Abstract
Background
Vaccination against COVID-19 continues apace, but side-effects, both common and severe, continue to be reported. We report here the first published case of COVID-19 vaccine-related encephalitis.
Case presentation
A young woman presented with acute neuropsychiatric symptoms following recent ChAdOx1 nCoV-19 vaccination. Extensive investigation did not identify alternative causes.
Conclusions
This difficult case is here described, including presentation, investigation, and management. Further study on neuropsychiatric side-effects of COVID-19 vaccination, including investigation as to whether there may be a causal link, is required.
Similar content being viewed by others
Key points
-
Management of acute neuropsychiatric presentations in young patients is challenging.
-
The temporal association, together with the clinical syndrome and lack of other causes on investigation suggests a possible COVID-19 vaccine-related encephalitis by Graus criteria.
-
Further research to determine causation of neurological symptoms after COVID-19 vaccination is required; in particular, determination of those that may be coincidental, and, where causation is possible, mechanisms, biomarkers, and case management.
Background
Vaccination against SARS-CoV-2 has proceeded apace in 2021 with several vaccine candidates. Reports of side effects, both common and rarer, are emerging. Here we present the first published case of ChAdOx1 nCoV-19 vaccine-associated encephalitis and the challenges inherent in our patient’s management.
Case presentation
A 22-year-old woman of Middle Eastern origin, born in Iran and recently living in Western Europe, presented to a UK hospital with a three-week history of intermittent frontal headache and fatigue a few days after she received her second dose of AstraZeneca ChAdOx1 nCoV-19 vaccine. These symptoms did not respond to paracetamol and progressed on to an acute two-day history of confusion and hallucinations (visual and tactile). She reported seeing “disco balls” and experiencing someone touching her skin. She had non-syndromic retinitis pigmentosa but no other medical co-morbidities, and there was no personal or family history of psychiatric illness. She was a non-smoker and non-drinker, and enjoying undergraduate studies at university.
On admission, she had one recorded fever of 38ºC, but otherwise-normal observations (HR 91, BP 123/81, RR 18, O2 saturations 100% on air). She was alert but disorientated to time, person and place, and agitated with a labile affect; she complained of auditory and visual hallucinations – for example, that the room was on fire – and delusions that were often hyper-religious in nature. She was also seen to be gesturing to the air as if responding to unseen stimuli. On examination, excepting very restricted visual fields, there was no focal neurology, meningism or photophobia, and cardio-respiratory and abdominal examination was normal. Initial investigations revealed Hb 126 g/L, WCC 6.6 × 109/L (neutrophils 4.6 × 109/L), CRP 1.1 mg/L (reference range < 5 mg/L), normal renal and liver function, platelets 275 × 109/L, and D-dimer of 1,240 ng/mL (reference range < 500 ng/mL). Chest X-ray was unremarkable, urine microscopy and culture negative, and PCR for SARS-CoV-2 and other respiratory viruses was negative (see Table 1). She was empirically commenced on intravenous ceftriaxone 2 g BD and acyclovir 800 mg TDS for possible meningo-encephalitis pending lumbar puncture (LP). She was transferred to the Infectious Diseases ward.
Initially she required rapid pharmacological tranquilisation with lorazepam and haloperidol to manage extreme agitation. CT head and CT venogram were unremarkable. Initial LP, performed 2 days after the fever, revealed an opening pressure of 30 cm H2O and WCC 6 cells/µL (100% lymphocytes) with negative microbiology and virology (see Table 2) on cerebrospinal fluid (CSF) analysis. She had no further recorded fevers throughout her admission and antibiotics and antivirals were stopped.
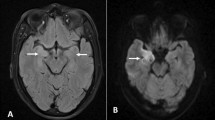
Her psychotic symptoms continued in the second week, and due to dystonia, the haloperidol was switched to regular olanzapine, titrated to a maximum of 7.5 mg/day, and PRN promethazine. MRI brain on day 7 was normal, and EEG on day 8 was also normal with no evidence of seizure activity or encephalopathy. CT imaging of the abdomen was not performed due to the patient’s age. Abdominal and pelvic ultrasound was therefore conducted to exclude ovarian teratoma as a secondary cause of autoimmune encephalopathy, and this was also normal. A second LP on day 7 showed abnormal WCC of 18 cells/µL (100% lymphocytes) and her CSF was positive for IgG oligoclonal bands (with negative paired serum oligoclonal bands). Serum and CSF was sent to UK national neuro-immunology and infection reference laboratories in Oxford and London, and Porton Down, respectively, with a variety of specialist tests undertaken (Table 1) based on the clinical history. Cell surface antibodies were tested using commercial kit-based assays. Her case was discussed in the encephalitis multidisciplinary team (MDT) meeting at the National Hospital for Neurology & Neurosurgery, UK, and a possibility of autoimmune encephalitis secondary to the COVID-19 vaccine was considered given the temporal association and CSF pleocytosis (possible autoimmune encephalitis by Graus criteria [1]). However, a decision was made to avoid giving any steroids or other immunomodulatory therapy given the possibility of an infective cause pending repeat LP and given early improvements in her clinical state.
In the third week her symptoms improved with no further hallucinations and a Montreal Cognitive Assessment (MoCA) score of 22/30, and she was weaned off olanzapine. She had a third lumbar puncture on day 14, second EEG on day 22, and a second MRI on day 23, which were all normal. Other investigations were undertaken (see Table 1). She had a mild relapse in her delirium with psychotic symptoms, with simple auditory and visual hallucinations (seeing “green lights” and hearing “the sound of coins pouring into a dish”, hyper-religiosity, continuous praying and labile mood). Neurological examination remained normal, with no unresponsive episodes, witnessed involuntary movements, seizure activity, or evidence of aura. These features stabilised with resumption of olanzapine (titrated to 5 mg twice-daily), and she was successfully discharged with ongoing follow-up with Neurology and Psychiatry. The case was notified to the national COVID-19 vaccine adverse event reporting scheme.
One month after discharge she remains on low dose olanzapine and is functionally well with independent activities of daily living. However, her family report that she has not recovered back to her pre-morbid state. She is quieter and more withdrawn now, and still has residual psychotic symptoms of occasionally seeing green lights and praying more than before.
Discussion and conclusion
This case presented substantial challenges for the treating medical team, not least due to the patient’s distress during her illness and the diagnostic conundrum presented. Neurology opinion was sought locally with input from the regional referral centre. Extensive involvement of Psychiatry colleagues was also paramount in management.
The presentation was of a limbic encephalitis. Neuroborreliosis was considered, but with absence of epidemiological risk such as travel to endemic areas within the UK or abroad, negative serum serology, normal brain imaging, and resolution of the CSF pleiocytosis, it was felt that this was unlikely; and there was an extensive workup for common known viruses. The variety of investigations outlined above aimed to identify autoimmune and paraneoplastic causes. Shin et al. provide further discussion of aetiology and management [2].
Isolated reports exist of anti-NMDA receptor–associated encephalitis following Japanese encephalitis, H1N1, and diphtheria, tetanus, pertussis and polio vaccinations, with plausible biochemical evidence of causality [3].
It is known that psychiatric illness, delirium, encephalopathy and encephalitis may complicate COVID-19 [4, 5], and potential biomarkers exist to support these diagnoses alongside imaging changes [6]. In this patient, however, multiple negative SARS-CoV-2 PCR tests made this diagnosis less likely, although an asymptomatic COVID-19infection around the time of vaccination cannot be excluded.
To our knowledge, there have not yet been any published case reports of encephalopathy, encephalitis, or neuropsychiatric syndromes following vaccination against COVID-19. Data from clinical trials until early in the global vaccination campaign was incomplete but overall reassuring [7]. The initial ChAdOx1 nCoV-19 Oxford vaccine trial was paused following a case of transverse myelitis that later was confirmed to be multiple sclerosis (MS), but there were no documented cases of encephalitis or psychosis in 12,408 participants vaccinated between April and December 2020 [8]. Yellow Card adverse incident reports to the UK Medicines & Healthcare Regulatory Agency (MHRA) from 4 January 2021 to 16 June 2021 list 32 cases of ‘encephalitis’, 4 cases of ‘noninfective encephalitis’, and 3 cases of ‘autoimmune encephalopathy’ temporally associated with ChAdOx1 nCoV-19 administration [9]. Various psychiatric conditions are also listed. It is not yet possible to analyse comprehensively the reports presented.
Whilst temporal relationship is not indicative of causation, the clinical syndrome, coupled with evidence of inflammatory changes in cerebrospinal fluid, and lack of evidence of an infective or immune-mediated cause, would plausibly fit with vaccine-induced encephalitis and encephalopathy. Determination of causality in this relationship is not currently possible as no specific test yet exists [10]. On this basis, a claim for litigation for a case of ‘acute encephalopathy’ reported in a ChAdOx1 nCoV-19 trial participant in India was dismissed as no evidence could be found of a causal link [11].
There is an association of psychosis and neurological complications after COVID-19, including high rates of stroke (such as in the study by Taquet et al. [12]), but overwhelming evidence suggests that vaccination is safe and effective, and that such risks are minimal compared to COVID-19 infection in the unvaccinated.
In summary, we believe that the patient presented in this case may have experienced a rare side-effect of COVID-19 vaccination, in the absence of another identifiable cause. Uncertainty remains, and there is no current definitive proof of causality for the patient’s symptoms and signs. Further work is urgently required to clarify this association and compare data with pre-pandemic disease incidence, to determine the mechanism involved, and to formulate appropriate treatment strategies. Encephalitis is a recognised complication of COVID-19 and at far greater rates than our sole case of uncertain causation with vaccination.
Patient perspective
My illness started as a headache, slowly becoming throbbing and waking me at night. Nineteen days after receiving my second vaccine dose, I started to hallucinate right after feeling euphoric. I then hallucinated silhouettes running past me in slow motion. We initially thought it could be cerebral venous thrombosis. The CT scan turned out to be normal. The first two weeks I spent at the hospital were very difficult: I only remember my hallucinations and don’t recall anything else (including the staff). I also remember being convinced that I had schizophrenia and was very distraught.
However, I was beginning to recover towards the third week of my stay and was no longer hallucinating frightening things. The last two weeks I spent at the hospital were wonderful; I remember the staff and they took excellent care of me. My recovery would’ve taken longer if it wasn’t for the staff and their caring and considerate attitude. The time I spent with the nurses allowed me to gain an insight into what it takes to be a nurse, and I hope to apply for further study next year. Overall, my experience at the hospital was very positive and that was made possible by the staff.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- BP:
-
Blood pressure
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- EEG:
-
Electroencephalogram
- HR:
-
Heart rate
- LP:
-
Lumbar puncture
- MoCA:
-
Montreal Cognitive Assessment
- MRI:
-
Magnetic resonance imaging
- MS:
-
Multiple sclerosis
- PCR:
-
Polymerase chain reaction
- RR:
-
Respiratory rate
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome Coronavirus 2
References
Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391–404. https://doi.org/10.1016/S1474-4422(15)00401-9.[published20February2016].
Shin Y-W, Lee S-T, Park K-I, et al. Treatment strategies for autoimmune encephalitis. Ther Adv Neurol Disord. 2017;11:1756285617722347. https://doi.org/10.1177/1756285617722347 ([published 16 August 2017]).
Wang H. Anti-NMDA receptor encephalitis and vaccination. Int J Mol Sci. 2017;18(1):193. https://doi.org/10.3390/ijms18010193 ([published 18 January 2017]).
Ross Russell A, Hardwick M, Jeyanantham A, et al. Spectrum, risk factors, and outcomes of neurological and psychiatric complications of COVID-19: A UK-wide cross-sectional surveillance study. SSRN [Preprint]. 24 June 2021 [cited 04 July 2021]. doi:1 0.2139/ssrn.3767901.
Siow I, Lee KS, Zhang JJY, et al. Encephalitis as a neurological complication of COVID-19: A systematic review and meta-analysis of incidence, outcomes, and predictors. Eur J Neurol. 2021;30(10):105863. https://doi.org/10.1111/ene.14913 (Published Online First 13 May 2021).
Paterson RW, Benjamin LA, Mehta PR, et al. Serum and cerebrospinal fluid biomarker profiles in acute SARS-CoV-2-associated neurological syndromes. Brain Commun 2021:fcab099 [published 12 May 2021]. doi:https://doi.org/10.1093/braincomms/fcab099.
Lu L, Xiong W, Mu J, et al. The potential neurological effect of the COVID-19 vaccines: A review. Acta Neurol Scand. 2021;2021(144):3–12. https://doi.org/10.1111/ane.13417.
Voysey M, Costa Clemens SA, Madhi SA, et al. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials. Lancet. 2021;397(10277):881–91. https://doi.org/10.1016/S0140-6736(21)00432-3.Erratum.In:Lancet2021;397(10277):880.
UK Medicines and Healthcare Regulatory Agency (MHRA) 2021 COVID-19 AstraZeneca Vaccine Analysis Print, MHRA, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/998492/COVID-19_AstraZeneca_Vaccine_Analysis_Print_DLP_23.06.2021.pdf (accessed 01 July 2021; updated 26 June 2021). 116pp.
Butler M, Tamborska A, Wood GK, et al. Defining causality in neurological & neuropsychiatric COVID-19 vaccine complications: What have we learnt from current and previous vaccination campaigns? SSRN [Preprint]. 9 April 2021 [cited 04 July 2021]. doi https://doi.org/10.2139/ssrn.3823441
Anon. Claims and counterclaims over alleged adverse reaction in covid-19 vaccine in India. BMJ. 2020;371:m4734. https://doi.org/10.1136/bmj.m4734.
Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8(5):416–27. https://doi.org/10.1016/S2215-0366(21)00084-5 ([published 6 April 2021]).
Acknowledgements
The Authors are grateful for the kind permission of the patient to publish their case. Thanks are also due to Dr. Michael K L Chou, Senior Healthcare Scientist in Neuroimmunology, Neuroimmunology & CSF Laboratory, National Hospital for Neurology & Neurosurgery, UK, for processing and reporting diagnostic samples.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
JT: Writing – Original draft preparation, Writing – Review & editing, Patient care. SMD: Writing – Original draft preparation, Writing – Review & editing, Patient care. SW: Writing – Review & editing, Patient care (Specialty consultation). MSZ: Writing – Review & editing, Patient care (Specialty consultation). JKS: Writing – Review & editing, Patient care (Specialty consultation). TWC: Conceptualisation, Writing – Review & editing, Supervision, Patient care (named Consultant). All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not required
Consent for publication
Written informed consent was obtained from the patient for publication of this Case Report and accompanying material. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The Authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Takata, J., Durkin, S.M., Wong, S. et al. A case report of ChAdOx1 nCoV-19 vaccine–associated encephalitis. BMC Neurol 21, 485 (2021). https://doi.org/10.1186/s12883-021-02517-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-021-02517-w