Abstract
Purpose of Review
To provide an update on current obesity prevalence trends and summarize the available evidence suggesting a possible plateau or stabilization in obesity rates after the previous sudden global rise.
Recent Findings
The escalating global obesity epidemic represents one of the most serious public health challenges. There have been some indications that in high-income populations, the rate of obesity increase in adults has been stabilized after the decade 2000–2010, suggesting a possible plateau. Current evidence also suggests that obesity rates have been stabilized in children and adolescents of most economically advanced countries since 2000, which is possibly related to healthier dietary habits and increased levels of physical activity. On the other hand, there is a steady uninterrupted rise in low-income nations, and the universal trend is obesity escalation rather than slowdown, mainly driven by sharp increases in the obesity prevalence of low-income populations. Furthermore, an increasing number of high- and middle-income countries are currently experiencing an epidemic of severe obesity. In high-income populations, severe obesity is expected to double its prevalence from 10 to 20% between 2020 and 2035, posing an enormous threat for healthcare systems. Even if transiently stabilized, the obesity prevalence remains globally at unacceptably high levels, and there is no guarantee that the current stability (if any) will be maintained for long.
Summary
In this review, we explore the underlying drivers of the global obesity epidemic; we provide possible explanations for the reported slowdown of the obesity rates in some countries; and we overall take a critical perspective on the obesity plateau hypothesis, emphasizing the urgent need for immediate effective actions at population and regional level in order to halt the alarming obesity escalation and its serious health risks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The escalating global increase in obesity, also referred to as “globesity,” represents one of the most serious public health challenges for societies and healthcare systems. In recognition of the overwhelming consequences of the rising obesity prevalence worldwide, obesity was declared as an epidemic by the World Health Organization (WHO) in 1997 [1]. Obesity is a complex, multifactorial, often relapsing, and difficult-to-treat chronic disease which is associated with significant morbidity and mortality, ranging from premature death to chronic conditions such as diabetes, cardiovascular diseases, and malignancies, which may severely compromise patients’ life expectancy and their overall quality of life [2]. In epidemiological terms, obesity is more common in women, socioeconomically disadvantaged racial/ethnic groups, and in individuals with lower education [3]. In low-income countries, obesity primarily affects middle-aged wealthy subjects, especially women from urban regions, whereas in high-income countries, obesity affects both sexes and all age groups, but with disproportionately greater impact in groups of lower socioeconomic status (SES) [4].
According to the World Obesity Atlas 2023 report, 38% of the global population are currently either overweight or obese [5••], having a body mass index (BMI) higher than 25 kg/m2. By 2035, the global overweight and obesity prevalence is projected to reach 51%, with South Pacific Islands leading the course of the obesity epidemic [5••]. Even more strikingly, by 2030, 78% of the US adults are projected to be overweight/obese [6••]. It has been estimated that obesity is expected to cost global economy more than four trillion US dollars of potential income in 2035, which is nearly 3% of current global gross domestic product (GDP), largely comparable to the financial impact of coronavirus 19 (Covid-19) pandemic in 2020 [5••]. All these ominous estimates and projections have been based on global and regional obesity trends between years 1975 and 2016. Not only adults but also the youth, namely children and adolescents, have been severely afflicted by the obesity epidemic. Over the last three decades of the twentieth century, a two- to three-fold increase in the prevalence of overweight and obesity has been reported in children of school age in several developed regions of the world [7]. Within Europe, Southern countries seem to have the highest overweight and obesity prevalence both in children/adolescents and in adults [8, 9•, 10•]. Particularly in Greece, one of the most affected European countries, the prevalence of adult obesity is expected to approach 40% in 2035 having a very high annual increase rate in both children and adults of approximately 2% [5••].
Both developed and developing countries are overwhelmed by obesity. Although current trends show a steady sharp increase in obesity prevalence in low- and middle-income countries [11], there have been some indications that in high-income countries, the rate of obesity increase has been stabilized after the decade 2000–2010, suggesting a possible plateau [12,13,14,15]. There have been also some encouraging reports for stable or even declining obesity rates in children and adolescents in high-income countries, reinforcing the obesity plateau theory also in the young populations [16,17,18,19,20,21]. The investigation of secular changes of obesity trends provides an invaluable opportunity for elucidating the complex dynamics of the epidemic and identifying its causal determinants. In case the pattern of exposure to a putative cause of obesity parallels the observed change in obesity trend over time, then this factor would represent an appropriate candidate to be further scrutinized for its potential causative role in obesity pathogenesis.
The aim of the present narrative review is to provide an update on current obesity prevalence trends and summarize the available evidence suggesting a possible plateau or stabilization in obesity rates after the previous sudden global rise. In this review, we analyze the underlying drivers of the global obesity epidemic, we provide possible explanations for the reported slowdown of the obesity rates in some countries, and we take overall a critical perspective on the obesity plateau hypothesis, emphasizing the urgent need for immediate effective actions at population and regional level in order to halt the alarmingly escalating obesity epidemic.
Methods of Literature Search and Review Criteria
For the preparation of this narrative review, we applied the search terms “obesity,” “overweight,” “central obesity,” “trends,” “trajectories,” “epidemic,” “pandemic,” “epidemiology,” “plateau,” “stabilization,” and “levelling off” in all possible combinations, in order to retrieve available literature data from PubMed, Medline, and Google Scholar from inception until June 2023. We included papers written in English language that involved synthetic methodology, systematic reviews, and epidemiological reports based on national databases.
The Explosive Rise in Obesity Rates between 1970 and 2000 and its Causes
The rising tide of the obesity epidemic began almost simultaneously in most developed countries in the 1970s and 1980s [22]. One of the theories that has been proposed to explain the obesity surge in the last decades of the twentieth century in developed countries is the energy balance flipping point hypothesis [4]. According to this, there was a critical switch in energy balance in 1960s and 1970s in most high-income countries. In the first half of the twentieth century (1910–1960), also termed as “pull phase,” the increasing urbanization and use of machines (mechanization) reduced the energy expenditure requirements for daily living. This reduced physical activity-related energy expenditure pulled down energy intake, so that people moved and ate less, keeping obesity prevalence relatively stable. In the second half of the twentieth century (post-1960), however, termed also as “push phase,” people got access to cheap and tasty obesogenic foods which increased their body weight (gain weight phase). The increased body size affected upwards energy expenditure through increased resting metabolic rate, restoring thus the energy balance equation at a higher level. Although obesity was far more prevalent in most countries after 1960 compared to the preceding decades, an exponential increase in both adult and childhood obesity occurred in the early 1980s. This striking epidemic rise in obesity was paralleled by sharp increases in the caloric density of foods and the consumption of fats and refined carbohydrates [4, 23].
The global obesity epidemic has been causally associated with a series of powerful driving forces mainly related to the international food production and supply system, which interact with local environmental factors, resulting in large heterogeneity in obesity prevalence between different populations. Food production and supply have radically changed since 1980 in the direction of increased energy availability [24]. Improved food manufacturing and distribution systems and pervasive marketing campaigns have made unhealthy, energy-dense foods, widely accessible even to lower-income populations [24]. More and more people gained abruptly access to cheap, palatable, highly processed foods of minimal nutritional quality. Furthermore, a number of obesogenic chemicals with endocrine-disrupting properties such as plastics, fertilizers, insecticides, and additives have gradually entered the global food chain, interfering possibly with human metabolism [24]. With regard to the environmental variables, an important condition for the development of obesity in a population is sufficient wealth and economic prosperity, although obesity can also develop in poor populations. Other important environmental determinants of obesity comprise the built environment (fast food restaurants, supermarkets, parks, transportation facilities) and sociocultural and socioeconomic conditions [25]. These local conditions act upon a population to either amplify or attenuate the effect of global drivers on obesity trends and serve as potent modulators of the slope of the obesity rise in distinct populations. Of note, different countries display different obesity trajectories based on unique sets of socioeconomic and cultural factors.
The attempts to explain the massive increases in obesity rates over the last decades of the twentieth century have mainly focused on a number of potential contributing factors, such as the increased caloric intake, changes in the dietary composition, declining levels of physical activity, and alterations in the gut microbiome [26,27,28,29,30]. The relative contribution of increased energy intake versus decreased energy expenditure in particular has been a matter of rigorous debate among researchers [28, 31,32,33,34]. Most evidence suggests that the increased energy intake constitutes the major underlying driving force of the obesity epidemic, and reduced physical activity contributes to a lesser extent. It has been shown that the increased food energy supply since 1970s and 1980s has been of sufficient magnitude to explain almost entirely the rise in obesity both in the USA [32] and in the UK [35]. The marked increases in caloric intake have been further related to increased portion sizes, massive production of low-cost, ultra-processed, calorie-dense foods, and increased snacking [36]. Changing trends in several aspects of daily physical activity, although of less impact on the course of the obesity epidemic compared to increased energy intake, can also explain some part of the obesity escalation. In the last decades, there has been an increase in leisure time (recreational) physical activity, but household and workplace-related physical activity have both decreased, and sedentary time spent in front of television and computer devices has increased [30, 37]. These changes may accentuate the adverse effect of increased energy intake on the obesity epidemic.
The Evolution Stages of the Obesity Epidemic: the “Obesity Transition” Theory
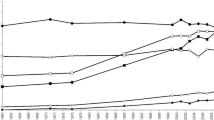
The “obesity transition” theory is a conceptual model which was proposed to describe the evolving characteristics of obesity epidemiology in different countries depending on the stage of their economic progression and development [38••]. According to this concept, the global obesity epidemic has evolved across four distinct stages, as graphically illustrated in Fig. 1. In Stage 1, populations are poor and afflicted by wars; the overall obesity rates are low, but the obesity prevalence starts slowly to rise among wealthy middle-aged subjects, especially women, and is much higher in adults than children. Many developing countries of South Asia and sub-Saharan Africa are currently at this stage. In Stage 2, as countries become richer, the obesity rates continue to increase: more in adults than in children, there is a faster transition in women compared to men due to their different adipose tissue physiology, but men start also to gain weight. At this stage, obesity shows a clear increasing trend in groups of lower SES. Many Latin American and Middle Eastern countries are currently at this stage. High-income East Asian countries are also at this stage, but with a lower prevalence of obesity. In Stage 3, the obesity prevalence gap between men and women becomes narrower, and the socioeconomic gradient becomes more pronounced with continuously rising obesity rates predominantly among people of lower income. At this point, obesity rises massively and takes on epidemic proportions. In children and women of high SES, obesity rates remain stable (plateau). Most European countries are now at this stage. Finally, in Stage 4, the obesity prevalence starts to decline, usually after a period of previous stabilization. Of note, no country shows currently decreasing trends or is projected to reduce its obesity prevalence in the near future across their entire population [5••, 38••].
Evidence for Levelling Off of Obesity Rates in Adults
Table 1 summarizes the most representative studies (mainly systematic reviews and national epidemiological reports) providing evidence for or against a plateau in obesity prevalence in adults as well as in children and adolescents [6••, 11,12,13,14,15,16,17, 19,20,21, 39,40,41,42,43,44,45,46,47,48].
A systematic analysis of global and regional prevalence of obesity in adults in the time frame between 1980 and 2013 has demonstrated steadily increasing obesity rates in both men and women in most regions of the world until 2006, but after that time point, a stabilization of obesity rates was observed, and there was some evidence that the increases that began in the 1980s started to attenuate in some developed countries [12]. These data were in line with a previous similar systematic analysis of national health examination surveys conducted in nearly 200 countries between 1980 and 2008, which showed flat and even decreasing obesity prevalence trends in women of Central and Eastern Europe [13].
A pooled analysis of population-based studies with measured weight and height in nearly 20 million participants from all around the world estimated BMI temporal trends between 1975 and 2014 and provided some preliminary evidence that the slope of BMI increase seemed to decline in most high-income countries after the year 2000 [11]. More specifically, this analysis has shown that after the year 2000, the rate of BMI increase was slower in both sexes in Oceania and most developed countries as well as in women of Latin America and Caribbean compared to the preceding 25 years. However, over the same period, the rate of BMI increase accelerated for men in Central and Eastern Europe, people of Southeast Asia, and most countries of Latin America and Caribbean, suggesting that the overall global obesity rates increased rather than slowed down [11]. Despite the apparent flattening of the BMI increase curve in most high-income countries post-2000, the final conclusion of this analysis performed by the Non-Communicable Diseases Risk Factor Collaboration study group (NCD-RisC) was that BMI had been still increasing alarmingly on a global scale [11]. The global age-standardized mean BMI increased from 21.7 to 24.2 kg/m2 between 1975 and 2014 in men and from 22.1 to 24.4 kg/m2 in women. Interestingly, the global prevalence of underweight decreased from 13.8 to 8.8% in men and from 14.6 to 9.7% in women, whereas the global prevalence of obesity increased from 3.2 to 10.8% in men and from 6.4 to 14.9% in women over four decades [11]. Based on these estimations, the authors predicted that if post-2000 secular obesity trends were to continue, the global obesity prevalence would reach 18% in men and surpass 21% in women by the year 2025, while severe obesity would surpass underweight in women, suggesting a practically zero probability of achieving the target of halting the obesity rise globally by 2025 and reducing its prevalence to 2010 levels.
The turning point of year 2000 as the onset of stabilization of obesity rates has also been supported by another review for the American population, although in that review, an escalating trend in the obesity prevalence in some European and Asian countries was also shown, with levelling off being less evident in low-SES countries [14]. Of note, no plateau in obesity was observed for Mexican–American people in the latter review, but only continuous increases [14]. Another longitudinal study in a large number of Swiss male conscripts provided clear indications for BMI stabilization at high levels and no further increases since 2010 [15].
On the other hand, some epidemiological analyses do not confirm an obesity plateau in adults. An analysis of large nationally representative databases in the USA has shown that obesity prevalence has steadily increased since 1999 with considerable differences according to sex, ethnicity, SES, and geographical variability [6••]. In men, the obesity prevalence was transiently stabilized in 2009–2012 at the high level of 33.7%, but resumed the increase to 38% in years 2015–2016 [6••]. In women, no temporary pause was observed but there was a rather continuous increase in obesity prevalence since 1999, reaching 41.5% in years 2015–2016 [6••]. This analysis has further shown that the prevalence of central obesity has consistently increased since 1999 in both sexes and was projected to reach 55.6% in men and 80% in women by the year 2030 [6••].
Evidence for Levelling Off of Obesity Rates in Children and Adolescents
As early as in the beginning of 2007, Mitchell et al. reported for the first time a levelling off of the obesity epidemic in Scottish children of primary school age [16]. Since then, a considerable number of national epidemiological studies and systematic reviews have consistently shown that obesity rates have remained stable or even decreased since early 2000s in children and adolescents from Australia, Europe, Russia, Japan, and the USA [14, 17, 19, 39,40,41,42,43,44,45,46,47, 49,50,51,52]. Well-designed studies from Australia, Denmark, England, France, Greece, the Netherlands, Sweden, and the USA have provided high quality evidence for a stabilization of obesity rates in children and adolescents since 2000 [17, 19, 39,40,41,42,43,44,45,46,47, 49]. In Swedish schoolchildren, the prevalence of obesity showed no significant increases across six municipalities over the period 1999–2005, and there was also a trend for reversal of the epidemic in girls preferentially, especially in urban regions of Sweden, suggesting possible sex-specific differences in childhood obesity trends over time [20]. In the same direction, an Irish systematic review reported a slightly decreasing prevalence of obesity in primary school children over the decade 2002–2012 in the Republic of Ireland [21]. In the nationally based studies analyzed in this review, the obesity prevalence remained stable at 7% between years 2002 and 2008 and declined to 4% thereafter [21]. In line with findings in children, a Greek study in a nationally representative sample of adolescents aged 12–19 years old has shown a levelling off in the pooled prevalence of overweight and abdominal obesity during the course of adolescence [48]. Overall, current evidence suggests that obesity rates have been stabilized, albeit at high levels, in children and adolescents of most economically advanced countries since 2000. Of note, although obesity plateau is experienced by children and adolescents of all socioeconomic backgrounds, it becomes less evident in those of lower SES, since socioeconomic inequalities in obesity prevalence have been widened in many countries post-2000 [53].
Possible Explanations for the Obesity Plateau Theory
Several hypotheses have been proposed to explain the presumed stabilization of adult obesity prevalence in developed countries. According to one of these, obesity has reached a biological limit in these countries, namely a saturation threshold for the proportion of people who can become obese, beyond which no further increase in its prevalence can occur. In other words, nearly all people who were genetically susceptible to gain excess weight and display behavioral patterns related to obesity have become obese already, and hence, there is too little space for further increases.
Another possible explanation relates to the market penetration. In high-income countries, the consumption of highly processed foods has been consistently elevated for several decades and is not expected to change any further in the future.
It has been further suggested that the obesity plateau could be the result of effective public health campaigns to increase awareness of the population, but also that of successful public health interventions and prevention policies. Promoting healthier food choices, implementing taxes for unhealthy foods, facilitating access to recreational facilities, and promoting supporting environments for physical activity might have had an impact on obesity rates. Indeed, the altered slope of the obesity rise in some countries may reflect an increased public awareness of the adverse health consequences of obesity, driven mainly by the substantial press attention to obesity since 2000. In support of this constantly increasing media attention hypothesis, it has been shown that media coverage of obesity has significantly increased in UK newspapers between 1996 and 2010, focusing more on societal rather than individual solutions [54]. However, public health campaigns and interventions targeting the obesity epidemic, especially population-based health education strategies, have not proven successful [55]. A systematic review evaluating the effectiveness of policies to combat the obesity epidemic in adults has found no evidence that policies intending to promote physical activity and healthy eating exert clinically meaningful beneficial effects on body weight outcomes [56]. Long-term sustainability, affordability, and stigmatization of people with obesity represent major challenges. To date, there is little evidence of successful community-based interventions able to reduce exposure to obesogenic stimuli and improve population health, and their impact on curbing the obesity epidemic and improving overall health outcomes has not been as expected [55]. Obesity prevention policies have mostly failed at implementation level because most of them have been designed as mainly to require individual responsibility and behavioral modification, rather than tackle the obesity structural (environmental) determinants [57••]. There have been some exceptions to this, such as Denmark and New York City initiatives, which implemented drastic restrictions in the use of trans fatty acids in food production by strict regulatory legislation [58], but the exceptions do not confirm the rule in this case.
With regard to the obesity plateau in children and adolescents, which is more solidly substantiated by literature compared to the presumed obesity plateau in adults, it has been speculated that the adoption of healthier dietary habits such as stable or decreasing trends in sweet drink consumption as reported for example for Australian children and adolescents between 2003 and 2008 [59], increased intake of fruits and fresh vegetables [20], constant or decreasing consumption of sweetened beverages and candies [20, 60], reduced intake of solid margarines [20], and breakfast eating [60] may partly account for the observed stagnation in obesity rates in youth of developed countries. It has been further suggested that increased physical activity and decreased sedentary time by less television viewing may also partly explain the obesity plateau in adolescents [60]. Increased media attention and local public health activities could also play a role.
A Critical Perspective on Current Obesity Trends: Have We Really Hit a Plateau?
Although there are some indications that obesity rates have plateaued at very high levels in some developed countries, there is a steady uninterrupted rise in low-income nations, and the universal trend is obesity escalation rather than slowdown, mainly driven by steep increases in obesity prevalence in low- and middle-income populations [6••, 11]. Furthermore, an increasing number of high- and middle-income countries are now experiencing an epidemic of severe obesity [11], which is often underappreciated but is extremely serious from a public health point of view. There has been a right shift in the BMI distribution curve in the USA between 1980 and 2017, and severe obesity is currently estimated at 20% of the American population and projected to climb to 36% by 2035, if current trends continue [5••]. In high-income populations, severe obesity is expected to double its prevalence from 10 to 20% between 2020 and 2035, posing an enormous threat for societies and healthcare systems [5••].
Another limitation of the studies suggesting an obesity plateau is that the prevalence of obesity was assessed with BMI, a crude anthropometric measure of adiposity, which is not able to capture all the variation in health outcomes related to adiposity [61]. Although BMI is considered an appropriate measure for monitoring the prevalence of obesity at the population level, it is not able to adequately reflect variations in body composition and fat distribution [61]. It could be thus speculated that obesity trends could have been different, if obesity had been defined by markers of central fat distribution such as waist circumference, waist-to-hip or waist-to-height ratio.
Furthermore, it is important to note that prevalence trends are not able to distinguish between changes in the incidence and changes in the duration of obesity cases. It is reminded at this point that the prevalence of a condition in a population is the product of its incidence and duration. So theoretically, the incidence rate of obesity could still be increasing during a period with seemingly stable obesity prevalence, if the average duration of the obesity cases has been reduced over time, either as a result of successful treatment (dietary, pharmacological, surgical) or due to premature mortality. It is likely that the observed stabilization of obesity rates in some countries is a result of changes in both incidence and duration. However, it is critical to disentangle the contribution of each component, both as a way of identifying possible successful public health initiatives and as a way to unravel the driving forces of the obesity epidemic. This would require a longitudinal approach with multiple sequential cohorts and repeated body weight measurements, which is not always feasible to perform.
Last but not least, a possible stabilization of obesity rates in some countries is under no circumstances synonymous or equivalent to reversal of the obesity epidemic. Even if temporarily stabilized, the obesity prevalence remains globally at unacceptably high levels, and there is no guarantee that the current stability (if any) will remain for long and the prevalence will not further increase in the future. In this context, it should be kept in mind that the obesity epidemic has evolved in a non-linear, stepwise, pattern in most countries over time [18, 62, 63]. This means that previous stable phases can be followed by further increases in the prevalence of obesity in the near or distant future, leaving no room for complacency and satisfaction. A typical example of this non-linear, stepwise, increase in the prevalence of obesity over time is Denmark, where the obesity epidemic developed over several sequential phases. In this case, a long stable phase was followed by the first peak related to birth cohorts from the early 1940s, which lasted about a decade and resulted in almost a tenfold increase in the prevalence of obesity. The latter increase was followed by another period of stability at the higher level, and subsequently, a second wave of BMI increase began with the birth cohorts from the early 1970s which was even steeper than the first [14].
Brief Overview of the Epidemiology of Major Obesity-Associated Comorbidities
The presumed plateau in obesity prevalence observed in some high-income countries is not confirmed in the epidemiology of major obesity-associated complications, although it should be noted that there is a lag time (time delay) between obesity and the manifestation of its adverse health consequences. Overall, the burden of major obesity-associated health problems such as type 2 diabetes mellitus (T2DM), metabolic syndrome (MS), and non-alcoholic fatty liver disease (NAFLD) is rising globally. In these trends, there is a strong impact of socioeconomic determinants of health, similar to obesity epidemiology.
In more detail, the mortality and disability related to obesity-associated T2DM have more than tripled over the period 1990–2019, with the most important upward trends reported for men, South Asia, low- and middle-income countries [64]. The burden of T2DM is rising fast in both developed and developing regions of the world, with an equal gender distribution and a peak of incidence at around 55 years of age [65]. Obesity and certain lifestyle factors, such as an unhealthy diet, smoking, and reduced physical activity, represent the major drivers of disability and mortality attributed to T2DM [66].
With regard to the global epidemiology of MS, it is noteworthy that its prevalence is often higher in urban regions of developing countries rather than in the developed world [67]. The prevalence of MS has increased from 28 to 37% during 1999–2018 in American adults, which was mainly driven by increases in the prevalence of elevated fasting glucose and obesity [68]. Only in American adolescents, the prevalence of MS remained stable at 4.36% over the same time period, but there was a notable increase in the prevalence of specific MS components such as an elevated waist circumference and hyperglycemia, especially in Mexican–American youth and adolescents of families with lower educational and socioeconomic level [69].
As far as the emerging NAFLD epidemic is concerned, global NAFLD prevalence has increased from 25% in 1990–2006 to 38% in 2016–2019, but its associated mortality and disability have both decreased [70, 71]. The affected regions in a descending order of magnitude of burden comprise: Latin America, Middle East and North Africa, South Asia, Southeast Asia, North America, East Asia, Asia Pacific, and Western Europe [70]. The highest prevalence, incidence, and mortality have been reported for middle-income countries [71]. The forecasted prevalence of NAFLD for year 2040 exceeds 50%, with an annual increase rate of 2.16% for the period 2020–2040 [72]. The projected NAFLD prevalence in 2040 is expected to be higher in males, but the steepest increasing trends have been reported for females and smokers [72].
Conclusions and Call for Future Actions
Taking all epidemiological evidence into consideration, it seems that there has been some stability in the prevalence of obesity in children and adolescents of most high-income populations, possibly related to their healthier dietary habits and increased levels of physical activity. However, the trends in adults are mixed and ambiguous and do not unequivocally support the obesity plateau hypothesis. Although there are some indications that adult obesity rates have plateaued at very high levels in some developed countries, current trends are far from being encouraging and reassuring, since there is a steady unmitigated rise of obesity in low-income nations, while an increasing number of high- and middle-income countries are currently confronted with an epidemic of severe obesity. Overall, the universal trend is obesity escalation rather than slowdown, mainly driven by the steep increases in the obesity prevalence of low- and middle-income populations. In view of these trends, which are graphically summarized in Fig. 2, it is nowadays more than ever imperative to sustain and intensify population-based strategies targeting the obesity epidemic. Unfortunately, current interventions have failed to impede the exponential rise in BMI in most countries. Interventions such as taxing unhealthy foods or making healthy foods cheaper have been evaluated in predictive models with encouraging results [73,74,75,76], but there has been little research and effort into changing the powerful sociocultural determinants of food choices and physical activity. In order to bring obesity rates down to acceptable levels and reach the less affluent socioeconomically deprived groups, multi-component initiatives at the individual and community level and population interventions requiring individuals to use a low level of individual agency to benefit are urgently needed. These efforts should definitely be reinforced by a stronger political will and determination.
According to the energy balance flipping point hypothesis, energy expenditure was the driving force for energy intake before 1960, but energy intake became a predominant force after 1960, driving energy expenditure. Although obesity was more prevalent in most countries after 1960 compared to the preceding decades, there was an exponential increase in both adult and childhood obesity rates in the early 1980s. This epidemic rise was paralleled by sharp increases in the caloric density of foods and the consumption of fats and refined carbohydrates (increased energy availability). There have been some indications that obesity rates have plateaued at high levels in some high-income countries after the decade 2000–2010, but on the other hand, there has been a continuous uninterrupted rise in low- and middle-income populations. Furthermore, the prevalence of severe obesity (BMI ≥ 35 kg/m2) is steadily increasing in a large number of countries. Even if transiently stabilized, the obesity prevalence remains at unacceptably high levels in high-income countries, and there is no guarantee that the current stability will be maintained for ever, and there will be no new wave of increase in the near or distant future.
Change history
17 October 2023
A Correction to this paper has been published: https://doi.org/10.1007/s13679-023-00533-0
Abbreviations
- BMI:
-
Body mass index
- EE:
-
Energy expenditure
- EI:
-
Energy intake
- HICs:
-
High-income countries
- LMICs:
-
Low- and middle-income countries
- WHO:
-
World Health Organization
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. Obesity : preventing and managing the global epidemic : report of a WHO consultation. World Health Organization; 2000.
Hruby A, Manson JE, Qi L, Malik VS, Rimm EB, Sun Q, et al. Determinants and consequences of obesity. Am J Public Health. 2016;106:1656–62.
Arroyo-Johnson C, Mincey KD. Obesity epidemiology worldwide. Gastroenterol Clin North Am. W.B. Saunders; 2016. p. 571–9.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. The Lancet. Elsevier B.V.; 2011. p. 804–14.
•• Lobstein T, Jackson-Leach R, Powis J, Brinsden H, Gray M. 2023. Available from: https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2023. Compiled by the World Obesity Federation, the World Obesity Atlas 2023 provides obesity prevalence projections and insights into the growing economic impact of overweight/obesity for the period 2020–2035. Alarmingly, over half of the global population is expected to have a high body mass index by the end of this period, and 1 in 4 people will be living with obesity compared to 1 in 7 today. Childhood obesity rates are rising very fast, and lower income countries are facing rapid increases in obesity prevalence.
•• Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2021;49:810–23. Based on large national databases, this analysis examined time trends in obesity prevalence across different socio-economic strata and geographic regions and made projections for the future course of the obesity epidemic in the USA. It was shown that obesity prevalence has been steadily rising since 1999, both in US adults and children/adolescents, despite some temporary stabilization (plateau) phases. There were great disparities across socioeconomic groups and geographical regions. The paper emphasized the need for effective, sustainable and culturally-tailored interventions.
Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25.
Wijnhoven TM, Van Raaij JM, Spinelli A, Starc G, Hassapidou M, Spiroski I, et al. WHO European childhood obesity surveillance initiative: Body mass index and level of overweight among 6–9-year-old children from school year 2007/2008 to school year 2009/2010. BMC Public Health. 2014;14.
• Touloumi G, Karakosta A, Kalpourtzi N, Gavana M, Vantarakis A, Kantzanou M, et al. High prevalence of cardiovascular risk factors in adults living in Greece: the EMENO National Health Examination Survey. BMC Public Health. 2020;20:1665. This paper presents national data on the prevalence of cardiovascular risk factors, including obesity, in Greek adults between 2013 and 2016, based on the findings of the national health examination survey EMENO. According to these data, the prevalence of obesity in the Greek adult population is alarmingly high.
• Siopis G, Moschonis G, Reppas K, Iotova V, Bazdarska Y, Chakurova N, et al. The emerging prevalence of obesity within families in Europe and its associations with family socio-demographic characteristics and lifestyle factors; a cross-sectional analysis of baseline data from the Feel4Diabetes Study. Nutrients. 2023;15:1283. This cross-sectional analysis of baseline data from the Feel4Diabetes Study, reported high obesity prevalence rates in Greek children of school age and examined the associations of obesity with sociodemographic and lifestyle characteristics of the affected families, emphasizing the need for tailored, family-based, interventions for obesity prevention.
Di Cesare M, Bentham J, Stevens GA, Zhou B, Danaei G, Lu Y, et al. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387:1377–96.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377:557–67.
Rokholm B, Baker JL, Sørensen TIA. The levelling off of the obesity epidemic since the year 1999-a review of evidence and perspectives. Obes Rev. 2010. p. 835–46.
Staub K, Bender N, Floris J, Pfister C, Rühli FJ. From undernutrition to overnutrition: the evolution of overweight and obesity among young men in Switzerland since the 19th century. Obes Facts. 2016;9:259–72.
Mitchell RT, McDougall CM, Crum JE. Decreasing prevalence of obesity in primary schoolchildren. Arch Dis Child. 2007;92:153–4.
Tambalis KD, Panagiotakos DB, Kavouras SA, Kallistratos AA, Moraiti IP, Douvis SJ, et al. Eleven-year prevalence trends of obesity in greek children: first evidence that prevalence of obesity is leveling off. Obesity. 2010;18:161–6.
Olds TS, Harten NR. One hundred years of growth: the evolution of height, mass, and body composition in Australian children, 1899–1999. Hum Biol. 2001;73:727–38.
Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–5.
Lissner L, Sohlström A, Sundblom E, Sjöberg A. Trends in overweight and obesity in Swedish schoolchildren 1999–2005: has the epidemic reached a plateau?: National prevalence of obesity. Obes Rev. 2010. p. 553–9.
Keane E, Kearney PM, Perry IJ, Kelleher CC, Harrington JM. Trends and prevalence of overweight and obesity in primary school aged children in the Republic of Ireland from 2002–2012: a systematic review. BMC Public Health. 2014;14.
Sassi F, Devaux M, Cecchini M, Rusticelli E. The obesity epidemic: analysis of past and projected future trends in selected OECD countries. 2009.
Centers for disease control and prevention (CDC). Trends in intake of energy and macronutrients--United States, 1971–2000. MMWR Morb Mortal Wkly Rep. 2004;53:80–2.
Zobel EH, Hansen TW, Rossing P, von Scholten BJ. Global changes in food supply and the obesity epidemic. Curr Obes Rep. 2016. p. 449–55.
Hruby A, Hu FB. The epidemiology of obesity: a big picture. pharmacoeconomics. Springer International Publishing; 2015. p. 673–89.
Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev. 1997;55:31–43.
Astrup A, Brand-Miller J. Diet composition and obesity. Lancet. 2012;379:1100; author reply 1100–1.
Prentice A, Jebb S. Energy intake/physical activity interactions in the homeostasis of body weight regulation. Nutr Rev. 2004;62:S98-104.
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21.
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6.
Swinburn B. Commentary: physical activity as a minor player in the obesity epidemic: what are the deep implications? Int J Epidemiol. 2013;42:1838–40.
Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009;90:1453–6.
Luke A, Cooper RS. Physical activity does not influence obesity risk: time to clarify the public health message. Int J Epidemiol. 2013;42:1831–6.
Blair SN, Archer E, Hand GA. Commentary: Luke and Cooper are wrong: physical activity has a crucial role in weight management and determinants of obesity. Int J Epidemiol. 2013;42:1836–8.
Scarborough P, Burg MR, Foster C, Swinburn B, Sacks G, Rayner M, et al. Increased energy intake entirely accounts for increase in body weight in women but not in men in the UK between 1986 and 2000. Br J Nutr. 2011;105:1399–404.
Finkelstein EA, Ruhm CJ, Kosa KM. Economic causes and consequences of obesity. Annu Rev Public Health. 2005. p. 239–57.
Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: what are the contributors? Annu Rev Public Health. 2005;26:421–43.
•• Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7:231–40. This paper described the evolving stages of obesity epidemiology in countries of different economic development by means of a four-stage conceptual model, the so-called “obesity transition model”. This model is intended to provide guidance to policy makers in identifying the current stage of the obesity transition in a population, and implementing preventive measures to attenuate the transition, taking into account local contextual factors.
Benson L, Baer HJ, Kaelber DC. Trends in the diagnosis of overweight and obesity in children and adolescents: 1999–2007. Pediatrics. 2009;123:e153–8.
Olds TS, Tomkinson GR, Ferrar KE, Maher CA. Trends in the prevalence of childhood overweight and obesity in Australia between 1985 and 2008. Int J Obes (Lond). 2010;34:57–66.
Stamatakis E, Zaninotto P, Falaschetti E, Mindell J, Head J. Time trends in childhood and adolescent obesity in England from 1995 to 2007 and projections of prevalence to 2015. J Epidemiol Community Health. 1978;2010(64):167–74.
Sjöberg A, Lissner L, Albertsson-Wikland K, Mårild S. Recent anthropometric trends among Swedish school children: evidence for decreasing prevalence of overweight in girls. Acta Paediatr. 2008;97:118–23.
Romon M, Lommez A, Tafflet M, Basdevant A, Oppert JM, Bresson JL, et al. Downward trends in the prevalence of childhood overweight in the setting of 12-year school- and community-based programmes. Public Health Nutr. 2009;12:1735–42.
Péneau S, Salanave B, Maillard-Teyssier L, Rolland-Cachera M-F, Vergnaud A-C, Méjean C, et al. Prevalence of overweight in 6- to 15-year-old children in central/western France from 1996 to 2006: trends toward stabilization. Int J Obes (Lond). 2009;33:401–7.
Pearson S, Hansen B, Sørensen TIA, Baker JL. Overweight and obesity trends in Copenhagen schoolchildren from 2002 to 2007. Acta Paediatr. 2010;99:1675–8.
Kolle E, Steene-Johannessen J, Holme I, Andersen LB, Anderssen SA. Secular trends in adiposity in Norwegian 9-year-olds from 1999–2000 to 2005. BMC Public Health. 2009;9:389.
de Wilde JA, van Dommelen P, Middelkoop BJC, Verkerk PH. Trends in overweight and obesity prevalence in Dutch, Turkish, Moroccan and Surinamese South Asian children in the Netherlands. Arch Dis Child. 2009;94:795–800.
Grammatikopoulou MG, Poulimeneas D, Gounitsioti IS, Gerothanasi K, Tsigga M, Kiranas E. Prevalence of simple and abdominal obesity in Greek adolescents: the ADONUT study. Clin Obes [Internet]. 2014;n/a-n/a. Available from: https://onlinelibrary.wiley.com/doi/10.1111/cob.12070.
Stamatakis E, Wardle J, Cole TJ. Childhood obesity and overweight prevalence trends in England: evidence for growing socioeconomic disparities. Int J Obes (Lond). 2010;34:41–7.
Bergström E, Blomquist HKS. Is the prevalence of overweight and obesity declining among 4-year-old Swedish children? Acta Paediatr. 2009;98:1956–8.
Schmidt Morgen C, Rokholm B, Sjöberg Brixval C, Schou Andersen C, Geisler Andersen L, Rasmussen M, et al. Trends in prevalence of overweight and obesity in danish infants, children and adolescents–are we still on a plateau? PLoS ONE. 2013;8: e69860.
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet [Internet]. 2017;390:2627–42. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673617321293.
Chung A, Backholer K, Wong E, Palermo C, Keating C, Peeters A. Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: a systematic review. Obes Rev. 2016;17:276–95.
Hilton S, Patterson C, Teyhan A. Escalating coverage of obesity in UK newspapers: the evolution and framing of the obesity epidemic from 1996 to 2010. Obesity. 2012;20:1688–95.
Walls HL, Peeters A, Proietto J, McNeil JJ. Public health campaigns and obesity-a critique. BMC Public Health. 2011;11:136.
Tseng E, Zhang A, Shogbesan O, Gudzune KA, Wilson RF, Kharrazi H, et al. Effectiveness of policies and programs to combat adult obesity: a systematic review. J Gen Intern Med. 2018;33:1990–2001.
•• Theis DRZ, White M. Is obesity policy in england fit for purpose? Analysis of government strategies and policies, 1992–2020. Milbank Q. 2021;99:126–70. This analysis found that government policies for obesity prevention and management in England lack implementation viability, that governments rarely evaluate previous strategies or learn from policy failures, that governments tend to adopt less interventional approaches, and that policies usually make high demands on individual agency, namely they rely on individuals to make behavioral changes rather than shape external influences, and are thus less likely to be effective.
Stender S, Dyerberg J, Astrup A. High levels of industrially produced trans fat in popular fast foods. N Engl J Med. 2006;354:1650–2.
Jensen BW, Nichols M, Allender S, De Silva-Sanigorski A, Millar L, Kremer P, et al. Consumption patterns of sweet drinks in a population of Australian children and adolescents (2003–2008). BMC Public Health. 2012.
Iannotti RJ, Wang J. Trends in physical activity, sedentary behavior, diet, and BMI among US adolescents, 2001–2009. Pediatrics. 2013;132:606–14.
Hruschka DJ, Hadley C. How much do universal anthropometric standards bias the global monitoring of obesity and undernutrition? Obesity Reviews. Blackwell Publishing Ltd; 2016. p. 1030–9.
Prentice AM, Jebb SA. Obesity in Britain: gluttony or sloth? BMJ. 1995;311:437–9.
Keith SW, Redden DT, Katzmarzyk PT, Boggiano MM, Hanlon EC, Benca RM, et al. Putative contributors to the secular increase in obesity: exploring the roads less traveled. Int J Obes (Lond). 2006;30:1585–94.
Uro-Chukwu H, Liu X, Malakan Rad E, Zeng Z, Hu B, Li Q. The global burden of type 2 diabetes attributable to high body mass index in 204 countries and territories, 1990–2019: an analysis of the Global Burden of Disease Study.
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Kaabi J Al. Epidemiology of type 2 diabetes-global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10:107–11.
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from, et al 1990 to 2025. Sci Rep. 2020;10.
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. Current Medicine Group LLC 1; 2018.
Yang C, Jia X, Wang Y, Fan J, Zhao C, Yang Y, et al. Trends and influence factors in the prevalence, intervention, and control of metabolic syndrome among US adults, 1999–2018. BMC Geriatr. 2022;22.
Liu J, Ma J, Orekoya O, Vangeepuram N, Liu J. Trends in metabolic syndrome among US youth, from 1999 to 2018. JAMA Pediatr. 2022;176:1043–5.
Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. 2023;77:1335–47.
Wang D, Xu Y, Zhu Z, Li Y, Li X, Li Y. Changes in the global, regional, and national burdens of NAFLD from, et al 1990 to 2019: a systematic analysis of the global burden of disease study 2019. Front Nutr. 2022;9.
Nguyen MH, Le MH, Yeo YH, Zou B, Barnet S, Henry L, et al. Forecasted 2040 global prevalence of nonalcoholic fatty liver disease using hierarchical Bayesian approach. Clin Mol Hepatol. 2022;28:841–50.
Ni Mhurchu C, Blakely T, Jiang Y, Eyles HC, Rodgers A. Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. Am J Clin Nutr. 2010;91:736–47.
Brownell KD, Frieden TR. Ounces of prevention–the public policy case for taxes on sugared beverages. N Engl J Med. 2009;360:1805–8.
Mytton O, Gray A, Rayner M, Rutter H. Could targeted food taxes improve health? J Epidemiol Community Health. 1978;2007(61):689–94.
Sacks G, Veerman JL, Moodie M, Swinburn B. “Traffic-light” nutrition labelling and “junk-food” tax: a modelled comparison of cost-effectiveness for obesity prevention. Int J Obes (Lond). 2011;35:1001–9.
Funding
Open access funding provided by HEAL-Link Greece.
Author information
Authors and Affiliations
Contributions
C.K. searched literature, wrote the main manuscript text and prepared Table 1, and Figs. 1 and 2. M.D. edited the manuscript and provided critical input. S.L. searched literature, critically reviewed and edited the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koliaki, C., Dalamaga, M. & Liatis, S. Update on the Obesity Epidemic: After the Sudden Rise, Is the Upward Trajectory Beginning to Flatten?. Curr Obes Rep 12, 514–527 (2023). https://doi.org/10.1007/s13679-023-00527-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-023-00527-y