Abstract
Background
Myelodysplastic syndromes (MDS) is a group of heterogeneous myeloid clonal diseases originating from hematopoietic stem cells. Clinically, elevated mature monocyte in bone marrow is often observed, but its clinical value still remains unclear.
Methods
We retrospectively analyzed a cohort of 216 MDS patients to explore the prognostic value of the percentage of mature monocyte in bone marrow (PMMBM). All patients were divided into elevated PMMBM group and the normal group by 6% PMMBM as the cut-off value.
Results
Our results showed that PMMBM> 6% was associated with inferior overall survival (OS) (P = 0.026) along with higher-risk IPSS-R (P = 0.025) and higher frequency of IDH2 mutation (P = 0.007). Multivariate analyses showed that besides older age (> 60 years) for OS, gender (male) for OS, lower neutrophil count (< 0.8 × 109/L) for OS, higher bone marrow blast percentage (> 5%) for OS and LFS, poorer karyotype for OS, elevated PMMBM was also an independent adverse prognostic factor for OS in MDS (P < 0.0001) but not for LFS (P = 0.736).
Conclusions
These findings indicate that increased PMMBM may assists Revised International Prognostic Scoring System (IPSS-R) to predict a poor outcome and provide a novel evaluation factor for MDS patients especially when their karyotype analyses fail.
Similar content being viewed by others
Background
Myelodysplastic syndromes (MDS), characterized by ineffective hematopoiesis, manifested by morphologic dysplasia in hematopoietic cells and peripheral cytopenia(s), is a group of heterogeneous myeloid clonal diseases originating from hematopoietic stem cells with a high risk of transforming to secondary acute myeloid leukemia (AML) [1]. The prognosis of MDS is extremely heterogeneous due to clinical and biological diversity. Herein, the International Prognostic Scoring System (IPSS) in 1997, the World Health Organization (WHO) Classification-Based Prognostic Scoring System (WPSS) in 2007, the MD Anderson Risk Model Score (MDAS) in 2008 and the Revised IPSS (IPSS-R) in 2012 were introduced to risk-stratify MDS patients [2,3,4,5]. Recently, lymphocyte-to-monocyte ratio and mutations such as TP53, SRSF2, IDH2 and ASXL1 were also demonstrated to predict the prognosis of MDS [6,7,8,9,10].
Before 2001, chronic myelomonocytic leukemia (CMML) was still categorized into MDS due to its MDS-like characteristics [11]. Unlike MDS, CMML is characterized by bone marrow (BM) dysplasia and persistent monocytosis, hence it is placed in a separate category of diseases [12]. Later, according to the 2016 revision of the WHO classification, CMML is subgrouped into 3-tiered blast-based categories: CMML-0 (peripheral blood (PB) < 2% and/or BM < 5%); CMML-1 (PB < 5%; BM < 10%) and CMML-2 (PB, 6 to 19%; BM, 10 to 19%) [13]. Under the prognostic model of IPSS-R, CMML-0 is in the very low and low-risk groups, CMML-1 in the low and intermediate groups, while most CMML-2 in the intermediate and high groups. Recently, Oligomonocytic CMML (OM-CMML) subtye (≥10% PB monocytes with absolute monocyte count (AMC) of 0.5–1 × 109/L) is proposed. Previous literatures reported that some patients initially manifest MDS characteristics could progress eventually into CMML [14, 15], a part of which belong to OM-CMML.
The monocyte includes monoblast, promonocyte, immature monocyte, and mature monocyte [16], among which monoblast and promonocyte together with myeloblast are regarded as “blast” [12]. However, clinical value of mature monocyte in BM remains unclear for “true” MDS. Hence, 216 MDS patients in our cohort were retrospectively analyzed to measure the prognostic value of the percentage of mature monocyte in bone marrow (PMMBM). Our results suggested that increased PMMBM was an independent predictor for adverse outcome in MDS.
Materials and methods
Patients
Clinical and follow-up data of 216 patients were collected who were diagnosed of MDS in Ningbo First Hospital from 2009 to 2018. Diagnosis and classification of MDS and leukemic transformation were made according to the 2016 WHO classification [1]. Risk stratifications of MDS were made according to IPSS-R [5]. Cases with follow-up for less than 6 months or fulfill the diagnostic criteria of OM-CMML and CMML were excluded from the analysis. More than half of the patients received symptomatic and supportive treatment. Sixty-nine patients acquired further treatment, of whom 49 patients (22.7%) were treated with intensive chemotherapy, 16 patients (7.4%) with hemopoietic stem cell transplantation (HSCT) and 4 patients (1.9%), hypomethylating agents. The range of the percentage of mature monocyte in normal BM differs in different reports [17, 18], so we set a control group of 100 non-hematological malignancy cases to determine the PMMBM range (4.4% ± 1.8%; mean ± SD) (data not shown). Thus all 216 MDS patients were grouped into two groups basing on 6% PMMBM as the cut-off value for further analyses. Approval for the retrospective review of these records was obtained from the Ethics Committee of Ningbo First Hospital and was in accordance with the Declaration of Helsinki. Informed consent was obtained from all adult subjects or parents if subjects are under 18.
Morphology analysis
The morphology of MDS myeloid cells were observed through Wright-Giemsa stained bone marrow smears. It was evaluated subjectively by light microscopy at low power (10 × objectives) for overall quality and distribution, and then was analyzed at high power (100 × oil objectives) for differential count including PMMBM count which was positively correlating with CD14 detected by flow cytometry (data not shown), with all cells in each containing field counted to maintain representative ratios of cell types [19]. All BM morphology findings were interpreted by two experienced and qualified clinical pathologists.
Cytogenetic analysis
BM cells were collected and cultured in RPMI-1640 medium supplemented with 20% newborn calf serum for 24 h. R-banded metaphases were karyotyped according to the International System for Human Cytogenetic Nomenclature (2016) (ISCN2016) [20].
Mutational analysis
Molecular analysis was performed as a part of the routine clinical work-up. Mutational analysis for 14 common genes of MDS including NRAS, DNMT3A, SF3B1, IDH1, IDH2, TET2, EZH2, JAK2, CBL, ETV6, TP53, SRSF2, ASXL1 and RUNX1 were performed with next generation sequencing.
Statistical analysis
Statistical analyses were performed by SPSS 21.0. OS was calculated from the date of initial diagnosis of MDS to the date of death, last follow-up or acquiring allo HSCT. Leukemia-free survival (LFS) was determined from the date of diagnosis to the date of leukemia transformation, last follow-up or acquiring allo HSCT. OS and LFS were analyzed using the Kaplan-Meier method and compared using the log-rank test. Multivariable analyses were used by Cox proportional hazard regression model. Differences in the distribution of continuous variables between categories were analyzed by Mann-Whitney U and categorical variables by Chi-squared test. The receiver operating characteristic (ROC) curve was used to evaluate the diagnostic value of PB monocyte for MDS and the optimal cutoff value was 0.1 × 109/L (data not shown). A P value of < 0.05 was considered statistically significant.
Results
Patients characteristics
A total of 216 patients of MDS including 99 females and 117 males were identified over a 10-year period with a median age of 61 years (range 16–90 years). Among these MDS patients, the median OS was 36 months (range 1–125 months, 95% CI 24.02–47.98 months) and 28 patients (13.0%) progressed to AML. Basing on the 2016 WHO classification, all patients were classified as MDS as follows: 29 (13.4%) MDS-SLD, 60 (27.8%) MDS-MLD, 13 (6.0%) MDS-RS, 47 (21.8%) MDS-EB1, 48 (22.2%) MDS-EB2, 1 (0.5%) MDS-del(5q), 18 (8.3%) MDS-U. Besides, 185 patients were stratified into IPSS-R risk groups as follows: 14 (7.6%) very low, 41 (22.2%) low, 64 (34.6%) intermediate, 33 (17.8%) high and 33 (17.8%) as very high. Of these, the median IPSS-R score was 4.0(1.0–10.0) and the average score was 4.4. Further information was provided in Table 1.
Elevated PMMBM in relation to clinical and laboratory factors
In our cohort, 216 patients were divided into two groups to analyze the correlation between elevated PMMBM and clinical and laboratory characteristics. It showed that the elevated PMMBM group had significantly higher counts of BM blast (P < 0.0001), higher PB monocyte percentage (P < 0.0001) and lower neutrophil counts (NE) (P = 0.022) as well as higher risk distribution in terms of IPSS-R (P = 0.025) compared with the normal PMMBM group. Also, the WHO subtype between these two groups had a significant difference (P = 0.005). Furthermore, in the elevated PMMBM group, 2 MDS patients were observed to evolve into CMML. There were no significant differences in other factors between two groups (Table 1).
Elevated PMMBM was accompanied with more mutation of IDH2
Mutations of 14 genes were detected in 57 patients, 41 (71.9%) of whom harbored mutations. Nine mutations with a minimum 5% frequency were identified in 14 genes in which ASXL1 mutation appeared the most (31.6%), followed by SRSF2 mutation (26.3%), TET2 mutation (15.8%), RUNX1 mutation (14.0%), ETV6, TP53 and DNMT3A mutations (both 10.5%), SF3B1 and IDH2 mutations (5.3%) (Fig. 1). The elevated PMMBM group harbored higher ratio of gene mutation in comparison with the normal PMMBM group, but the difference was not statistically significant (87.5% vs. 69.4%, P = 0.290). Among these mutations, the elevated PMMBM group showed higher mutation frequency of IDH2 compared with the normal PMMBM group (25.0% vs. 2.0%, P = 0.007).
Elevated PMMBM was sociated with a poor prognosis
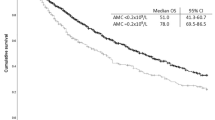
Compared with the normal PMMBM group, the median OS in the elevated PMMBM group was significantly shorter (24 months vs 37 months, P = 0.026; Fig. 2a). But when it comes to LFS, the significance was in borderline (P = 0.058; Fig. 2b).
In univariate analysis, OS was adversely associated with older age (> 60 years) (P < 0.0001), male (P = 0.002), higher-risk IPSS-R (P < 0.0001), higher BM blast percentage (> 5%) (P < 0.0001), lower hemoglobin (HB) (< 10 g/dl) (P = 0.003), NE (< 0.8 × 109/L) (P = 0.005) and PB monocyte counts (< 0.1 × 109/L) (P = 0.012) (Table 2).
Multivariate analyses showed that older age (> 60 years) (P < 0.0001), gender (male) (P = 0.047), higher BM blast percentage (> 5%) (P < 0.0001), lower NE counts (< 0.8 × 109/L) (P = 0.039) and poor karyotype (P = 0.011) were adverse factors and elevated PMMBM was a significant prognostic factor for worse OS (P < 0.0001) but not for LFS (P = 0.736) (Table 2).
Discussion
In our 216 MDS patients, elevated PMMBM was associated with a higher BM blast percentage at diagnosis, in accordance with higher IPSS-R scores. Our research suggested that elevated PMMBM was an independent adverse prognostic factor for OS.
A series of studies [14, 15, 21] have showed that a subgroup of MDS patients can evolve into CMML and present a poor prognosis. E. Schuler et al [22] conducted similar opinion that MDS patients with BM monocytic proliferation exerted CMML-like characteristics more often. However, the effect of elevated PMMBM on the prognosis of MDS remains unclear. To our knowledge, this study is the first to identify elevated PMMBM as the adverse prognostic impact on MDS. Recently, L Saeed et al [6] found that subnormal AMC of MDS was associated with an adverse OS in univariate analysis but not in multivariate analysis which is in accordance with our results. Nonetheless, elevated PMMBM is associated with adverse OS in our study.
The BM microenvironment is composed of BM stromal cells, mesenchymal stem cells, vascular endothelial cells, fibroblasts, mononuclear phagocyte system and cytokines [23]. Monocytes are essential cellular components of the host defense system. Due to their high plasticity, monocytes are involved in several cancer-associated processes including immune-tolerance, metastatic spread and neoangiogenesis along with M1 and M2-like macrophages induction [24, 25]. Recent studies have found that M2-like macrophages, called tumor-associated macrophages (TAMs), were involved in promoting tumor progression and metastasis by boosting angiogenesis, stimulating tumor cells’ proliferation, migration and invasion [26,27,28]. Although TAMs are initially considered to affect solid tumors, they are later found to predict poor outcomes in blood diseases such as lymphoma, leukemia and multiple myeloma [29]. But the roles of TAMs in MDS patients have not been fully elucidated. It is also considered that monocytes can contribute to tumor angiogenesis along with vascular endothelial growth factor (VEGF) to help tumor cells to evade the killing effect of immunocytes, and they can impede differentiation, maturation and proliferation of lymphocytes and promote survival of malignant T cells [30, 31]. Thus, we speculate that elevated PMMBM played an important role in the transformation and progression of MDS.
Further, it was demonstrated in our cohort that MDS patients with elevated PMMBM harbored higher BM blast percentage, PB monocyte count and especially IPSS-R score. It is well known that IPSS-R was widely used in measuring the prognosis of MDS since it was introduced in 2012 [5]. Our results showed that elevated PMMBM at the time of diagnosis significantly correlated with inferior outcomes and was closely accompanied with higher IPSS-R which is associated with a shorter OS.
In recent 10 years, recurrent somatic mutations in more than 50 genes have been demonstrated in 80–90% MDS [32], some of which are identified to predict the prognosis of this disease [7,8,9,10]. In our cohort, mutational analyses of 14 genes relevant to MDS were performed in 80 patients and elevated PMMBM patients harbored a higher mutational rate in IDH2.
IDH2 mutation as a DNA methylation regulatory gene can induce a block in cellular differentiation through epigenetic modifications, which plays an important role in contributing to premalignant disorders as well as oncogenesis [33,34,35]. It has been found in many solid tumors including gliomas, intrahepatic cholangiocarcinoma and enchondroma. Moreover, it has also rapidly been found in hematologic malignancies such as AML, MDS, myeloproliferative neoplasm, primary myelofibrosis and so on [36]. The prognostic impact of IDH2 in MDS remains controversial [8, 37,38,39,40]. But a large cohort study conducted that mutation of IDH2 was strongly associated with a short OS in MDS [41]. These results indicated that elevated PMMBM MDS patients could have distinct characteristics.
Conclusions
In summary, we demonstrated that elevated PMMBM accompanied with higher frequency of IDH2 mutation was associated with a poor prognosis. PMMBM as a prognostic factor could assist IPSS-R to provide a convenient for measuring the prognosis of MDS patients especially when their karyotype analysis fails.
Availability of data and materials
The data that support the findings of this study are available from Ningbo First Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Ningbo First Hospital. An Wu, the first author, should be contacted if someone wants to request the data from this study.
Abbreviations
- MDS:
-
Myelodysplastic syndromes
- PMMBM:
-
The percentage of mature monocyte in bone marrow
- OS:
-
Overall survival
- LFS:
-
Leukemia-free survival
- IPSS-R:
-
Revised International Prognostic Scoring System
- AML:
-
Acute myeloid leukemia
- IPSS:
-
International Prognostic Scoring System
- WHO:
-
World Health Organization
- WPSS:
-
World Health Organization Classification-Based Prognostic Scoring System
- MDAS:
-
The MD Anderson Risk Model Score
- CMML:
-
Chronic myelomonocytic leukemia
- BM:
-
Bone marrow
- PB:
-
Peripheral blood
- OM-CMML:
-
Oligomonocytic CMML
- AMC:
-
Absolute monocyte count
- HSCT:
-
Hemopoietic stem cell transplantation
- ISCN2016:
-
International System for Human Cytogenetic Nomenclature (2016)
- ROC:
-
Receiver operating characteristic curve
- NE:
-
Neutrophil
- HB:
-
Hemoglobin
- TAMs:
-
Tumor-associated macrophages
- VEGF:
-
Vascular endothelial growth factor
- PLT:
-
Platelet
- SF:
-
Serum ferritin
- β2-MG:
-
β2-microglobulin
- LDH:
-
lactate dehydrogenase
- MDS-SLD:
-
MDS with single lineage dysplasia
- MDS-MLD:
-
MDS with multilineage dysplasia
- MDS-RS:
-
MDS with ring sideroblasts
- MDS-EB:
-
MDS with excess blasts
- MDS-U:
-
MDS with unclassifiable
References
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. https://doi.org/10.1182/blood-2016-03-643544.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in Myelodysplastic syndromes. Blood. 1997;89(6):2079–88. https://doi.org/10.1182/blood.V89.6.2079.
Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R, et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007;25(23):3503–10. https://doi.org/10.1200/JCO.2006.08.5696.
Kantarjian H, O'Brien S, Ravandi F, Cortes J, Shan J, Bennett JM, et al. Proposal for a new risk model in myelodysplastic syndrome that accounts for events not considered in the original international prognostic scoring system. Cancer. 2008;113(6):1351–61. https://doi.org/10.1002/cncr.23697.
Schanz J, Tuchler H, Sole F, Mallo M, Luno E, Cervera J, et al. New comprehensive cytogenetic scoring system for primary myelodysplastic syndromes (MDS) and oligoblastic acute myeloid leukemia after MDS derived from an international database merge. J Clin Oncol. 2012;30(8):820–9. https://doi.org/10.1200/JCO.2011.35.6394.
Saeed L, Patnaik MM, Begna KH, Al-Kali A, Litzow MR, Hanson CA, et al. Prognostic relevance of lymphocytopenia, monocytopenia and lymphocyte-to-monocyte ratio in primary myelodysplastic syndromes: a single center experience in 889 patients. Blood Cancer J. 2017;7(3):e550. https://doi.org/10.1038/bcj.2017.30.
Ren Y, Mei C, Ye L, Luo Y, Zhou X, Yang H, et al. Analysis of clinical and molecular features of MDS patients with complex karyotype in China. Blood Cells Mol Dis. 2019;75:13–9. https://doi.org/10.1016/j.bcmd.2018.11.006.
Tefferi A, Lasho TL, Patnaik MM, Saeed L, Mudireddy M, Idossa D, et al. Targeted next-generation sequencing in myelodysplastic syndromes and prognostic interaction between mutations and IPSS-R. Am J Hematol. 2017;92(12):1311–7. https://doi.org/10.1002/ajh.24901.
Arbab Jafari P, Ayatollahi H, Sadeghi R, Sheikhi M, Asghari A. Prognostic significance of SRSF2 mutations in myelodysplastic syndromes and chronic myelomonocytic leukemia: a meta-analysis. Hematology (Amsterdam, Netherlands). 2018;23(10):778–84.
Lin P, Luo Y, Zhu S, Maggio D, Yang H, Hu C, et al. Isocitrate dehydrogenase 2 mutations correlate with leukemic transformation and are predicted by 2-hydroxyglutarate in myelodysplastic syndromes. J Cancer Res Clin Oncol. 2018;144(6):1037–47. https://doi.org/10.1007/s00432-018-2627-3.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51(2):189–99. https://doi.org/10.1111/j.1365-2141.1982.tb08475.x.
Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) classification of the myeloid neoplasms. Blood. 2002;100(7):2292–302. https://doi.org/10.1182/blood-2002-04-1199.
Orazi A, Bennett JM, Germing U, et al. Chronic Myelomonocytic Leukemia. In: SHCE S, Harris NL, Jaffe ES, et al., editors. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC; 2017. p. 82–6.
Selimoglu-Buet D, Badaoui B, Benayoun E, Toma A, Fenaux P, Quesnel B, et al. Accumulation of classical monocytes defines a subgroup of MDS that frequently evolves into CMML. Blood. 2017;130(6):832–5. https://doi.org/10.1182/blood-2017-04-779579.
Wang SA, Galili N, Cerny J, Sechman E, Chen SS, Loew J, et al. Chronic myelomonocytic leukemia evolving from preexisting myelodysplasia shares many features with de novo disease. Am J Clin Pathol. 2006;126(5):789–97.
Goasguen JE, Bennett JM, Bain BJ, Vallespi T, Brunning R, Mufti GJ. Morphological evaluation of monocytes and their precursors. Haematologica. 2009;94(7):994–7. https://doi.org/10.3324/haematol.2008.005421.
Wenrong Xu JW. Clinical hematologic examination. 5th ed. Beijing: People's sanitary publishing press; 2012.
Bain BJ. The bone marrow aspirate of healthy subjects. Br J Haematol. 1996;94(1):206–9. https://doi.org/10.1046/j.1365-2141.1996.d01-1786.x.
Reagan WJ, Irizarry-Rovira A, Poitout-Belissent F, Bolliger AP, Ramaiah SK, Travlos G, et al. Best practices for evaluation of bone marrow in nonclinical toxicity studies. Toxicol Pathol. 2011;39(2):435–48. https://doi.org/10.1177/0192623310396907.
McGowan-Jordan J, Simons A, Schmid M. ISCN 2016: An International System for Human Cytogenomic Nomenclature (2016). Basel: S KARGER AG; 2016.
Valent P. Oligo-monocytic CMML and other pre-CMML states: clinical impact, prognostication and management. Best Pract Res Clin Haematol. 2020;33(2):101137. https://doi.org/10.1016/j.beha.2019.101137.
Schuler E, Frank F, Hildebrandt B, Betz B, Strupp C, Rudelius M, et al. Myelodysplastic syndromes without peripheral monocytosis but with evidence of marrow monocytosis share clinical and molecular characteristics with CMML. Leuk Res. 2018;65(undefined):1–4.
Shafat MS, Gnaneswaran B, Bowles KM, Rushworth SA. The bone marrow microenvironment - Home of the leukemic blasts. (1532-1681 (Electronic)).
Canè S, Ugel S, Trovato R, Marigo I, De Sanctis F, Sartoris S, et al. The endless Saga of monocyte diversity. Front Immunol. 2019;10:1786. https://doi.org/10.3389/fimmu.2019.01786.
Geissmann F, Manz MG, Jung S, Sieweke MH, Merad M, Ley K. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327(5966):656–61. https://doi.org/10.1126/science.1178331.
Pollard JW. Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer. 2004;4(1):71–8. https://doi.org/10.1038/nrc1256.
Ruffell B, Affara NI, Coussens LM. Differential macrophage programming in the tumor microenvironment. Trends Immunol. 2012;33(3):119–26. https://doi.org/10.1016/j.it.2011.12.001.
Yao RR, Li JH, Zhang R, Chen RX, Wang YH. M2-polarized tumor-associated macrophages facilitated migration and epithelial-mesenchymal transition of HCC cells via the TLR4/STAT3 signaling pathway. World J Surg Oncol. 2018;16(1):9. https://doi.org/10.1186/s12957-018-1312-y.
Petty AJ, Yang Y. Tumor-Associated Macrophages in Hematologic Malignancies: New Insights and Targeted Therapies. Cells. 2019;8(12):1526. https://doi.org/10.3390/cells8121526.
Wilcox RA, Wada DA, Ziesmer SC, Elsawa SF, Comfere NI, Dietz AB, et al. Monocytes promote tumor cell survival in T-cell lymphoproliferative disorders and are impaired in their ability to differentiate into mature dendritic cells. Blood. 2009;114(14):2936–44. https://doi.org/10.1182/blood-2009-05-220111.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44. https://doi.org/10.1038/nature07205.
Hosono N. Genetic abnormalities and pathophysiology of MDS. Int J Clin Oncol. 2019;24(8):885–92. https://doi.org/10.1007/s10147-019-01462-6.
Koivunen P, Lee S, Duncan CG, Lopez G, Lu G, Ramkissoon S, et al. Transformation by the (R)-enantiomer of 2-hydroxyglutarate linked to EGLN activation. Nature. 2012;483(7390):484–8. https://doi.org/10.1038/nature10898.
Xu W, Yang H, Liu Y, Yang Y, Wang P, Kim SH, et al. Oncometabolite 2-hydroxyglutarate is a competitive inhibitor of alpha-ketoglutarate-dependent dioxygenases. Cancer Cell. 2011;19(1):17–30. https://doi.org/10.1016/j.ccr.2010.12.014.
Lu C, Ward PS, Kapoor GS, Rohle D, Turcan S, Abdel-Wahab O, et al. IDH mutation impairs histone demethylation and results in a block to cell differentiation. Nature. 2012;483(7390):474–8. https://doi.org/10.1038/nature10860.
Dang L, Yen K, Attar EC. IDH mutations in cancer and progress toward development of targeted therapeutics. Ann Oncol. 2016;27(4):599–608. https://doi.org/10.1093/annonc/mdw013.
Bejar R, Stevenson K, Abdel-Wahab O, Galili N, Nilsson B, Garcia-Manero G, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011;364(26):2496–506. https://doi.org/10.1056/NEJMoa1013343.
Kosmider O, Gelsi-Boyer V, Slama L, Dreyfus F, Beyne-Rauzy O, Quesnel B, et al. Mutations of IDH1 and IDH2 genes in early and accelerated phases of myelodysplastic syndromes and MDS/myeloproliferative neoplasms. Leukemia. 2010;24(5):1094–6. https://doi.org/10.1038/leu.2010.52.
Lin TL, Nagata Y, Kao HW, Sanada M, Okuno Y, Huang CF, et al. Clonal leukemic evolution in myelodysplastic syndromes with TET2 and IDH1/2 mutations. Haematologica. 2014;99(1):28–36. https://doi.org/10.3324/haematol.2013.091249.
Nazha A, Bejar R. Molecular data and the IPSS-R: how mutational burden can affect prognostication in MDS. Curr Hematol Malig Rep. 2017;12(5):461–7. https://doi.org/10.1007/s11899-017-0407-9.
Bejar R, Papaemmanuil E, Haferlach T, Garcia-Manero G, Maciejewski JP, Sekeres MA, et al. Somatic mutations in MDS patients are associated with clinical features and predict prognosis independent of the IPSS-R: analysis of combined datasets from the international working Group for Prognosis in MDS-Molecular Committee. Blood. 2015;126(23):907. https://doi.org/10.1182/blood.V126.23.907.907.
Acknowledgements
Not applicable.
Funding
This research was supported by Zhejiang Provincial Natural Science Foundation of China under Grant No. (LY20H080001 and LY17H160005), the Medical and Health Science and Technology Projects of Zhejiang Province (2019KY158, 2019KY170, and 2019KY171), the National Science Foundation of Ningbo (2018A610390 and 2016A610152), and the Chinese Medicine Science and Technology Plan Project of Zhejiang Province (2015ZZ018).
Author information
Authors and Affiliations
Contributions
A.W. collected and analyzed data and was a major contributor in writing the manuscript. L.S., G.O. and Q.M. designed research and reviewed the manuscript. P.G., N.W., C.S., Z.H., C.R. and Y.S. collected data. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Approval for the retrospective review of these records was obtained from the Ethics Committee of Ningbo First Hospital (2020-R196) and was in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, A., Gao, P., Wu, N. et al. Elevated mature monocytes in bone marrow accompanied with a higher IPSS-R score predicts a poor prognosis in myelodysplastic syndromes. BMC Cancer 21, 546 (2021). https://doi.org/10.1186/s12885-021-08303-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08303-8