Abstract
Purpose
The previous studies that examined the effectiveness of unsupervised machine learning methods versus traditional methods in assessing dietary patterns and their association with incident hypertension showed contradictory results. Consequently, our aim is to explore the correlation between the incidence of hypertension and overall dietary patterns that were extracted using unsupervised machine learning techniques.
Methods
Data were obtained from Japanese male participants enrolled in a prospective cohort study between August 2008 and August 2010. A final dataset of 447 male participants was used for analysis. Dimension reduction using uniform manifold approximation and projection (UMAP) and subsequent K-means clustering was used to derive dietary patterns. In addition, multivariable logistic regression was used to evaluate the association between dietary patterns and the incidence of hypertension.
Results
We identified four dietary patterns: ‘Low-protein/fiber High-sugar,’ ‘Dairy/vegetable-based,’ ‘Meat-based,’ and ‘Seafood and Alcohol.’ Compared with ‘Seafood and Alcohol’ as a reference, the protective dietary patterns for hypertension were ‘Dairy/vegetable-based’ (OR 0.39, 95% CI 0.19–0.80, P = 0.013) and the ‘Meat-based’ (OR 0.37, 95% CI 0.16–0.86, P = 0.022) after adjusting for potential confounding factors, including age, body mass index, smoking, education, physical activity, dyslipidemia, and diabetes. An age-matched sensitivity analysis confirmed this finding.
Conclusion
This study finds that relative to the ‘Seafood and Alcohol’ pattern, the ‘Dairy/vegetable-based’ and ‘Meat-based’ dietary patterns are associated with a lower risk of hypertension among men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension has been recognized as a serious health risk [1], affecting a staggering number of over 1.1 billion individuals [2]. Especially uncontrolled hypertension is a risk factor for future cardiovascular diseases globally [3]. Patients with hypertension were estimated as 43 million in Japan [4,5,6]. Hypertension is a complex condition influenced by genetic and environmental factors, but environmental factors play a primary role in its development and progression [7, 8]. Therefore, mitigating the effects of environmental factors to minimize or delay the development of hypertension is a significant challenge in hypertension management and prevention policies.
Dietary factors have been intensively investigated as one of the environmental factors associated with the risk of hypertension [9, 10]. To simplify the situation, many studies have focused on the relationship between the risk of hypertension and particular foods or nutrients [11], particularly the effect of a single nutrient, food, or food group. However, this approach has several limitations because foods and nutrients are generally consumed with interactive or synergistic effects [12]. Some healthy dietary patterns (e.g., a healthy diet with the consumption of nuts and seeds, low-fat dairy products, vegetables, fruits, poultry, and fish; and an unhealthy diet with foods such as red meat, fast food, high-fat dairy products, refined grain, salty snacks, and drinks, etc.) are associated with a lower blood pressure and risk of hypertension [13,14,15,16]. Generally, a dietary pattern is a comprehensive variable that integrates the consumption of several food groups. For instance, the ‘fruit and milk’ pattern was associated with a lower prevalence of hypertension among adult Chinese men [14], and the traditional Japanese diets, which are characterized by high consumption of vegetables, seaweeds, mushrooms, potatoes, fruits, fish, and soybeans including tofu and miso, were significantly related to lower blood pressure [15, 17].
Furthermore, dietary behavior (e.g., more frequent meals at home, eating speed, or skipping breakfast) and cooking methods (e.g., boiling or frying) influence hypertension [18,19,20,21]. Food and taste preferences could also impact hypertension. For instance, it has been reported that the frequency of dairy product consumption is related to a risk of hypertension [19] and that reducing salt and seasoning consumption significantly improves blood pressure [20]. The combination of food intake, dietary behavior, and cooking methods has been shown to affect the disease risk more than any single nutrient [18, 22]. Therefore, a more holistic approach is needed to capture the dietary tendency or patterns, including food items, dietary behaviors, and cooking methods.
Two main approaches used to extract dietary patterns are hypothesis-driven and data-driven approaches [23,24,25]. The first approach aims to calculate a graded score or index based on recommended diets or dietary guidelines [26, 27]. However, the hypothesis-driven approaches have two limitations: (1) they do not consider the correlation structure between food frequency intake and dietary habits (dietary behavior and cooking methods), and (2) they reflect only the individual effects of each food or nutrient without considering how they interact with each other within a diet [28]. The data-driven approach, also known as the a posteriori or exploratory approach, involves extracting dietary patterns from the data [26]. This approach uses statistical exploratory procedures such as principal component analysis (PCA) [13, 16], cluster methods [29] and factor analysis [15], which are widely applied in nutritional epidemiology. PCA is a commonly used data-driven method to derive dietary patterns [30, 31]; however, despite its popularity in dietary pattern studies, it has several limitations. Although PCA has been used for the dimension reduction of multidimensional datasets, the procedure generally results in a loss of information [32]. Furthermore, the standard PCA cannot analyze nonlinear relationships [33] or categorical data reported as dietary habits, such as dietary behavior and cooking methods.
Unsupervised machine learning analysis is a recent procedure for data-driven approaches to identify dietary patterns [34]. This approach has recently been applied in some studies to reveal different dietary patterns [35, 36]. Unsupervised machine learning techniques for clustering and dimensionality reduction algorithms [37] can be used to overcome some PCA limitations and improve the results. Uniform manifold approximation and projection (UMAP) is a nonlinear technique capable of preserving the global structure of the data, making it well suited for use in unsupervised clustering applications [38]. Compared with PCA, UMAP has the advantage of handling categorical variables and preserving relationships between categorical variables and other features in the data [39]. UMAP makes it an attractive option for unsupervised clustering, where the goal is to identify patterns and relationships in the data without needing prior knowledge or labeled data. Therefore, combining food intake, dietary behavior, and cooking methods based on unsupervised technique analysis may be more suitable for deriving dietary patterns.
The first purpose of this study was to derive dietary patterns among Japanese men based on a brief-type self-administered diet history questionnaire (BDHQ) dataset using unsupervised machine learning. The second purpose was to examine the association between extracted clusters of dietary patterns and the incidence of hypertension to show the validity of the novel method for identifying dietary patterns. We show here how these UMAP-identified patterns are associated with incidence of hypertension among Japanese male population. Furthermore, in this study, we will explore how these identified dietary patterns are linked to the incidence of hypertension among the Japanese population. Our study would provide helpful insights into dietary interventions for the prevention of hypertension in Japanese males.
Methods
Participants and selection design
This study used data from the Oroshisho study, a longitudinal study of the lifestyle-related influences on chronic noncommunicable diseases and health status of 1,253 individual Japanese adult employees working at Sendai Oroshisho Center Sendai, conducted between 2008 and 2011. Details of the Oroshisho study have been described previously [40]. The protocol for the current study was approved by the Institutional Review Board of Tohoku University School of Medicine (Approval Number: 2019-1-394).
The 2008 dataset was used as the baseline. The selection procedure for the participants is presented in Fig. 1. Briefly, we recruited 1,253 individuals at baseline who underwent an annual health examination. Our study employed data collected in 2008 (as a baseline) and 2010 (as a follow-up). Of the participants, 1154 provided written informed consent to participate in the study, resulting in a 92.1%. Female participants (n = 295) were also excluded from the analysis due to their sample size, low prevalence, and, especially, sex-related difference in the risk of hypertension, which was demonstrated by a recent meta-analyses [41]. Among the excluded participants, 68 individuals were removed from the analysis due to incomplete baseline data, including missing dietary information (n = 16) and incomplete health examination records (n = 52). Additionally, a total of 344 individuals were excluded from the analysis due to incomplete baseline data, which included the presence of heart disease (n = 9), systolic blood pressure ≥ 140 mmHg (n = 188), diastolic blood pressure ≥ 90 mmHg (n = 39), self-reported history of previously diagnosed hypertension or current medication for hypertension at the health examination (n = 44), and failure to undergo follow-up examinations during the study period (n = 64). We did not include data from 2011 because some participants may have changed their dietary habits due to the 2011 Great East Japan Earthquake in March 2011. It was possible that the study participants have chosen to eat less seafood than before, considering the risk of potential contamination of agricultural and fishery products due to the Fukushima nuclear plant accident. Finally, 447 male participants were included in the final analysis (Fig. 1).
Blood pressure measurement and hypertension diagnosis
Systolic and diastolic blood pressures were measured in the upper right arm using an automatic device (Yamasu 605P; Kenzmedico, Saitama, Japan) in a sitting position according to our previous study [42]. According to the study protocol, a participant with a systolic blood pressure of > 150 mmHg or diastolic blood pressure of > 100 mmHg at the initial measurement was considered to undergo a second measurement. In such case, the blood pressure values of the second measurement were adopted. Hypertension was defined as a systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, self-reported history of hypertension, or use of medication for hypertension. Individuals without hypertension at baseline (2008) were considered to have incident hypertension when they met any of these conditions during the subsequent health checkups from August 2009 to August 2010.
Analysis of dietary habits
Information about dietary habits was obtained through the BDHQ [43]. In the BDHQ, 79 items were inquiries about food intake of 58 different food items, 12 dietary behavior, and 9 cooking methods. For food intakes, the participants indicated their mean frequency of consumption in terms of the specified serving size by checking one of seven frequency categories ranging from ‘almost never’ to ‘two or more times/day.’ For alcohol items, the participants indicated their mean frequency of consumption in terms of the specified serving size by checking one of seven frequency categories ranging from ‘almost never’ to ‘four cups or more times/day.’ For beverage items, the participants indicated their mean frequency of consumption in terms of the specified serving size by checking one of eight frequency categories ranging from ‘almost never’ to ‘four cups or more times/day.’ Twelve dietary behaviors include 1: noodle soup meals, 2: taste of seasonings at home compared to eating out, 3: preference for the meat fat (beef and pork), 4: frequency of breakfast consumption, 5: amount of soy sauce or equivalent used for their meals, 6: frequency of soy sauce or equivalent used for meals, 7: number of side dishes at home compared to eating out, 8: amount of rice at home compared to eating out, 9: eating speed of meals, 10: intentional alterations in their eating habits using, 11: dietary supplements, and 12: receiving dietary guidance. Participants indicated a five-point scale from ‘do not like’ to ‘like very much’ for the noodle soup meals; a five-point scale from ‘light’ to ‘heavy’ for the taste of seasonings at home compared to eating out; a five-point scale from ‘do not eat’ to ‘like very much’ for the preference for the meat fat (beef and pork); a nine-point scale from ‘almost never’ to ‘daily’ for the frequency of breakfast consumption; a five-point scale from ‘very little’ to ‘very much’ for the amount of soy sauce or equivalent used for their meals; a five-point scale from ‘almost never’ to ‘always’ for the frequency of soy sauce or equivalent used for their meals; a five-point scale from ‘more at home’ to ‘more eating out’ for the number of side dishes at home compared to eating out and the amount of rice at home compared to eating out; a five-point scale from ‘very slow’ to ‘very fast’ for the eating speed of meals; a two-point scale choosing ‘positive’ or ‘negative’ for the intentional alterations in their eating habits; a seven-point scale from ‘almost never’ to ‘two or more times/day’ for the dietary supplements; and a two-point scale choosing ‘received’ or ‘not received’ for the receiving dietary guidance. For cooking methods of different fish and meats, the participants indicated the frequency of consuming raw fish on a seven-point scale ranging from ‘almost never’ to ‘two times/day.’ The same protocol was followed for boiled fish, grilled fish, tempura/fried fish, grilled meat, grilled meat pate, fried meat, stir fried meat, and stewed meat. The reproducibility and validity of the BDHQ have been described in detail in a previous study [15].
Clustering dietary patterns using unsupervised machine learning
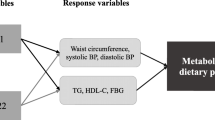
Analysis with unsupervised machine learning used all 79 variables, including 58 foods and non-alcoholic beverage items, 12 dietary behaviors, and 9 cooking methods common in the general Japanese population [44]. We applied dimension reduction using UMAP [38, 39] and a subsequent clustering using the K-means algorithm [45] using the raw data. UMAP dimension reduction (reduce_dimension) was performed using the following parameters: umap_min_dist = 0.1, max_components = 2, clustering neighbors (n_neighbors) = 10, and ‘Chebyshev’ as the metric. We determined the values of each parameter after the parameter tuning, in which each parameter was changed in a certain range to produce well-separated cluster distribution. 2D data were applied to K-means clustering; the default settings were used for K-means clustering. The number of clusters was determined using the elbow method and silhouette analysis [28, 46] (Supplementary Fig. 2) and the final cluster number was also confirmed as peak numbers in the contour map (Fig. 2).
Scatter plot and contour map. The graph illustrates the relative distances between participants in the Oroshisho cohort study using unsupervised machine learning and dimension reduction techniques based on BDHQ data. The data has been reduced to two dimensions (Dimension 1 (D1) and Dimension 2 (D2)) using UMAP. Each point on the graph represents an individual participant in the study. The contour lines are curves that show areas of constant Gaussian values in the 2D space, connecting points of similar 2D values. Number clusters (n = 4) were chosen optimally by contour map analysis. Exemplary 2D visualization of the relative distances between all participants in the Oroshisho cohort study using UMAP. Colors indicate cluster assignment using K-means clustering (K = 4). An interpretable name for the dietary pattern is then defined for each cluster based on the trend value (see ‘Methods’ for details)
To quantitatively evaluate the dietary patterns among the clusters, we introduced a “trend score” converted from the original BDHQ scale. First, the BDHQ scale was transformed into trend values as “weight” shown in Table 1. Because the proportion of each “weight” (Supplementary Fig. 1) could be suitable for understanding patterns among valuables or clusters and not for performing quantitative comparisons, the “proportion” of each “weight” against the total number was calculated (Supplementary Fig. 1). Finally, the “weight” was multiplied by the “proportion” and summed up to obtain the “trend score” for each variable.
where ω and π are “weight” and “proportion”, respectively.
Unsupervised machine learning algorithms were executed using Python programming language (version 3.7.10) deployed by Anaconda (version 2.1.1) in the Mac operating system (version 12.5). In addition, all necessary libraries (umap-learn version 0.3.10, scikit-learn version 0.21.3) were installed on a Jupyter Notebook (version 6.4.6).
Dietary approach to stop hypertension (DASH) score
A 40-point DASH score was estimated according to the previous study [47] to evaluate our dataset conformity to a DASH-style diet. The score comprises 8 dietary components, with recommended increases in the consumption of certain items (fruits, vegetables, nuts and legumes, low-fat dairy, and whole grains) and restrictions on others (sodium, sweetened beverages, and red and processed meats). Participants' sub-scores (1 to 5) for each component were determined based on sex-specific quintiles. The final DASH score, ranging from 8 to 40, was derived by summing the sub-scores for each component.
Absolute intake and relative intake
Absolute intake of each food item was obtained with BDHQBOX service (EBNJAPAN, DHQ Support Center, Tokyo, Japan). Absolute intake estimated from the BDHQ is based on Japan's Standard Tables of Food Composition (5th edition) [56]. Relative intake was calculated using the equation below:
where total energy intake was also obtained with BDHQBOX service.
Salt intake estimation
The estimated values of daily salt intake were also obtained with the BDHQBOX service (EBNJAPAN, DHQ Support Center, Tokyo, Japan) according to the previous studies [99, 100].”
Grouping food items
By consolidating similar food items from the original intake data, we generated a unified representation, yielding a new dataset that captures aggregated dietary patterns by PCA. The process entailed combining categories, such as fish, milk, beverages, eggs, noodles, desserts, meats, and vegetables, into composite data using average intake frequencies. A new dataset was presented in Supplementary Data 1.
Assessment of covariates
Other lifestyle-related and sociodemographic information, including age, smoking status, sleep duration, living status (alone), and educational level (≥ college or not), were obtained using a self-administered questionnaire. The average sleep duration per night was estimated based on when the participants went to bed and awoke without considering of week or weekend and categorized into ‘6–8 h per day’ (typical sleep duration) or not (atypically shorter or longer). Anthropometric parameters (height, body weight, and waist circumference) were measured according to a standardized protocol. The body mass index (BMI) was calculated as weight/height2 (kg/m2). Educational level was assessed by determining the final grade level and was divided into two categories: “less than college” and “college or above”.
Physical activity (PA) was measured using the International Physical Activity Questionnaire (IPAQ) [48]. Total weekly PA (metabolic equivalents [METs] × hours/week) was calculated and classified into three categories: 0 (The '0' category represents individuals in a state of rest or very low activity at baseline [42, 48]), 0.1–22.9, and ≥ 23 (METs × hours/week), the recommended level of physical activity for preventing lifestyle-related diseases in Japan is represented by the category ≥ 23 METs × hours/week [42, 48]. Depressive symptoms were assessed using the Japanese version of the Self-Rating Depression Scale (SDS) [49]. The SDS score ranging from 0 to 100, was used to evaluate the severity of depressive symptoms. An SDS score ≥ 40 was the cutoff point for relatively mild or severe depressive symptoms [50]. A score below 40 indicates the absence of significant depressive symptoms, while a score of 40 or higher suggests mild to severe depressive symptoms [50]. Blood samples were collected in siliconized vacuum glass tubes containing sodium fluoride to analyze the levels of fasting blood glucose, uric acid (UA), and lipids. Fasting blood glucose (FBG) was measured using an enzymatic method (Eerotec, Tokyo, Japan). Serum UA levels were measured enzymatically using a Pureauto SUA kit (Sekisui Medical Co. Ltd., Tokyo, Japan). The concentrations of triglycerides, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were measured by enzymatic methods using the appropriate kits. Moreover, a history of physical illness and current medication, including diabetes and dyslipidemia, were noted from ‘yes’ or ‘no.’ Diabetes was defined as an FBG level > 126 mg/dL, or a self-reported history of previously diagnosed diabetes or current medication for diabetes was regarded as having diabetes [51, 52]. Dyslipidemia was defined as a low-density lipoprotein cholesterol level ≥ 140 mg/dL, a high-density lipoprotein cholesterol level < 40 mg/dL, a triglyceride level ≥ 150 mg/dL, or the use of medications for dyslipidemia [53].
Statistical analysis
JMP software (version 16.2.0) was used for statistical analyses. The normality of variables was checked using the Kolmogorov–Smirnov test [54]. Continuous variables were checked for normality and transformation was not required. Descriptive statistics (i.e., mean and standard deviation [SD] for continuous variables and frequencies and percentages for categorical variables) were reported for all variables by cluster. ANOVA for continuous variables and Chi-square tests for categorical variables were used to assess cluster differences. Proportional band graphs were used to evaluate cluster features for each variable (Supplementary Material 1).
Multivariable logistic regression analysis was used to examine the association between each cluster and the incidence of hypertension. Hypertension was used as the dependent variable and the cluster of dietary patterns was used as the independent variable. The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using the likelihood ratio method to test, the p value for the incidence of hypertension compared to a reference cluster. Model 1 was a crude model. Model 2 was adjusted for age and BMI at the baseline. For model 3, all variables in model 2 and baseline smoking status, PA, and education were used. Model 4 was further adjusted for baseline dyslipidemia and diabetes mellitus. Model 5 was further adjusted for salt intake, a potential mediator, to examine the extent to which the association between different dietary patterns and hypertension could be attenuated.
Sensitivity analysis was used to examine the impact of residual confounding of age on the association between clusters characterized by dietary patterns and the incidence of hypertension. Furthermore, two analyses were performed; first, we checked the age distribution across the dietary pattern groups. We used box plot diagrams to determine whether there was sufficient age overlap among men of different cluster statuses to examine the effects of clusters and age separately. Next, we performed an age-matched group analysis. Each participant in each group was age-matched based on two matched ranges: ± 0 and ± 2 years. For each participant in cluster A, participants are selected from clusters B, C, and D who fall within the specified age ranges. These age ranges are ± 0 years (meaning participants with exactly the same age) and ± 2 years (participants who are within a 2-year age range of the participant from cluster A). We then performed the same multivariable logistic regression analysis as the main analysis. The same analysis methods as for the primary outcome were used to compare the use of food items alone with the outcome of combing food items, cooking methods, and dietary behavior to be driven dietary patterns with the incidence of hypertension. A P value < 0.05 was considered statistically significant in all analyses.
Results
Dietary patterns clustered using unsupervised machine learning
A dataset with 79 dimensions (79 variables) was reduced to two dimensions using the UMAP algorithm. The first and second dimensions were plotted on the x and y axes. A suitable number of clusters was determined to be four using the elbow method (see Supplementary Fig. 2). A 2D scatter plot of the clusters is presented in Fig. 2. The 2D scatter plot was overlaid with a density contour map showing four peaks consistent with the cluster number (Fig. 2).
Characteristics of dietary patterns by the trend scores
Instead of using the original BDHQ sore, we introduced a “trend score” (Table 2) to compare quantitatively the dietary patterns among the clusters (see “Methods” for details). The characteristics description for each cluster is below. The statistical significance was also examined among clusters for each variable. Cluster A was characterized by the highest consumption of western-type confectioneries (2.880), pasta (2.453), coffee (5.987), cola drink/soft drink (3.880), sugar (1.880), and persimmon-seasonal (3.347) in the food items; noodle soup (3.560) and meat fat (beef and pork) (3.093) in the dietary behaviors. Cluster A showed the lowest scores in many food items (26/58 items), especially proteins and vegetables, and the cooking methods (7/9 methods). The participants in this cluster tended to skip breakfast and appear to have unhealthy dietary behaviors such as taking noodle soup (high salt intake) or meat fat (high fat intake). The identified pattern was named the ‘Low-protein/fiber High-sugar’ pattern. Cluster B was characterized by the highest scores in many food items (29/58 items), especially dairy products, vegetables, and fruits, the cooking methods (5/9 methods), and dietary behaviors (6/12 behaviors). This cluster appeared to show healthy dietary behaviors and was named the ‘Dairy/vegetable-based’ pattern. Cluster C was characterized by the highest scores of chicken meat (3.190) and pork/beef (3.720), mayonnaise (3.700), bread (3.980), Chinese noodles (3.140), and beer (3.530) in the food items; grilled meat/steak (2.530) in the cooking methods; frequency of soy sauce or equivalent used for meals (3.790), amount of soy sauce or equivalent used for meals (3.020), and supplements (1.850) in the dietary behaviors. The Cluster C was referred to as the ‘Meat-based’ pattern. Cluster D was characterized by the highest consumption of most seafood (5/6 items) and alcohol (5/6 items) in the food items and fish-related items in the cooking methods (4 methods). This cluster was named the ‘Seafood and Alcohol’ pattern.
Characteristics according to cluster categories of dietary patterns
Table 3 presents the characteristics of the clusters of dietary patterns. Differences were observed in lifestyle parameters; we observed heterogeneity in these variables across all the patterns. The mean age and BMI were higher in the ‘Dairy/vegetable-based’ pattern (age: 44.88 ± 10.5 years, BMI: 23.73 ± 3.14) and the ‘Seafood and Alcohol’ pattern (age: 47.58 ± 9.69 years, BMI: 23.08 ± 2.84) compared to ‘Low-Fiber High-Sugar’ pattern (age: 40.25 ± 8.27 years, BMI: 22.90 ± 2.48) and ‘Meat-based’ pattern (age: 43.74 ± 8.86 years, BMI: 22.75 ± 2.69). The ‘Meat-based’ pattern exhibited a higher proportion of eating dinner before bedtime (67.0%), smoking (70%), or skipping breakfast (64.0%). However, the distribution of education level and sleep quality was different across all patterns (P < 0.05). Additionally, differences were observed in diagnostic and blood examination parameters; participants in the ‘Low-Fiber High-Sugar’ pattern exhibited the lowest level of SBP (118.05 ± 11.57 mmHg), DBP (72.16 ± 8.90 mmHg), and fasting glucose (91.29 ± 8.74), and demonstrated the highest level of LDL-C (128.24 ± 32.60 mg/dL). Compared with other patterns, the ‘Seafood and Alcohol’ pattern had a higher proportion of diabetes (9.9%) and the highest level of HDL-C (56.65 ± 13.19 mg/dL). Table 3 also shows that the participants in the 'Dairy/vegetable-based' pattern (12.05 ± 4.15) and 'Seafood and Alcohol' pattern (11.56 ± 3.06) were taking higher amount of salt than those in the 'Low-Fiber High-Sugar' pattern (10.45 ± 2.55) and 'Meat-based' pattern (10.93 ± 2.85). No association was observed between the clusters and the other factors.
Association of clusters with hypertension
Table 4 presents the ORs and 95% CI for the incidence of hypertension according to the clusters of dietary patterns. We attempted to identify a dietary pattern with a high risk of hypertension and chose cluster D as a reference to reduce multiple comparisons since the cluster showed the largest sample size and the highest hypertension prevalence, indicating it could be an aversive dietary pattern. As indicated in the crude model with the ‘Seafood and Alcohol’ dietary pattern as the reference, the mean OR for hypertension according to clusters was 0.29 (95% CI 0.12–0.75) for the ‘Low-Fiber High-Sugar’ pattern, 0.517 (95% CI 0.272–0.984) for ‘Dairy/vegetable-based’ pattern, and 0.339 (95% CI 0.154–0.749) for ‘Meat-based’ pattern (P = 0.006). Even after adjustment for age, and BMI (Model 2), a similar association was still maintained (P = 0.049). Although the association was attenuated (P = 0.055) after adjusting for age, BMI, smoking, education, and PA (Model 3), the difference was confirmed after a fully adjusted model 4 (P = 0.014). The difference in the mean OR for hypertension between the ‘Low-Fiber High-Sugar,’ ‘Dairy/vegetable-based,’ and ‘Meat-based’ dietary patterns was confirmed in the fully adjusted model 4, with respective ORs of 0.34 (95% CI 0.13–0.91), 0.39 (95% CI 0.19–0.80), and 0.37 (95% CI 0.16–0.86). In Model 5, the same association remained (P = 0.018) even after adjusting for salt intake, with respective ORs of 0.35 (95% CI 0.13, 0.92), 0.43 (95% CI 0.21, 0.86), and 0.38 (95% CI 0.16, 0.86).
Age-matched analysis (sensitivity analysis)
As ca be seen in Fig. 3, the distribution of age was imbalanced in each cluster. When we performed an age-matching group analysis, similar associations were obtained in the age-matched analyses (Tables 5, 6). In the analyses comparing age-matched groups, an association was observed with a range of ± 0 and ± 2 years old, respectively, with p-values of 0.030 and 0.009. Furthermore, the same association remained significant (P = 0.077, P = 0.012) even after adjusting for salt intake. However, the age-matched analysis with the range of ± 2 years old did not detect the difference between the “Low-Fiber High-Sugar” pattern and the “Seafood and Alcohol” pattern (Table 6).
Absolute intake and relative intake
We also evaluate the clustering using absolute or relative intakes, instead of frequency of food item intake. However, neither cluster showed four obvious clusters (Supplementary Figs. 7 and 8). Three ambiguous or seven sparse clusters were observed in absolute or relative intakes, respectively. The number of clusters was chosen by the elbow method (Supplementary Figs. 7 and 8). The results suggest a lack of clear clustering patterns in absolute and relative intakes, indicating a distinct difference in structure or grouping. These findings highlight the complexity and variability of the data, underscoring the importance of the chosen parameter for the clustering analysis.
Comparison to analysis using DASH scores
Regarding hypertension, the diet based on Dietary Approaches to Stop Hypertension (DASH) has been shown to reduce blood pressure in the previous studies [55, 56]. We estimated the DASH score using our dataset according to the procedure reported previously [55] (see ‘Methods’) and compared it with our result. Compared with previous studies, our data showed relatively lower DASH scores (DASH scores: 5–9 in Q1, 9–12 in Q2, 12–14 in Q3, and 14–23 in Q4) and no association with the incidence of hypertension between the lowest DASH score group and the others (Supplementary Table 1). Supplementary Table 2 shows the proportions of DASH scores ranging from Q1 to Q4 for each cluster. Cluster D, which exhibited the highest risk for hypertension and the lowest DASH score, demonstrated statistical differences in quantile composition from clusters A and B, but not cluster C. Cluster D also showed differences in average DASH scores from clusters A and B, but not cluster C (Supplementary Table 2).
Examining parameter categories in clustering
We also examined the contribution of the category of parameters to clustering (Supplementary Table 3). When removing “cooking methods” category from the original parameter set (food items + dietary behaviors + cooking methods), four clusters were also observed (Supplementary Fig. 5) and the most fraction of clusters coincided with the clustering (overlap percentages for Clusters A = 90.7%, B = 91.5%, C = 79.0%, D = 88.7%). However, removing “dietary behaviors” or “dietary behaviors + cooking methods (only food items)” resulted in no obvious four clusters observed (Supplementary Figs. 3 and 4). Two dense clusters were observed by clustering using only “dietary behaviors” (Supplementary Fig. 5). This result suggests a critical contribution of “dietary behaviors” to clustering and dietary patterns represented as food items could become clearer by combining different categories of parameters.
Evaluation and optimization of food cluster grouping using principal component analysis
Procedure grouping similar food items is frequently used to reduce valuables by prior knowledge or after principal component analysis. We assessed the effect of grouping parameters on our clustering approach. We reclassified similar food items into each typical category, such as yogurt and milk, into the dairy product category. The grouping results are shown in Supplementary Data 1. The grouped dataset failed to produce clear clusters (Supplementary Fig. 6).
Discussion
This study applied unsupervised machine learning to identify dietary patterns based on food intake frequency, dietary behaviors, and cooking methods. We identified four dietary patterns: ‘Low-Fiber High-Sugar,’ ‘Dairy/vegetable-based,’ ‘Meat-based,’ and ‘Seafood and Alcohol’ patterns. A series of statistical analyses revealed that ‘Dairy/vegetable-based’ and ‘Meat-based’ patterns are associated with a lower risk of hypertension than ‘Seafood and Alcohol’ patterns. Furthermore, the results remained similar even when age-matched group analyses were performed.
Since there is no ‘gold standard’ procedure for classifying dietary patterns, pattern classification has often been based on relevant expertise or experience. Identifying dietary patterns can be applied to validated dietary assessment methods, such as food frequency questionnaires [15] or 24-h dietary recalls [57], using established dietary pattern analysis techniques, such as PCA [13] and factor analysis [15]. PCA and factor analysis, utilizing data on food intake [28, 58], can help identify the essential food groups or factors contributing to an individual’s diet and minimizes data complexity by reducing the number of variables. PCA, however, has a limitation in that it is a linear method and may not effectively capture nonlinear relationships in the data [59]. Additionally, PCA is sensitive to outliers and extreme values, which can result in distorted results [60]. Factor analysis also has limitations, including the subjective nature of defining and interpreting the factors [61], the impact of the number of factors to extract and the method of extraction from the results [61], and the assumption of a specific structure in the data, which may not always hold true [62]. Therefore, the development of new, practical dietary approaches is desirable. Combining UMAP and K-means may be a powerful tool for analyzing dietary patterns in epidemiological studies. UMAP has gained popularity for dimensionality reduction and visualization due to its capacity to reveal intricate relationships in high-dimensional data, since this method stands out for its exceptional ability to capture complex nonlinear patterns within data while preserving global structure [38]. UMAP often outperforms traditional techniques like t-SNE and PCA in terms of preserving the underlying data structure [63]. UMAP is commonly used to visualize high-dimensional datasets containing over 20,000 genes in transcriptomics or population genetics [64,65,66]. Recently, UMAP has begun to be applied for identifying sub-groups from demographic features or visualizing clusters of food items in epidemiological data [37, 68]. On the other hand, K-means is frequently used for its simplicity and efficiency in clustering data points, especially in scenarios where the number of clusters is known in advance, since this algorithm was shown to be highly scalable and competitive with other clustering algorithms when applied to large datasets [67]. K-means is commonly used to group similar food items and identify common dietary patterns after PCA [45, 68]. In summary, UMAP offers superior nonlinear dimensionality reduction capabilities, while K-means provides a straightforward and efficient solution for clustering tasks, as shown by our approach successfully identified dietary patterns associated with the incidence of hypertension.
Dietary patterns are not solely determined by the types of food intake but are also influenced by dietary behaviors and cooking methods [69,70,71]. Therefore, when evaluating dietary patterns, it is suggested that considering such dietary behavior as portion sizes, frequency of meals, speed of eating, and eating out frequency can impact the overall nutritional quality of a person's diet [72, 73]. Cooking methods also play a crucial role in determining the nutrient content, caloric intake, and fat intake of food [74, 75]. For instance, deep-frying can increase the calorie and fat content, while steaming or grilling can help retain the nutrient content of vegetables [76,77,78]. Considering food intake, dietary behavior, and cooking methods is crucial when evaluating dietary patterns, as this can provide a comprehensive understanding of the population's eating habits. It can also identify areas where dietary interventions can be targeted to improve overall health and well-being.
This study identified four distinct dietary patterns: Cluster A, Low-protein/fiber High-sugar; Cluster B, Dairy/vegetable-based; Cluster C, Meat-based; and Cluster D, Seafood and Alcohol, named according to the trend score ranking. Notably, 17 of 58 food items, 3 of 9 cooking methods, and 1 of 12 dietary behaviors showed differences among clusters (Table 2). However, named patterns by the ranking of the trend scores are not always consistent with differences. This could result from a complex combination of 79 variables and might reflect holistic interaction between groups or patterns of variables. However, the patterns identified demonstrated some similarities to previous studies among Japanese adults. For example, the ‘Dairy/vegetable-based’ pattern was similar to the ‘Traditional Japanese’ pattern (vegetables, fruits, potatoes, mushrooms, seafood, grains, milk, legumes, and low intake of beverages) identified by the nutritional dietary survey [16]. Additionally, the ‘Sweet-fat’ pattern (Western and Japanese confectioneries, mayonnaise and other dressings, bread, and ice cream) was previously identified similarly in the Nagano Nutrition and Health Study [79]. The ‘Fast Food/Sweet’ pattern (ice cream, desserts, chocolate, soft drink, and bread) from Qatar Biobank survey was similar to the ‘Low-Fiber High-Sugar’ patterns identified in this study [80].
Furthermore, the ‘Seafood and Alcohol’ pattern was similar to the ‘Izakaya’ or ‘Seafood-Alcohol’ patterns (sea fish and alcohol) identified in Japanese studies [40, 79]. Lastly, the ‘Meat-based’ pattern (vegetables, root vegetables, mushrooms, seaweed, soybean products, potatoes, fruit, and a balanced intake of fish, meat, and dishes) was identified as a Japanese dietary pattern different from the ‘Dairy/vegetable-based’ pattern. This pattern was similar to the dietary pattern reported as the ‘Healthy Japanese’ pattern identified in a Japanese study [79]. These studies focused solely on food-related variables and did not consider other factors, such as dietary behavior and cooking methods. For example, the frequency of eating out [73], meal skipping [81], and the use of seasoning in cooking can all affect dietary patterns [82]. Simplifying dietary patterns can reduce related dietary behavior and cooking [83], but can also result in losing important information on dietary patterns. Therefore, it is vital to use a systematic approach in creating dietary patterns and consider food intake, dietary behavior, and cooking in the analysis [84,85,86]; this provides a more comprehensive understanding of the diet and helps identify specific dietary patterns.
In this study associations of ‘Dairy/vegetable-based’ and ‘Meat-based’ patterns with a lower risk of hypertension were observed. Our findings are consistent with previous studies revealing an inverse association between the risk of hypertension and the intake of beans, potatoes, mushrooms, vegetables, and healthy dietary behavior and healthy cooking [15, 16, 18, 19, 87], all of which were essential components of ‘Meat-based healthy’ dietary pattern identified in this study. A similar observation with a ‘Dairy/vegetable-based’ pattern was obtained in a large cohort study [88] demonstrating an association between ‘Vegetarian’ diet and a reduced risk of hypertension. The possible reasons for the reduced risk in ‘Dairy/vegetable-based’ dietary pattern may be in the lower intake of saturated fat, higher fiber consumption, and healthy dietary behavior. ‘Low-Fiber High-Sugar’ and ‘Seafood and Alcohol’ patterns were not specifically associated with the risk of hypertension. Previous reviews revealed similar results, indicating that compositions of diet patterns similar to our findings are associated with hypertension and other markers of metabolic dysfunction (blood pressure), with risk factors similar to those of hypertension [89]. Although marine products and vegetables have positive nutrient attributes, the patterns of other components, such as alcohol [90, 91], sweets [92, 93], and unhealthy dietary behavior (“eating speed” and “frequency of seasoning use in cooking”, etc.) [94, 95] related to higher risk of hypertension may have cancelled the benefit.
The BDHQ (Brief Self-Administered Diet History Questionnaire) employs a range of scales to represent the diverse and complex Japanese diet accurately. Varying scales are selected to capture subtle intake variations (e.g., a 7-point scale) or simpler scales are used when appropriate (e.g., a 5-point scale) [96]. This approach reflects the intricacies of assessing different foods, some straightforward and others requiring more detailed scales due to complexity or infrequent consumption. Researchers should be mindful of these scales when analyzing BDHQ data to maintain consistency and comparability in their findings, ensuring more comprehensive and reliable dietary research and nutritional assessment in Japan.
In this study, we did not include data from the year 2011 due to the potential impact of the Fukushima nuclear accident on the dietary habits of the study participants. This dietary change should be significant because nuclear contamination by accident [97] led to concern about food safety [96], which might affect hypertension development. Changes in the dietary patterns of the Fukushima nuclear accident would be an interesting topic, but it is beyond the current study. Similarly, another interesting issue would be the relationship between the dietary pattern change and the prevalence of other physical/mental disorders after the Fukushima nuclear accident. However, we have the health check-up data in 2011 but not the subsequent years, making it hard for longitudinal analysis. Therefore, we decided to focus on the relationship between dietary patterns and health by excluding 2011 data to avoid the potential impact of the Fukushima nuclear accident.
The results of the analysis in Table 3 (see Supplementary Table 3) indicate that food alone was not a strong predictor of incident hypertension. This was found using UMAP, K-means clustering algorithms, and multivariable logistic regression. This suggests that other factors, such as cooking methods and dietary behavior, may play a more important role in influencing the development of hypertension. It appears that the combination of foods, cooking methods, and dietary behaviors, as captured by the derived dietary patterns, gave a better prediction of the incidence of hypertension than the use of foods alone. This suggests that considering a wider range of dietary and lifestyle factors may provide a more accurate insight into the development of hypertension.
Additionally, it is essential to explore the possibility of 'white coat hypertension,' wherein blood pressure remains consistently elevated during out-of-office measurements but appears normal during in-office readings. This phenomenon may have implications for the interpretation of our results and should be considered in future research. To address this concern, we recommend that future studies explore methods for identifying patients at risk for white coat hypertension and utilize out-of-office readings for a more comprehensive assessment of participants' blood pressure. Furthermore, we encourage researchers to verify the validity of the blood pressure monitoring devices used in their studies.
Confounding factors are variables that can distort the relationship between exposure and outcome. In our study, we adjusted for confounding risk factors such as age, BMI, smoking, education, physical activity, dyslipidemia, diabetes, and salt intake and found an association between dietary patterns and hypertension. Salt intake was a potential mediator in our study, but the association between dietary patterns and hypertension persisted even after adjusting for salt intake, suggesting that other dietary factors may have contributed to the incidence of hypertension. This result is noteworthy because it suggests that there may be other dietary components, besides salt, that contribute to the incidence of hypertension. For instance, reducing salt intake alone was not associated with a reduction in blood pressure in the individuals with resistant hypertension [98, 99]. This fact implies that simply lowering salt intake may be insufficient to prevent hypertension and a more comprehensive approach that considers other dietary factors may be necessary [100]. Further research is needed to validate these findings and inform public health interventions to prevent hypertension.
Regarding hypertension, the diet based on Dietary Approaches to Stop Hypertension (DASH) has been shown to reduce blood pressure in previous studies [55, 56]. We estimated the DASH score using our dataset according to the procedure reported previously [55] (Supplementary Data 1) and compared with our results. In Table 1, the proportions of DASH scores ranging from Q1 to Q4 were presented for each cluster. The results revealed a noteworthy finding. We then analyzed the DASH scores for each cluster. Cluster D, a group with the highest risk of hypertension, showed the lowest DASH score. To evaluate the association between DASH scores and hypertension risk in Cluster D, we employed Cox proportional-hazards model. Our data showed relatively lower DASH scores compared with previous studies and no association with the incidence of hypertension (Table 2). This finding contrasts sharply with conclusions drawn previously using unsupervised machine learning methods. This suggests that within our dataset, unsupervised learning effectively identifies dietary patterns associated with the incidence of hypertension, possibly due to the presence of features related to dietary patterns that are well captured by unsupervised machine learning. However, when we shifted to using the DASH, we failed to observe similar associations in the data. This may indicate that the relationship between the DASH and the incidence of hypertension is not significant in our study sample, or alternatively, the DASH may not be a strong predictor in our dataset.
DASH scores from our dataset were relatively low compared with previous studies and showed no association with the incidence of hypertension (Supplementary Table 1), which contrasts sharply with the result using our unsupervised machine learning approach. This suggests that our machine learning approach could effectively identify dietary patterns associated with the incidence of hypertension even in the population with relatively low total DASH scores. Our result that there was no difference between quantile groups by DASH scores also suggests that DASH scores might overlook hypertension incidence when the contrast in the evaluation by DASH score is insufficient.
In the re-cluster with reduced categories, we observed that “only food items + dietary behaviors” could be effectively grouped into four clusters, while the other two sets, “Food items + cooking methods” and “Food items,” could only be categorized into two clusters. This suggests a critical contribution of dietary behaviors to clustering dietary patterns according to food items. Our study emphasizes the necessity of a multi-dimensional evaluation, including dietary behaviors and cooking methods in hypertension prevention.
Variable selection or aggregation of variables is often performed for providing more precise estimates, even though its effect has been controversial [104,105,106]. We also assessed the effect of grouping parameters on our clustering approach. We reclassified similar food items into each typical category, such as yogurt and milk, into the dairy product category. The grouping results are shown in Supplementary Data 1, providing two variables. Grouped dataset failed to produce clear clusters (Supplementary Fig. 6), possibly due to lower resolution by reduced parameter number.
However, our approach using unsupervised machine learning failed clustering by grouping similar food items (Supplementary Fig. 4). Dietary patterns are often complex and multifaceted, involving not only food types but also cooking methods and meal times [101]. Ignoring these factors can lead to oversimplification of dietary patterns, making it challenging to capture the true relationships within the data. By focusing solely on food items and neglecting dietary behaviors and cooking methods, essential dimensions of dietary patterns were omitted [102]. Different cooking methods can significantly alter the nutritional content and overall health impact of a meal, which is vital for understanding the complete picture of dietary habits [103]. The success of unsupervised machine learning techniques heavily depends on the quality and representativeness of the data [104]. If the dataset is incomplete, biased, or lacks diversity, the algorithm may struggle to identify meaningful patterns. It is crucial to ensure that the dataset used for clustering is comprehensive and accurately reflects the population's dietary habits.
Clustering using absolute and relative intake data failed to observe clear clusters in UMAP analyses as shown in Supplementary Figs. 7 and 8. The difference from our procedure using the BDHQ food intake frequency might be caused by absolute and relative intake “estimated” from the BDHQ frequency dataset with many assumptions, even though the previous study reported that the BDHQ showed reasonable validity regarding food intake estimates [43]. While our procedure used the frequency directly as a primary dataset with a simple conversion, the absolute intake and the total energy intake to calculate relative intake were estimated by “an ad hoc computer algorithm including weighting factors” (as described in the literature) which is not available in public [43], suggesting the estimated values by “black box” might make direct comparison difficult.
This study has several limitations. First, the self-reported method of dietary intake is susceptible to recall bias and social desirability bias, leading to the misclassification of food consumption and dietary behaviors. Although the validation of the BDHQ used in this study has been reported [43, 44, 105], the approach of asking about the frequency of food items consumed still has limitations in estimating the precise amount of nutrient intake [106, 107]. Additionally, the survey was conducted annually, and periodic changes were not considered. Furthermore, subjective bias can persist based on statistical thresholds or modeling selection, even in a data-driven approach. The other concern is that we hardly exclude the population and situation biases. Our participants, employees of Sendai Oroshisho Center, may not fully represent the diversity of Japanese males in terms of lifestyle, socio-economic backgrounds, and health behaviors. Our data also could not exclude the effect of “white coat hypertension” [108, 109], even though the blood pressure measurement was repeated when it showed higher values than medical standards. The measurement of the blood pressure by wearable devices or portable devices at home might be preferable to detect hypertension diagnosis more precisely. Lastly, it is crucial to note that in this study, we did not conduct a post hoc power analysis, which may impact the accuracy of interpreting and inferring observational effects. Future research should consider sample size and effect size during the design phase to ensure that the study has sufficient power. Another concern in the study is that the biased sample size (smaller sample size of Cluster A) might result in no difference compared to the reference (Cluster D) in the naïve analysis (Table 4, Models 2 and 3). Considering the possibility of over-adjustment, however, we performed a stepwise modeling through age-matched analyses and observed no difference for Cluster A in the age-matched ± 2 model (Table 6). This suggests that the confounding effect of age might be observed in Cluster A.
Conclusion
Using unsupervised machine learning, UMAP and K-means clustering, on a cohort dataset of Japanese male population, we identified four dietary patterns: ‘Low-protein/fiber High-sugar,’ ‘Dairy/vegetable-based,’ ‘Meat-based,’ and ‘Seafood and Alcohol.’ ‘Seafood and Alcohol’ was identified as a risk dietary pattern with a highest prevalence of hypertension. The ‘Dairy/vegetable-based’ and ‘Meat-based’ showed a lower risk of hypertension incident compared to the ‘Seafood and Alcohol.’ Our study would be valuable for uncovering hidden patterns that traditional statistics and PCA approaches might overlook in nutritional research since our approach could consider food items, behavior, and cooking methods, offering insights into complex dietary patterns. Our holistic approach enhances understanding of how dietary choices impact the incidence of hypertension risk. Our study would provide a novel approach to identify specific patterns with potential implications for the incidence of hypertension.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Zhao D, Qi Y, Zheng Z, Wang Y, Zhang XY, Li HJ, Liu HH, Zhang XT, Du J, Liu J (2011) Dietary factors associated with hypertension. Nat Rev Cardiol 8(8):456–465. https://doi.org/10.1038/nrcardio.2011.75
NCD Risk Factor Collaboration (2017) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 389(10064):37–55. https://doi.org/10.1016/s0140-6736(16)31919-5
Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 21 June 2021.
Ogihara T, Rakugi H (2005) Hypertension in the elderly: a Japanese perspective. Drugs Aging 22(4):297–314. https://doi.org/10.2165/00002512-200522040-00003
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, Ito M, Ito S, Iwashima Y, Kai H, Kamide K, Kanno Y, Kashihara N, Kawano Y, Kikuchi T, Kitamura K, Kitazono T, Kohara K, Kudo M, Kumagai H, Matsumura K, Matsuura H, Miura K, Mukoyama M, Nakamura S, Ohkubo T, Ohya Y, Okura T, Rakugi H, Saitoh S, Shibata H, Shimosawa T, Suzuki H, Takahashi S, Tamura K, Tomiyama H, Tsuchihashi T, Ueda S, Uehara Y, Urata H, Hirawa N (2019) The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res 42(9):1235–1481. https://doi.org/10.1038/s41440-019-0284-9
Hisamatsu T, Segawa H, Kadota A, Ohkubo T, Arima H, Miura K (2020) Epidemiology of hypertension in Japan: beyond the new 2019 Japanese guidelines. Hypertens Res 43(12):1344–1351. https://doi.org/10.1038/s41440-020-0508-z
Weder AB (2007) Genetics of hypertension. In: Izzo JL, Sica DA, Black HR (eds) Hypertension primer: the essentials of high blood pressure: basic science, population science, and clinical management, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 229–231
Guilbert JJ (2003) The world health report 2002—reducing risks, promoting healthy life. Educ Health (Abingdon) 16(2):230. https://doi.org/10.1080/1357628031000116808
Nissensohn M, Román-Viñas B, Sánchez-Villegas A, Piscopo S, Serra-Majem L (2016) The effect of the Mediterranean diet on hypertension: a systematic review and meta-analysis. J Nutr Educ Behav 48(1):42-53.e41. https://doi.org/10.1016/j.jneb.2015.08.023
Lin PD, Cardenas A, Hauser R, Gold DR, Kleinman KP, Hivert MF, Fleisch AF, Calafat AM, Webster TF, Horton ES, Oken E (2019) Per- and polyfluoroalkyl substances and blood lipid levels in pre-diabetic adults-longitudinal analysis of the diabetes prevention program outcomes study. Environ Int 129:343–353. https://doi.org/10.1016/j.envint.2019.05.027
Takashima Y, Iwase Y, Yoshida M, Kokaze A, Takagi Y, Taubono Y, Tsugane S, Takahashi T, Iitoi Y, Akabane M, Watanabe S, Akamatsu T (1998) Relationship of food intake and dietary patterns with blood pressure levels among middle-aged Japanese men. J Epidemiol 8(2):106–115. https://doi.org/10.2188/jea.8.106
Yap RWK, Shidoji Y, Yap WS, Masaki M (2017) Association and interaction effect of AGTR1 and AGTR2 gene polymorphisms with dietary pattern on metabolic risk factors of cardiovascular disease in Malaysian adults. Nutrients 9(8):853. https://doi.org/10.3390/nu9080853
Ramezankhani A, Hosseini-Esfahani F, Mirmiran P, Azizi F, Hadaegh F (2021) The association of priori and posteriori dietary patterns with the risk of incident hypertension: Tehran Lipid and Glucose Study. J Transl Med 19(1):44. https://doi.org/10.1186/s12967-021-02704-w
Lee SA, Cai H, Yang G, Xu WH, Zheng W, Li H, Gao YT, Xiang YB, Shu XO (2010) Dietary patterns and blood pressure among middle-aged and elderly Chinese men in Shanghai. Br J Nutr 104(2):265–275. https://doi.org/10.1017/s0007114510000383
Sadakane A, Tsutsumi A, Gotoh T, Ishikawa S, Ojima T, Kario K, Nakamura Y, Kayaba K (2008) Dietary patterns and levels of blood pressure and serum lipids in a Japanese population. J Epidemiol 18(2):58–67. https://doi.org/10.2188/jea.18.58
Htun NC, Suga H, Imai S, Shimizu W, Ishikawa-Takata K, Takimoto H (2018) Dietary pattern and its association with blood pressure and blood lipid profiles among Japanese adults in the 2012 Japan National Health and Nutrition Survey. Asia Pac J Clin Nutr 27(5):1048–1061. https://doi.org/10.6133/apjcn.072018.04
Niu K, Momma H, Kobayashi Y, Guan L, Chujo M, Otomo A, Ouchi E, Nagatomi R (2016) The traditional Japanese dietary pattern and longitudinal changes in cardiovascular disease risk factors in apparently healthy Japanese adults. Eur J Nutr 55(1):267–279. https://doi.org/10.1007/s00394-015-0844-y
Zhang Y, Tang T, Tang K (2019) Cooking frequency and hypertension with gender as a modifier. Nutr J 18(1):79. https://doi.org/10.1186/s12937-019-0509-4
Umesawa M, Kitamura A, Kiyama M, Okada T, Shimizu Y, Imano H, Ohira T, Nakamura M, Maruyama K, Iso H (2013) Association between dietary behavior and risk of hypertension among Japanese male workers. Hypertens Res 36(4):374–380. https://doi.org/10.1038/hr.2012.205
Kitaoka K, Nagaoka J, Matsuoka T, Shigemura C, Harada K, Aoi W, Wada S, Asano H, Sakane N, Higashi A (2013) Dietary intervention with cooking instructions and self-monitoring of the diet in free-living hypertensive men. Clin Exp Hypertens 35(2):120–127. https://doi.org/10.3109/10641963.2012.702830
Garcidueñas-Fimbres TE, Paz-Graniel I, Nishi SK, Salas-Salvadó J, Babio N (2021) Eating speed, eating frequency, and their relationships with diet quality, adiposity, and metabolic syndrome, or its components. Nutrients 13(5):1687. https://doi.org/10.3390/nu13051687
Govindaraju T, Sahle BW, McCaffrey TA, McNeil JJ, Owen AJ (2018) Dietary patterns and quality of life in older adults: a systematic review. Nutrients 10(8):971. https://doi.org/10.3390/nu10080971
Mazzucca CB, Raineri D, Cappellano G, Chiocchetti A (2021) How to tackle the relationship between autoimmune diseases and diet: well begun is half-done. Nutrients 13(11):3956. https://doi.org/10.3390/nu13113956
Guinter MA, McCullough ML, Gapstur SM, Campbell PT (2018) Associations of pre- and postdiagnosis diet quality with risk of mortality among men and women with colorectal cancer. J Clin Oncol 36(34):Jco800714. https://doi.org/10.1200/jco.18.00714
Previdelli ÁN, de Andrade SC, Fisberg RM, Marchioni DM (2016) Using two different approaches to assess dietary patterns: hypothesis-driven and data-driven analysis. Nutrients 8(10):593. https://doi.org/10.3390/nu8100593
Smith E, Ericson U, Hellstrand S, Orho-Melander M, Nilsson PM, Fernandez C, Melander O, Ottosson F (2022) A healthy dietary metabolic signature is associated with a lower risk for type 2 diabetes and coronary artery disease. BMC Med 20(1):122. https://doi.org/10.1186/s12916-022-02326-z
McNaughton SA, Mishra GD, Brunner EJ (2008) Dietary patterns, insulin resistance, and incidence of type 2 diabetes in the Whitehall II Study. Diabetes Care 31(7):1343–1348. https://doi.org/10.2337/dc07-1946
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9. https://doi.org/10.1097/00041433-200202000-00002
Li Y, Jaddoe VW, Qi L, He Y, Wang D, Lai J, Zhang J, Fu P, Yang X, Hu FB (2011) Exposure to the chinese famine in early life and the risk of metabolic syndrome in adulthood. Diabetes Care 34(4):1014–1018. https://doi.org/10.2337/dc10-2039
Gorst-Rasmussen A, Dahm CC, Dethlefsen C, Scheike T, Overvad K (2011) Exploring dietary patterns by using the treelet transform. Am J Epidemiol 173(10):1097–1104. https://doi.org/10.1093/aje/kwr060
Varraso R, Garcia-Aymerich J, Monier F, Le Moual N, De Batlle J, Miranda G, Pison C, Romieu I, Kauffmann F, Maccario J (2012) Assessment of dietary patterns in nutritional epidemiology: principal component analysis compared with confirmatory factor analysis. Am J Clin Nutr 96(5):1079–1092. https://doi.org/10.3945/ajcn.112.038109
Geiger BC, Kubin G (2012) Relative information loss in the PCA. In: 2012 IEEE information theory workshop. Lausanne, Switzerland, pp 562–566. https://doi.org/10.1109/ITW.2012.6404738
Pate ME, Turner MK, Thornhill NF, Titchener-Hooker NJ (2004) Principal component analysis of nonlinear chromatography. Biotechnol Prog 20(1):215–222. https://doi.org/10.1021/bp034133a
Murakami K, Shinozaki N, Fujiwara A, Yuan X, Hashimoto A, Fujihashi H, Wang HC, Livingstone MBE, Sasaki S (2019) A systematic review of principal component analysis-derived dietary patterns in Japanese adults: are major dietary patterns reproducible within a country? Adv Nutr 10(2):237–249. https://doi.org/10.1093/advances/nmy079
Tatoli R, Lampignano L, Bortone I, Donghia R, Castellana F, Zupo R, Tirelli S, De Nucci S, Sila A, Natuzzi A, Lozupone M, Griseta C, Sciarra S, Aresta S, De Pergola G, Sorino P, Lofù D, Panza F, Di Noia T, Sardone R (2022) Dietary patterns associated with diabetes in an older population from Southern Italy Using an unsupervised learning approach. Sensors (Basel, Switzerland) 22(6):2193. https://doi.org/10.3390/s22062193
Limketkai BN, Hamideh M, Shah R, Sauk JS, Jaffe N (2022) Dietary patterns and their association with symptoms activity in inflammatory bowel diseases. Inflamm Bowel Dis 28(11):1627–1636. https://doi.org/10.1093/ibd/izab335
Hozumi Y, Wang R, Yin C, Wei GW (2021) UMAP-assisted K-means clustering of large-scale SARS-CoV-2 mutation datasets. Comput Biol Med 131:104264. https://doi.org/10.1016/j.compbiomed.2021.104264
Grollemund V, Chat GL, Secchi-Buhour MS, Delbot F, Pradat-Peyre JF, Bede P, Pradat PF (2020) Development and validation of a 1-year survival prognosis estimation model for amyotrophic lateral sclerosis using manifold learning algorithm UMAP. Sci Rep 10(1):13378. https://doi.org/10.1038/s41598-020-70125-8
Bej S, Sarkar J, Biswas S, Mitra P, Chakrabarti P, Wolkenhauer O (2022) Identification and epidemiological characterization of type-2 diabetes sub-population using an unsupervised machine learning approach. Nutr Diabetes 12(1):27. https://doi.org/10.1038/s41387-022-00206-2
Guo H, Niu K, Monma H, Kobayashi Y, Guan L, Sato M, Minamishima D, Nagatomi R (2012) Association of Japanese dietary pattern with serum adiponectin concentration in Japanese adult men. Nutr Metab Cardiovasc Dis 22(3):277–284. https://doi.org/10.1016/j.numecd.2010.06.006
Dubey RK, Oparil S, Imthurn B, Jackson EK (2002) Sex hormones and hypertension. Cardiovasc Res 53(3):688–708. https://doi.org/10.1016/s0008-6363(01)00527-2
Huang C, Niu K, Momma H, Kobayashi Y, Guan L, Chujo M, Otomo A, Cui Y, Nagatomi R (2014) Breakfast consumption frequency is associated with grip strength in a population of healthy Japanese adults. Nutr Metab Cardiovasc Dis 24(6):648–655. https://doi.org/10.1016/j.numecd.2013.12.013
Sasaki S, Ushio F, Amano K, Morihara M, Todoriki O, Uehara Y, Toyooka E (2000) Serum biomarker-based validation of a self-administered diet history questionnaire for Japanese subjects. J Nutr Sci Vitaminol (Tokyo) 46(6):285–296. https://doi.org/10.3177/jnsv.46.285
Kobayashi S, Murakami K, Sasaki S, Okubo H, Hirota N, Notsu A, Fukui M, Date C (2011) Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr 14(7):1200–1211. https://doi.org/10.1017/s1368980011000504
Stricker MD, Onland-Moret NC, Boer JM, van der Schouw YT, Verschuren WM, May AM, Peeters PH, Beulens JW (2013) Dietary patterns derived from principal component- and k-means cluster analysis: long-term association with coronary heart disease and stroke. Nutr Metab Cardiovasc Dis 23(3):250–256. https://doi.org/10.1016/j.numecd.2012.02.006
Shutaywi M, Kachouie NN (2021) Silhouette analysis for performance evaluation in machine learning with applications to clustering. Entropy (Basel, Switzerland) 23(6):759. https://doi.org/10.3390/e23060759
Karanja NM, Obarzanek E, Lin PH, McCullough ML, Phillips KM, Swain JF, Champagne CM, Hoben KP (1999) Descriptive characteristics of the dietary patterns used in the Dietary Approaches to Stop Hypertension Trial. DASH Collaborative Research Group. J Am Diet Assoc 99(8 Suppl):S19-27. https://doi.org/10.1016/s0002-8223(99)00412-5
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395. https://doi.org/10.1249/01.Mss.0000078924.61453.Fb
Zung WW, Richards CB, Short MJ (1965) Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch Gen Psychiatry 13(6):508–515. https://doi.org/10.1001/archpsyc.1965.01730060026004
Barrett J, Hurst MW, DiScala C, Rose RM (1978) Prevalence of depression over a 12-month period in a nonpatient population. Arch Gen Psychiatry 35(6):741–744. https://doi.org/10.1001/archpsyc.1978.01770300083009
Momma H, Sawada SS, Sloan RA, Gando Y, Kawakami R, Terada S, Miyachi M, Kinugawa C, Okamoto T, Tsukamoto K, Huang C, Nagatomi R, Blair SN (2018) Importance of achieving a “fit” cardiorespiratory fitness level for several years on the incidence of type 2 diabetes mellitus: a Japanese cohort study. J Epidemiol 28(5):230–236. https://doi.org/10.2188/jea.JE20160199
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 157:107843. https://doi.org/10.1016/j.diabres.2019.107843
Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, Egusa G, Hiro T, Hirobe K, Iida M, Kihara S, Kinoshita M, Maruyama C, Ohta T, Okamura T, Yamashita S, Yokode M, Yokote K (2014) Other types of primary hyperlipoproteinemia(hyperlipidemia). Executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan–2012 version. J Atheroscler Thromb 21(2):82–85. https://doi.org/10.5551/jat.19141
Stanisz A. The accessible course of statistics with use the STATISTICA PL for medicine examples. Basic Stat StatSoft Poland, Cracow; 2006. p. 259–288. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=The+accessible+course+of+statistics+with+use+the+STATISTICA+PL+for+medicine+examples&btnG=
Lelong H, Blacher J, Baudry J, Adriouch S, Galan P, Fezeu L, Hercberg S, Kesse-Guyot E (2017) Individual and combined effects of dietary factors on risk of incident hypertension: prospective analysis from the NutriNet-Santé Cohort. Hypertension 70(4):712–720. https://doi.org/10.1161/hypertensionaha.117.09622
Schulze MB, Hoffmann K, Kroke A, Boeing H (2003) Risk of hypertension among women in the EPIC-Potsdam Study: comparison of relative risk estimates for exploratory and hypothesis-oriented dietary patterns. Am J Epidemiol 158(4):365–373. https://doi.org/10.1093/aje/kwg156
Laouali N, Benmarhnia T, Oulhote Y (2022) Potential benefits of joint hypothetical interventions on diet, lead, and cadmium on mortality in US adults. Environ Health 21(1):93. https://doi.org/10.1186/s12940-022-00905-4
Garcia-Larsen V, Morton V, Norat T, Moreira A, Potts JF, Reeves T, Bakolis I (2019) Dietary patterns derived from principal component analysis (PCA) and risk of colorectal cancer: a systematic review and meta-analysis. Eur J Clin Nutr 73(3):366–386. https://doi.org/10.1038/s41430-018-0234-7
Zhuo Z, Zhou Z (2020) Low dimensional discriminative representation of fully connected layer features using extended LargeVis method for high-resolution remote sensing image retrieval. Sensors (Basel, Switzerland) 20(17):4718. https://doi.org/10.3390/s20174718
Serneels S, Verdonck T (2008) Principal component analysis for data containing outliers and missing elements. Comput Stat Data Anal 52(3):1712–1727. https://doi.org/10.1016/j.csda.2007.05.024
Horak FB, Mancini M, Carlson-Kuhta P, Nutt JG, Salarian A (2016) Balance and gait represent independent domains of mobility in Parkinson disease. Phys Ther 96(9):1364–1371. https://doi.org/10.2522/ptj.20150580
Ferrari F, Dunson DB (2021) Bayesian factor analysis for inference on interactions. J Am Stat Assoc 116(535):1521–1532. https://doi.org/10.1080/01621459.2020.1745813
Mcinnes L, Healy J (2018) UMAP: Uniform Manifold Approximation and Projection for Dimension Reduction. J Open Sour Softw 3(29):861 (arXiv.1802.03426)
Becht E, McInnes L, Healy J, Dutertre CA, Kwok IWH, Ng LG, Ginhoux F, Newell EW (2018) Dimensionality reduction for visualizing single-cell data using UMAP. Nat Biotechnol. https://doi.org/10.1038/nbt.4314
Yang Y, Sun H, Zhang Y, Zhang T, Gong J, Wei Y, Duan YG, Shu M, Yang Y, Wu D, Yu D (2021) Dimensionality reduction by UMAP reinforces sample heterogeneity analysis in bulk transcriptomic data. Cell Rep 36(4):109442. https://doi.org/10.1016/j.celrep.2021.109442
Diaz-Papkovich A, Anderson-Trocmé L, Gravel S (2021) A review of UMAP in population genetics. J Hum Genet 66(1):85–91. https://doi.org/10.1038/s10038-020-00851-4
Jain AK (2010) Data clustering: 50 years beyond K-means. Pattern Recogn Lett 31(8):651–666. https://doi.org/10.1016/j.patrec.2009.09.011
Smith AD, Emmett PM, Newby PK, Northstone K (2011) A comparison of dietary patterns derived by cluster and principal components analysis in a UK cohort of children. Eur J Clin Nutr 65(10):1102–1109. https://doi.org/10.1038/ejcn.2011.96
Panagiotakos DB, Pitsavos C, Stefanadis C (2006) Dietary patterns: a Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metab Cardiovasc Dis 16(8):559–568. https://doi.org/10.1016/j.numecd.2005.08.006
Shin A, Lim S-Y, Sung J, Shin H-R, Kim J (2009) Dietary intake, eating habits, and metabolic syndrome in Korean men. J Am Diet Assoc 109(4):633–640. https://doi.org/10.1016/j.jada.2008.12.015
Pineda E, Ortega-Vélez MI, Preciado-Rodríguez M, Saucedo-Tamayo S, Caire-Juvera G (2022) Dietary patterns, cooking methods and breast cancer risk in Mexico: an exploratory case-control study. Nutr Health. https://doi.org/10.1177/02601060221119260
Kant AK, Graubard BI (2004) Eating out in America, 1987–2000: trends and nutritional correlates. Prev Med 38(2):243–249. https://doi.org/10.1016/j.ypmed.2003.10.004
Lachat C, Nago E, Verstraeten R, Roberfroid D, Van Camp J, Kolsteren P (2012) Eating out of home and its association with dietary intake: a systematic review of the evidence. Obes Rev 13(4):329–346. https://doi.org/10.1111/j.1467-789X.2011.00953.x
Fillion L, Henry C (1998) Nutrient losses and gains during frying: a review. Int J Food Sci Nutr 49(2):157–168. https://doi.org/10.3109/09637489809089395
Fabbri AD, Crosby GA (2016) A review of the impact of preparation and cooking on the nutritional quality of vegetables and legumes. Int J Gastron Food Sci 3:2–11. https://doi.org/10.1080/10408398.2014.989958
National Institutes of Health OoDS. Health Information. 2016. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/#h1.
Buratti S, Cappa C, Benedetti S, Giovanelli G (2020) Influence of cooking conditions on nutritional properties and sensory characteristics interpreted by E-senses: case-study on selected vegetables. Foods. https://doi.org/10.3390/foods9050607
Moradi Y, Bakar J, Motalebi A, Syed Muhamad S, Che Man Y (2011) A review on fish lipid: composition and changes during cooking methods. J Aquat Food Prod Technol 20(4):379–390. https://doi.org/10.1080/10498850.2011.576449
Konishi K (2021) Associations between healthy Japanese dietary patterns and depression in Japanese women. Public Health Nutr 24(7):1753–1765. https://doi.org/10.1017/s1368980020001548
Shi Z, El-Obeid T, Meftah Z, Alawi A, Said S, Ganji V (2022) Fast food and sweet intake pattern is directly associated with the prevalence of asthma in a Qatari population. Eur J Clin Nutr 76(3):428–433. https://doi.org/10.1038/s41430-021-00959-6
Zeballos E, Todd JE (2020) The effects of skipping a meal on daily energy intake and diet quality. Public Health Nutr 23(18):3346–3355. https://doi.org/10.1017/S1368980020000683
Thomas A, Boobyer C, Borgonha Z, Heuvel E, van den, Appleton, KM. (2021) Adding flavours: use of and attitudes towards sauces and seasonings in a sample of community-Dwelling UK older adults. Foods 10(11):2828. https://doi.org/10.3390/foods10112828
Monteiro JP, Fuzo CA, Ued FV, Kaput J (2021) Dietary patterns related to zinc and polyunsaturated fatty acids intake are associated with serum linoleic/dihomo-γ-linolenic ratio in NHANES males and females. Sci Rep 11(1):12215. https://doi.org/10.1038/s41598-021-91611-7
Hoffmann K, Schulze MB, Schienkiewitz A, Nöthlings U, Boeing H (2004) Application of a new statistical method to derive dietary patterns in nutritional epidemiology. Am J Epidemiol 159(10):935–944. https://doi.org/10.1093/aje/kwh134
Schulze MB, Hoffmann K, Kroke A, Boeing H (2001) Dietary patterns and their association with food and nutrient intake in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam study. Br J Nutr 85(3):363–373. https://doi.org/10.1079/bjn2000254
Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, Sampson L, Willett WC (1999) Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr 69(2):243–249. https://doi.org/10.1093/ajcn/69.2.243
Tahergorabi R, Beamer SK, Matak KE, Jaczynski J (2012) Isoelectric solubilization/precipitation as a means to recover protein isolate from striped bass (Morone saxatilis) and its physicochemical properties in a nutraceutical seafood product. J Agric Food Chem 60(23):5979–5987. https://doi.org/10.1021/jf3001197
Pettersen BJ, Anousheh R, Fan J, Jaceldo-Siegl K, Fraser GE (2012) Vegetarian diets and blood pressure among white subjects: results from the Adventist Health Study-2 (AHS-2). Public Health Nutr 15(10):1909–1916. https://doi.org/10.1017/s1368980011003454
Ndanuko RN, Tapsell LC, Charlton KE, Neale EP, Batterham MJ (2016) Dietary patterns and blood pressure in adults: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr 7(1):76–89. https://doi.org/10.3945/an.115.009753
Appel LJ (2017) The effects of dietary factors on blood pressure. Cardiol Clin 35(2):197–212. https://doi.org/10.1016/j.ccl.2016.12.002
Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J (2017) The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health 2(2):e108–e120. https://doi.org/10.1016/s2468-2667(17)30003-8
Qin P, Li Q, Zhao Y, Chen Q, Sun X, Liu Y, Li H, Wang T, Chen X, Zhou Q, Guo C, Zhang D, Tian G, Liu D, Qie R, Han M, Huang S, Wu X, Li Y, Feng Y, Yang X, Hu F, Hu D, Zhang M (2020) Sugar and artificially sweetened beverages and risk of obesity, type 2 diabetes mellitus, hypertension, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol 35(7):655–671. https://doi.org/10.1007/s10654-020-00655-y
Malik AH, Akram Y, Shetty S, Malik SS, Yanchou Njike V (2014) Impact of sugar-sweetened beverages on blood pressure. Am J Cardiol 113(9):1574–1580. https://doi.org/10.1016/j.amjcard.2014.01.437
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 71(19):e127–e248. https://doi.org/10.1016/j.jacc.2017.11.006
Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, Roccella EJ, Stout R, Vallbona C, Winston MC, Karimbakas J (2002) Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA 288(15):1882–1888. https://doi.org/10.1001/jama.288.15.1882
Sugimoto T, Shinozaki T, Naruse T, Miyamoto Y (2014) Who was concerned about radiation, food safety, and natural disasters after the great East Japan earthquake and Fukushima catastrophe? A nationwide cross-sectional survey in 2012. PLoS One 9(9):e106377. https://doi.org/10.1371/journal.pone.0106377
Aono T, Yoshida S, Akashi M (2016) Initial and present situation of food contamination in japan after the accident at the Fukushima Dai-ichi nuclear power plant. Radiat Prot Dosim 171(1):14–19. https://doi.org/10.1093/rpd/ncw183
Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell’Italia LJ, Calhoun DA (2009) Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension 54(3):475–481. https://doi.org/10.1161/hypertensionaha.109.131235
Patel SM, Cobb P, Saydah S, Zhang X, de Jesus JM, Cogswell ME (2015) Dietary sodium reduction does not affect circulating glucose concentrations in fasting children or adults: findings from a systematic review and meta-analysis. J Nutr 145(3):505–513. https://doi.org/10.3945/jn.114.195982
Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI, Chrysochoou CA, Nihoyannopoulos PI, Tousoulis DM (2020) Dietary approaches to stop hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr 11(5):1150–1160. https://doi.org/10.1093/advances/nmaa041
Dondi A, Candela E, Morigi F, Lenzi J, Pierantoni L, Lanari M (2020) Parents’ perception of food insecurity and of its effects on their children in Italy six months after the COVID-19 pandemic outbreak. Nutrients 13(1):121. https://doi.org/10.3390/nu13010121
Doustmohammadian A, Pishgar E, Clark CCT, Sobhrakhshankhah E, Nikkhah M, Faraji AH, Motamed N, Mansourian MR, Amirkalali B, Maadi M, Kasaii MS, Ebrahimi H, Zamani F (2022) Empirically-derived dietary patterns in relation to non-alcoholic fatty liver diseases among adult participants in Amol, Northern Iran: a structural equation modeling approach. Front Nutr 9:821544. https://doi.org/10.3389/fnut.2022.821544
Yan M, Liu Y, Wu L, Liu H, Wang Y, Chen F, Pei L, Zhao Y, Zeng L, Dang S, Yan H, Mi B (2022) The association between dietary purine intake and mortality: evidence from the CHNS cohort study. Nutrients 14(9):1718. https://doi.org/10.3390/nu14091718
Lampe L, Huppertz HJ, Anderl-Straub S, Albrecht F, Ballarini T, Bisenius S, Mueller K, Niehaus S, Fassbender K, Fliessbach K, Jahn H, Kornhuber J, Lauer M, Prudlo J, Schneider A, Synofzik M, Kassubek J, Danek A, Villringer A, Diehl-Schmid J, Otto M, Schroeter ML (2023) Multiclass prediction of different dementia syndromes based on multi-centric volumetric MRI imaging. Neuroimage Clin 37:103320. https://doi.org/10.1016/j.nicl.2023.103320
Kobayashi S, Honda S, Murakami K, Sasaki S, Okubo H, Hirota N, Notsu A, Fukui M, Date C (2012) Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J Epidemiol 22(2):151–159. https://doi.org/10.2188/jea.je20110075
Eicher-Miller HA, Boushey CJ (2017) How often and how Much? Differences in dietary intake by frequency and energy contribution vary among US. Adults in NHANES 2007–2012. Nutrients 9(1):86. https://doi.org/10.3390/nu9010086
Leung CW, Ding EL, Catalano PJ, Villamor E, Rimm EB, Willett WC (2012) Dietary intake and dietary quality of low-income adults in the Supplemental Nutrition Assistance Program. Am J Clin Nutr 96(5):977–988. https://doi.org/10.3945/ajcn.112.040014
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71(6):1269–1324. https://doi.org/10.1161/hyp.0000000000000066
Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, Harris KC, Nakhla M, Cloutier L, Gelfer M, Lamarre-Cliche M, Milot A, Bolli P, Tremblay G, McLean D, Padwal RS, Tran KC, Grover S, Rabkin SW, Moe GW, Howlett JG, Lindsay P, Hill MD, Sharma M, Field T, Wein TH, Shoamanesh A, Dresser GK, Hamet P, Herman RJ, Burgess E, Gryn SE, Grégoire JC, Lewanczuk R, Poirier L, Campbell TS, Feldman RD, Lavoie KL, Tsuyuki RT, Honos G, Prebtani APH, Kline G, Schiffrin EL, Don-Wauchope A, Tobe SW, Gilbert RE, Leiter LA, Jones C, Woo V, Hegele RA, Selby P, Pipe A, McFarlane PA, Oh P, Gupta M, Bacon SL, Kaczorowski J, Trudeau L, Campbell NRC, Hiremath S, Roerecke M, Arcand J, Ruzicka M, Prasad GVR, Vallée M, Edwards C, Sivapalan P, Penner SB, Fournier A, Benoit G, Feber J, Dionne J, Magee LA, Logan AG, Côté AM, Rey E, Firoz T, Kuyper LM, Gabor JY, Townsend RR, Rabi DM, Daskalopoulou SS (2018) Hypertension Canada’s 2018 Guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol 34(5):506–525. https://doi.org/10.1016/j.cjca.2018.02.022
Acknowledgements
The authors would like to acknowledge the study participants for their informed consent and the staff at the Sendai Oroshisho Center for their dedicated work.
Funding
This work was supported by JST, the establishment of university fellowships toward the creation of science technology innovation, Grant number JPMJFS2102. The authors acknowledge the “Pioneering Research Support Project” and were supported by a Grant-in-Aid for the “Knowledge Cluster Initiative” from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Contributions
LL: conceptualization, methodology, data analysis, interpretation, and original draft writing. HI: data analysis and interpretation, methodology, writing, review, and editing and supervised the study. HM: writing, review, and editing. HC: screening articles for inclusion criteria and planning the analysis. SSN: contributed to data analysis. YX: screened articles for inclusion criteria and planned the analysis. RN: methodology and supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethics approval and consent to participate
Written informed consent was obtained from all participants, and the protocol for the present study was approved by the Institutional Review Board of the Tohoku University Graduate School of Medicine (Approval Number: 2019-1-394)).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, L., Momma, H., Chen, H. et al. Dietary patterns associated with the incidence of hypertension among adult Japanese males: application of machine learning to a cohort study. Eur J Nutr 63, 1293–1314 (2024). https://doi.org/10.1007/s00394-024-03342-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-024-03342-w