Abstract
Background
Matrix-induced autologous chondrocyte implantation (mACI) can be performed in a full arthroscopic or mini-open fashion. A systematic review was conducted to investigate whether arthroscopy provides better surgical outcomes compared with the mini-open approach for mACI in the knee at midterm follow-up.
Methods
This systematic review was conducted following the PRISMA guidelines. The literature search was performed in May 2021. All the prospective studies reporting outcomes after mACI chondral defects of the knee were accessed. Only studies that clearly stated the surgical approach (arthroscopic or mini-open) were included. Only studies reporting a follow-up longer than 12 months were eligible. Studies reporting data from combined surgeries were not eligible, nor were those combining mACI with less committed cells (e.g., mesenchymal stem cells).
Results
Sixteen studies were included, and 770 patients were retrieved: 421 in the arthroscopy group, 349 in the mini-open. The mean follow-up was 44.3 (12–60) months. No difference between the two groups was found in terms of mean duration of symptoms, age, body mass index (BMI), gender, defect size (P > 0.1). No difference was found in terms of Tegner Score (P = 0.3), Lysholm Score (P = 0.2), and International Knee Documentation Committee (IKDC) Score (P = 0.1). No difference was found in the rate of failures (P = 0.2) and revisions (P = 0.06).
Conclusion
Arthroscopy and mini-arthrotomy approaches for mACI in knee achieve similar outcomes at midterm follow-up.
Level of evidence
II, systematic review of prospective studies.
Similar content being viewed by others
Introduction
Focal chondral defects of the knee are common [1]. Hyaline cartilage is avascular, alymphatic, and hypocellular, with low metabolic activity [2,3,4]. Given these proprieties, the healing process often does not result in restitutio ad integrum, and residual defects are common [5, 6]. Symptomatic chondral defects are debilitating, and may lead to retirement from sports activities [7]. In patients with focal chondral defects, surgical treatment is often required [8, 9]. For smaller defects, microfractures are commonly performed [10,11,12,13,14]. Matrix-induced autologous chondrocyte implantation (mACI) has been commonly used to address bigger defects [15, 16]. During mACI, chondrocytes are harvested from a nonweightbearing zone of the articular cartilage of the knee in a first surgical session, seeded over a membrane, then expanded in vitro [17, 18]. In a second surgical session, the membrane loaded with autologous expanded chondrocytes is trimmed to fit the defect size, then placed into the defect [19, 20]. This second surgical session can be performed arthroscopically or with an arthrotomy in a minimally invasive fashion (mini-open). Whether the surgical approach influences the surgical outcome of mACI in the knee has not been previously investigated. Thus, a systematic review was conducted to investigate whether arthroscopy provides better surgical outcomes compared with the mini-open approach for mACI in knee at midterm follow-up. The focus of the present work was on patient-reported outcome measures (PROMs) and complications.
Material and methods
Search strategy
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21]. The PICOTD framework was followed:
-
P (Problem): knee chondral defect;
-
I (Intervention): mACI;
-
C (Comparison): arthroscopy versus mini-open surgery;
-
O (Outcomes): clinical scores and complications;
-
T (Timing): \(\ge\) 12 months follow-up;
-
D (Design): prospective trials.
Data source and extraction
Two authors (**;**) independently conducted the literature search in January 2021. The main online databases were accessed: PubMed, Google scholar, Embase, and Scopus. The following keywords were used in combination: chodral, cartilage, articular, damage, defect, injury, chondropathy, knee, pain, matrix-induced, autologous, chondrocyte, transplantation, implantation, mACI, therapy, management, surgery, arthroscopy, mini-open, outcomes. The same authors performed separately the initial screening. The full text of the articles of interest was accessed. A cross reference of the bibliographies was also conducted. Disagreements were debated and solved by a third author (**).
Eligibility criteria
All the studies reporting outcomes after mACI for knee chondral defects were accessed. According to the authors’ language capabilities, articles in English, German, Italian, French, and Spanish were eligible. Only prospective studies with levels I to II of evidence, according to Oxford Centre of Evidence-Based Medicine [22], were considered. Only studies that clearly stated the fashion of the surgical approach (arthroscopic or mini-open) were included. Procedures other than mACI were excluded. Only studies reporting a follow-up \(\ge\) 12 months were considered eligible. Animal or in vitro studies were not eligible. Studies investigating other surgical approaches rather than arthroscopic or mini-open were not eligible. Studies reporting data from combined surgeries were not eligible. Studies combining mACI with other less committed cells (e.g., mesenchymal stem cells) were not considered. Reviews, comments, letters, editorials, and techniques were not eligible. Only articles reporting quantitative data under the outcomes of interest were considered for inclusion. Missing data under the outcomes of interest warranted exclusion from the present study. Table 1 displays the eligibility criteria.
Data extraction
Two independent authors (**;**) performed data extraction. Study generalities (author, year, journal, type of study) and patient baseline demographic information were collected (number of samples and related mean BMI and age, duration of the symptoms, duration of the follow-up, percentage of female). For every approach, the following data were retrieved: Lysholm Knee Scoring Scale [23], Tegner Activity Scale [24], and International Knee Documentation Committee (IKDC) [25] Score. Data from complications were also collected: rate of failures and revisions.
Methodology quality assessment
The methodological quality assessment was performed by two independent authors (**;**). The risk of bias graph tool of the Review Manager Software (The Nordic Cochrane Collaboration, Copenhagen) was used. The following risks of bias were evaluated: selection, detection, attrition, and other source of bias.
Statistical analysis
The statistical analyses were performed with IBM SPSS Version 25. Continuous data were reported as mean difference (MD) and standard deviation. For binary data, odds ratio (OR) effect measure was calculated. The confidence interval (CI) was set at 95% in all the comparisons. t-Test and \(\chi\)2 tests were evaluated for continuous and binary data, respectively, with P < 0.05 considered statistically significant.
Results
Search result
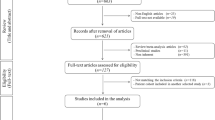
The literature search identified 559 clinical investigations. Of them, 201 were excluded as they were duplicates. A further 342 articles were excluded because they did not fulfill our eligibility criteria: not focused on mACI (N = 171), not clearly stating the approach (N = 74), retrospective nature of the study design (N = 29), performing arthrotomy (N = 27), combined with stem cells (N = 13), other (N = 19), not reporting quantitative data under the outcomes of interest (N = 6), language limitations (N = 3). This left 16 studies for inclusion in the present investigation: six randomized controlled trials (RCTs) and ten non-RCTs. The flowchart of the literature search is shown in Fig. 1.
Methodological quality assessment
Given the limited number of included RCTs, the graph evidenced moderate risk of selection bias. The risk of selection bias of allocation concealment was low. The risk of detection bias was moderate, since the outcome assessments were rarely blinded. The risk of attrition and reporting bias were both moderate to low, as were the risk of other biases. Concluding, the overall review of the authors’ judgments about each risk of bias item was low, attesting to this study’s good methodological assessment. The risk of bias graph is shown in Fig. 2.
Patient demographics
Data from 770 patients were retrieved: 421 in the arthroscopy group, 349 in the mini-open group. The mean duration of symptoms before the index surgery was 48.6 (26.4–91.2) months. Women accounted for 35% (273 of 770) of the sample. The mean age of the patients was 34.1 ± 4.6 years, and the mean BMI was 25.1 ± 0.8 kg/m2. The mean defect size was 4.0 ± 1.4 cm2. The mean follow-up was 44.3 (12–60) months. No difference between the two groups was found in terms of mean duration of symptoms, age, BMI, gender, or defect size (P > 0.1). Generalities and demographic of the studies are presented in Table 2.
Efficacy of the procedure
At a mean follow-up of 44.3 (12–60) months, all PROMs of interest were improved (Table 3): VAS (MD −3.2; P = 0.008), Tegner (+2.2; P = 0.001), Lysholm (+31.9; P = 0.0002), IKDC (+33.2; P < 0.0001).
Outcomes of interest
No difference was found in terms of Tegner Score (MD 0.5; P = 0.3), Lysholm Score (MD 6.9; P = 0.2), and IKDC Score (MD 6.8; P = 0.1). Similarly, no difference was found in the rate of failures (OR 1.4; P = 0.2) and revisions (OR 0.1; P = 0.06). Results of the scores are presented in Table 4 and those of complications in Table 5.
Discussion
This systematic review was conducted to investigate whether arthroscopy provides better surgical outcomes compared with the mini-open approach for mACI in knee at midterm follow-up. According to the main findings of the present study, no difference was found between the two approaches in terms of PROMs. Additionally, at a mean of 44 months follow-up, no difference was found in the rate of failure and revision surgeries.
We were able to identify one study that compared open ACI covered by autologous periosteal flap (pACI) versus arthroscopic mACI [30]. PACI was performed in the fashion described by Bittermber et al. [39]. During arthroscopic mACI, expanded chondrocytes are seeded into a three-dimensional hyaluronic acid membrane (Hyaff-11; Fidia Advanced Biopolymers, Abano Terme, Italy), producing the scaffold called Hyalograft C. The membrane was then delivered into the defect in a “dry” arthroscopy after trimming using a suitable sized cylindrical cutting device. If necessary, several grafts can be applied to fill the defect, using an arthroscopic impactor. This technique produced better results compared with the open pACI in terms of IKDC and complications. However, whether this superiority arose from the approach or the surgical technique is unclear. The same arthroscopic technique was used by Filiardo et al., who reported very good results [31, 32]. The same arthroscopic technique using Hyalograft C was compared with a mini-open mACI (22 versus 39 patients, respectively) [33]. However, they used a porcine resorbable collagen I/III membrane for the mini-open procedure. They found comparable results at 5 years follow-up. There were four failures in the arthroscopic group (18.2%) and eight in the mini-open group (20.5%), with no statistically significant difference between them. The arthroscopic group reported a greater IKDC (55.9 ± 22.1 versus 67.4 ± 21.5; P = 0.05) at 1-year follow-up, with no differences at 24- and 60-month follow-up. These results suggested that the arthroscopic approach allows quicker recovery, but similar outcomes at midterm follow-up. However, they used two different membrane (Hyalograft C versus porcine resorbable collagen I/III membrane). Thus, it is unclear whether the quicker recovery seen at 12-month follow-up related to the approach or the different membrane. Two studies by Ebert et al. [27, 28] performed a similar full-arthroscopic procedure: after shaving and debridement, the defect was mapped in several planes using a graduated arthroscopy probe. The membrane was trimmed so as to be slightly oversized. At dry arthroscopy, the defect was dried using an arthroscopic sucker, and an adrenaline-soaked patty was pressed onto the subchondral bone to further dry it and prevent bleeding. Using a no-valves large-bore arthroscopic cannula, the membrane was positioned into the defect. The membrane was successively extracted out of the joint, and the size was finalized to correctly fit the defect ensuring correctly orientation of the graft. The membrane was glued, and a Silastic Foley catheter was introduced in the knee. The balloon was then inflated with saline for 30 s to compress the membrane and to secure it to the defect. There were minor variations in the execution of the surgical techniques in the arthroscopic group; minor variations were also evidenced in the mini-arthrotomy group. Indeed, two studies avoid membrane fixation [17, 29], while three studies [17, 26, 34, 37] employed fibrin glue to fix the graft. In one study, in addition to the glue, the membrane was sutured to ensure stability [18]. In the mini-open group, one study [29] used a resorbable collagen I graft, while five [17, 18, 26, 34, 37] used a resorbable collagen I/III membrane. Other studies enhanced the membrane with chondrocyte spheroids (Chondrosphere) [35, 36, 38]. Concluding, variations were evident both in the arthroscopic and mini-arthrotomy groups, and represent the most important limitations of the present study. We were unable to identify studies that compare arthroscopy and mini-open with the same protocol of membrane choice and fixation. Overall, the analyses were limited to a restricted number of procedures, representing another important limitation. The surgical techniques presented some minimal differences between authors, and cell culture and expansion protocols were heterogeneous between studies. Hence, these results should be been interpreted within the limitations of the present investigation, opening new perspectives and challenges to future studies.
Conclusion
Arthroscopy and mini-open approaches for mACI in patients with chondral defects of the knee score were similar at midterm follow-up.
Availability of data and materials
The data underlying this article are available in the article and in its online supplementary material.
Abbreviations
- mACI:
-
Matrix-induced autologous chondrocyte implantation
- PROMs:
-
Patient-reported outcome measures
- RCT:
-
Randomized clinical trial
- BMI:
-
Body mass index
- IKDC:
-
Knee Documentation Committee
- MD:
-
Mean difference
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- pACI:
-
Periosteal-flap autologous chondrocyte implantation
References
Migliorini F, Berton A, Salvatore G, Candela V, Khan W, Longo UG et al (2020) Autologous chondrocyte implantation and mesenchymal stem cells for the treatments of chondral defects of the knee—a systematic review. Curr Stem Cell Res Ther. https://doi.org/10.2174/1574888X15666200221122834
Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M et al (2006) Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthr Cartil 14:1119–1125
Scillia AJ, Aune KT, Andrachuk JS, Cain EL, Dugas JR, Fleisig GS et al (2015) Return to play after chondroplasty of the knee in National Football League athletes. Am J Sports Med 43:663–668
Davila Castrodad IM, Mease SJ, Werheim E, McInerney VK, Scillia AJ (2020) Arthroscopic chondral defect repair with extracellular matrix scaffold and bone marrow aspirate concentrate. Arthrosc Tech 9:e1241–e1247
Atala A, Irvine DJ, Moses M, Shaunak S (2010) Wound healing versus regeneration: role of the tissue environment in regenerative medicine. MRS Bull. https://doi.org/10.1557/mrs2010.528
Buckwalter JA (2002) Articular cartilage injuries. Clin Orthop Relat Res 402:21–37
Robinson PG, Williamson T, Murray IR, Al-Hourani K, White TO (2020) Sporting participation following the operative management of chondral defects of the knee at mid-term follow up: a systematic review and meta-analysis. J Exp Orthop 7:76
Carey JL, Remmers AE, Flanigan DC (2020) Use of MACI (autologous cultured chondrocytes on porcine collagen membrane) in the United States: preliminary experience. Orthop J Sports Med 8:2325967120941816
Ebert JR, Robertson WB, Woodhouse J, Fallon M, Zheng MH, Ackland T et al (2011) Clinical and magnetic resonance imaging-based outcomes to 5 years after matrix-induced autologous chondrocyte implantation to address articular cartilage defects in the knee. Am J Sports Med 39:753–763
Gudas R, Kalesinskas RJ, Kimtys V, Stankevicius E, Toliusis V, Bernotavicius G et al (2005) A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy 21:1066–1075
Richter DL, Schenck RC Jr, Wascher DC, Treme G (2016) Knee articular cartilage repair and restoration techniques: a review of the literature. Sports Health 8:153–160
Bertho P, Pauvert A, Pouderoux T, Robert H, Orthopaedics and Traumatology Society of Western France (SOO) (2018) Treatment of large deep osteochondritis lesions of the knee by autologous matrix-induced chondrogenesis (AMIC): preliminary results in 13 patients. Orthop Traumatol Surg Res 104:695–700
Smith GD, Knutsen G, Richardson JB (2005) A clinical review of cartilage repair techniques. J Bone Joint Surg Br 87:445–449
Steinwachs MR, Guggi T, Kreuz PC (2008) Marrow stimulation techniques. Injury 39(Suppl 1):S26-31
Behrens P, Bitter T, Kurz B, Russlies M (2006) Matrix-associated autologous chondrocyte transplantation/implantation (MACT/MACI)—5-year follow-up. Knee 13:194–202
Bartlett W, Skinner JA, Gooding CR, Carrington RW, Flanagan AM, Briggs TW et al (2005) Autologous chondrocyte implantation versus matrix-induced autologous chondrocyte implantation for osteochondral defects of the knee: a prospective, randomised study. J Bone Joint Surg Br 87:640–645
Basad E, Ishaque B, Bachmann G, Sturz H, Steinmeyer J (2010) Matrix-induced autologous chondrocyte implantation versus microfracture in the treatment of cartilage defects of the knee: a 2-year randomised study. Knee Surg Sports Traumatol Arthrosc 18:519–527
Akgun I, Unlu MC, Erdal OA, Ogut T, Erturk M, Ovali E et al (2015) Matrix-induced autologous mesenchymal stem cell implantation versus matrix-induced autologous chondrocyte implantation in the treatment of chondral defects of the knee: a 2-year randomized study. Arch Orthop Trauma Surg 135:251–263
Nawaz SZ, Bentley G, Briggs TW, Carrington RW, Skinner JA, Gallagher KR et al (2014) Autologous chondrocyte implantation in the knee: mid-term to long-term results. J Bone Joint Surg Am 96:824–830
Hoburg A, Loer I, Korsmeier K, Siebold R, Niemeyer P, Fickert S et al (2019) Matrix-associated autologous chondrocyte implantation is an effective treatment at midterm follow-up in adolescents and young adults. Orthop J Sports Med 7:2325967119841077
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Howick J CI, Glasziou P, Greenhalgh T, Carl Heneghan, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M. The 2011 Oxford CEBM Levels of Evidence. Oxford Centre for Evidence-Based Medicine. 2011. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. Accessed Mar 2021
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 37:890–897
Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R et al (2007) Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine 74:594–599
Basad E, Wissing FR, Fehrenbach P, Rickert M, Steinmeyer J, Ishaque B (2015) Matrix-induced autologous chondrocyte implantation (MACI) in the knee: clinical outcomes and challenges. Knee Surg Sports Traumatol Arthrosc 23:3729–3735
Ebert JR, Fallon M, Ackland TR, Wood DJ, Janes GC (2012) Arthroscopic matrix-induced autologous chondrocyte implantation: 2-year outcomes. Arthroscopy 28(952–64):e1-2
Ebert JR, Fallon M, Wood DJ, Janes GC (2017) A prospective clinical and radiological evaluation at 5 years after arthroscopic matrix-induced autologous chondrocyte implantation. Am J Sports Med 45:59–69
Efe T, Theisen C, Fuchs-Winkelmann S, Stein T, Getgood A, Rominger MB et al (2012) Cell-free collagen type I matrix for repair of cartilage defects-clinical and magnetic resonance imaging results. Knee Surg Sports Traumatol Arthrosc 20:1915–1922
Ferruzzi A, Buda R, Faldini C, Vannini F, Di Caprio F, Luciani D et al (2008) Autologous chondrocyte implantation in the knee joint: open compared with arthroscopic technique. Comparison at a minimum follow-up of five years. J Bone Joint Surg Am 90(Suppl 4):90–101
Filardo G, Kon E, Di Martino A, Iacono F, Marcacci M (2011) Arthroscopic second-generation autologous chondrocyte implantation: a prospective 7-year follow-up study. Am J Sports Med 39:2153–2160
Filardo G, Kon E, Andriolo L, Di Matteo B, Balboni F, Marcacci M (2014) Clinical profiling in cartilage regeneration: prognostic factors for midterm results of matrix-assisted autologous chondrocyte transplantation. Am J Sports Med 42:898–905
Kon E, Filardo G, Condello V, Collarile M, Di Martino A, Zorzi C et al (2011) Second-generation autologous chondrocyte implantation: results in patients older than 40 years. Am J Sports Med 39:1668–1675
Marlovits S, Aldrian S, Wondrasch B, Zak L, Albrecht C, Welsch G et al (2012) Clinical and radiological outcomes 5 years after matrix-induced autologous chondrocyte implantation in patients with symptomatic, traumatic chondral defects. Am J Sports Med 40:2273–2280
Niemeyer P, Laute V, John T, Becher C, Diehl P, Kolombe T et al (2016) The effect of cell dose on the early magnetic resonance morphological outcomes of autologous cell implantation for articular cartilage defects in the knee: a randomized clinical trial. Am J Sports Med 44:2005–2014
Niemeyer P, Laute V, Zinser W, Becher C, Kolombe T, Fay J et al (2019) A Prospective, randomized, open-label, multicenter, phase III noninferiority trial to compare the clinical efficacy of matrix-associated autologous chondrocyte implantation with spheroid technology versus arthroscopic microfracture for cartilage defects of the knee. Orthop J Sports Med 7:2325967119854442
Saris D, Price A, Widuchowski W, Bertrand-Marchand M, Caron J, Drogset JO et al (2014) Matrix-applied characterized autologous cultured chondrocytes versus microfracture: two-year follow-up of a prospective randomized trial. Am J Sports Med 42:1384–1394
Siebold R, Suezer F, Schmitt B, Trattnig S, Essig M (2018) Good clinical and MRI outcome after arthroscopic autologous chondrocyte implantation for cartilage repair in the knee. Knee Surg Sports Traumatol Arthrosc 26:831–839
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331:889–895
Acknowledgements
None.
Funding
Open Access funding enabled and organized by Projekt DEAL. No external source of funding was used.
Author information
Authors and Affiliations
Contributions
FM: literature search, data extraction, methodological quality assessment, writing, final approval; FS: literature search, data extraction, methodological quality assessment, final approval; JE: supervision, final approval; MT: supervision, final approval; NM: revision, final approval. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Migliorini, F., Eschweiler, J., Spiezia, F. et al. Arthroscopy versus mini-arthrotomy approach for matrix-induced autologous chondrocyte implantation in the knee: a systematic review. J Orthop Traumatol 22, 23 (2021). https://doi.org/10.1186/s10195-021-00588-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-021-00588-6