showed that the deterioration of PaO2/FiO2 is an independent predictor of hospital mortality during extracorporeal membrane oxygenation (ECMO) treatment [29]. A cross-sectional study from Italy showed that moderate to severe PaO2/FiO2 impairment was independently associated with a three-fold increased risk of in-hospital mortality in COVID-19 patients [30]. In our study, we collected the lowest level of PaO2/FiO2 within 48 h of admission to the ICU, which suggested that the lower the PaO2/FiO2 ratio, the higher the risk of death.
The APACHE II scoring system has been used extensively for the clinical assessment of critical diseases and as an important guide for the prognosis of ICU admissions. Although APACHE III and APACHE IV scoring systems have been developed and validated for diagnostic accuracy, the classic APACHE II scoring model remains the gold standard for the prognosis of critical care patients in the ICU worldwide [31]. As the APACHE II score does not rely on complex computer algorithms, it is easier to operationalize in clinical practice. Li et al. analyzed clinical data from a cohort of patients with pneumonia in the ICU who participated in a randomized controlled trial that focused on thromboprophylaxis and demonstrated that a higher APACHE II score at admission was one of the factors that influenced survival in these populations [32]. Our study also demonstrated that the APACHE II score is an independent risk factor influencing the prognosis of patients with severe pneumonia in the ICU.
The most common type of shock complicated by SCAP is septic shock, which is one of the main diagnostic criteria for SCAP [13]. Septic shock is associated with high virulence and severe damage to organ function. It is a widely recognized poor prognostic predictor of sepsis [33]. A large multicenter nested cohort study reported an overall mortality rate of 51% in patients with pneumonia-complicated septic shock [34]. Our study also confirmed that patients with SCAP in combination with shock had a worse prognosis.
Nomograms can quantify and visualize every variable’s contribution statistically, eliminating possible confounders among individual variables. In this study, we collected and analyzed the data of patients with SCAP in the ICU to establish a nomogram model. Further, data from another hospital were chosen for external validation. The results show that the model has high predictive effectiveness and provides better discrimination. Currently, there are no uniform assessment criteria to evaluate the risk of in-hospital mortality in SCAP. APACHE II and SOFA scoring systems are used widely in clinical practice. By comparing with their analysis, our prediction model showed higher accuracy and clinical application value. Owing to its high value for clinical application and accessibility of each variable, the model could help ICU physicians better evaluate the prognosis of patients.
The study had several limitations. First, it was a retrospective observational study, and selection bias could not be ruled out entirely. Second, the study only included patients from two hospitals, which may limit its generalizability to other geographical regions and populations. Third, the follow-up period was short and long-term mortality was not observed. In the future, it will be necessary to perform large-sample, multi-center prospective cohort studies to confirm our study results.
Conclusions
In summary, based on the clinical data of patients with SCAP admitted to the ICU, our study established a visualized nomogram model using lymphocytes, PaO2/FiO2 ratio, APACHE II score, and shock as the central mortality risk factors. The model demonstrated high predictive accuracy, discriminatory power, and clinical usefulness in predicting the risk of in-hospital mortality for patients with SCAP in the ICU. Our study will assist ICU physicians in improving the prognosis of patients with SCAPs.
Data availability
The data that support the fndings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- SCAP:
-
Severe community-acquired pneumonia
- ICU:
-
Intensive care unit
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the receiver operating characteristic curve
- DCA:
-
Decision curve analysis
- PaO2:
-
arterial oxygen partial pressure
- FiO2:
-
inhaled oxygen concentration
- APACHE:
-
Acute Physiology And Chronic Health Evaluation
- HAP:
-
Hospital-acquired pneumonia
- CRP:
-
C-reactive protein
- PCT:
-
procalcitonin
- PaCO2:
-
arterial carbon dioxide partial pressure
- SOFA:
-
Sequential Organ Failure Assessment;MV, mechanical ventilation.ORs:Odds ratios
- CIs:
-
confidence intervals
- ILCs:
-
innate lymphoid cells
- CXR:
-
Chest X-ray
- ECMO:
-
Extracorporeal membrane oxygenation
References
Torres A, Cilloniz C, Niederman MS, Menendez R, Chalmers JD, Wunderink RG, van der Poll T. Pneumonia. Nat Rev Dis Primers. 2021;7:25.
Cavallazzi R, Furmanek S, Arnold FW, Beavin LA, Wunderink RG, Niederman MS, Ramirez JA. The Burden of Community-Acquired Pneumonia requiring admission to ICU in the United States. Chest. 2020;158:1008–16.
Restrepo MI, Mortensen EM, Rello J, Brody J, Anzueto A. Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest. 2010;137:552–7.
Walden AP, Clarke GM, McKechnie S, Hutton P, Gordon AC, Rello J, Chiche JD, Stueber F, Garrard CS, Hinds CJ, Investigators EEG. Patients with community acquired pneumonia admitted to european intensive care units: an epidemiological survey of the GenOSept cohort. Crit Care. 2014;18:R58.
Torres A, Chalmers JD, Dela Cruz CS, Dominedo C, Kollef M, Martin-Loeches I, Niederman M, Wunderink RG. Challenges in severe community-acquired pneumonia: a point-of-view review. Intensive Care Med. 2019;45:159–71.
Cillóniz C, Torres A, Niederman MS. Management of pneumonia in critically ill patients. BMJ 2021.
Nair GB, Niederman MS. Updates on community acquired pneumonia management in the ICU. Pharmacol Ther. 2021;217:107663.
Garau J, Baquero F, Perez-Trallero E, Perez JL, Martin-Sanchez AM, Garcia-Rey C, Martin-Herrero JE, Dal-Re R, Group N. Factors impacting on length of stay and mortality of community-acquired pneumonia. Clin Microbiol Infect. 2008;14:322–9.
Xie J, Li Y, Wang M, He W, Zhao X. Diagnostic and Prognostic Value of Dysregulated miR-10a-3p in patients with severe pneumonia. J Inflamm Res. 2022;15:6097–104.
Hu L, Zhang Y, Wang J, Xuan J, Yang J, Wang J, Wei B. A prognostic model for In-Hospital mortality in critically ill patients with Pneumonia. Infect Drug Resist. 2022;15:6441–50.
Huang D, He D, Yao R, Wang W, He Q, Wu Z, Shi Y, Liang Z. Association of admission lactate with mortality in adult patients with severe community-acquired pneumonia. Am J Emerg Med. 2023;65:87–94.
Wang X, Jiao J, Wei R, Feng Y, Ma X, Li Y, Du Y. A new method to predict hospital mortality in severe community acquired pneumonia. Eur J Intern Med. 2017;40:56–63.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM Jr, Musher DM, Niederman MS, et al. Infectious Diseases Society of America/American thoracic society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):27–72.
Liapikou A, Ferrer M, Polverino E, Balasso V, Esperatti M, Piner R, Mensa J, Luque N, Ewig S, Menendez R, et al. Severe community-acquired pneumonia: validation of the infectious Diseases Society of America/American thoracic society guidelines to predict an intensive care unit admission. Clin Infect Dis. 2009;48:377–85.
Song Y, Wang X, Lang K, Wei T, Luo J, Song Y, Yang D. Development and validation of a Nomogram for Predicting 28-Day mortality on Admission in Elderly patients with severe community-acquired pneumonia. J Inflamm Res. 2022;15:4149–58.
Yang L, He D, Huang D, Zhang Z, Liang Z. Development and validation of Nomogram for Hospital Mortality in Immunocompromised patients with severe pneumonia in Intensive Care units: a Single-Center, Retrospective Cohort Study. Int J Gen Med. 2022;15:451–63.
Ferrer M, Travierso C, Cilloniz C, Gabarrus A, Ranzani OT, Polverino E, Liapikou A, Blasi F, Torres A. Severe community-acquired pneumonia: characteristics and prognostic factors in ventilated and non-ventilated patients. PLoS ONE. 2018;13:e0191721.
McKenzie ANJ, Spits H, Eberl G. Innate lymphoid cells in inflammation and immunity. Immunity. 2014;41:366–74.
Spits H, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, Koyasu S, Locksley RM, McKenzie AN, Mebius RE, et al. Innate lymphoid cells–a proposal for uniform nomenclature. Nat Rev Immunol. 2013;13:145–9.
Silver JS, Kearley J, Copenhaver AM, Sanden C, Mori M, Yu L, Pritchard GH, Berlin AA, Hunter CA, Bowler R, et al. Inflammatory triggers associated with exacerbations of COPD orchestrate plasticity of group 2 innate lymphoid cells in the lungs. Nat Immunol. 2016;17:626–35.
De Grove KC, Provoost S, Verhamme FM, Bracke KR, Joos GF, Maes T, Brusselle GG. Characterization and quantification of innate lymphoid cell subsets in human lung. PLoS ONE. 2016;11:e0145961.
Huang Y, Mao K, Chen X, Sun MA, Kawabe T, Li W, Usher N, Zhu J, Urban JF Jr, Paul WE, Germain RN. S1P-dependent interorgan trafficking of group 2 innate lymphoid cells supports host defense. Science. 2018;359:114–9.
Xiong H, Keith JW, Samilo DW, Carter RA, Leiner IM, Pamer EG. Innate Lymphocyte/Ly6C(hi) monocyte crosstalk promotes Klebsiella Pneumoniae Clearance. Cell. 2016;165:679–89.
Delano MJ, Ward PA. Sepsis-induced immune dysfunction: can immune therapies reduce mortality? J Clin Invest. 2016;126:23–31.
Chousterman BG, Swirski FK, Weber GF. Cytokine storm and sepsis disease pathogenesis. Semin Immunopathol. 2017;39:517–28.
Kwack WG. Evaluation of the Daily Change in PaO(2)/FiO(2) ratio as a predictor of abnormal chest X-rays in Intensive Care Unit Patients Post Mechanical Ventilation Weaning: a retrospective cohort study. Med (Kaunas) 2022, 58.
Godinas L, Lau EM, Chemla D, Lador F, Savale L, Montani D, Jais X, Sitbon O, Simonneau G, Humbert M, Herve P. Diagnostic concordance of different criteria for exercise pulmonary hypertension in subjects with normal resting pulmonary artery pressure. Eur Respir J. 2016;48:254–7.
Quah J, Liew CJY, Zou L, Koh XH, Alsuwaigh R, Narayan V, Lu TY, Ngoh C, Wang Z, Koh JZ et al. Chest radiograph-based artificial intelligence predictive model for mortality in community-acquired pneumonia. BMJ Open Respir Res 2021, 8.
Roncon-Albuquerque R Jr, Ferreira-Coimbra J, Vilares-Morgado R, Figueiredo P, Paiva JA. PaO(2)/FiO(2) deterioration during stable extracorporeal membrane Oxygenation Associates with protracted recovery and increased mortality in severe Acute Respiratory Distress Syndrome. Ann Thorac Surg. 2016;102:1878–85.
Sinatti G, Santini SJ, Tarantino G, Picchi G, Cosimini B, Ranfone F, Casano N, Zingaropoli MA, Iapadre N, Bianconi S, et al. PaO(2)/FiO(2) ratio forecasts COVID-19 patients’ outcome regardless of age: a cross-sectional, monocentric study. Intern Emerg Med. 2022;17:665–73.
Czajka S, Ziebinska K, Marczenko K, Posmyk B, Szczepanska AJ, Krzych LJ. Validation of APACHE II, APACHE III and SAPS II scores in in-hospital and one year mortality prediction in a mixed intensive care unit in Poland: a cohort study. BMC Anesthesiol. 2020;20:296.
Li G, Cook DJ, Thabane L, Friedrich JO, Crozier TM, Muscedere J, Granton J, Mehta S, Reynolds SC, Lopes RD, et al. Risk factors for mortality in patients admitted to intensive care units with pneumonia. Respir Res. 2016;17:80.
Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–51.
Speiser JL, Karvellas CJ, Shumilak G, Sligl WI, Mirzanejad Y, Gurka D, Kumar A, Kumar A. Institutional review boards of the Cooperative Antimicrobial Therapy of Septic Shock Database Research G: Predicting in-hospital mortality in pneumonia-associated septic shock patients using a classification and regression tree: a nested cohort study. J Intensive Care. 2018;6:66.
Acknowledgements
We thank the anonymous reviewers for their constructive comments. Thanks for the data support provided by the First Affiliated Hospital of Anhui Medical University and Anhui Chest Hospital.
Funding
This work was supported by Key Research and Development Program of Anhui. Province (No. 2022e07020039). Research project:The effect of Venoarterial extracorporeal membrane oxygenation on MAIT cells in patients with acute myocardial infarction.
Author information
Authors and Affiliations
Contributions
JP, TG, MS, and ZG conceived and designed the research. JP and TG drafted the manuscript. JP and WB collected the data. JP and TG analyzed the data. JP and TG prepared the figures and tables. MS, and ZG edited and revised the manuscript. MS and ZG approved the final version of manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Informed consent of patients was waived by the First Affiliated Hospital Ethics Committee of Anhui Medical University because this study was retrospective. This study was approved by the First Affiliated Hospital Ethics Committee of Anhui Medical University. We conducted the study in strict compliance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pan, J., Bu, W., Guo, T. et al. Development and validation of an in-hospital mortality risk prediction model for patients with severe community-acquired pneumonia in the intensive care unit. BMC Pulm Med 23, 303 (2023). https://doi.org/10.1186/s12890-023-02567-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02567-5