Abstract
Background
Medical image analysis has evolved to facilitate the development of methods for high-throughput extraction of quantitative features that can potentially contribute to the diagnostic and treatment paradigm of cancer. There is a need for further improvement in the accuracy of predictive markers of response to neo-adjuvant chemotherapy (NAC). The aim of this study was to develop a radiomic classifier to enhance current approaches to predicting the response to NAC breast cancer.
Methods
Data on patients treated for breast cancer with NAC prior to surgery who had a pre-NAC dynamic contrast enhanced breast MRI were included. Response to NAC was assessed using the Miller–Payne system on the excised tumor. Tumor segmentation was carried out manually under the supervision of a consultant breast radiologist. Features were selected using least absolute shrinkage selection operator regression. A support vector machine learning model was used to classify response to NAC.
Results
74 patients were included. Patients were classified as having a poor response to NAC (reduction in cellularity < 90%, n = 44) and an excellent response (> 90% reduction in cellularity, n = 30). 4 radiomics features (discretized kurtosis, NGDLM contrast, GLZLM_SZE and GLZLM_ZP) were identified as pertinent predictors of response to NAC. A SVM model using these features stratified patients into poor and excellent response groups producing an AUC of 0.75. Addition of estrogen receptor status improved the accuracy of the model with an AUC of 0.811.
Conclusion
This study identified a radiomic classifier incorporating 4 radiomics features to augment subtype based classification of response to NAC in breast cancer.
Similar content being viewed by others
Background
Neoadjuvant chemotherapy (NAC), administered prior to tumor resection, plays an established role in the contemporary management of early stage breast cancer. NAC can enable less extensive surgery to be performed and provides valuable prognostic information [1]. NAC generates in-vivo data on tumor chemosensitivity, and response to NAC which is typically assessed by magnetic resonance imaging (MRI) can further inform clinicians of the biological characteristics of the tumor and the patient’s prognosis [2, 3]. Response to NAC is assessed primarily by post-treatment pathology and can be stratified using histologic grading systems such as the Miller–Payne system [4] which classifies response based on the reduction in tumor cellularity. Complete pathological response (pCR) is defined as having no residual carcinoma in the breast tissue following surgery and is associated with an improved prognosis [5].
The pCR rate in breast cancer following NAC ranges from 10 to 50% and is related to patient factors, tumor subtype and NAC regime received [6]. pCR rate is highest among patients with HER2 positive and triple-negative breast cancer (TNBC), while Luminal A breast cancer has the lowest rate of pCR to systemic chemotherapy [7,8,9]. There is a need for robust and reliable biomarkers to predict response to NAC in order to optimally tailor treatment to individual patients. This could potentially spare a subset of patients, who are unlikely to derive significant benefit from NAC, from the deleterious effects of chemotherapy [10]. Biomarkers in clinical use that improve risk stratification and prediction of response to NAC in breast cancer beyond conventional clinico-pathological factors include Oncotype DX, Mammaprint and ProSigna [11]. These gene-profiling tests require tumor tissue for analysis and while they have utility in recurrence prediction, they were not designed specifically to predict response to NAC. There is a currently unmet clinical need for non-invasive methods to predict response to NAC to further personalize breast cancer management.
Radiomics is a developing field that involves the application of computer-automated software to extract high-throughput quantitative features from radiologic/imaging investigations that can quantify disease phenotype and heterogeneity [12, 13]. Radiomics features include conventional quantitative measurements such as shape/ diameter and surface area. First order features examine the distribution of voxels in isolation and include kurtosis and skewness. Second order features are derived from the spatial relationship between voxels and matrices such as the grey-level co-occurrence matrix (GLCM) [14, 15]. Prediction models using radiomics features incorporating machine learning have shown potential for non-invasive identification of treatment response in breast and other cancers [16,17,18,19,20]. The aim of our study was to develop a radiomics model to predict the response to NAC in breast cancer using pre-NAC breast MRI.
Methods
Clinical database
This study was undertaken at Galway University Hospital, a tertiary referral specialist breast cancer unit. This study was conducted in accordance with the granted University College Hospital Galway ethical approval.
Patients who were treated with chemotherapy for breast cancer were identified from a prospectively maintained institutional database including patient demographics, tumor clinicopathology, and surgical and medical therapeutic information. Patients were categorized as receiving NAC or adjuvant chemotherapy based on whether they had treatment before or after their curative surgery. Clinical decisions relating to surgical intervention and neoadjuvant/adjuvant local and systemic therapy are made by discussion and consensus at a multidisciplinary team meeting with medical, surgical, and radiation oncologists present. Residual tumor size and response to NAC were assessed using postoperative pathology of the resected breast specimen by a consultant histopathologist at GUH.
The Miller–Payne grading system is as follows: Grade 1: residual tumor demonstrates no change or some minor alteration in individual malignant cells, but no reduction in overall cellularity. Grade 2: minor loss of tumor cells but overall high cellularity with up to 30% reduction of cellularity. Grade 3: estimated 30% and 90% reduction in tumor cellularity. Grade 4: marked disappearance of more than 90% of tumor cells such that only small clusters or widely dispersed individual cells remain (near pCR). Grade 5: no invasive malignant cells identifiable in sections from the site of the tumor (complete pCR).
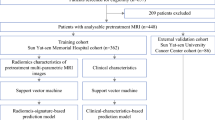
Patients with multifocal breast cancer, inflammatory disease and metastatic disease at presentation were excluded from this study (Fig. 1).
MRI protocol
Magnetic resonance imaging analyses were performed on a short bore 1.5 T magnet (Magnetom Espree 1.5 T, Siemens Healthcare, Erlangen, Germany) using 8-channel breast phase array breast coil for signal reception using the dynamic contrast enhanced (DCE) breast MRI protocol, utilising the following protocol: Sagittal T2 (TR/TE 6570/111, Gap 1 mm, Flip angle 160°, Matrix 340 × 75), Axial T2 FS fl3d pre contrast (TR/TE 5.15/2.39, Gap 0.6 mm, Flip angle 10°, Matrix 320 × 100), Sagittal T1 fl3d (TR/TE 5.18/1.64, Gap 0.6 mm, Flip angle 10°, Matrix 320 × 100, this sequence is repeated 6 times; 1 pre-contrast and 5 post-contrast with peak enhancement in the third run), Axial T1 FS fl3d postcontrast. The section thickness was 3 mm for all sequences. The contrast employed was Gadoterate meglumine (Gd-DOTA). Digitally recreated subtraction image 3-1 postcontrast enhanced was used for final feature analysis.
Tumor segmentation and radiomic feature analysis
MR images were evaluated by one researcher (PM) under the supervision of a Consultant specialist breast radiologist (SW). Tumor segmentation was performed by manually delineating the tumor border on axial slices using ITKSnap software (Fig. 2) [21]. Feature extraction was carried out on LIFEx [22], an International Biomarker Standardization Initiative (IBSI)-compliant [23] and validated [24, 25] software package.
An image intensity discretization applying a fixed bin width of 64 was used for feature extraction in MR. Voxel size resampling was performed before feature extraction using cubic interpolation. Images were resampled to isotropic voxels of size 2 × 2 × 2 mm3 by 3-dimensional Lagrangian interpolation.
61 features were extracted from each tumor including size and shape features and from several matrices including Histogram-based matrix (HISTO), Grey-level co-occurrence matrix (GLCM), Grey-level run length matrix (GLRLM), Grey-level zone length matrix (GLZLM) and Neighborhood grey-level dependence matrix (NGLDM).
Radiomic feature selection and machine learning model
To counteract the high throughput nature of data driven radiomics and the high relative correlation between the features produced it is important to first reduce the number of features prior to model training to prevent over-fitting, reduce collinearity and minimize noise [26, 27]. A combination of least absolute shrinkage selection operator (LASSO) regression for feature selection and support vector machine learning (SVM) for model building provide excellent model performance in radiomics and was utilised for this study [28]. LASSO introduces a tuning parameter (λ) that penalizes large coefficients of variables entered into the regression model, reduces the possibility of overfitting [29] and reducing non-pertinent features to zero. In this study, λ was set at 1 and the convergence threshold was 0.0000001. The selected features were used to construct the SVM model with a linear kernel with standardisation pre-processing and a tolerance threshold of 0.001. Receiver operator curve (ROC) was built for the model and area under the curve (AUC) was used to classify model performance.
Statistical analysis
Data analysis was carried out using IBM SPSS statistics 26.0 and R 4.0.3 with extension XLSTAT v2020.5. A p-value of < 0.05 was assumed to represent statistical significance. Continuous variables were summarised using descriptive statistics, including mean, standard deviation, and median. Sensitivity as well as accuracy values were expressed as percentages. Adjustment for confounders was undertaken using multivariable linear or logistic regression for continuous or binary-dependent variables, respectively. The R package “glmnet” was used for LASSO regression and the machine learning module was used to produce the SVM model.
Results
Clinicopathological details and response to NAC
Following exclusion of patients with bilateral/ multifocal disease, inflammatory breast cancer and metastatic disease at presentation, 74 patients were included in this study. The majority of patients had invasive ductal carcinoma (n = 56), T2/T3 tumors and luminal A biologic subtype (n = 40) (Table 1).
Response to NAC was assessed using the Miller–Payne response classification based on reduction in tumor cellularity. Response was further stratified into poor (< 90%, n = 44) and excellent (> 90%, n = 30) response to NAC (Table 2).
Response to NAC differed significantly between subtypes, with triple negative and HER2 disease achieving the highest rates of pCR (Table 3). Patients with luminal A breast cancer (n = 39) were significantly less likely to achieve a pCR compared to non-luminal A patients (n = 35) (5% vs. 37%, p < 0.001) and less likely to have an “excellent” response to NAC (> 90% reduction in cellularity), (23% vs. 60%, p < 0.001).
Feature selection
61 radiomic features were extracted from each tumor. Following LASSO regression, 4 features were selected; (1) Discretized kurtosis, (2) neighbourhood grey-level different matrix (NGLDM) contrast, (3) grey-level zone length matrix short zone grey level emphasis (GLZLM_SZE) and (4) GLZLM zone percentage (ZP) (Figs. 3 and 4).
Radiomic model
A predictive model was constructed using a SVM approach with the 4 above selected features to differentiate patients with a poor response to NAC (n = 44) from those with an excellent response to NAC (n = 30) (Table 4). This radiomic model demonstrated good predictive performance with an AUC of 0.753 (Fig. 5).
Radiomic model with estrogen receptor status
Estrogen receptor status was added to the radiomics model, improving the AUC to 0.81. This improved model correctly identified 91% of poor responders and 70% of excellent responders (Table 5, Fig. 6).
Discussion
NAC is a central element of contemporary breast cancer management, however there is a wide spectrum of response to NAC between patients which can vary based on host, tumor and treatment factors. Patients with locally advanced breast cancer and selected patients with early stage breast cancer are offered NAC with the aim of down-staging the tumor size or gaining valuable information relating to in-vivo tumor response. [30]. Appropriate patient selection for NAC is vital and can be informed by gene expression biomarkers and indexes of proliferation such as ki67. Recent evidence suggests that radiomic features from pre-NAC MRI imaging can be utilised to non-invasively predict response to NAC [31,32,33,34,35] and potentially contribute to the existing patient-selection paradigm.
This study has identified 4 radiomic features from pre-NAC MRI to stratify a cohort of 74 patients with invasive breast cancer into poor and excellent response groups. A machine learning approach was utilised to select these pertinent features and to build a model to predict response to NAC. The addition of estrogen receptor status improved the overall performance of the model, with an AUC of 0.811, identifying poor responders with 90% sensitivity and 70% specificity.
Conventional molecular subtypes help inform likelihood of response to NAC. A study of 838 patients demonstrated significantly different rates of pCR between Luminal A, Luminal B, HER2 over-expressing and Triple-Negative subtypes (6%, 16%, 37% and 38% respectively) [36]. The results of this study compare favourably to similar studies investigating the role of biomarkers in predicting response to NAC. Oncotype DX has been validated in adjuvant therapy, however its’ role in NAC is less clear; a 2019 study of 989 breast cancer patients found that a high Oncotype recurrence score (> 30) was significantly associated with pCR (Odds ratio 4.87) [37]. OncoMasTR is another multi-gene prognostic signature in development specifically to predict NAC response and incorporates 3 master transcription regulator genes as well as tumor size and nodal status [38]. A 2020 study of 813 breast cancer patients showed that OncoMasTR score was significantly associated with pCR (OR 1.68) [39].
Recent evidence supports the addition of radiomic features as potential predictors of NAC response, including in breast cancer [40]. A 2019 study investigating histopathological residual cancer burden in 38 breast cancer patients utilised 23 pharmacokinetic features obtained from DCE-MRI in addition to conventional pathological factors to classify response to NAC with an AUC of 0.92 [34]. A 2020 study of 222 breast cancers utilised a model composed of 12 MRI-derived radiomics features in addition to molecular subtype to identify pCR, producing an AUC of 0.8 using a random forest machine learning approach [31]. In cervical cancer, a 2019 study of 275 patients demonstrated an AUC of 0.999 in predicting response to NAC [41, 42].
The radiomic features identified and tested may further describe the intrinsic tumor environment and the degree of intra-tumor heterogeneity which may impact NAC response. Kurtosis can be used as a measure to assess deviation from the normal distribution of pixel values. Invasiveness may be explained by the degree of pixel-kurtosis in breast cancer [43] and has been shown to be associated with response to chemotherapy in pancreatic cancer [44]. Texture based features evaluating the relationship between pixels are produced by using spatial grey-level dependant matrices. NGLDM (neighbourhood grey-level different matrix) describes the difference in grey-levels between 1 voxel and it’s 26 neighbours in 3 dimensions. NGLDM contrast corresponds to intensity difference between neighbouring regions, and this is the first report of this radiomic feature in association with cancer prognosis or response to chemotherapy.
Grey-level zone length matrix (GLZLM) provide information on the size of homogenous zones for each grey level in 3 dimensions. GLZLM_SZE (short zone emphasis) is a measure of the distribution of the short homogenous zones in an image, while GLZLM_ZP (zone percentage) measures the homogeneity of the homogenous zones. Indices derived from the GLZLM, in addition with kurtosis, were significantly associated with overall survival in a study investigating radiomics features in gastric B-cell lymphoma [44]. A 2020 study that assessed PET scan radiomic features of patients with pancreatic cancer demonstrated that GLZLM non-uniformity was significantly associated with one-year survival and could stratify patients into survival categories [45].
Radiomic features alone show great promise in the stratifying response to NAC, and models incorporating a combination of radiomics and molecular feature are superior [46, 47]. It is conceivable that radiomic features could be a component of future multi-omic panels including genomic and metabolomic markers to aid in the management of breast cancer [48, 49]. We added ER status to moderately improve the overall accuracy of the model to predict response to NAC and produce a greater accuracy in classifying patients into poor and excellent response groups than conventional molecular subtype alone. However, response to NAC can vary significantly even within subtype and is thought to be as result of intra-tumor heterogeneity [50]. Genomic heterogeneity has been shown to impact treatment response and drive resistance to targeted therapies in cancer [51, 52]. Image-based assessment of tumor heterogeneity, incorporating quantitative descriptors of grey-level relationships mentioned above, could potentially reveal aggressive tumor sub-regions for determining prognosis and treatment [53, 54] and be incorporated into the multi-modal decision process of selecting patients for NAC.
This study has a number of limitations. Firstly, it is a single centre retrospective study. While we were able to establish a discrete number of radiomic features to predict response to NAC, a larger sample size is needed to validate the radiomic model. Because radiomics is itself a developing field, there is a paucity of large cohort, prospective studies assessing the clinical utility of radiomic models. Establishing a robust, reproducible radiomics pipeline as is demonstrated in this study, is vital to integrate radiomic biomarkers into clinical practice in the near future [55].
In our study, tumor segmentation was carried out manually by a single researcher, under the supervision of a Consultant Radiologist. Manual segmentation is at present the most reliable method of establishing a region of interest (ROI) for analysis by radiomics software [15]. However, this method can be subject to inter-observer variability. Automatic segmentation by artificial intelligence shows great promise in solving this issue however is some way from being optimised [56].
Pre-processing of images by resampling has been shown to reduce more repeatable and less sensitive to change results [57, 58]. Here, we used a fixed bin width of 64 and carried out voxel resampling to isotropic voxels of size 2 × 2 × 2 mm3 by 3-dimensional Lagrangian interpolation, as described in previous studies assessing breast MRI [59, 60]. Fuzzy pre-processing may enable standardised image pre-processing particularly for non-technical experts prior to performing radiomic analysis [61]. Optimal and standardized pre-processing must be established to ensure reproducibility across radiomics studies [62].
In terms of feature extraction software, LIFEx was utilised that produces radiomics features compliant with the International Biomarker Standardization Initiative (IBSI) [63]. This 2020 initiative describes 169 standardized radiomics features that are reproducible across a number of software platforms and can potentially be investigated as clinical biomarkers. As radiomics evolves in the coming years it is likely that the number of software programmes available will increase and it is imperative that rigorous assessment of features continues to ensure reproducibility and reliability of studies.
In conclusion, this study identifies radiomic features that could potentially contribute to the management of patients receiving NAC for breast cancer.
Availability of data and materials
All data is available from the corresponding author on request.
Abbreviations
- DCE:
-
Dynamic contrast-enhanced
- GLCM:
-
Grey-level co-occurrence matrix
- GLZLM:
-
Grey-level zone length matrix
- GLZLM_SZE:
-
Grey-level zone length matrix short zone emphasis
- GLZLM_ZP:
-
Grey-level zone length matrix zone percentage
- GUH:
-
Galway University Hospital
- LASSO:
-
Least absolute shrinkage and selection operator
- MRI:
-
Magnetic resonance imaging
- NAC:
-
Neo-adjuvant chemotherapy
- NGLDM:
-
Neighbourhood grey-level different matrix
- pCR:
-
Complete pathological response
- ROC:
-
Receiver operating characteristic
- SVM:
-
Support vector machine
References
Symmans WF, Wei C, Gould R, Yu X, Zhang Y, Liu M, et al. Long-term prognostic risk after neoadjuvant chemotherapy associated with residual cancer burden and breast cancer subtype. J Clin Oncol. 2017;35(10):1049–60.
Gentile LF, Plitas G, Zabor EC, Stempel M, Morrow M, Barrio AV. Tumor biology predicts pathologic complete response to neoadjuvant chemotherapy in patients presenting with locally advanced breast cancer. Ann Surg Oncol. 2017;24(13):3896–902.
Ballesio L, Gigli S, Di Pastena F, Giraldi G, Manganaro L, Anastasi E, et al. Magnetic resonance imaging tumor regression shrinkage patterns after neoadjuvant chemotherapy in patients with locally advanced breast cancer: correlation with tumor biological subtypes and pathological response after therapy. Tumor Biology. 2017;39(3):1010428317694540.
Ogston KN, Miller ID, Payne S, Hutcheon AW, Sarkar TK, Smith I, et al. A new histological grading system to assess response of breast cancers to primary chemotherapy: prognostic significance and survival. Breast. 2003;12(5):320–7.
von Minckwitz G, Untch M, Blohmer J-U, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796–804.
Earl H, Provenzano E, Abraham J, Dunn J, Vallier AL, Gounaris I, et al. Neoadjuvant trials in early breast cancer: pathological response at surgery and correlation to longer term outcomes - what does it all mean? BMC Med. 2015;13:234.
Houssami N, Macaskill P, von Minckwitz G, Marinovich ML, Mamounas E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer. 2012;48(18):3342–54.
Boland MR, McVeigh TP, O’Flaherty N, Gullo G, Keane M, Quinn CM, et al. Impact of receptor phenotype on nodal burden in patients with breast cancer who have undergone neoadjuvant chemotherapy. BJS Open. 2017;1(2):39–45.
Collins PM, Brennan MJ, Elliott JA, Abd Elwahab S, Barry K, Sweeney K, et al. Neoadjuvant chemotherapy for luminal a breast cancer: Factors predictive of histopathologic response and oncologic outcome. Am J Surg. 2020;222:368–76.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med. 2015;373(21):2005–14.
Harris LN, Ismaila N, McShane LM, Andre F, Collyar DE, Gonzalez-Angulo AM, et al. Use of biomarkers to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer: american society of clinical oncology clinical practice guideline. J Clin Oncol. 2016;34(10):1134–50.
Park BW, Kim JK, Heo C, Park KJ. Reliability of CT radiomic features reflecting tumor heterogeneity according to image quality and image processing parameters. Sci Rep. 2020;10(1):3852.
Sala E, Mema E, Himoto Y, Veeraraghavan H, Brenton JD, Snyder A, et al. Unravelling tumor heterogeneity using next-generation imaging: radiomics, radiogenomics, and habitat imaging. Clin Radiol. 2017;72(1):3–10.
El Naqa I, Grigsby PW, Apte A, Kidd E, Donnelly E, Khullar D, et al. Exploring feature-based approaches in PET images for predicting cancer treatment outcomes. Pattern Recogn. 2009;42(6):1162–71.
van Timmeren JE, Cester D, Tanadini-Lang S, Alkadhi H, Baessler B. Radiomics in medical imaging—“how-to” guide and critical reflection. Insights Imaging. 2020;11(1):91.
Goorts B, Dreuning KMA, Houwers JB, Kooreman LFS, Boerma E-JG, Mann RM, et al. MRI-based response patterns during neoadjuvant chemotherapy can predict pathological (complete) response in patients with breast cancer. Breast Cancer Res. 2018;20(1):34.
Drukker K, Edwards A, Doyle C, Papaioannou J, Kulkarni K, Giger ML. Breast MRI radiomics for the pretreatment prediction of response to neoadjuvant chemotherapy in node-positive breast cancer patients. J Med Imaging. 2019;6(3):034502.
Zhou J, Lu J, Gao C, Zeng J, Zhou C, Lai X, et al. Predicting the response to neoadjuvant chemotherapy for breast cancer: wavelet transforming radiomics in MRI. BMC Cancer. 2020;20(1):100.
Tokuda Y, Yanagawa M, Minamitani K, Naoi Y, Noguchi S, Tomiyama N. Radiogenomics of magnetic resonance imaging and a new multi-gene classifier for predicting recurrence prognosis in estrogen receptor-positive breast cancer: a preliminary study. Medicine. 2020;99(16): e19664.
Bismeijer T, van der Velden BHM, Canisius S, Lips EH, Loo CE, Viergever MA, et al. Radiogenomic analysis of breast cancer by linking MRI phenotypes with tumor gene expression. Radiology. 2020;296(2):277–87.
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage. 2006;31(3):1116–28.
Nioche C, Orlhac F, Boughdad S, Reuzé S, Goya-Outi J, Robert C, et al. LIFEx: a freeware for radiomic feature calculation in multimodality imaging to accelerate advances in the characterization of tumor heterogeneity. Can Res. 2018;78(16):4786.
Hatt M, Vallieres M, Visvikis D, Zwanenburg A. IBSI: an international community radiomics standardization initiative. J Nucl Med. 2018;59(supplement 1):287.
Ding J, Chen S, Serrano Sosa M, Cattell R, Lei L, Sun J, et al. Optimizing the peritumoral region size in radiomics analysis for sentinel lymph node status prediction in breast cancer. Acad Radiol. 2020.
Kim C, Han S-A, Won KY, Hong IK, Kim DY. Early prediction of tumor response to neoadjuvant chemotherapy and clinical outcome in breast cancer using a novel FDG-PET parameter for cancer stem cell metabolism. J Personal Med. 2020;10(3):132.
Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J, et al. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14(12):749–62.
Huang Y, Liu Z, He L, Chen X, Pan D, Ma Z, et al. Radiomics signature: a potential biomarker for the prediction of disease-free survival in early-stage (I or II) non—small cell lung cancer. Radiology. 2016;281(3):947–57.
Delzell DAP, Magnuson S, Peter T, Smith M, Smith BJ. Machine learning and feature selection methods for disease classification with application to lung cancer screening image data. Front Oncol. 2019;9:1393.
Tibshirani R. Regression shrinkage and selection via the Lasso. J Roy Stat Soc Ser B (Methodol). 1996;58(1):267–88.
Mathew J, Asgeirsson KS, Cheung KL, Chan S, Dahda A, Robertson JFR. Neoadjuvant chemotherapy for locally advanced breast cancer: a review of the literature and future directions. Eur J Surg Oncol (EJSO). 2009;35(2):113–22.
Sutton EJ, Onishi N, Fehr DA, Dashevsky BZ, Sadinski M, Pinker K, et al. A machine learning model that classifies breast cancer pathologic complete response on MRI post-neoadjuvant chemotherapy. Breast Cancer Res. 2020;22(1):57.
Braman NM, Etesami M, Prasanna P, Dubchuk C, Gilmore H, Tiwari P, et al. Intratumoral and peritumoral radiomics for the pretreatment prediction of pathological complete response to neoadjuvant chemotherapy based on breast DCE-MRI. Breast Cancer Res. 2017;19(1):57.
Chamming’s F, Ueno Y, Ferré R, Kao E, Jannot AS, Chong J, et al. Features from computerized texture analysis of breast cancers at pretreatment MR imaging are associated with response to neoadjuvant chemotherapy. Radiology. 2018;286(2):412–20.
Tahmassebi A, Wengert GJ, Helbich TH, Bago-Horvath Z, Alaei S, Bartsch R, et al. Impact of machine learning with multiparametric magnetic resonance imaging of the breast for early prediction of response to neoadjuvant chemotherapy and survival outcomes in breast cancer patients. Invest Radiol. 2019;54(2):110–7.
Wu J, Cao G, Sun X, Lee J, Rubin DL, Napel S, et al. Intratumoral spatial heterogeneity at perfusion MR imaging predicts recurrence-free survival in locally advanced breast cancer treated with neoadjuvant chemotherapy. Radiology. 2018;288(1):26–35.
Prat A, Fan C, Fernández A, Hoadley KA, Martinello R, Vidal M, et al. Response and survival of breast cancer intrinsic subtypes following multi-agent neoadjuvant chemotherapy. BMC Med. 2015;13(1):303.
Pease AM, Riba LA, Gruner RA, Tung NM, James TA. Oncotype DX® recurrence score as a predictor of response to neoadjuvant chemotherapy. Ann Surg Oncol. 2019;26(2):366–71.
Buus R, Sestak I, Barron S, Loughman T, Fender B, Ruiz CL, et al. Validation of the OncoMasTR risk score in estrogen receptor-positive/HER2-negative patients: a TransATAC study. Clin Cancer Res. 2020;26(3):623–31.
Mazo C, Barron S, Mooney C, Gallagher WM. Multi-gene prognostic signatures and prediction of pathological complete response to neoadjuvant chemotherapy in ER-positive, HER2-negative breast cancer patients. Cancers. 2020;12(5):1133.
Xiong Q, Zhou X, Liu Z, Lei C, Yang C, Yang M, Zhang L, Zhu T, Zhuang X, Liang C, Liu Z, Tian J, Wang K. Multiparametric MRI-based radiomics analysis for prediction of breast cancers insensitive to neoadjuvant chemotherapy. Clin Transl Oncol. 2020;22(1):50–9. https://doi.org/10.1007/s12094-019-02109-8.
Sun C, Tian X, Liu Z, Li W, Li P, Chen J, et al. Radiomic analysis for pretreatment prediction of response to neoadjuvant chemotherapy in locally advanced cervical cancer: a multicentre study. EBioMedicine. 2019;46:160–9.
Bickelhaupt S, Jaeger PF, Laun FB, Lederer W, Daniel H, Kuder TA, et al. Radiomics based on adapted diffusion kurtosis imaging helps to clarify most mammographic findings suspicious for cancer. Radiology. 2018;287(3):761–70.
Chen X, Oshima K, Schott D, Wu H, Hall W, Song Y, et al. Assessment of treatment response during chemoradiation therapy for pancreatic cancer based on quantitative radiomic analysis of daily CTs: an exploratory study. PLoS ONE. 2017;12(6): e0178961.
Zhou Y, Ma X-L, Pu L-T, Zhou R-F, Ou X-J, Tian R. Prediction of overall survival and progression-free survival by the (18)F-FDG PET/CT radiomic features in patients with primary gastric diffuse large B-cell lymphoma. Contrast Media Mol Imaging. 2019;2019:5963607.
Toyama Y, Hotta M, Motoi F, Takanami K, Minamimoto R, Takase K. Prognostic value of FDG-PET radiomics with machine learning in pancreatic cancer. Sci Rep. 2020;10(1):17024.
Yeh AC, Li H, Zhu Y, Zhang J, Khramtsova G, Drukker K, et al. Radiogenomics of breast cancer using dynamic contrast enhanced MRI and gene expression profiling. Cancer Imaging. 2019;19(1):48.
Nam KJ, Park H, Ko ES, Lim Y, Cho HH, Lee JE. Radiomics signature on 3T dynamic contrast-enhanced magnetic resonance imaging for estrogen receptor-positive invasive breast cancers: Preliminary results for correlation with Oncotype DX recurrence scores. Medicine. 2019;98(23): e15871.
Chen Y-X, Chen H, Rong Y, Jiang F, Chen J-B, Duan Y-Y, et al. An integrative multi-omics network-based approach identifies key regulators for breast cancer. Comput Struct Biotechnol J. 2020;18:2826–35.
Turanli B, Karagoz K, Bidkhori G, Sinha R, Gatza ML, Uhlen M, et al. Multi-omic data interpretation to repurpose subtype specific drug candidates for breast cancer. Front Genet. 2019;10:420.
Ng CKY, Bidard F-C, Piscuoglio S, Geyer FC, Lim RS, de Bruijn I, et al. Genetic heterogeneity in therapy-naïve synchronous primary breast cancers and their metastases. Clin Cancer Res. 2017;23(15):4402.
Sieuwerts AM, Willis S, Burns MB, Look MP, Gelder MEM-V, Schlicker A, et al. Elevated APOBEC3B correlates with poor outcomes for estrogen-receptor-positive breast cancers. Horm Cancer. 2014;5(6):405–13.
Ramón y Cajal S, Sesé M, Capdevila C, Aasen T, De Mattos-Arruda L, Diaz-Cano SJ, et al. Clinical implications of intratumor heterogeneity: challenges and opportunities. J Mol Med. 2020;98(2):161–77.
Gatenby RA, Grove O, Gillies RJ. Quantitative imaging in cancer evolution and ecology. Radiology. 2013;269(1):8–15.
Wu J, Gong G, Cui Y, Li R. Intratumor partitioning and texture analysis of dynamic contrast-enhanced (DCE)-MRI identifies relevant tumor subregions to predict pathological response of breast cancer to neoadjuvant chemotherapy. J Magn Reson Imaging. 2016;44(5):1107–15.
van Timmeren JE, Carvalho S, Leijenaar RTH, Troost EGC, van Elmpt W, de Ruysscher D, et al. Challenges and caveats of a multi-center retrospective radiomics study: an example of early treatment response assessment for NSCLC patients using FDG-PET/CT radiomics. PLoS ONE. 2019;14(6): e0217536.
Clifton H, Vial A, Miller A, Ritz C, Field M, Holloway L, et al., editors. Using machine learning applied to radiomic image features for segmenting tumor structures. In: 2019 Asia-Pacific signal and information processing association annual summit and conference (APSIPA ASC); 2019. pp 18–21.
Leijenaar RTH, Nalbantov G, Carvalho S, van Elmpt WJC, Troost EGC, Boellaard R, et al. The effect of SUV discretization in quantitative FDG-PET radiomics: the need for standardized methodology in tumor texture analysis. Sci Rep. 2015;5(1):11075.
Orlhac F, Soussan M, Chouahnia K, Martinod E, Buvat I. 18F-FDG PET-derived textural indices reflect tissue-specific uptake pattern in non-small cell lung cancer. PLoS ONE. 2015;10(12): e0145063.
Huang S-y, Franc BL, Harnish RJ, Liu G, Mitra D, Copeland TP, et al. Exploration of PET and MRI radiomic features for decoding breast cancer phenotypes and prognosis. npj Breast Cancer. 2018;4(1):24.
Granzier RWY, Verbakel NMH, Ibrahim A, van Timmeren JE, van Nijnatten TJA, Leijenaar RTH, et al. MRI-based radiomics in breast cancer: feature robustness with respect to inter-observer segmentation variability. Sci Rep. 2020;10(1):14163.
Versaci M, Calcagno S, Carlo Morabito F. Fuzzy geometrical approach based on unit hyper-cubes for image contrast enhancement. In: 2015 IEEE international conference on signal and image processing applications (ICSIPA). https://doi.org/10.1109/ICSIPA.2015.7412240
Moradmand H, Aghamiri SMR, Ghaderi R. Impact of image preprocessing methods on reproducibility of radiomic features in multimodal magnetic resonance imaging in glioblastoma. J Appl Clin Med Phys. 2020;21(1):179–90.
Zwanenburg A, Vallières M, Abdalah MA, Aerts H, Andrearczyk V, Apte A, et al. The image biomarker standardization initiative: standardized quantitative radiomics for high-throughput image-based phenotyping. Radiology. 2020;295(2):328–38.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
PM and BM wrote the main manuscript text. PM carried out the data analysis. RB, NOH and LW prepared and collected the data. SW reviewed the imaging analysis procedure. DS/KS/MK and AL reviewed the main manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the granted University College Hospital Galway ethical approval. The methods were carried out in accordance with the ethical standards as laid down in the 1964 declaration of Helsinki and it’s later amendments.
Consent for publication
All data was anonymized, therefore this is not applicable.
Competing interests
We disclose no conflict of interest and none of the authors are/ have been employed or consulted to companies in the medical industry.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McAnena, P., Moloney, B.M., Browne, R. et al. A radiomic model to classify response to neoadjuvant chemotherapy in breast cancer. BMC Med Imaging 22, 225 (2022). https://doi.org/10.1186/s12880-022-00956-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-022-00956-6