Abstract
Background
Diabetes has become a prominent global public health problem, which is an important cause of death, disease burden, and medical and health economic burden.
Previous studies have reported that majority of persons diagnosed with diabetes later presented with psychological and mental health diseases. The study aimed to explore the mediation role of anxiety on social support and depression among diabetic patents in elderly caring social organizations (SOs).
Methods
A multi-stage stratified cluster random sampling method was used in this cross-sectional study, and a questionnaire consisting of demographic questionnaire, MSPSS, GAD-7, and CES-D-10 was utilized to gather data. SPSS 22.0 and MPLUS 7.4 were used for statistical analysis. Spearman correlation analysis was employed to investigate correlations of key variables. A generalized linear model was used to exam factors associated with depression. Finally, the mediation effect among study variables was investigated by structural equation modeling (SEM).
Results
The average scores of social support, anxiety, and depression were 58.41 ± 14.67, 2.95 ± 3.95, and 7.24 ± 5.53, respectively. The factors of gender, social support, and anxiety were identified as significantly influential factors related to depression among diabetic patients in elderly caring SOs. The effect of social support on depression was significantly mediated by anxiety (β = -0.467, 95%CI: -0.813 to -0.251). Furthermore, anxiety partially mediated the relationship between family support and depression (β = -0.112, 95%CI: -0.229 to -0.012), and anxiety functioned as a complete mediator in the effect of significant others' support and depression (β = -0.135, 95%CI: -0.282 to -0.024).
Conclusions
The indirect effect of social support on depression through anxiety among diabetic patients in elderly caring SOs was elucidated. Social support played a key role in maintaining and regulating their mental health, particularly from family and significant others. Social support provided by both family and significant others exerted an important influence on maintaining and regulating their mental health. In light of this pathway, the elderly caring SOs should enhance the magnitude of social support from these two sources, thereby diminishing the likelihood of experiencing anxiety and depression.
Similar content being viewed by others
Introduction
With the progress of society and the development of medicine, the life expectancy of the population is gradually extended. Associated with this global phenomenon is the problem of aging populations. Therefore, biopsychosocial health, well-being, and quality of life of aging population are receiving increasing public and social attention. In China, in addition to providing home-based care from family, services for the elderly could be provided by nursing homes, elder care facilities, and senior apartments, which managed by governmental agencies, social organizations (SOs), or individual financiers [1, 2]. In contemporary China, due to the evolving family structure and shifting societal attitudes towards aging care, more and more older adults choose the elderly caring SOs to receive care services and support for themselves. Social organizations, also known as non-governmental or non-profit organizations, have emerged as pivotal actors within the realm of elderly care service, assuming a progressively prominent role [3].
Currently, diabetes is recognized as one of the prevalent chronic diseases globally. The incidence rate of diabetes is progressively increasing annually due to improvements in people's living standards, population aging, and the rising prevalence of obesity. According to the 10th edition of the Diabetes Atlas in 2021, the total diabetic patients around the world was 537 million, with 141 million in China [4]. In China, the prevalence of diabetes was 12.8%, indicating that approximately 1 in 10 individuals had diabetes [4]. Furthermore, diabetes is also common among residents of elderly caring SOs [5,6,7], and is associated with higher risk of institutionalization even after adjusting for complications [8, 9]. Health complications (stroke, blindness, renal failure, etc.) linked to diabetes include but not limited to. Those diabetic patients often experience comorbid psychological and mental diseases, with depression and anxiety emerging as the predominant conditions. Diabetes has become a prominent global public health problem, which is an important cause of death, disease burden, and economic burden. Previous studies revealed that diabetic older people in elderly caring SOs have more serious psychological problems than elderly diabetic patients who are living in personal homes [10, 11]. The group of older people with diabetes in the organizations had a lower social score in psychological domain than those who living in home through the WHOQOL questionnaire, but in physical and social domains the result was in contrast [11]. Furthermore, it is reported that the prevalence of diabetes among residents in organizations is generally on the rise [12]. More attention needs to be paid to the group of diabetic elderly who living in the elderly caring SOs.
Depression, as a severe mood disorder, can result in a notable deterioration of physical and social functioning [13]. What’s more, the psychological health of millions human around the world has been influenced by the COVID-19 pandemic, as it has intensified people's short-term and long-term stress, and damage. The World Mental Health Report released by WHO in June 2022 reported that the incidence rate of depression and anxiety increased by more than 25% in the first year of the pandemic [14]. The Chinese mental health survey in 2022, as documented in the Blue Book of Depression, unveiled a reported incidence rate of 3.4% for depression among the adult population in China. Depression stands as the primary contributor to disability among individuals diagnosed with chronic diseases. Many studies have shown that depression can affect medical symptoms related to diabetes by changing physiological processes and health-related behaviors [15, 16]. Despite the causal factor being a subject of ongoing debate, diabetic patients have an elevated risk of developing depression. Likewise, individuals with depression are more susceptible to developing diabetes [13, 17,18,19]. Research indicates that the incidence rate of depression in diabetic patients is twice that of the general population [20]. Besides, negative emotion associated with depression reduces the self-management ability and compliance with doctors' orders among diabetic patients. The ability to deal with interpersonal relationships and take care of themselves in life decreases, which leads to further deterioration of patients' condition [15, 21, 22]. These studies emphasize the significance of solving depression in individuals with diabetes. As a particularly vulnerable group, residents of nursing home were quarantined and socially isolated for a long time due to lockdown during the COVID-19, which lead to residents suffered from mental health problems, especially depression and anxiety [23,24,25].
Social support encompasses the perceived availability of social resources from individuals' social network members [2, 26]. It involves emotional, instrumental, and informational assistance provided by family, friends, and significant others, which individuals rely on to cope with stress, solve problems, and meet various needs. Social support has gained increasing recognition as a crucial determinant in promoting the well-being of diabetic patients, which can effectively reduce patients’ depression in nursing home [27, 28]. Earlier researches suggest that lower social support was related to depression, and poor adherence and glycemic control of diabetes [28,29,30], all of which contributed to worsening the biopsychological health of diabetic patients. Besides, social support from family was important to improve patients’ adherence [31].
In addition to depression, anxiety is another common complication of individuals with diabetes [32, 33]. The increased anxiety among diabetic patients can occur at the moment of being diagnosed, onset of complications, and the fear of hypoglycemia [32]. Overall, our study suggest that diabetes is associated with an increased risk of anxiety. A prior investigation revealed that up to 90% of individuals with anxiety disorders experience comorbid depression [34]. This has been corroborated another investigation which demonstrated that 39% of individuals diagnosed with anxiety met the criteria for depression [35]. Many studies have consistently shown an inverse relationship between anxiety and social support [2, 36]. Nevertheless, the relationship between social support and anxiety among residents with diabetes in elderly caring SOs remains unclear.
A number of researches has explored the relationship among social support, anxiety, and depression [37,38,39]. While most studies have investigated how social support mediates the association between anxiety and depression [40, 41], limited research has focused on understanding how anxiety influences the link between social support and depression specifically in diabetic patients. Nonetheless, some studies have provided evidence of a positive correlation between depression and anxiety in individuals diagnosed with type 2 diabetes, while depression is negatively correlated with social support [38]. Given recent research findings suggesting that anxiety played a predictive role in depression and the protective mechanism of social support in anxiety and depression [2, 42,43,44], we aim to examine the mediation role of anxiety on social support and depression among diabetic patents in elderly caring SOs.
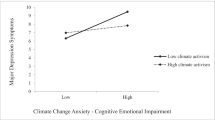
Therefore, we proposed the following hypotheses (Table 1) in alignment with the theoretical model (Fig. 1). To prove the above research hypotheses, structural equation model (SEM) was used. Finally, we aim to provide guidance for implementing intervention measures aimed at enhancing the biopsychosocial health of residents with diabetes in organizations.
Methods
Data and population
This study was carried out in July and August 2022 in Chongqing Province, China. A multi-stage stratified cluster random sampling method was employed to select participants [2], and data collection was conducted through a structured questionnaire. A total of 80 elderly caring SOs were selected from 4 districts (D, J, T, and R) in Chongqing province. Through the health records of the elderly caring SOs, which contained information on residents’ chronic diseases, potential participant diagnosed with diabetes in secondary hospitals and above were identified. Following that, face-to-face interviews were conducted. The objective and procedure of this survey were explained to the interviewees, and then informed consent was obtained before starting the survey. The inclusion criteria included (1) age 60 years or over, (2) diagnosed with diabetes in secondary hospitals and above (3) willingness to participate in this study. The exclusion criteria included (1) could not effectively communicate with investigators resulting from organic mental conditions such as visual impairments, auditory impairments, and so on (2) unwillingness to participate in this study. What’s more, our survey team was composed of members from Chongqing Medical University and Anhui Medical University who were well-trained and skilled. In total, 205 completed and valid questionnaires were analyzed.
Measures
Demographic characteristics
Demographic data includes gender, age, marital status, education, whether visited by relatives, and self-reported institutional satisfaction. Age was divided into ≤ 74, 75–89, and ≥ 90 years. Marital status was categorized into three groups: married (with spouses), single, and other (including widowed, divorced, or other). Education was classified into four groups: uneducated, primary school, middle school, and high school and above. Whether visited by relatives was divided into yes, no. Self-reported institutional satisfaction was sorted into low, medium, and high.
Multidimensional Scale of Perceived Social Support (MSPSS)
Social support was assessed based on three informal sources (family, friends, and significant others) using MSPSS [45]. The MSPSS has demonstrated strong internal consistency and good reliability in previous research [2, 46]. The instrument was composed of 12 self-assessment items, with each item rated on a seven-point Likert scale. Consequently, the total score of MSPSS ranged from 12 to 84, with a higher score indicating greater social support. In this survey, the Cronbach's α for the total scale and its subscales were as follows: 0.923 for social support, 0.956 for family support, 0.952 for friends’ support, and 0.921 for significant others’ support.
The 7-item self-reported Generalized Anxiety Disorder Scale (GAD-7)
Anxiety was gathered with GAD-7 [47, 48]. Respondents were asked to answer 7 items on a 4-point scale by considering the last 2 weeks. Multiple studies have demonstrated the acceptable internal consistency and good reliability of the GAD-7 [45, 49]. Cronbach’s α of this scale among current sample was 0.906. The GAD-7 yielded a total score ranging from 0 to 21, with higher scores indicating greater anxiety. Additionally, the cut-off scores of 5, 10, and 15 are commonly used to identify mild, moderate, and severe levels of anxiety symptoms, respectively [49].
The 10-item Center for Epidemiologic Studies Depression Scale (CES-D-10)
Depression was measured by CES-D-10 [50], which was a validated instrument used in China [51]. Extensive research has provided evidence of this scale's good reliability and validity [52]. Participants were asked to answer 10 items on a 4-point scale. The response options for the 8 negative items were scored on a scale ranging from 0 = “rarely or none of the time” (< 1 day) to 3 = “most or all of the time” (5–7 days), while the scoring of the response options for the 2 positive items was reversed. A week recall period was used. Thus, the total score of this scale fell within the range of 0 to 30, with higher scores indicating greater depression. The reliability of CES-D-10 in this study was good with Cronbach's α yielded a coefficient of 0.814.
Statistical analysis
SPSS 22.0 and MPLUS 7.4 were used for statistical analysis. First, descriptive statistics were employed to provide an overview of participant characteristics. Second, Spearman correlation analysis was conducted among study variable. Third, a generalized linear model was utilized to find the important influencing factors of depression and exam the relationship among social support, depression, and anxiety. Lastly, SEM was conducted to examine our seven hypotheses, while controlling significant influencing variables. The total score of social support and anxiety were treated as latent variables, while depression was measured as a measurement variable. In this study, p < 0.05 was considered significant.
In the structural equation modeling, bootstrap analysis was used. 95% bias-corrected confidence intervals for the indirect effect and moderated mediation effect from 1000 resamples of the data were produced by bootstrap analysis [53]. The model fit was considered acceptable if χ2 / df ≤ 3, CFI ≥ 0.90, TLI ≥ 0.90, SRMR ≤ 0.08, and RMSEA ≤ 0.10 [54, 55].
Results
Descriptive analysis
The average age of the 205 diabetic patients residing in elderly caring SOs was 78.37 ± 9.39 years, 53.20% were female, and 61.50% were widowed, divorced or other. Majority of the respondents were visited by their relatives (75.10%), and 35.6% of them had primary school level education. Furthermore, the mean score of anxiety, social support, and depression were 2.95 ± 3.95, 58.41 ± 14.67, and 7.24 ± 5.53, respectively (Table 2).
Correlation among study variables
Spearman correlation analysis revealed a significantly negative association between anxiety and social support, along with its three dimensions (Table 3). Nevertheless, a positive correlation was found between anxiety and depression. Likewise, the three dimensions of social support showed positive correlations with each other.
A generalized linear model
Model 1 analyzed the effects of anxiety and social support on depression. Table 4 revealed that gender was a significantly influential factor of depression among diabetic patients in elderly caring SOs, in addition to social support and anxiety. Furthermore, females (β = 1.273, p = 0.044) displayed elevated levels of depression compared to males. Model 2 analyzed the effect of anxiety and the three subscales of social support on depression. The findings indicated a significant association between depression and factors such as gender, family support, friends' support, and anxiety. Additionally, family support (β = -0.130, p = 0.018) exhibited a negative correlation with depression, as well as friends' support (β = -0.118, p = 0.045), while anxiety (β = -0.867, p < 0.001) was positively associated with depression. However, support from significant others had no significant correlation with depression.
Structural equation modeling
Under the condition of controlling variables that have a significant influence on the study variables, models were built to examine the mediation role of anxiety on social support and depression among diabetic patients in elderly caring SOs (Fig. 2). The model demonstrated good fit: χ2/df = 2.70, CFI = 0.929, TLI = 0.910, SRMR = 0.057, RMSEA = 0.091.
Figure 2 and Table 5 present the standardized direct and indirect effects among three key variables. Depression exhibited a significantly negative correlation with social support (β = -0.309, 95%CI: -0.618 to -0.010), thus, supporting Hypothesis 1. The findings of the study indicated that anxiety had a significantly positive impact on predicting depression (β = 0.883, 95%CI: 0.679 to 1.149), corroborating Hypothesis 2. Social support exhibited a significantly negative predictive effect on anxiety (β = -0.529, 95%CI: -0.921 to -0.275), which support Hypothesis 3. After including the mediator variable (anxiety), social support showed a significant adverse effect on depression (β = -0.467, 95%CI: -0.813 to -0.251), thereby supporting Hypothesis 4. Moreover, anxiety accounted for 60.18% of the mediated effect (-0.467/-0.776).
In the further analysis, mediation of anxiety was performed between the three subscales of social support and depression. The model showed good fit: χ2/df = 2.025, CFI = 0.955, TLI = 0.940, SRMR = 0.034, RMSEA = 0.071. As shown in Table 5, anxiety partially mediated the relationship between family support and depression (β = -0.112, 95%CI: -0.229 to -0.012), and anxiety accounted for 44.44% of the mediated effect of family support on depression (-0.112/-0.252). Therefore, Hypothesis 4-a was confirmed. In addition, anxiety played a full mediating role in the effect of significant others’ support and depression (β = -0.135, 95%CI: -0.282 to -0.024), which confirmed Hypothesis 4-c.
Discussion
Diabetes has become a prominent global public health problem, which is related to biopsychological diseases such as depression and anxiety [32]. Especially amid the COVID-19 pandemic, the residents in elderly caring SOs, as a particularly vulnerable group, are at a strong risk of experiencing psychological diseases due to diabetes and social isolation [23, 24]. The study was dedicated to explore the mediating role of anxiety in the relationship between social support (including its three subscales) and depression among diabetic patents in elderly caring SOs. The results revealed that compared to diabetic patients in the community, the diabetic patents in elderly caring SOs targeted in this study had lower overall social support, with consistent results in the family support and friends’ support dimensions. However, in the dimension of support from significant others, diabetic patents in elderly caring SOs had higher levels of support, which may be due to their friendly interactions with staff and other companions in the organizations, receiving emotional and practical assistance [56]. The level of social support in the population under investigation in this study was moderately satisfactory [45, 57]. A study from Sichuan, China, also indicated a moderate degree of social support among diabetic patients [27]. Their anxiety levels in this study were relatively mild, which was lower than the anxiety levels observed among diabetes patients in a hospital in Nepal [58]. In terms of depressive symptoms, they displayed either no symptoms of depression or extremely mild depressive symptoms, which was lower than the estimates reported in another study [59]. The differences in depressive and anxiety conditions may be attributed to the varying environments in which diabetes patients are situated. More importantly, during the COVID-19, family members and significant others might lose the opportunity for in-person visits, while the frequency of communication through alternative means such as phone calls and video chats may be higher. This may reduce their level of anxiety and depression. Additionally, compared to usual circumstances, the employees of elderly caring SOs would place greater emphasis on the health conditions of the residents [60, 61].
Based on the study findings, gender emerges as a predictive factor for depression among the population targeted in this study, with female patients being more susceptible to experiencing depressive symptoms. This phenomenon has been consistently documented in previous studies, suggesting a greater incidence of depression among females in elderly caring SOs compared to their male counterparts [62,63,64,65]. One possible explanation is that female diabetic patients residing in elderly caring SOs may have limited social interactions, leading to a stronger desire to share their emotions. Due to their usual residence in such facilities and relatively less attention from family members, combined with restricted visitation during the pandemic, the female diabetic patients perhaps were more inclined to seek "help". Thus, amplifying the pain caused by their illness in the hope of receiving understanding and assistance from others [66].
Under the controlled conditions of influential variables, we have identified the following connections among the core variables. Firstly, a negative association was found between social support and depression, suggesting that targeted people in this study who exhibit lower levels of social support are more prone to experiencing heightened levels of depression. This finding aligns with preceding research findings [67,68,69]. This research also found a positive correlation between anxiety and depression, highlighting the crucial function of anxiety in this context [70]. Interestingly, we observed that an even more remarkable finding is that we have also discovered that social support did not only directly influences depression but also exerted an indirect influence through anxiety, thereby establishing an indirect negative correlation mediated by anxiety. This aligns with the results presented by Ji Kai in his study [44, 49]. Our study has unveiled a novel pathway through which social support alleviates depression by means of anxiety. This discovery opens up new avenues for shaping the trajectory of late-life health and well-being. From a practical standpoint, elderly caring SOs should place greater emphasis on the extent to which social support meets the companionship and support needs of diabetic patients. It is crucial to promptly identify anxiety emotions within the population and actively guide individuals to prevent the escalation of depressive conditions on a larger scale [71, 72].
Importantly, the further mediation analyses conducted on the three dimensions of social support showed that lower levels of support from family members and significant others act as catalysts for depression. This effect is mediated through anxiety, resulting in an elevation of depressive symptoms. Moreover, it was found that support from significant others exerted influence on depression exclusively through anxiety. This finding is consistent with the research conducted by Rehan Aziz, who identified social support, diabetes, and anxiety as factors influencing depression [63]. Relatedly, in a study focusing on perinatal depression among women, it was found that inadequate support from partners, friends, and family members was linked to a higher likelihood of experiencing depression and anxiety [73]. This might be because family members and significant others can help individuals build a strong support network, which contributes to the prevention of depression. They can provide emotional support, encouragement, and understanding, making individuals feel cared for and supported. This helps reduce anxiety about illness and life, thus reducing the occurrence of depressive symptoms. Additionally, family members and significant others can provide information and education about mental health and depression. Understanding the symptoms and coping methods of depression can help individuals better understand their own situation and take early action.
In order to effectively reduce depression levels among the targeted people in this study and enhance their overall quality of life in later stages, we propose the following recommendations. Firstly, leveraging advancements in modern technology, such as remote video communication, home network connectivity devices, and digital photo albums, can bridge the gap between diabetic patients and their family members. Secondly, we suggest incorporating an innovative theory, namely the Act-Belong-Commit mental health promotion campaigns. Act-Belong-Commit is a mental health promotion campaign aimed at enhancing the mental health of individuals and communities. By encouraging people to actively engage in sports, artistic activities, volunteer work, social interactions, and other activities beneficial to mental health, Act-Belong-Commit aims to foster meaningful relationships and community involvement to help individuals and communities establish positive mental health habits and lifestyles. These activities are crucial for enhancing social support and reducing feelings of loneliness, ultimately facilitating social connections among diabetic patients with emotional issues [71]. This applies to elderly caring social SOs, where it is recommended that nursing homes facilitate a wide range of cultural and recreational activities. Collaboration with other institutions can be considered to foster the integration of social networks among individuals with diabetes. Thirdly, the elderly caring SOs should collaborate with the government, medical institutions, and other relevant organizations to provide comprehensive services that integrate elderly care, medical services, and nursing, aiming to achieve a transition towards an integrated model of medical and elderly care. This will help establish a new type of elderly caring SOs. Fourthly, to further alleviate the anxiety of diabetic patients in elderly caring SOs, we encourage elderly who can exercise independently to engage in moderate physical activity every day, including walking, yoga, Tai Chi, and light running. For elderly with physical limitations, we suggest fully utilizing the volunteer resources of the organization to channel their passive emotions. Finally, we hope that the government can further fulfill its leading role by collaborating with social organizations and private capital to promote the high-quality development of elderly care institutions. This includes meeting the diverse care needs of the service recipients and gradually addressing their psychological and emotional needs.
We acknowledge this study has some limitations. Firstly, our research design employed a cross-sectional approach, focusing only on diabetic patients in specific elderly caring SOs in Chongqing during COVID-19 pandemic period. As a result, the causal inference capability of the study findings is limited. Secondly, our study was conducted solely in Chongqing, which poses challenges in generalizing the research results to other populations. In future research, we aim to address these limitations and further enhance the study's scope.
Conclusion
Our study suggests that gender, social support, and anxiety can all be factors influencing depression among diabetic patients in elderly caring SOs. Simultaneously, our study is a significant step towards clarifying the important role of anxiety in mediating the relationship between social support and depression, especially social support from family and significant others, which offers fresh perspectives on improving targeted people’s quality of life. The elderly caring SOs should actively engage in collaborative activities, expand the social network of diabetic patients, enhance the magnitude of social support, and further alleviate anxiety levels, thereby diminishing the likelihood of experiencing depression.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- S.E.:
-
Standard error
- CI:
-
Confidence interval
- Ref:
-
Reference
References
Chu LW, Chi I. Nursing homes in China. J Am Med Dir Assoc. 2008;9(4):237–43.
Zhao L, Zheng X, Ji K, Wang Z, Sang L, Chen X, Tang L, Zhu Y, Bai Z, Chen R. The Relationship between Social Support and Anxiety among Rural Older People in Elderly Caring Social Organizations: A Cross-Sectional Study. Int J Environ Res Public Health. 2022;19(18):11411.
Chen X, Tang L, Liu L, Bai Z, Chen R. Factors related to turnover intention among staff of elderly caring social organizations in Anhui Province, China: a cross-sectional study. BMC Health Serv Res. 2021;21(1):1265.
Federation ID. IDF Diabetes Atlas, 10th edition. In., 10th edn. Brussels, Belgium. 2021.
Migdal A, Yarandi SS, Smiley D, Umpierrez GE. Update on diabetes in the elderly and in nursing home residents. J Am Med Dir Assoc. 2011;12(9):627-632.e622.
Jorde R, Hagen T. Screening for diabetes using HbA1c in elderly subjects. Acta Diabetol. 2006;43(2):52–6.
Andreassen LM, Sandberg S, Kristensen GB, Sølvik U, Kjome RL. Nursing home patients with diabetes: prevalence, drug treatment and glycemic control. Diabetes Res Clin Pract. 2014;105(1):102–9.
Rodríguez-Sánchez B, Angelini V, Feenstra T, Alessie RJ. Diabetes-Associated Factors as Predictors of Nursing Home Admission and Costs in the Elderly Across Europe. J Am Med Dir Assoc. 2017;18(1):74–82.
Valiyeva E, Russell LB, Miller JE, Safford MM. Lifestyle-related risk factors and risk of future nursing home admission. Arch Intern Med. 2006;166(9):985–90.
Bahrmann A, Abel A, Specht-Leible N, Abel A, Wörz E, Hölscher E, Zieschang T, Oster P, Zeyfang A. Treatment quality in geriatric patients with diabetes mellitus in various home environments. Z Gerontol Geriatr. 2010;43(6):386–92.
Ghassemzadeh R, Nasseh H, Arastoo AA, Kamali M, Rahimi Foroushani A, Arzaghi M. Quality of life in elderly diabetic: comparison between home and nursing home. Acta Med Iran. 2013;51(4):254–9.
Dybicz SB, Thompson S, Molotsky S, Stuart B. Prevalence of diabetes and the burden of comorbid conditions among elderly nursing home residents. Am J Geriatr Pharmacother. 2011;9(4):212–23.
Tovar E, Rayens MK, Gokun Y, Clark M. Mediators of adherence among adults with comorbid diabetes and depression: The role of self-efficacy and social support. J Health Psychol. 2015;20(11):1405–15.
Organization WH. World mental health report: Transforming mental health for all. 2022.
Sacco WP, Yanover T. Diabetes and depression: the role of social support and medical symptoms. J Behav Med. 2006;29(6):523–31.
Talbot F, Nouwen A. A review of the relationship between depression and diabetes in adults: is there a link? Diabetes Care. 2000;23(10):1556–62.
Sartorius N. Depression and diabetes. Dialogues Clin Neurosci. 2018;20(1):47–52.
Holt RI, de Groot M, Lucki I, Hunter CM, Sartorius N, Golden SH. NIDDK international conference report on diabetes and depression: current understanding and future directions. Diabetes Care. 2014;37(8):2067–77.
Vancampfort D, Mitchell AJ, De Hert M, Sienaert P, Probst M, Buys R, Stubbs B. Type 2 diabetes in patients with major depressive disorder: a meta-analysis of prevalence estimates and predictors. Depress Anxiety. 2015;32(10):763–73.
Moulton CD, Pickup JC, Ismail K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015;3(6):461–71.
Hermanns N, Caputo S, Dzida G, Khunti K, Meneghini LF, Snoek F. Screening, evaluation and management of depression in people with diabetes in primary care. Prim Care Diabetes. 2013;7(1):1–10.
Prigge R, Wild SH, Jackson CA. Depression, diabetes, comorbid depression and diabetes and risk of all-cause and cause-specific mortality: a prospective cohort study. Diabetologia. 2022;65(9):1450–60.
Pitkälä KH. COVID-19 has hit nursing homes hard. Eur Geriatr Med. 2020;11(6):889–91.
Dichter MN, Sander M, Seismann-Petersen S, Köpke S. COVID-19: it is time to balance infection management and person-centered care to maintain mental health of people living in German nursing homes. Int Psychogeriatr. 2020;32(10):1157–60.
Boucaud-Maitre D, Villeneuve R, Tabue-Teguo M. Post-containment management of nursing homes: a new public health concern. Eur Geriatr Med. 2020;11(4):707–8.
Helgeson VS. Social support and quality of life. Qual Life Res. 2003;12(Suppl 1):25–31.
Liu Y, Meng H, Tu N, Liu D. The Relationship Between Health Literacy, Social Support, Depression, and Frailty Among Community-Dwelling Older Patients With Hypertension and Diabetes in China. Front Public Health. 2020;8:280.
Burns RJ, Deschênes SS, Schmitz N. Associations between Depressive Symptoms and Social Support in Adults with Diabetes: Comparing Directionality Hypotheses with a Longitudinal Cohort. Ann Behav Med. 2016;50(3):348–57.
Ibarra-Rovillard MS, Kuiper NA. Social support and social negativity findings in depression: perceived responsiveness to basic psychological needs. Clin Psychol Rev. 2011;31(3):342–52.
Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr DiabRep. 2012;12(6):769–81.
Onyango JT, Namatovu JF, Besigye IK, Kaddumukasa M, Mbalinda SN. The relationship between perceived social support from family and diabetes self-management among patients in Uganda. Pan Afr Med J. 2022;41:279.
Ducat L, Rubenstein A, Philipson LH, Anderson BJ. A review of the mental health issues of diabetes conference. Diabetes Care. 2015;38(2):333–8.
Bickett A, Tapp H. Anxiety and diabetes: Innovative approaches to management in primary care. Exp Biol Med (Maywood). 2016;241(15):1724–31.
Tiller JWG. Depression and anxiety. Med J Aust. 2013;199(S6):S28–31.
Hunt C, Issakidis C, Andrews G. DSM-IV generalized anxiety disorder in the Australian National Survey of Mental Health and Well-Being. Psychol Med. 2002;32(4):649–59.
Baharvand P, Anbari K, Hamidi H. Perceived social support in pregnant women with gestational diabetes attending hospitals in western Iran compared to healthy controls and its relationship with perceived anxiety. J Diabetes Metab Disord. 2022;21(2):1549–55.
Zhan J, Chen C, Yan X, Wei X, Zhan L, Chen H, Lu L. Relationship between social support, anxiety, and depression among frontline healthcare workers in China during COVID-19 pandemic. Front Psych. 2022;13:947945.
Wu SF, Young LS, Yeh FC, Jian YM, Cheng KC, Lee MC. Correlations among social support, depression, and anxiety in patients with type-2 diabetes. J Nurs Res. 2013;21(2):129–38.
Al-Dwaikat TN, Rababa M, Alaloul F. Relationship of stigmatization and social support with depression and anxiety among cognitively intact older adults. Heliyon. 2022;8(9):e10722.
Xu H, Peng L, Wang Z, Liu X. Effects of psychological capital and social support availability on anxiety and depression among Chinese emergency physicians: Testing moderated mediation model. Front Psychol. 2022;13:991239.
Cheng B, Roberts N, Zhou Y, Wang X, Li Y, Chen Y, Zhao Y, Deng P. Social support mediates the influence of cerebellum functional connectivity strength on postpartum depression and postpartum depression with anxiety. Transl Psychiatry. 2022;12(1):54.
Li X, Yang P, Jiang Y, Gao D. Influence of fear of COVID-19 on depression: The mediating effects of anxiety and the moderating effects of perceived social support and stress perception. Front Psychol. 2022;13:1005909.
Gay MC, Vrignaud P, Garitte C, Meunier C. Predictors of depression in multiple sclerosis patients. Acta Neurol Scand. 2010;121(3):161–70.
Gay MC, Bungener C, Thomas S, Vrignaud P, Thomas PW, Baker R, Montel S, Heinzlef O, Papeix C, Assouad R, et al. Anxiety, emotional processing and depression in people with multiple sclerosis. BMC Neurol. 2017;17(1):43.
Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55(3–4):610–7.
Cao W, Li L, Zhou X, Zhou C. Social capital and depression: evidence from urban elderly in China. Aging Ment Health. 2015;19(5):418–29.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Choi EPH, Hui BPH, Wan EYF. Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020;17(10):3740.
Ji K, Bai Z, Tang L, Yan H, Zhu Y, Chen G, Chen R. Institutional Satisfaction and Anxiety Mediate the Relationship Between Social Support and Depression in Hypertension Patients in Elderly Caring Social Organizations: A Cross-Sectional Study. Front Psychol. 2021;12:772092.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84.
Chen H, Mui AC. Factorial validity of the Center for Epidemiologic Studies Depression Scale short form in older population in China. Int Psychogeriatr. 2014;26(1):49–57.
Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. 1999;14(8):608–17.
Hayes A. Introduction to mediation, moderation, and conditional process analysis. J Educ Meas. 2013;51(3):335–7.
Kelloway EK. Using LISREL for structural equation modeling: A researcher’s guide. 1998.
Lt Hu. Bentler PM: Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55.
Yang Juan LJ, Tang F, Li Y, Liu J. Investigation of depression status of type 2 diabetic patients live incommunity and relative factors (in Chinese). Chin Nurs J. 2009;44(07):658–60.
Liu Y, Zhang L, Guo N, Jiang H. Postpartum depression and postpartum post-traumatic stress disorder: prevalence and associated factors. BMC Psychiatry. 2021;21(1):487.
Sharma K, Dhungana G, Adhikari S, Bista Pandey A, Sharma M. Depression and Anxiety among Patients with Type II Diabetes Mellitus in Chitwan Medical College Teaching Hospital. Nepal Nurs Res Pract. 2021;2021:8846915.
Swenson SL, Rose M, Vittinghoff E, Stewart A, Schillinger D. The influence of depressive symptoms on clinician-patient communication among patients with type 2 diabetes. Med Care. 2008;46(3):257–65.
Pinazo-Hernandis S, Sales A, Martinez D. Older Women’s Loneliness and Depression Decreased by a Reminiscence Program in Times of COVID-19. Front Psychol. 2022;13:802925.
Tak YR, Woo HY, Han Yi L, Kim AR. Useful lessons for the provision of services in long-term care facilities in South Korea: operators’ experiences illuminate the phenomenon of working with the elderly in the field. Int J Qual Stud Health Well-being. 2019;14(1):1565238.
Li H, Liu X, Zheng Q, Zeng S, Luo X. Gender differences and determinants of late-life depression in China: A cross-sectional study based on CHARLS. J Affect Disord. 2022;309:178–85.
Aziz R, Steffens DC. What are the causes of late-life depression? Psychiatr Clin North Am. 2013;36(4):497–516.
Moreno X, Gajardo J, Monsalves MJ. Gender differences in positive screen for depression and diagnosis among older adults in Chile. BMC Geriatr. 2022;22(1):54.
Lee YC, Sousa TV, Stretton-Smith PA, Gold C, Geretsegger M, Baker FA. Demographic and clinical profile of residents living with dementia and depressive symptoms in Australian private residential aged care: Data from the Music Interventions for Dementia and Depression in ELderly care (MIDDEL) cluster-randomised controlled trial. Australas J Ageing. 2022;41(4):e387–96.
Parker G, Brotchie H. Gender differences in depression. Int Rev Psychiatry. 2010;22(5):429–36.
Domènech-Abella J, Lara E, Rubio-Valera M, Olaya B, Moneta MV, Rico-Uribe LA, Ayuso-Mateos JL, Mundó J, Haro JM. Loneliness and depression in the elderly: the role of social network. Soc Psychiatry Psychiatr Epidemiol. 2017;52(4):381–90.
Levy M, Burns RJ, Deschênes SS, Schmitz N. Does Social Support Moderate the Association Among Major Depression, Generalized Anxiety Disorder, and Functional Disability in Adults With Diabetes? Psychosomatics. 2017;58(4):364–74.
Schmitz N, Messier L, Nitka D, Ivanova A, Gariepy G, Wang J, Malla A, Boyer R, Lesage A, Strychar I. Factors associated with disability and depressive symptoms among individuals with diabetes: a community study in Quebec. Psychosomatics. 2011;52(2):167–77.
Xu J, Wei Y. Social support as a moderator of the relationship between anxiety and depression: an empirical study with adult survivors of Wenchuan earthquake. PLoS ONE. 2013;8(10):e79045.
Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, Meilstrup C, Madsen KR, Koushede V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62–70.
Huang D, Zeng T, Mao J, Zhao M, Wu M. The unmet needs of older adults living in nursing homes in Mainland China: a nation-wide observational study. BMC Geriatr. 2022;22(1):989.
Sufredini F, Catling C, Zugai J, Chang S. The effects of social support on depression and anxiety in the perinatal period: A mixed-methods systematic review. J Affect Disord. 2022;319:119–41.
Acknowledgements
NA.
Funding
This study was funded by the National Science Foundation of China (NO.71874002 and NO.72174001), National Science Foundation of China's international cooperation and exchange projects (NO.72111530207), Royal Society of Edinburgh (961_YANG), Scientific Research Projects for Higher Education of Anhui Province under Grant 2023AH010036, Graduate Research and Practice Innovation projects in Anhui Medical University (N0. YJS20230052). These organizations had no role in the research design, data collection, data analysis, manuscript writing, and submission.
Author information
Authors and Affiliations
Contributions
Lanlan Zhao and Fuqin Xu contributed equally to this work and should be regarded as co-first authors. LL Z and FQ X drafted the manuscript together. KJ and B O revised the manuscript. SD and GQ L participated in investigation and verification. XZ and SF Y obtained funding and revised the manuscript. RC performed the study concept, participated in its design and coordination, obtained funding and helped to draft the manuscript. ZW X participated in the subsequent revision of the paper. All authors read and approved the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Biomedical Ethics Committee of Anhui Medical University (No. 20180181; 1 March 2018). Informed consent was obtained from all subjects involved in the study.
Consent for publication
NA.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, L., Xu, F., Zheng, X. et al. Mediation role of anxiety on social support and depression among diabetic patients in elderly caring social organizations in China during COVID-19 pandemic: a cross-sectional study. BMC Geriatr 23, 790 (2023). https://doi.org/10.1186/s12877-023-04502-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04502-z