Abstract
Purpose of Review
The purpose of this study is to review established prognostic models in myelodysplastic syndromes (MDS) and describe how molecular data can be used to improve patient risk stratification.
Recent Findings
Somatic mutations are common in MDS and are associated with disease features including outcomes. Several recurrently mutated genes have prognostic significance independent of risk stratification tools used in practice. However, this prognostic impact can depend on the clinicogenetic context in which mutations occur. Qualitatively, SF3B1 mutations appear favorable only in patients with < 5% bone marrow blasts while mutations of several genes, including ASXL1, SRSF2, U2AF1, NRAS, and IDH2, appear adverse in this context. Mutations of TP53, RUNX1, and EZH2 appear adverse regardless of blast percentage. Consensus on how to best incorporate mutations into risk assessment is still being developed.
Summary
Somatic mutations can refine risk stratification and improve the accuracy of existing prognostic models, often upstaging or downstaging patients across the boundary of higher- and lower-risk MDS.

Similar content being viewed by others
References
Bejar R, Steensma DP. Myelodysplastic syndromes. In: Kaushansky K, Lichtman MA, Prchal JT, Levi MM, Press OW, Burns LJ, et al., editors. Williams hematology. New York: McGraw-Hill Education; 2015. p. 9e.
Tefferi A, Vardiman JW. Myelodysplastic syndromes. N Engl J Med. 2009;361(19):1872–85.
Greenberg PL, Stone RM, Al-Kali A, Barta SK, Bejar R, Bennett JM, et al. Myelodysplastic syndromes, version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2017;15(1):60–87.
Malcovati L, Hellstrom-Lindberg E, Bowen D, Ades L, Cermak J, Del Canizo C, et al. Diagnosis and treatment of primary myelodysplastic syndromes in adults: recommendations from the European LeukemiaNet. Blood. 2013;122(17):2943–64.
Sekeres MA, Cutler C. How we treat higher-risk myelodysplastic syndromes. Blood. 2014;123(6):829–36.
Fenaux P, Adès L. How we treat lower-risk myelodysplastic syndromes. Blood. 2013;121(21):4280–6.
Malcovati L, Della Porta MG, Strupp C, Ambaglio I, Kuendgen A, Nachtkamp K, et al. Impact of the degree of anemia on the outcome of patients with myelodysplastic syndrome and its integration into the WHO classification-based prognostic scoring system (WPSS). Haematologica. 2011;96(10):1433–40.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89(6):2079–88.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65.
Kantarjian H, O'Brien S, Ravandi F, Cortes J, Shan J, Bennett JM, et al. Proposal for a new risk model in myelodysplastic syndrome that accounts for events not considered in the original international prognostic scoring system. Cancer. 2008;113(6):1351–61.
Garcia-Manero G, Shan J, Faderl S, Cortes J, Ravandi F, Borthakur G, et al. A prognostic score for patients with lower risk myelodysplastic syndrome. Leukemia. 2008;22(3):538–43.
Nazha A, Sekeres MA. Improving prognostic modeling in myelodysplastic syndromes. Curr Hematol Malig Rep. 2016;11(6):395–401.
Bejar R. Prognostic models in myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2013;2013:504–10.
Bejar R, Papaemmanuil E, Haferlach T, Garcia-Manero G, Maciejewski JP, Sekeres MA, et al. Somatic mutations in MDS patients are associated with clinical features and predict prognosis independent of the IPSS-R: analysis of combined datasets from the international working group for prognosis in MDS-molecular committee. Blood. 2015;126(23):907. -
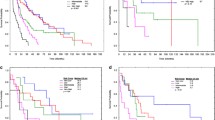
Bejar R, Stevenson K, Abdel-Wahab O, Galili N, Nilsson B, Garcia-Manero G, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011;364(26):2496–506.
Papaemmanuil E, Gerstung M, Malcovati L, Tauro S, Gundem G, Van Loo P, et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood. 2013;122(22):3616–27.
Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G, et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia. 2014;28(2):241–7.
Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R, et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol Off J Am Soc Clin Oncol. 2007;25(23):3503–10.
Nazha A, Seastone D, Keng M, Hobson S, Kalaycio M, Maciejewski JP, et al. The revised international prognostic scoring system (IPSS-R) is not predictive of survival in patients with secondary myelodysplastic syndromes. Leuk Lymphoma. 2015;56(12):3437–9. https://doi.org/10.3109/10428194.2015.1041391.
Quintas-Cardama A, Daver N, Kim H, Dinardo C, Jabbour E, Kadia T, et al. A prognostic model of therapy-related myelodysplastic syndrome for predicting survival and transformation to acute myeloid leukemia. Clin Lymphoma Myeloma Leuk. 2014;14(5):401–10.
Padron E, Garcia-Manero G, Patnaik MM, Itzykson R, Lasho T, Nazha A, et al. An international data set for CMML validates prognostic scoring systems and demonstrates a need for novel prognostication strategies. Blood Cancer J. 2015;5:e333.
Nazha A, Komrokji RS, Garcia-Manero G, Barnard J, Roboz GJ, Steensma DP, et al. The efficacy of current prognostic models in predicting outcome of patients with myelodysplastic syndromes at the time of hypomethylating agent failure. Haematologica. 2016;101(6):224–7. https://doi.org/10.3324/haematol.2015.140962.
Garcia-Manero G, Gore SD, Kambhampati S, Scott B, Tefferi A, Cogle CR, et al. Efficacy and safety of extended dosing schedules of CC-486 (oral azacitidine) in patients with lower-risk myelodysplastic syndromes. Leukemia. 2016;30(4):889–96.
Bejar R, Stevenson KE, Caughey BA, Abdel-Wahab O, Steensma DP, Galili N, et al. Validation of a prognostic model and the impact of mutations in patients with lower-risk myelodysplastic syndromes. J Clin Oncol. 2012;30(27):3376–82.
Sekeres MA, Swern AS, Fenaux P, Greenberg PL, Sanz GF, Bennett JM, et al. Validation of the IPSS-R in lenalidomide-treated, lower-risk myelodysplastic syndrome patients with del(5q). Blood Cancer J. 2014;4:e242.
Gerds AT, Gooley TA, Wilson WA, Deeg HJ. Components of the revised international prognostic scoring system and outcome after hematopoietic cell transplantation for myelodysplastic syndrome. Blood. 2013;121(19):4007–8.
Della Porta MG, Alessandrino EP, Bacigalupo A, van Lint MT, Malcovati L, Pascutto C, et al. Predictive factors for the outcome of allogeneic transplantation in patients with MDS stratified according to the revised IPSS-R. Blood. 2014;123(15):2333–42.
Zeidan AM, Sekeres MA, Garcia-Manero G, Steensma DP, Zell K, Barnard J, et al. Comparison of risk stratification tools in predicting outcomes of patients with higher-risk myelodysplastic syndromes treated with azanucleosides. Leukemia. 2016;30(3):649–57. https://doi.org/10.1038/leu.2015.283.
Walter MJ, Shen D, Ding L, Shao J, Koboldt DC, Chen K, et al. Clonal architecture of secondary acute myeloid leukemia. N Engl J Med. 2012;366(12):1090–8.
Makishima H, Yoshizato T, Yoshida K, Sekeres MA, Radivoyevitch T, Suzuki H, et al. Dynamics of clonal evolution in myelodysplastic syndromes. Nat Genet. 2017;49(2):204–12.
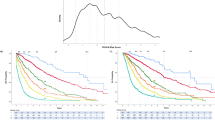
Nazha A, Narkhede M, Radivoyevitch T, Seastone DJ, Patel BJ, Gerds AT, et al. Incorporation of molecular data into the revised international prognostic scoring system in treated patients with myelodysplastic syndromes. Leukemia. 2016;30(11):2214–20.
Malcovati L, Karimi M, Papaemmanuil E, Ambaglio I, Jadersten M, Jansson M, et al. SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood. 2015;126(2):233–41.
Al-Issa K, Sekeres MA, Nielsen A, Jha B, Przychodzen BP, Aly M, et al. <em>TP53</em> mutations and outcome in patients with myelodysplastic syndromes (MDS). Blood. 2016;128(22):4336. -
Bejar R, Stevenson KE, Caughey B, Lindsley RC, Mar BG, Stojanov P, et al. Somatic mutations predict poor outcome in patients with myelodysplastic syndrome after hematopoietic stem-cell transplantation. J Clin Oncol Off J Am Soc Clin Oncol. 2014;32(25):2691–8.
Della Porta MG, Galli A, Bacigalupo A, Zibellini S, Bernardi M, Rizzo E, et al. Clinical effects of driver somatic mutations on the outcomes of patients with myelodysplastic syndromes treated with allogeneic hematopoietic stem-cell transplantation. J Clin Oncol Off J Am Soc J Clin Oncol. 2016. https://doi.org/10.1200/JCO.2016.67.3616.
Yoshizato T, Nannya Y, Atsuta Y, Shiozawa Y, Iijima-Yamashita Y, Yoshida K, et al. Impact of genetic alterations in stem-cell transplantation for myelodysplasia and secondary acute myeloid leukemia. Blood. 2017;129(17):2347–58. https://doi.org/10.1182/blood-2016-12-754796.
Lindsley RC, Saber W, Mar BG, Redd R, Wang T, Haagenson MD, et al. Prognostic mutations in myelodysplastic syndrome after stem-cell transplantation. N Engl J Med. 2017;376(6):536–47.
Bejar R. Clinical and genetic predictors of prognosis in myelodysplastic syndromes. Haematologica. 2014;99(6):956–64.
Al-Issa K, Zarzour A, Radivoyevitch T, Kalaycio M, Hamilton BK, Gerds AT, et al. Incorporation of molecular data into the current prognostic models in treated patients with myelodysplastic syndromes: which model is the best. Blood. 2016;128(22):50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Aziz Nazha declares no potential conflicts of interest.
Rafael Bejar reports personal fees and other from Genoptix, grants, personal fees and other from Celgene, other from AbbVie, personal fees and other from Foundation Medicine, and other from Otsuka/Astex, outside the submitted work. In addition, Dr. Bejar has a patent prognostic mutation signature in MDS with royalties paid.
Human and Animal Rights and Informed Consent
This article contains no studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Myelodysplastic Syndromes
Rights and permissions
About this article
Cite this article
Nazha, A., Bejar, R. Molecular Data and the IPSS-R: How Mutational Burden Can Affect Prognostication in MDS. Curr Hematol Malig Rep 12, 461–467 (2017). https://doi.org/10.1007/s11899-017-0407-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-017-0407-9