Abstract
Purpose
Autoimmune encephalitis is a neurological emergency of new-onset altered mental status, caused by an exaggerated immune-mediated response that targets the central nervous system. Autoimmune encephalitis has become an emerging differential diagnosis, when a classical infection cannot explain neurological symptoms. Displaying overlapping clinical presentations, ranging from the insidious onset of cognitive deficiency to more severe forms of encephalopathy with refractory seizures, autoimmune encephalitis can be challenging for clinicians. When evidence of malignancy is absent and pathogenic autoantibodies are undetected, with typical clinical and imaging features of autoimmune encephalitis, seronegative autoimmune encephalitis may be considered. Recently, vaccination-related autoimmune encephalitis and acute encephalitis after COVID-19 vaccination have attracted attention.
Methods and results
We report a case series consisting of three patients with autoimmune encephalitis occurring shortly after COVID-19 vaccination and a current review of all previous reported autoimmune encephalitis related to COVID-19 vaccines.
Conclusion
We emphasise on the prompt diagnosis of autoimmune encephalitis induced by Covid-19 vaccines and its timely treatment to improve the clinical outcome of this severe neurological condition. Post-licencing vaccine safety surveillance for potential adverse events is essential for vaccine safety and public confidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Two years after its emergence and despite being developed at an unprecedented speed, COVID-19 vaccines had demonstrated a well-established safety and efficacy in controlling the COVID-19 pandemic [1]. Common, expected, and self-limited adverse drug reactions (ADRs) have been related to COVID-19 vaccines, including site injection reactions, fever with chills, fatigue, and swollen lymph nodes [2]. However, the occurrence of serious vaccination-associated ADRs such as neurological complications has been described, including transverse myelitis, facial palsy, Guillain–Barre syndrome (GBS), ischemic stroke, and cerebral venous thrombosis [3]. Autoimmune encephalitis (AIE), accounting for 20% of all acute encephalitis, is a severe immune-mediated inflammatory disorder of the brain and one of the most common causes of noninfectious encephalitis [4]. It is characterised by a myriad of clinical manifestations, including behavioural and psychiatric symptoms, autonomic disturbances, movement disorders, and seizures [5]. Triggered mostly by tumour or infections, AIE has drawn attention as one of the potential causes of acute encephalitis that may be induced by vaccines, which includes the COVID-19 vaccine. However, the causal relationship is not yet established, and the pathophysiology of those complications is still being speculative. Herein, we describe a case series consisting of three patients with AIE that occurred following COVID-19 vaccination. All the reported cases had been notified to the national COVID-19 vaccine adverse event reporting system. A current review of all previous reported AIE related to COVID-19 vaccines aims to shed light on this potential ADR.
Case reports
Case no. 1
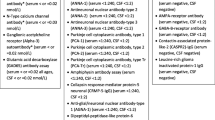
A 40-year-old female patient with a medical history of rheumatoid arthritis treated with steroid and methotrexate had received her first dose of the BNT162b2 Comirnaty®, BioNTech and Pfizer vaccine. Three days later, she complained of headache and nausea complicated by four episodes of generalised tonic–clonic seizures and disorientation, for which she was admitted to the emergency room. On physical examination, the patient had a fever (40 °C) with no signs of meningeal irritation. However, she had significant word-finding difficulties, memory disturbance, and tachycardia. Magnetic resonance imaging (MRI) brain ruled out a vascular aetiology and revealed bilateral hyperintense FLAIR and diffusion signals in the temporal lobes and limbic systems predominant in the right side suggestive of limbic encephalitis (Fig. 1). The results of biological tests were within normal limits. Cerebrospinal fluid (CSF) showed normal protein and glucose levels without pleocytosis. Given concern for infectious encephalitis, acyclovir, amikacin, and ciprofloxacin were started empirically along with levetiracetam for 21 days. Nevertheless, cognitive deficit and memory impairment deteriorated further during subsequent days, with a calculated Montreal Cognitive Assessment (MoCA) score of 12/30 (normal range 26–30): short-term memory loss, severe dysexecutive syndrome, transcortical sensory aphasia, constructional apraxia, dysarthria, and reduced voluntary movement were observed. No sensory or cranial nerve affection was objected. Contemporarily, the patient developed signs of dysautonomia: hypersalivation with weak spontaneous breathing and decreased oxygen saturation at 74%, increased blood pressure at 180–100, and loss of consciousness (Glasgow Coma Scale (GCS) score of 7/15). She was transferred to the intensive care unit, where she was intubated and mechanically ventilated. A second MRI scan revealed extended hyperintensities to occipital and frontal lobes (Fig. 2). Extensive workup for encephalitis excluded other competing diagnoses, such as infective encephalitis, systemic, neoplastic, metabolic, or vascular causes (Table 1 summarises the laboratory workup). As differential diagnoses were ruled out, the patient met clinical diagnostic criteria for autoimmune encephalitis. Intravenous immunoglobulin 0.4 g/kg/day was started with drastic clinical improvement on day 2. She was discharged from the hospital 1 month later on oral levetiracetam and prednisone. At follow-up, she was fully oriented, but neuropsychological assessments revealed short-term memory and language impairment. Her MoCA score improved, reaching 21/30 with 2 weeks of ongoing corticotherapy treatment. Another MRI scan, performed 4 months later, showed a clear improvement of cerebral FLAIR hyperintensities, but with the appearance of atrophy next to lesions (Fig. 3).
Case no. 2
A 35-year-old female with a history of hypothyroidism, palpitations, and eczema had been vaccinated against COVID-19 with mRNA-1273 Spikevax® vaccine (first dose). Twenty days later, she started to show behavioural changes with gradual onset of confusion, prosopagnosia, apraxia, unsteady shuffling gait, and slurred with nonfluent speech. She presented to the emergency room, the following day, with status epilepticus refractory to levetiracetam and valproic acid. MRI brain showed diffuse brain oedema with a hyperintense signal (FLAIR and diffusion) in the splenium, with no contrast enhancement after gadolinium injection (Fig. 4). The CSF was colourless, but revealed lymphocytic pleocytosis of 50 leukocytes/μL. Medical treatment, including intravenous lorazepam, levetiracetam, and phenobarbital, was started to control seizures. Anti-infective medication with acyclovir, cefotaxime, and vancomycin was initiated to treat possible infectious meningoencephalitis. Despite the 12-day ongoing treatment, the patient remained drowsy, with a GCS score of 9/14. In view of her young age, persistent seizures, MRI features, and exclusion of other diagnoses (Table 1), autoimmune encephalitis was highly considered. Intravenous immunoglobulins 0.4 g/kg/day were initiated followed by another 5-day cycle of high-dose methylprednisolone 1 g/day leading to an immediate and significant improvement of the symptomatology. The patient regained consciousness on the following day and progressively showed slight improvements in speech and motor function. Her MoCA score improved from 14/30 to 25/30, 2 weeks later, reflecting a marked improvement in her clinical presentation. At discharge, there was still mild cognitive slowing without functional impairment. At the follow-up 2 months later, the patient had sequelae of memory impairment and was maintained on levetiracetam and oral prednisone. Notably, repeated MRI revealed the resolution of the previous abnormalities (Fig. 5).
Case no. 3
A 63-year-old cognitively normal female developed, 2 weeks after receiving the third dose of BNT162b2 Comirnaty®, BioNTech and Pfizer, progressive mental alteration with anterograde amnesia, loss of attention and concentration, murmuring, and unsteadiness. Two days later, she presented to the emergency department, as she experienced periods of unresponsiveness and sudden loss of consciousness. Upon presentation, the patient was afebrile and had status epilepticus, with normal systolic and diastolic blood pressure values of 120 mmHg/70 mmHg, respectively. She did not complain about headaches or visual disturbances. Her past medical history included well-controlled hypertension, gout, and coronary heart disease. MRI was notable for subcortical and cortical oedema, with a predominance of hyperintensity on T2-weighted/FLAIR in parietal and occipital lobes (Fig. 6). Laboratory investigations were unremarkable except for an inflammatory syndrome (CRP 61 mg/L) with a normal white blood cell count and absence of renal impairment. CSF analysis revealed significant pleocytosis and elevated protein levels. Her status epilepticus resolved when treated with intravenous levetiracetam and valproic acid. She had received a 7-day course of ceftriaxone, vancomycin, and acyclovir for presumed meningoencephalitis, but her disorientation and aggressiveness worsened. As the extensive diagnostic workup remained negative, antimicrobial therapy was discontinued, and AIE was considered. Intravenous methylprednisolone (1 g/day) was then administered, and the patient started to respond with considerable improvement. She became able to understand and answer questions, and her neurological deficits gradually resolved thereafter (with an improvement of her MoCA score from 15/30 to 25/30, 2 weeks later). After 2 months of hospitalisation, amnesia persisted as the only residual neurological deficit observed.
Discussion
We report a case series of three clinical pictures consistent with the diagnosis of AIE triggered by COVID-19 vaccines. In all three cases, criteria for possible AIE defined by Graus et al. were fulfilled [6] including (i) subacute onset of brainstem and cerebellar signs, (ii) new focal CNS findings or CSF pleocytosis or neuroimaging findings or seizures not explained by a previously known seizure disorder, and (iii) exclusion of alternative causes. Consequently, the diagnosis of AIE was established in our cases, and immunosuppressive therapy was initiated with remarkable improvement. In view of the suggestive temporal relationship between vaccination and symptom onset and the exclusion of differential diagnoses including infective and non-infective causes, COVID-19-induced AIE was “probable” with a score of 6, according to the Naranjo probability scale [7]. Owing to the lack of any identifiable direct causative biomarkers or antibodies, we cannot be decisively conclusive.
Various neurologic complications may occur following vaccination, with SARS-CoV-2 being no exception. Mild, ambulatory, manageable, and transient neurological ADRs involving, dizziness, headache, myalgia, muscle spasms, and paraesthesia are the most widely mentioned [3]. Nevertheless, severe neurological complications, including vaccine-induced thrombotic thrombocytopenia with cerebral venous thrombosis, GBS, optic neuritis, polymyositis, myasthenia, and transverse myelitis, have been reported [8], many of which are of autoimmune nature [9]. A wide variety of autoimmune neurological syndromes have been reported following different types of viral vaccination: GBS and giant cell arteritis following influenza vaccine, CNS demyelination following HPV, hepatitis A or B, rabies, and measles vaccination [10]. AIE is a non-infectious immune-mediated disease of the central nervous system that implicates a widely variable spectrum of clinical presentations, ranging from the relatively mild or insidious onset of cognitive impairment to more complex forms of encephalopathy with refractory seizures. Might be triggered by vaccination, AIE has been described previously with H1N1 influenza or poliomyelitis vaccines [11]. COVID-19 vaccines, as well, have recently been linked to AIE as increasing cases are emerging, despite the unproven direct causality. To our knowledge, 32 cases of AIE induced by COVID-19 vaccines have been reported in the literature (Table 2 summarises all previous case reports/series of AIE related to COVID-19 vaccines).
In our cases, the diagnosis of a seronegative AIE was established, based on the exclusion of pathogen-induced encephalitis, the dramatic improvement after receiving methylprednisolone, supporting an immune-mediated mechanism. In view of the lack of antibody detection, the diagnosis of a seronegative AIE was retained. Our results are in line with the majority of AIE cases reported in the literature, in which antibody panels were negative (Table 1). Only two cases reported by Zlotnick et al. and Flanney et al. described AIE with respectively positive pathological antibody anti-LGI1 and anti-NMDAR induced by BNT162b2 vaccine [12, 13]. Autoimmune encephalitis is reported to occur within the first week following COVID-19 vaccination (26 /32 cases), which are the case of patients 1 and 3, with an onset time of 3 and 2 days, respectively. However, a long frame time of 20 days between vaccination and AIE was observed in patient 2. This similar long-onset (21 days) of AIE has been outlined in two cases reported by Takata et al. and Grosi et al. indicating that AIE may exhibit a variable incubation period [14, 15]. All of our cases were related to mRNA-based vaccines (Comirnaty®: 2, Spikevax®: 1), which is in accordance with the majority of AIE reported in the literature (19/32: Spikevax® (13/32), Comirnaty® (6/32)), followed by viral vector vaccines (11/32). Only two cases were related to an inactivated COVID-19 vaccine [16, 17]. Like other reported cases of immune-mediated encephalitis, all three patients responded well to immunosuppressive therapy. In fact, appropriate, early, and intense treatment is important to achieve a good outcome in AIE [16]. Corticosteroids are frequently the first choice to manage AIE, followed by intravenous immunoglobulin and plasmapheresis [5]. Nevertheless, some sporadic cases reported the use of rituximab as a second-line immunotherapy in order to treat AIE induced by COVID-19 vaccine [13, 18, 19]. Fortunately, our patients responded well to methylprednisolone alone or combined to intravenous immunoglobulin. It was considered that AIE after COVID-19 vaccination have good prognosis when diagnosed and treated timely and properly as most described cases had a favourable outcome (Table 1). Nevertheless, fatality can complicate the course of AIE: two cases were described in the literature by Kheder et al. following ChAdOx1 nCov-19 vaccination, in which, despite an aggressive immunosuppressive therapy including rituximab/tocilizumab and methylprednisolone, clinical features of patients deteriorated leading to death [20]. In view of the potential severity and as long as the pathological mechanism of COVID-19 vaccine–induced autoimmune disease disturbance remained unclear, COVID-19 vaccines had to be definitively contraindicated in our cases.
Indeed, several pathogenic mechanisms have been postulated to ascertain how COVID-19 vaccines can lead to AIE. Molecular mimicry is believed to be one of the main immunopathogenic factors. In fact, antibodies against spike proteins produced by vaccines can trigger an undesired immune response. Neuro-inflammation process caused by COVID-19 vaccines is claimed to be also the consequence of exaggerated immune response to mRNA vaccines with a strong expression of pro-inflammatory cytokines and a T cell response reaching the brain known as cytokine storm–associated encephalopathy [21,22,23]. Another plausible explanation is that vaccine adjuvants are implied in post-vaccination autoimmune reaction, mainly BNT162 adjuvant polyethylene glycol (PEG), as it has been considered to be a trigger of autoimmune syndrome induced by adjuvants (ASIA-syndrome) [24].
Here, we report three cases of encephalitis fulfilling the criteria of possible autoimmune AIE and believed to be related to COVID-19 vaccines. Despite its rare occurrence, AIE following COVID-19 vaccination should be considered with timely treatment, and a favourable prognosis can be obtained. Post-licencing vaccine safety surveillance for potential adverse events is essential for vaccine safety and public confidence. Thus, further large pooled observational epidemiologic data are required before attributing definite causality.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Chi WY, Li YD, Huang HC, Chan TEH, Chow SY, Su JH et al (2022) COVID-19 vaccine update: vaccine effectiveness, SARS-CoV-2 variants, boosters, adverse effects, and immune correlates of protection. J Biomed Sci 29(1):82
Hernández AF, Calina D, Poulas K, Docea AO, Tsatsakis AM (2021) Safety of COVID-19 vaccines administered in the EU: should we be concerned? Toxicol Rep 1(8):871–879
Goss AL, Samudralwar RD, Das RR, Nath A (2021) ANA investigates: neurological complications of COVID-19 vaccines. Ann Neurol 89(5):856–857
Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D et al (2010) Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 10(12):835–844
Dutra LA, Abrantes F, Toso FF, Pedroso JL, Barsottini OGP, Hoftberger R (2018) Autoimmune encephalitis: a review of diagnosis and treatment. Arq Neuro-Psiquiatr 76:41–49
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15(4):391–404
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA et al (1981) A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 30(2):239–245
Kaulen LD, Doubrovinskaia S, Mooshage C, Jordan B, Purrucker J, Haubner C et al (2022) Neurological autoimmune diseases following vaccinations against SARS-CoV-2: a case series. Eur J Neurol 29(2):555–563
Chen Y, Xu Z, Wang P, Li XM, Shuai ZW, Ye DQ et al (2022) New-onset autoimmune phenomena post-COVID-19 vaccination. Immunology 165(4):386–401
Ismail II, Salama S (2022) A systematic review of cases of CNS demyelination following COVID-19 vaccination. J Neuroimmunol 15(362):577765
Wang H (2017) Anti-NMDA receptor encephalitis and vaccination. Int J Mol Sci 18(1):193
Zlotnik Y, Gadoth A, Abu-Salameh I, Horev A, Novoa R, Ifergane G (2022) Case report: anti-LGI1 encephalitis following COVID-19 vaccination. Front Immunol 12. [cited 2022 Aug 10]. Available from: https://doi.org/10.3389/fimmu.2021.813487
Flannery P, Yang I, Keyvani M, Sakoulas G (2021) Acute psychosis due to anti-N-methyl D-aspartate receptor encephalitis following COVID-19 vaccination: a case report. Front Neurol 4(12):764197
Takata J, Durkin SM, Wong S, Zandi MS, Swanton JK, Corrah TW (2021) A case report of ChAdOx1 nCoV-19 vaccine–associated encephalitis. BMC Neurol 21(1):485
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK et al (2021) Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 397(10269):99–111
Abu-Riash A, Tareef AB, Aldwairy A (2021) Could Sinopharm COVID-19 vaccine cause autoimmune encephalitis? A case report. [cited 2022 Aug 11]. Available from: https://www.medicalandresearch.com/journals/view_article/893
Vences MA, Araujo-Chumacero MM, Cardenas E, Canales D, Alvarez A, Barja E et al (2022) Autoimmune encephalitis after BBIBP-CorV (Sinopharm) COVID-19 vaccination: a case report. BMC Neurol 22(1):427
Shin HR, Kim B kyun, Lee ST, Kim A (2022) Autoimmune encephalitis as an adverse event of COVID-19 vaccination. J Clin Neurol 18(1):114–6
Kwon H, Kim T (2022) Autoimmune encephalitis following ChAdOx1-S SARS-CoV-2 vaccination. Neurol Sci 43(3):1487–1489
Khedr D (2022) Post COVID-19 vaccine encephalitis and romboencephalitis: three cases report. OAJNN 16(5):01–05
Baldelli L, Amore G, Montini A, Panzera I, Rossi S, Cortelli P et al (2021) Hyperacute reversible encephalopathy related to cytokine storm following COVID-19 vaccine. J Neuroimmunol 15(358):577661
Sriwastava S, Sharma K, Khalid SH, Bhansali S, Shrestha AK, Elkhooly M et al (2022) COVID-19 vaccination and neurological manifestations: a review of case reports and case series. Brain Sci 12(3):407
Huang YF, Ho TC, Chang CC, Shen DHY, Chan HP, Chuang KP et al (2022) A rare adverse effect of the COVID-19 vaccine on autoimmune encephalitis. Vaccines (Basel) 10(7):1114
Vera-Lastra O, Ordinola Navarro A, Cruz Domiguez MP, Medina G, Sánchez Valadez TI, Jara LJ (2021) Two cases of Graves’ disease following SARS-CoV-2 vaccination: an autoimmune/inflammatory syndrome induced by adjuvants. Thyroid 31(9):1436–1439
Zuhorn F, Graf T, Klingebiel R, Schäbitz W, Rogalewski A (2021) Postvaccinal encephalitis after ChAdOx1 nCov-19. Ann Neurol 90(3):506–511
Kobayashi Y, Karasawa S, Ohashi N, Yamamoto K (2022) A case of encephalitis following COVID-19 vaccine. J Infect Chemother 28(7):975–977
Sluyts Y, Arnst Y, Vanhemelryck T, De Cauwer H (2022) COVID-19-booster vaccine-induced encephalitis. Acta Neurol Belg 122(2):579–581
Vences MA, Canales D, Albujar MF, Barja E, Araujo-Chumacero MM, Cardenas E et al (2022) Post-vaccinal encephalitis with early relapse after BNT162b2 (COMIRNATY) COVID-19 vaccine: a case report. Vaccines 10(7):1065
Solís Tarazona LR, Sanchis Llopis CM, Galiano Blancart RF, Ferrer Casanova JM and Landete Pascual L (2021) PostSARS-CoV-2-Vaccine Autoimmune Encephalitis: A Case Report. SVOA Neurology 2(5):155–157
Rosso M, Anziska Y, Levine SR (2022) Acute transient encephalopathy after Moderna COVID-19 vaccine. CRN 14:231–236
McCullough J, Ahmad M, Tam I, et al. (May 11, 2022) Posterior Reversible Encephalopathy Syndrome Onset Within 24 Hours Following Moderna mRNA Booster COVID-19 Vaccination: Vaccine Adverse Event Vs. Hypertension?. Cureus 14(5):e24919
Fan HT, Lin YY, Chiang WF, Lin CY, Chen MH, Wu KA et al (2022) COVID-19 vaccine-induced encephalitis and status epilepticus. QJM 115(2):91–3
Grosi E, Tsolaki A, Saoulidis I, Liouta E, Savopoulos C, Bakaimi I, et al. (2022) Encephalitis on an Immunocompromised Patient Following COVID-19 Vaccination Causal or Coincidental Correlation. J Vaccines Vaccin S18:001
Asaduzzaman M, Purkayastha B, Alam MMJ, Chakraborty SR, Roy S, Ahmed N (2022) COVID-19 mRNA vaccine-associated encephalopathy, myocarditis, and thrombocytopenia with excellent response to methylprednisolone: a case report. J Neuroimmunol 15(368):577883
Liu BD, Ugolini C, Jha P. Two cases of post-Moderna COVID-19 vaccine encephalopathy associated with nonconvulsive status epilepticus. Cureus 13(7):e16172
Al-Mashdali AF, Ata YM, Sadik N (2021) Post-COVID-19 vaccine acute hyperactive encephalopathy with dramatic response to methylprednisolone: a case report. Ann Med Surg (Lond) 6(69):102803
Torrealba-Acosta G, Martin JC, Huttenbach Y, Garcia CR, Sohail MR, Agarwal SK et al (2021) Acute encephalitis, myoclonus and Sweet syndrome after mRNA-1273 vaccine. BMJ Case Rep 14(7):e243173
Shyu S, Fan HT, Shang ST, Chan JS, Chiang WF, Chiu CC et al (2022) Clinical manifestation, management, and outcomes in patients with COVID-19 vaccine-induced acute encephalitis: two case reports and a literature review. Vaccines 10(8):1230
Li SY, Chen HH, Liu PY, Shi ZY, Lin YH, Tsai CA et al. Case report of acute encephalitis following the AstraZeneca COVID-19 vaccine. Int J Rheumat Dis n/a(n/a). [cited 2022 Aug 11]. Available from: https://doi.org/10.1111/1756-185X.14372
Cepero GS, Freiberg MB, Mucha S (2022) 196: Encephalopathy after COVID-19 INFECTION and vaccine in a patient with underlying autoimmune disease. Crit Care Med 50(1):82
Abu-Abaa M, Dawood G, Arshad H, Jumaah O, Landau D (2022) A possible case of autoimmune encephalitis after mRNA COVID-19 booster vaccine: a case report. Cureus 14(11). [cited 2022 Dec 21]. Available from: https://www.cureus.com/articles/120580-a-possible-case-of-autoimmune-encephalitis-after-mrna-covid-19-booster-vaccine-a-case-report
Albsheer K, Fadul A, Abdalla Elm, Mohamed G, Elawad M, Zafar A (2022) Post-COVID-19 vaccine limbic encephalitis: a case report. Cureus 14(9). [cited 2022 Dec 21]. Available from: https://www.cureus.com/articles/106375-post-covid-19-vaccine-limbic-encephalitis-a-case-report
Author information
Authors and Affiliations
Contributions
Khadija Mansour and Zohra Chadli wrote the manuscript. Samia Younes and Ichrak Ghachem made the diagnosis, patient supervision, and patient follow-up. Haifa Ben Romdhane, Najah Ben Fadhel, and Nadia Ben Fredj performed the drug probability scale. Aouam Karim, Amel Chaabane, and Naceurs Boughatas performed a literature search. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from described patients to publish their clinical details.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mansour, K., Chadli, Z., Ghachem, I. et al. Seronegative acute encephalitis following COVID-19 vaccines: a case series of an overlooked diagnosis with literature review. Eur J Clin Pharmacol 79, 975–987 (2023). https://doi.org/10.1007/s00228-023-03510-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03510-7