Abstract
Background
Obesity is a major independent risk factor for chronic diseases such as hypertension and coronary diseases, it might not be only related to the amount of body fat but its distribution. The single body mass index (BMI), waist circumference (WC), waist to hip ratio (WHR) or waist to stature ratio (WSR) provides limited information on fat distribution, and the debate about which one is the best remained. On the other hand, the current classification of body shape is qualitative rather than quantitative, and only crudely measure fat distribution. Therefore, a synthetical index is highly desirable to quantify body shape.
Methods
Based on the China Health and Nutrition Survey (CHNS) data, using Lohmäller PLSPM algorithm, six Partial Least Squares Path Models (PLSPMs) between the different obesity measurements and hypertension as well as two synthetical body shape scores (BSS1 by BMI/WC/Hip circumference, BSS2 by BMI/WC/WHR/WSR) were created. Simulation and real data analysis were conducted to assess their performance.
Results
Statistical simulation showed the proposed model was stable and powerful. Totally 15,172 (6,939 male and 8,233 female) participants aged from 18 to 87 years old were included. It indicated that age, height, weight, WC, WHR, WSR, SBP, DBP, the prevalence of hypertension and obesity were significantly sex-different. BMI, WC, WHR, WSR, Hip, BSS1 and BSS2 between hypertension and normotensive group are significantly different (p < 0.05). PLSPM method illustrated the biggest path coefficients (95% confidence interval, CI) were 0.220(0.196, 0.244) for male and 0.205(0.182, 0.228) for female in model of BSS1. The area under receiver-operating characteristic curve (AUC(95% CI)) of BSS1(0.839(0.831,0.847)) was significantly larger than that of BSS2(0.834(0.825,0.842)) as well as the four single indices for female, and similar trend can be found for male.
Conclusions
BSS1 was an excellent measurement for quantifying body shape and detecting the association between body shape and hypertension.
Similar content being viewed by others
Background
It is well known that overweight and obesity is a major independent risk factor for chronic diseases such as hypertension, coronary disease and diabetes [1,2]. Many epidemiological studies suggested a progressive increase in the prevalence of elevated blood pressure or hypertension with increasing obesity [3,4]. Several obesity measurements, including body mass index (BMI), waist circumference (WC), waist to hip ratio (WHR), and waist to stature ratio (WSR), have been proposed as markers for these chronic diseases in adults [5,6]. BMI, though most preferred [7], simply measures the mean weight under given body surface area and is affected by the amount of body fat, but unable to represent it’s distribution on human body [8]. However, one common sense is that health is not only affected by the amount of body fat but also distribution [9]. Various studies had shown that people with abdominal fat (with more weight around the waist) have higher risks of cardiovascular diseases (CVD) and other related diseases (such as hypertension, type 2 diabetes, and high cholesterol) than those with hip obesity (with more weight around the hip) [10,11]. Therefore, WC and WHR were widely used to measure abdominal fat for screening CVD and other related diseases (e.g. diabetes) in community population as well as in clinical practice [12,13]. Furthermore, WSR was recently confirmed as a better index of obesity over WC and BMI for detecting cardiometabolic risk factors [14], and it trumped BMI as screening tool for cardiometabolic risk. This indicated that body shape, which concentrates on fat distribution on human body, might be the more suitable for detecting the obesity related diseases.
However, WC, WHR or WSR, though gives a clearer indication of relative abdominal shape, still provide limited information on fat distribution. As a measurement of obesity, BMI represents a very crude index of shape, while WHR or WSR gives clearer indication of relative abdominal shape by taking account of the difference in body structure. Hence, it is possible for two man (or woman) to have vastly different BMIs but the same WHRs (or WSRs), or to have the same BMIs but vastly different WHRs or WSRs [15]. In practice, the influence of body fat distribution has been linked with body shape, which was generally broken down into four distinct types named after the fruits they resemble most [16,17], including apple (with more weight around the waist), pear (with more weight around the hip), pear-apple (with the WHR above the standard), Chilli (with normal BMI). Research shows that people with “apple” body shape face more health risks than those with “pear” body shape, and the combination of WHR and BMI is a better predictor of CVD risk and mortality than BMI alone [18]. However, this classification of body shape is qualitative rather than quantitative, and still crudely measure fat distribution on human body. Therefore, the structural equation model (SEM) between body shape and hypertension under the framework of Partial Least Squares Path Model (PLSPM) was built in this study. The synthetical index (body shape score, BSS) for quantifying body shape was constructed by the four basic measurements of BMI, WC, WHR and WSR in order to better explain the relationship between body shape and high blood pressure. Simulations are conducted to illuminate whether the proposed model is stable and efficient. Moreover, the China Health and Nutrition Survey (CHNS) data is further analyzed to assess whether the proposed model is in line with reality and to illustrate the performance of the constructed BSS to predict hypertension.
Methods
Study sample and measurements
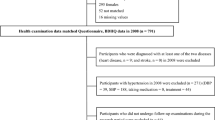
CHNS data which was conducted in nine provinces of China (including Guangxi, Guizhou, Heilongjiang, Henan, Hubei, Hunan, Jiangsu, Liaoning and Shandong) from 1993 to 2012, was used to construct our PLSPM between body shape and hypertension for both statistical simulation and real data analysis. Details about the CHNS have been published elsewhere [19]. In order to use enough sample to validate the proposed model, we used most waves of CHNS study (1993, 1997, 2000, 2004, 2006 and 2009) and took the first survey result for repeated measurements of each individual. A total of 25,753 individuals aged 18 years or older were potential eligible in this study. However, 10,581 persons were excluded since they did not provide anthropometry data such as height, weight, WC, hip circumference, systolic blood pressure (SBP), diastolic blood pressure (DBP) and current use of antihypertensive medications. At last, 15,172 (6,939 male and 8,233 female) participants with 18 to 87 years old were included in the final data analysis. All participants underwent a standardized medical examination included the collection of a systolic blood pressure (SBP), diastolic blood pressure (DBP). Blood pressure (BP) was measured by trained examiners on the right arm using a mercury sphygmomanometer according to a standard protocol [20]. The three BP values were measured and the average of three readings was chosen as the BP values. Anthropometric measurements were taken after the participants had removed their shoes, heavy clothing, and belts. Height, weight, WC and hip circumference (Hip) were measured by the trained nurses. BMI was calculated as weight (kg)/height2 (m2), WC was measured at the level midway between the lower rib margin and the iliac crest while the participants breathed out gently. Hip was taken at the level of maximal gluteal protrusion. WHR and WSR were calculated as WC(cm)/Hip(cm) and WC(cm)/stature(cm) respectively. The presence of hypertension was defined by an SBP ≥ 140 mmHg, a DBP ≥ 90 mmHg or self-reported current use of antihypertensive medications [21]. All participants provided written informed consent and the study was approved by institutional review committees of the University of North Carolina at Chapel Hill and the National Institute for Nutrition and Food Safety, Chinese Center for Disease Control and Prevention.
Model structure
Figure 1 showed the model structure between hypertension and body shape under framework of PLSPM using different manifest anthropometric measurements, with (a) by BMI/WC/Hip, (b) by BMI/WC/WHR/WSR, (c) by BMI; (d) by WC; (e) by WHR; (f) by WSR. Figure 1(a) defined a latent quantitative measurement of body shape score (ξ1) extracted from BMI, WC and Hip (BSS1), while BSS2 from BMI, WC, WHR and WSR (Figure 1b). The latent score of blood pressure (BPS, ξ2) was summarized by binary variable of hypertension. We exemplified Figure 1(a) to explain the variables and their relationships : (1) The variables in the squared boxes were the manifest variables actually measured such as BP, age, BMI, WC and Hip; (2) The variables in the ellipses were the latent variables such as BPS(ξ2), BSS1(ξ1) and age(ξ3)calculated through the corresponding manifest variables, (3) The latent variable BSS1(ξ1) corresponded to the manifest variables BMI, WC and Hip, while the latent variable BPS(ξ2)to BP, and (ξ3)to the single variable age. Three types of parameters were included: (1) Latent variable scores (ξ) as combinations of their manifest variables obtained iteratively from an ordinary least squares (OLS)-type algorithm; (2) path coefficients (β) between dependent (ξ2) and independent latent variable (ξ1) by OLS or partial least squares (PLS); (3) loadings (λ) of each block of manifest variables with its latent variables by OLS, and the arrows was from the manifest variable to the latent variable when single manifest exist, otherwise the arrow direction is opposite. In this paper, the Lohmäller PLSPM algorithm was used [22].
Non-parametric test by bootstrap procedure
As the distribution of parameters from PLSPM is unknown, significant test of path coefficients and loadings were furnished by bootstrap procedures [23,24]. Significance of a parameter (w) under the null hypothesis: H0: w = 0 and the alternative hypothesis H1: w ≠ 0 was tested via a normal test in the form \( \mathrm{U}=\frac{\left|\mathrm{w}-0\right|}{\mathrm{se}\left(\mathrm{w}\right)} \) (e.g., \( \mathrm{U}=\frac{\left|{\beta}_{21}-0\right|}{\mathrm{se}\left({\beta}_{21}\right)} \)) where se(w) is the bootstrapped standard error.
Data simulation
We performed a real-data-based statistical simulation under the null hypothesis (H0) and alternative hypothesis (H1) to assess the PLSPM-based body shape statistics. The simulation was based on the indices included BMI, WC, HIP, SBP and DBP in CHNS data and steps were as follows: (1) Calculated the mean and covariance matrix of BMI, WC, HIP, and generated the multivariate normal distribution data, used the R package mvtnorm [25]; (2) identified δ as the range of 0.1 to 0.3 (0.10, 0.15, 0.20, 0.25, 0.30) by the standardized regression coefficient of a simple regression model \( \mathrm{S}\mathrm{B}\widehat{\mathrm{P}}=0.325\mathrm{B}\mathrm{M}\mathrm{I} \) based on initial data, SBP and DBP were obtained by BMI for each given δ. (3) Built the PLSPMs and performed the statistical simulation: the simulation data under different sample sizes were sampled from the simulated population (500,000 individuals). Under the null hypothesis (H0), repeat 1,000 simulations under different sample sizes (n = 500, 1000, 1500, 2000, 2500) to assess the type I error. Under the alternative hypothesis (H1), for each model with different effect- δ (δ =0.10, 0.15, 0.20, 0.25, 0.30), conduct 1,000 simulation under different sample sizes to assess the statistical power.
Real data analysis
For detecting the association between body shape and hypertension, student's t-test was firstly used to test the difference of the variables (age, SBP, DBP, height, weight, Hip, WC, BMI, WHR, WSR) between male and female, as well as the difference of BMI, WC, WHR, WSR, Hip, BSS1 and BSS2 between normotension and hypertension for male and female group respectively. χ2 test was used to test the prevalence of hypertension and prevalence of obesity based on BMI. Pearson correlation coefficient was then used to detect correlation between the five obesity related measurements (BMI, WC, WHR, WSR, Hip). The Lohmaller PLSPM algorithm was further used to calculate BSS. Along with the risk of obesity, body shape was classified into nine [26] (1 ~ 9) types by WHR increasing under given BMI increasing (see Table 1). F test and LSD test were finally used to detect linear relationship between BSS1 and body shape type (BST).
Based on the PLSPM of BSS1 and BSS2, the association between body shape and hypertension was obtained using path coefficients from BSS1/BSS2 to BPS. Six PLSPMs were created by defining the measurement model using BMI/WC/Hip, BMI/WC/WHR/WSR, BMI, WC, WHR, WSR as the manifest variable of body shape respectively (see Figure 1). By comparing the path coefficients (β21) in the six different models, we assessed their performances for detecting the association between body shape and hypertension. Furthermore, the area under receiver-operating characteristic (ROC) curve (AUC) was used to evaluate the performance of the six different BSS for predicting hypertension by adjusting age in the PLSPMs. The SmartPLS2.0 was used to build PLSPMs, SPSS16.0 was used to run t test, F test and χ2 test. ROC curve was created by the Medcalc program version 9.3.9.0 ( MedCalc software, Mariakerke, Belgium ).
Results
Simulation
As shown in Figure 2, the type I error rates of PLSPM model was close to nominal levels (0.05, 0.01) as a function of sample sizes (Figure 2a and b), and the power monotonically increases with sample size, effect size (δ) at α = 0.05 level and α = 0.01 (Figure 2c and d). This indicated that our PLSPM was suitable for detecting the association between body shape and hypertension.
The performance of PLSPM based model in Figure1(a) in type I error and power. With (a), (c) for α = 0.05, and (b), (d) for α = 0.01.
The real data analysis
The distribution of age, blood pressure, and obesity related variables between male and female were summarized in Table 2, and the prevalence of hypertension and obesity based on BMI are listed in Table 2. Definition of obesity based on BMI is in accordance with the standards of China [27]. It showed that age, height, weight, WC, WHR, WSR, SBP, DBP, the prevalence of hypertension and obesity were significantly different between the two groups, suggesting that PLSPM should be constructed for male and female respectively. Furthermore, the distribution of the obesity related measurements (BMI, WC, WHR, WSR, Hip, BSS1, BSS2) between hypertension and normotensive group are showed in Table 3 for male and female respectively. It demonstrated that all the variables were significantly different between hypertension and normotensive group for both male and female, suggesting that the BPS should be obtained from binary variable (hypertension = 1 vs normotensive = 0 ) for developing PLSPM.
Table 4 showed the correlation matrix of BMI, WC, WHR, WSR, hip for male and female group. It illustrated that strong correlation between them existed, suggesting that the reflective PLSPM should be selected for defining the measurement model.
Table 5 showed the path coefficient from BSS to BPS in the six PLSPM models (see Figure 1) for male and female respectively. It indicated that the biggest path coefficient was in model of BSS1 → BPS, followed by BSS2, and other single index for both male and female groups, suggesting that the synthetical BSS have better performance than the single one for detecting the association between body shape and hypertension. It demonstrated that the AUC of BSS1 was significantly larger than that of BSS2 as well as the four single indices for female, and so as in males though no statistical significance can be found.
Table 6 showed the relationship between quantitative body shape score (BSS1) and qualitative body shape type (BST), suggesting that, 1) there was significant sex difference of overall body shape types ( χ2 = 242.55, P < 0.0001); 2) for both male and female, along with the risk of obesity, BSS1 was monotonically increasing from types 1 to 9 (Table 6), with significant differences between given two types except type 7 and type 8 (F = 1431.84, P < 0.0001 for male, F = 1738.24, P < 0.0001 for female, both with p < 0.05 according to LSD test). 3) Linear regression between the BSS1 and BST had good fit for male (F = 10988.28, P < 0.0001, R2 = 0.61) and female (F = 12860.00, P < 0.0001, R2 = 0.61), indicating that BSS1 was an excellent measurement for body shape.
Discussions
Obesity is an independent risk factor for hypertension, and the relationship between them has been confirmed in some studies. However, hypertension might not be only affected by the amount of body fat but also distribution. Traditionally, BMI is frequently used for the assessment of obesity in a clinical setting, but it just reflected the amount of body fat rather than their distribution, which is more likely to be associated with health-related risks. To overcome this limitation of BMI, various indices have been proposed for measuring obesity, and were used to detect the association between obesity and hypertension. Generally, the four anthropometric markers (BMI, WC, WHR and WSR) have all been proved to be associated with hypertension [28,29]. Although they were reported to be associated with hypertension, the debate about which one is the best remained. Among the obesity related indices of BMI, WC, WHR and WSR, various studies showed that WC was the best predictor of hypertension not only by cross-sectional study [30] but cohort study [31], while other studies suggested that WSR should be the best predictor [32-34], and they might depend on gender [35,36] in different population. In addition, WSR was confirmed with similar predictive power to WHR for hypertension [37]. However, several studies [38-40] indicated that BMI was not less powerful than WC, WHR or WSR for predicting hypertension. These inconsistent results might due to their single index rather than using the combined information of the four obesity measurements. Actually, some studies recommended the combination of WHR and BMI [41,42], and the combination of BMI and WC [43], to overcome the shortage of the single index. These combination methods not only embody the amount of body fat but also their distribution, which hints different types of body shape. For simplicity, four basic types of body shape (Chilli, pear, apple and pear-apple) have been proposed, and the research showed that people with “apple-shaped” bodies face more health risks than those with “pear-shaped”, and the combination of WHR and BMI is a better predictor of CVD risk and mortality than BMI alone [44,45]. However, this classification of body shape is qualitative rather than quantitative, and still crudely to measure fat distribution on human body, and the quantitative body shape index is highly desirable. We thus proposed two synthetical scores (BSS1 and BSS2) to quantify body shape using PLSPM method, BSS1 is extracted from BMI, WC and Hip, while BSS2 from BMI, WC, WHR and WSR, and both of them were further used to detect the association between obesity and hypertension. Statistical simulation showed that the proposed model was stable (Figure 2a and b), and powerful (Figure 2c and d) for detecting the association between body shape and hypertension. Further real data analysis using CHNS database illustrated that BSS1 had the better performance than BSS2 as well as the single index (BMI, WC, WHR and WSR) for detecting the association between obesity and hypertension (Table 5), and for predicting hypertension (Table 5). In addition, along with the risk of body shape, BSS1 was monotonically increasing and the linear relationship between them had been proven (Table 6). In conclusion, BSS1 was an excellent measurement for quantifying body shape and for detecting the association between body shape and hypertension.
Body shape is linked with multiple anthropology indices (BMI, WC, WHR, WSR and Hip) rather than the single one. For quantifying human body shape, the SEM method should be used to extract latent synthetical body shape score from the above manifest anthropology indices. However, as the stronger multicollinearity between the anthropology indices (BMI, WC, WHR, WSR and Hip), the ordinary linear SEM usually loses power for detecting the association between body shape score and hypertension. We, therefore, adopted PLSPM method to build the SEM model for extracting BSS, and further detecting its association with hypertension. Theoretically, compared to SEM, PLSPM is robust to multicollinearity commonly encountered in anthropometric indices data (such as high correlation between BMI, WC, WHR, WSR and Hip). It is a“soft modeling” approach requiring very few distributional assumptions, variables can be numerical, ordinal or nominal, and no need for normality assumptions, while covariance-based SEM is a “hard modeling” with heavy distribution assumptions. In addition, compared with the other methods such as logistic regression, support vector machine (SVM), decision trees and naïve Baye, traditional multivariate logistic regression may fail to deal with the multiple independent variables with multicollinearity. On the other hand, although Support vector machine (SVM), decision trees and naïve Bayes can be used for discriminant analysis and may not be affected heavily by multicollinearity, it seems unable for them to synthesize the manifest variables to get a latent score. Thus, PLSPM was preferred to construct the latent variable of body shape. In this study, the proposed synthetical BSS was only based on the cross-sectional survey data in CHNS study, further work should be conducted to evaluate its performance in the cohort study. On the other hand, it has become more and more clinically important to assess body shape based on the pattern of body fat distribution and redistribution, rather than to assess obesity simply based on an increased amount of body fat. The proposed BSS1, though just having a little higher AUC values, was still significantly better than other indices, indicating that BSS1 can indeed have superior performance. Actually, just like many previous large sample studies, the difference in AUC value is usually small when comparing different indices, and it seems that, to some extent, little increase cannot be unnecessary. On the other hand, the calculation of proposed BSS is not quite complex, and it is not quite difficult to use in the public health and clinical practice. In addition, this study also provides new insights to construct the better obesity index. Several recent studies proposed three-dimensional body scan and confirmed the relationships of three-dimensional body scanning results to hypertension [44]. Further, quantitative BSS based on the measurements of three-dimensional body scans should be developed for measuring the body shape and for detecting the association between obesity and hypertension accurately.
Conclusions
In conclusion, BSS1 was an excellent measurement for quantifying body shape and detecting the association between body shape and hypertension.
References
Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects), Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383:970–83.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010;23:247–69.
Okafor C, Anyaehie U, Ofoegbu E. The magnitude of obesity and its relationship to blood pressure among the residents of enugu metropolis in South East Nigeria. Ann Med Health Sci Res. 2014;4:624–9.
Chandra A, Neeland IJ, Berry JD, Ayers CR, Rohatgi A, Das SR, et al. The relationship of body mass and fat distribution with incident hypertension: observations from the Dallas Heart Study. J Am Coll Cardiol. 2014;64:997–1002.
Takahashi M, Shimomura K, Proks P, Craig TJ, Negishi M, Akuzawa M, et al. A proposal of combined evaluation of waist circumference and BMI for the diagnosis of metabolic syndrome. Endocr J. 2009;56:1079–82.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275–86.
Su D. Body mass index and old-age survival: a comparative study between the Union Army Records and the NHANES-I Epidemiological Follow-Up Sample. Am J Hum Biol. 2005;17:341–54.
Donini LM, Poggiogalle E, Del Balzo V, Lubrano C, Faliva M, Opizzi A, et al. How to estimate fat mass in overweight and obese subjects. Int J Endocrinol. 2013;4:1–10.
Bae CY, Kang YG, Suh YS, Han JH, Kim SS, Shim KW. A model for estimating body shape biological age based on clinical parameters associated with body composition. Clin Interv Aging. 2013;8:11–8.
Wells JC, Treleaven P, Cole TJ. BMI compared with 3-dimensional body shape: the UK National Sizing Survey. Am J Clin Nutr. 2007;85:419–25.
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27000 participants from 52 countries: a case–control study. Lancet. 2005;366:1640–9.
Mamtani M, Kulkarni H, Dyer TD, Almasy L, Mahaney MC, Duggirala R, et al. Waist circumference independently associates with the risk of insulin resistance and type 2 diabetes in mexican american families. PLoS One. 2013;8:e59153.
Brambilla P, Bedogni G, Heo M, Pietrobelli A. Waist circumference-to-height ratio predicts adiposity better than body mass index in children and adolescents. Int J Obes (Lond). 2013;37:943–6.
Lim LL, Seubsman SA, Sleigh A, Bain C. Validity of self-reported abdominal obesity in Thai adults: a comparison of waist circumference, waist-to-hip ratio and waist-to-stature ratio. Nutr Metab Cardiovasc Dis. 2012;22:42–9.
Akpinar E, Bashan I, Bozdemir N, Saatci E. Which is the best anthropometric technique to identify obesity: body mass index, waist circumference or waist-hip ratio? Coll Antropol. 2007;31:387–93.
Ashwell M. Obesity risk: importance of the waist-to-height ratio. Nurs Stand. 2009;23:49–54.
Walsh P. Research profile. The apple shape. Causes and effects. Diabetes Forecast. 2004;57:73–5.
Walton C, Lees B, Crook D, Worthington M, Godsland IF, Stevenson JC. Body fat distribution, rather than overall adiposity, influences serum lipids and lipoproteins in healthy men independently of age. Am J Med. 1995;99:459–64.
Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: The China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39(6):1435–40.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72.
Yan S, Li J, Li S, Zhang B, Du S, Gordon-Larsen P, et al. The expanding burden of cardiometabolic risk in China: the China Health and Nutrition Survey. Obes Rev. 2012;13(9):810–21.
Esposito VV, Chin WW, Henseler J, Wang H. Handbook of Partial Least Squares: Concepts, Methods and Applications. Berlin Heidelberg: Springer; 2010.
Henseler J, Ringle CM, Sinkowics RR. The Use of Partial Least Squares Path Modeling in International Marketing. Advin Intern Mark. 2009;20:277–319.
Davison AC, Hinkley DV. Bootstrap methods and their application. New York NY: Cambridge University Press; 2003.
Mi X, Miwa T, Hothorn T. mvtnorm: New numerical algorithm for multivariate normal probabilities. The R Journal. 2009;1:37–39.
Xue F, Li S, Luan J, Yuan Z, Luben RN, Khaw KT, et al. A latent variable partial least squares path modeling approach to regional association and polygenic effect with applications to a human obesity study. PLoS One. 2012;7:e31927.
Chen C, Lu FC, Department of Disease Control Ministry of Health, P.R. China. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36.
Moni MA, Rahman MA, Haque MA, Islam MS, Ahmed K. Blood pressure in relation to selected anthropometric measurements in senior citizens. Mymensingh Med J. 2010;19:254–8.
Gupta S, Kapoor S. Sex differences in blood pressure levels and its association with obesity indices: Who is at greater risk. Ethn Dis. 2010;20:370–5.
Al-Sharbatti S, Shaikh R, Mathew E, Sreedharan J, Muttappallymyalil J, Basha S. The Use of Obesity Indicators for the Prediction of Hypertension Risk among Youth in the United Arab Emirates. Iran J Public Health. 2011;40:33–40.
Panagiotakos DB, Chrysohoou C, Pitsavos C, Skoumas J, Lentzas Y, Katinioti A, et al. Hierarchical analysis of anthropometric indices in the prediction of 5-year incidence of hypertension in apparently healthy adults: the ATTICA study. Atherosclerosis. 2009;206:314–20.
Lee CM, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61:646–53.
Can AS, Bersot TP, Gönen M, Pekcan G, Rakıcıoğlu N, Samur G, et al. Anthropometric indices and their relationship with cardiometabolic risk factors in a sample of Turkish adults. Public Health Nutr. 2009;12:538–46.
Anyanwu GE, Ekezie J, Danborno B, Ugochukwu AI. Body size and adiposity indicators and their relationship with blood pressure levels in Ibos of Nigeria. Niger J Med. 2011;20:44–51.
Zhou Z, Hu D, Chen J. Association between obesity indices and blood pressure or hypertension: which index is the best? Public Health Nutr. 2009;12:1061–71.
Wai WS, Dhami RS, Gelaye B, Girma B, Lemma S, Berhane Y, et al. Comparison of measures of adiposity in identifying cardiovascular disease risk among Ethiopian adults. Obesity (Silver Spring). 2012;20:1887–95.
Rodrigues SL, Baldo MP, Mill JG. Association of waist-stature ratio with hypertension and metabolic syndrome: population-based study. Arq Bras Cardiol. 2010;95:186–91.
Tuan NT, Adair LS, Stevens J, Popkin BM. Prediction of hypertension by different anthropometric indices in adults: the change in estimate approach. Public Health Nutr. 2010;13:639–46.
Kaur P, Radhakrishnan E, Sankarasubbaiyan S, Rao SR, Kondalsamy-Chennakesavan S, Rao TV, et al. A comparison of anthropometric indices for predicting hypertension and type 2 diabetes in a male industrial population of Chennai, South India. Ethn Dis. 2008;18:31–6.
Silva DA, Petroski EL, Peres MA. Accuracy and measures of association of anthropometric indexes of obesity to identify the presence of hypertension in adults: a population-based study in Southern Brazil. Eur J Nutr. 2013;52:237–46.
Ko GT, Chan JC, Cockram CS, Woo J. Prediction of hypertension, diabetes, dyslipidemia or albuminuria using simple anthropometric indexes in Hong Kong Chinese. Int J Obes Relat Metab Disord. 1999;23:1136–42.
Chagas P, Caramori P, Barcellos C, Galdino TP, Gomes I, Schwanke CH. Optimal cut-off values of anthropometric markers to predict hypertension in North Indian population. Arq Bras Cardiol. 2011;97:397–401.
Ostchega Y, Hughes JP, Terry A, Fakhouri TH, Miller I. Abdominal Obesity, Body Mass Index, and Hypertension in US Adults: NHANES 2007–2010. Am J Hypertens. 2012;25:1271–8.
Lin JD, Chiou WK, Weng HF, Tsai YH, Liu TH. Comparison of three-dimensional anthropometric body surface scanning to waist-hip ratio and body mass index in correlation with metabolic risk factors. J Clin Epidemiol. 2002;55:757–66.
Lapidus L, Bengtsson C, Larsson B, Pennert K, Rybo E, Sjöström L. Distribution of adipose tissue and risk of cardiovascular disease and death: a 12 year follow up of participants in the population study of women in Gothenburg. Sweden Br Med J (Clin Res Ed). 1984;289:1257–61.
Funding statement
This work was supported by grants from the National Natural Science Fund (No.81102191) of China. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests. All authors had access to the data and were involved in drafting the article and revising it critically for important intellectual content.
Authors’ contributions
In our work, SW and FX conducted the study design, the statistical analysis and wrote the manuscript. YL and HJ helped the study design, FL carried out data analysis and LL helped to write the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wang, S., Liu, Y., Li, F. et al. A novel quantitative body shape score for detecting association between obesity and hypertension in China. BMC Public Health 15, 7 (2015). https://doi.org/10.1186/s12889-014-1334-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-014-1334-5