Abstract
Over 30 years ago Weil and Shubin proposed a re-classification of shock states and identified hypovolemic, cardiogenic, obstructive and distributive shock. The first three categories have in common that they are associated with a fall in cardiac output. Distributive shock, such as occurs during sepsis and septic shock, however, is associated with an abnormal distribution of microvascular blood flow and metabolic distress in the presence of normal or even supranormal levels of cardiac output. This Bench-to-bedside review looks at the recent insights that have been gained into the nature of distributive shock. Its pathophysiology can best be described as a microcirculatory and mitochondrial distress syndrome, where time and therapy form an integral part of the definition. The clinical introduction of new microcirculatory imaging techniques, such as orthogonal polarization spectral and side-stream dark-field imaging, have allowed direct observation of the microcirculation at the bedside. Images of the sublingual microcirculation during septic shock and resuscitation have revealed that the distributive defect of blood flow occurs at the capillary level. In this paper, we classify the different types of heterogeneous flow patterns of microcirculatory abnormalities found during different types of distributive shock. Analysis of these patterns gave a five class classification system to define the types of microcirculatory abnormalities found in different types of distributive shock and indicated that distributive shock occurs in many other clinical conditions than just sepsis and septic shock. It is likely that different mechanisms defined by pathology and treatment underlie these abnormalities observed in the different classes. Functionally, however, they all cause a distributive defect resulting in microcirculatory shunting and regional dysoxia. It is hoped that this classification system will help in the identification of mechanisms underlying these abnormalities and indicate optimal therapies for resuscitating septic and other types of distributive shock.
Similar content being viewed by others
Introduction
Shock is the condition in which there is insufficient transport of blood carrying oxygen to meet the metabolic demand of the tissue cells. Weil and Shubin [1], in their classic work, classified four states of shock: hypovolemic (loss of intravascular volume), cardiogenic (impaired pump function), obstructive (of the heart, arteries or of the large veins) and distributive shock. They developed a conceptual framework to categorize these states, which gained wide acceptance probably due its clear pathophysiological substrate [2, 3]. The first three categories predictably result in a decrease in cardiac output leading to anaerobic tissue metabolism. However, distributive shock such as septic shock has been more difficult to characterize. This difficulty is primarily due to the fact that this type of shock results from heterogeneous alterations in tissue perfusion caused by microcirculatory dysfunction, resulting in an abnormal distribution of a normal or increased cardiac output [1]. The ensuing disparity between systemic and regional tissue oxygenation makes monitoring difficult and end-points in the treatment of distributive shock difficult to define [2].
Shunting of oxygen transport to the tissues is the main pathogenic feature of distributive shock [4]. It is characterized by hypoxemic shunted microcirculatory weak units, resulting in regional dysoxia. Although Weil and Shubin had already identified these concepts, the past decade has provided more insight into the nature of functional shunts and their relationship to impaired oxygen extraction in regional tissue during sepsis (for example, see [4–8]). The advent of new optical imaging techniques, such as orthogonal polarization spectral (OPS) and sidestream dark-field (SDF) imaging, now allows direct observation of the microcirculation at the bedside. These techniques are applied on organ surfaces and make use of optical modalities to filter out surface reflections of incident light when observations are made. Embodied in a hand-held type of microscope with image guides, these techniques allow direct observation of microcirculatory flow at the bedside when placed on organ surfaces. In critically ill patients, these techniques have been applied to the study of sublingual microcirculation and have revealed the central role of microcirculatory function in distributive shock [8–10].
This Bench-to-bedside review first briefly describes the different components and functions of the microcirculation in health and disease. The second part of the review discusses how OPS and SDF imaging have exposed microcirculatory abnormalities associated with distributive shock. A five class classification system is introduced for the different types of sublingual capillary flow abnormalities seen during various types of distributive shock.
The microcirculation as an oxygen distributing organ
The microcirculation can be regarded as a vital organ of the cardiovascular system whose function ensures the adequate delivery of oxygen by blood to the various tissue cells [11]. The entire organ is lined with endothelial cells surrounding the plasma and blood cells. A layer of glycocalyx covering the endothelial cells forms an important barrier and transduction system between the lumen of the capillaries and the endothelium and can be disrupted under conditions of inflammation and cardiovascular disease [12]. Smooth muscle cells can be found mainly around arterioles. A large number of cellular components complete the picture: platelets, coagulation factors, cytokines and chemokines. Apart from transporting nutrients and removing waste products, oxygen delivery is the prime function of this organ. The microcirculation is a complex network of resistance and exchange vessels, where perfusion is dependent on numerous factors. These include arterial oxygen saturation, oxygen consumption, blood viscosity, red and white blood cell deformability and flow, shunting of vessels, vasodilatation, vasoconstriction or stasis in arterioles and capillaries, diffusion constants of gasses and nutrients and distances from cells to the nearest blood vessel.
The endothelium is an important regulator of oxygen delivery. It responds to changes in blood flow as well as local stimuli. This results in upstream signaling that causes the smooth muscle of the feeding arterioles to dilate [13]. The physical properties of red blood cells, such as deformability and aggregability, play an important role in ensuring optimal perfusion of the microcirculation. Recent findings have shown that red blood cells not only transport oxygen, which is their main function, but can sense hypoxia and release vasodilator substances such as nitric oxide and ATP [14], indicating that red blood cells have an important role in regulating microcirculatory oxygenation. These mechanisms control highly heterogeneous flow patterns in the microcirculation but, through regulation, ensure homogenous oxygenation of the tissues [15]. Direct diffusion of oxygen from arterioles to other vessels with lower oxygen content, bypassing capillaries, contributes to this process [16]. New recent insights revealing oxygen pressure gradients between flowing red blood cells [17] and complex oxygen consumption by the vessel wall [18] indicate that oxygen transport kinetics at the capillary level are highly complex.
Marked differences in microcirculatory oxygen pressure (PO2) values can be found in different organs and their sub-compartments. For example, epicardial microcirculatory PO2 is high whereas that of the endocardium is lower [19]. In the gut, serosal PO2 is higher [5] than that of the mucosa. Similarly, in the kidney, the cortex PO2 is higher than that of the medulla under normal conditions [20–22].
The microcirculation in distributive shock
In sepsis, all the components of the microcirculation listed above are affected, causing a severe dysfunction in its regulatory function and resulting in a regional mismatch of oxygen supply and demand [4]. In summary, endothelial cells are less responsive to vasoactive agents, loose their anionic charge and normal glycocalyx, become leaky and give rise to massive over-expression of nitric oxide. Disturbed gap junctions disrupt intercellular endothelial communication and thus regulation [13]. Both red and white blood cell deformability is reduced, which may cause microvascular plugging. The interaction of white blood cells and endothelium represents the crossroads between inflammation and coagulation.
Numerous mediators facilitate intercellular communication and are responsible for white blood cell activation and the induction of a procoagulable state. The latter may give rise to disseminated intravascular coagulation, leading to diminished flow as a result of micro-thrombus formation.
Abnormalities in the nitric oxide system induced by inflammatory activation can be regarded as one of the key mechanisms responsible for the distributive defects associated with severe sepsis and septic shock. Indeed, various studies have shown hemodynamic stabilization after blocking the inflammatory up-regulation of inducible nitric oxide synthase (iNOS) expression (for example, [5]). Inhomogeneous expression of iNOS interferes with regional blood flow and promotes shunting from vulnerable weak microcirculatory units [23]. Inhomogenous expression of endothelial adhesion molecules, such as intercellular adhesion molecules and selectines, can also be expected to contribute to distributive alterations of blood flow through its effect on white blood cell kinetics [24].
Animal experiments have shown a reduction in perfused capillary density, stopped flow next to areas of hyperdynamic blood flow, resulting in increased heterogeneity in skeletal and intestinal microvascular beds, despite frequent normo-tensive conditions [6, 25]. An increased heterogeneity of the microcirculation was shown to provoke areas of hypoxia and generally impair oxygen extraction, both mathematically and in animal models of septic shock [5, 25, 26]. Microcirculatory PO2 measurements by palladium porphyrin phosphorescence revealed that, during various conditions of shock and resuscitation, microcirculatory PO2 levels become lower than venous PO2 levels, providing direct evidence for the action of functional shunting pathways [4, 5, 19, 27, 28]. Acidosis, hypocapnia and hypercapnia occurring during disease and therapy have been reported to have differential effects on the microcirculation, with acidosis in the presence of nitric oxide inhibition and hypocapnia causing arteriolar constriction, and hypercapnia resulting in venular dilation [29, 30].
Elevated mixed venous oxygen saturation and metabolic distress, such as occurs during distributive shock, indicates a deficit in oxygen extraction rate. This may be caused by either the oxygen not reaching the microcirculation (e.g., being shunted) [27] and/or that oxygen is not being utilized by the mitochondria of the tissue cells to perform oxidative phosphorylation [31]. The latter has been termed cytopathic hypoxia [32]. This entity, combined with observed microvascular derangements, led us to introduce the term 'microcirculatory and mitochondrial distress syndrome' (MMDS) to identify the compartments and pathophysiology of this condition [4]. The nature of MMDS in this definition is not only defined by the condition that led to shock, the co-morbidity present and the genetic profile of the patient, but also by the length of time the condition has persisted and the treatment regime that a patient has undergone.
Classifying microvascular flow abnormalities in shock
Many of the above insights into the microcirculatory mechanisms underlying distributive defects in sepsis have been obtained from animal experiments. Until recently, observations of microcirculatory hemodynamics in humans were limited to those of skin capillaries in patient nail folds using large microscopes. This changed with the introduction of OPS imaging [33]. It is an optical technique implemented in a hand-held microscope for visualizing the microcirculation on organ and mucous surfaces using polarized green light and cross-polarized images. We were instrumental in its introduction into the clinic in a surgical setting, which allowed the first observations of the microcirculation in the internal organs of humans [33, 34]. OPS imaging in healthy subjects shows capillaries equally distributed between the tissue cells, ensuring an adequate functional capillary density. One of the most striking findings of OPS imaging in disease is the pathological heterogeneity of microcirculatory flow. Some vascular beds show a preserved functional capillary density whereas others have a sluggish blood flow and some have no flow at all. Capillaries can be recruited and depleted of flow depending on intrinsic and extrinsic factors. When the flow ceases in the capillaries, cells that are close to the capillaries are suddenly far away from their source of oxygen and nutrients, as the diffusion distance of oxygen to the cell increases [6].
An improved optical modality in terms of technology and image quality called SDF imaging has recently been developed for viewing the microcirculation in patients [4, 35]. It uses light-emitting diodes (LEDs) placed around the tip of the light guide with a center core optically isolated from the outer ring (Fig. 1). When the light guide is placed on tissue surfaces, the light from the outer ring penetrates the tissue, illuminating the microcirculation from the interior. This dark-field illumination thus completely avoids reflections from the tissue surface. This imaging modality yields a clear image of microcirculatory components, with both flowing red and white blood cells. Due to its better image quality, SDF imaging has allowed semi-automated software to be applied in the analysis of the images.
Sidestream dark-field (SDF) imaging This imaging technique is an improved method of observing the human microcirculation at the bedside. SDF imaging consists of a light guide surrounded by green light-emitting diodes (LEDs; wavelength 530 nm) whose light penetrates the tissue and illuminates the microcirculation from within. The light is absorbed by hemoglobin of the red blood cells and scattered by leukocytes. A magnifying lens projects the image onto a video camera. Placed on organ surfaces, SDF imaging provides crisp images of the red blood cells and leukocytes flowing through the microcirculation. Reproduced with permission [1].
Over the past years, using these new techniques, the human microcirculation has been observed in a large variety of clinical settings both by us and others. Microcirculatory recordings have been made of virtually every type of shock.
In hypovolemic, cardiogenic and obstructive shock, microvascular changes are directly related to the limitation in cardiac output. In these conditions, a uniform discontinuity of microcirculatory blood flow in arterioles, capillaries and venules can be observed. All shock states in which the microcirculation was observed were associated with significant metabolic dysfunction (elevated lactate, tissue CO2, strong ion difference). This is in accordance with the findings that metabolic tissue distress, both in hemorrhagic as well as septic shock, is directly dependent on microcirculatory flow [36–38]. In distributive shock, the systemic hemodynamic profile is relatively normal while abnormal disturbed patterns of microcirculatory flow heterogeneity are seen [8, 9]. Over the years we have conducted many clinical microcirculatory observations in a wide range of disease states. These occurred during different types of surgery, infectious and cardiovascular diseases, hematological disorders and critical illness and showed that distributive shock, from a hemodynamic perspective, covers a much wider definition than just sepsis and septic shock. For example, activation of inflammatory pathways and circulatory dysfunction can be caused by cardiopulmonary bypass-pump circuits during cardiac surgery [39], a condition which should also be regarded as distributive shock. Similar conditions can also occur during inflammatory activation during reperfusion injury [40]. Although the main features of normal hemo-dynamics, inflammation and metabolic distress are common in these different types of distributive shock, the microcirculatory distributive alterations observed by OPS/SDF imaging showed differences in capillary flow patterns under different conditions. To differentiate between the types of flow abnormalities and focusing on sublingual microcirculation due to its clinical accessibility, we clustered similar abnormalities together to establish a classification system that allows a more precise definition of underlying pathologies during different clinical conditions.
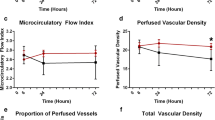
At the microcirculatory level, all classes of abnormalities seen during distributive shock show normal to hyperdynamic venular flow [8, 9]. It is at the capillary level that the distributive defect is seen, with heterogeneous perfused capillaries resulting in the shunting of areas of the microcirculation. Although the classes of capillary abnormalities we identified may be caused by different mechanisms, they all have in common a distributive defect caused by functional shunting of capillaries in the presence of normal or hyperdynamic venular flow. This is also why we did not make a distinction between stagnant and stopped flow, as both of these result in functional shunting. Since microcirculatory abnormalities are mainly characterized by a heterogeneous pattern of flow, we summarized the abnormalities per class in two main types of capillary flow patterns. This is shown in cartoon form in Figure 2 as two capillaries below each other, each with different flow patterns. Venules are depicted as a single large curved vessel over the capillaries (Fig. 2). In this way, we identified five classes of sublingual capillary flow abnormalities (Fig. 2). A Class I abnormality is defined by all capillaries being stagnant in the presence of normal or sluggish venular flow (Fig. 3). It is a condition that can be found in pressure resuscitated septic patients where pressors have been used excessively to normalize blood pressure [8, 9]. Class II microcirculatory flow abnormalities are defined by empty capillaries next to capillaries with flowing red blood cells. This decrease of capillary density makes the diffusion distance between red blood cells in the remaining capillaries and the tissue cells larger, leading to regional hypoxia [6]. The red blood cells in the remaining capillaries show a high microcirculatory hemoglobin saturation, indicating poor oxygen off-loading associated with the reduction in capillary exchange surface area [41]. Class II abnormalities were most frequently found during use of extracorporeal circuits in coronary artery bypass grafting (CABG) surgery and extracorporeal membrane oxygenation (ECMO). Class III abnormalities are described by capillaries with stagnant blood cells next to capillaries with normal flow. These abnormalities were most frequently observed in sickle cell patients and critically ill malaria patients, but also in septic patients. In critically ill malaria patients, who are often in a coma, strikingly normal hemodynamics are seen in the presence of high lactate levels. This feature, together with class III microcirculatory abnormalities, also identifies this condition as distributive shock. Class IV abnormalities show hyperdynamic flow patterns in some capillaries next to capillaries with stagnant cells (Fig. 3). Venules in such cases frequently also show a hyperdynamic flow profile. This condition is seen in resuscitated hyperdynamic septic patients. Class V abnormalities describe the condition where hyperdynamic flow is seen at all levels of the microcirculation. Blood cells usually travel so fast that individual cells can not be distinguished from each other. Metabolic distress seen under such conditions could be the result of cells moving too fast to off-load their oxygen, or, that they may originate from other organs or compartments being shunted [28]. Interestingly, the class V types of abnormality are also observed in extreme exercise. The pathogenic nature of class V abnormalities in septic patients remains to be determined. In Table 1, the diseases observed so far are listed next to the different classes of microcirculatory abnormalities seen in Figure 2. They are by no means complete and it is hoped that this list will continue to expand as more insight is obtained into the nature of distributive alterations. Scoring systems developed to quantify such images should greatly aid this process [42]. Examples of OPS/SDF movies of each class of abnormality can be viewed on our web site [43].
A classification system for categorizing sublingual microcirculatory flow abnormalities seen in distributive shock as observed by OPS/sidestream dark-field imaging. Each class consists of a venule with two capillaries. In this way, the heterogeneity of the capillary flow is described by showing the two most characteristic types of flow seen. Solid arrows depict normal flow whereas the striped arrows represent hyperdynamic flow. No arrow depicts stagnant flow (examples of real-time films of each class of abnormality can be downloaded from our web site [43]).
Examples of sidestream dark-field images of sublingual microcirculation from septic patients with distributive shock. (a) Image taken from a resuscitated septic patient with a class I type of microcirculatory abnormality, complete stasis in the capillaries. (b) An example of a patient with class IV abnormalities with some capillaries showing stasis and others showing high flow. (c) Image of a healthy volunteer with microcirculatory flow in all vessels.
The complex interaction of pathology and treatment define the abnormalities seen at the microcirculatory level in distributive shock. From this perspective, it can be expected that the different classes of microcirculatry abnormalities shown in Figure 2 are caused by a combination of different regional pathogenic mechanisms while having a similar systemic hemodynamics profile. Several pathogenic mechanisms associated with disease and therapy could be considered in this context. Normalizing arterial pressure by excessive use of pressor agents, for example, will cause a rise in arterial pressure but at the cost of microcirculatory flow [44]. Such a condition can underlie the class I type of distributive abnormality. Hyperoxia, as applied during the treatment of sepsis with high levels of inspired oxygen, or during cardiopulmonary bypass in CABG surgery, can lead to arteriolar constriction, causing a reduction in functional capillary density and distributive microcirculatory alterations [45]. Hemodilution, applied in various clinical scenarios, causes a decrease in blood viscosity, altered red blood cell rigidity and functional shunting of the microcirculation [28]. The reduced blood viscosity results in a reduction in longitudinal capillary pressure gradient due to reduced resistance of the blood and can result in a fall out of capillary flow. This condition could lead to class II abnormalities. Hemorheological alterations occurring during sepsis and infectious diseases such as malaria [46, 47] are caused by increased red and white blood cell aggregability and rigidity, which can result in the obstruction of capillary blood flow, resulting in class I, III or IV abnormalities. Heterogenous iNOS expression and excessive production of nitric oxide, causing regional vasodilation and an increase in microcirculatory driving pressure, could result in the hyperdynamic images described by class IV and V types of abnormalities. The heterogeneous expression of iNOS in the various organs could explain why, in the presence of similar systemic hemo-dynamic profiles, regional variation in class V abnormalities might persist [23]. From the above considerations, it can be concluded that a combination of the described pathogenic mechanisms associated with disease and therapy can result in the various microcirculatory abnormalities described in Figure 2. Different types of microcirculatory abnormalities could persist in different organ systems, depending on the action of regional pathogenic mechanisms and regional response to applied therapies. Future research using microcirculatory monitoring techniques should identify which disease state combined with which type of therapy underlies these abnormalities. These insights could then identify which microcirculatory recruitment maneuvers are most appropriate for improving organ function in distributive shock.
Resuscitating microcirculatory defects underlying distributive shock
Microcirculation recruitment maneuvers may be able to correct the observed abnormalities [23]. They can be regarded as a two step approach. First, the microcirculation should be opened and kept open. This implies the need for fluids, inotropics, vasodilators and restricted use of vaso-pressors. Second, pathological flow heterogeneity and microvascular shunting should be corrected. This demands control of inflammation, vascular function and coagulation [4]. In this respect, it is important to realize that MMDS and its distributive alterations are not static entities but evolve in time in active interaction with therapy and disease.
The manner in which therapy can improve systemic variables, while leaving the microcirculation unaffected, was shown in an early study by LeDoux and co-workers in septic patients [48]. That therapy can actually impair the microcirculation and affect outcome was reported by Boerma and co-workers in a case study in a septic shock patient receiving the vasopressin analog terlipressin [49]. Here it was found that while this compound was effective in improving hemodynamics and urine output, it resulted in microcirculatory flow stasis and a deterioration of the patient. The finding that vasopressin, in a similar setting of distributive shock, had no such effect on the microcirculation while improving systemic hemodynamics underscores the need to monitor individual cases [50].
Application of microcirculatory recruitment maneuver procedures has been shown to be effective in promoting microcirculatory blood flow and correct metabolic distress in clinical studies using OPS/SDF imaging (for example, [37, 38]). Fluids in combination with nitroglycerine therapy were shown to recruit disturbed microcirculation following pressure guided resuscitation in septic shock patients, suggesting a role for vasodilator therapy in the treatment of sepsis [9, 51]. De Backer and colleagues had also shown that such disturbed microcirculation can be recruited by topical application of acetylcholine [8]. Support of pump function by dobutamine therapy has been shown to improve microcirculatory flow independent of improvement of global hemo-dynamic parameters [52]. Correction of endothelial function and coagulatory abnormalities by activated protein C has been recently shown to recruit microcirculatory function during septic shock [53]. Recently, Spronk and co-workers [37] reported a case study where thrombolysis therapy using a recombinant tissue plasminogen activator in fulminant purpura was effective in recruiting sublingual microcirculation and normalizing sublingual capnography. Thus, it is clear that therapies are available that are effective in recruiting the microcirculation. Although persistent microcirculatory abnormalities have a very bad prognosis [54] and need to be corrected, the efficacy of such microcirculatory recruitment procedures in affecting outcome still has to be determined in controlled trial settings. The availability of microcirculatory imaging technologies and effective scoring methods will greatly aid in answering these questions.
Conclusion
It is now clear that optimizing global hemodynamic and oxygen derived parameters in patients in shock does not necessarily resuscitate the microcirculation. As this is the organ that is ultimately responsible for oxygen delivery to tissue, it seems sensible to monitor this organ and, if necessary, improve its function.
Observing the microcirculation in different shock states shows equally different flow patterns. These depend on the pathophysiology of the disease, its time course and the instituted therapy. The number of affected microcirculatory components and the severity of their disturbance are set by these three factors, which will ultimately determine what we see when recording dynamic images.
The now commonplace classic shock classification based on global hemodynamics is invaluable in optimizing systemic circulation and oxygen delivery. However, microvascular resuscitation could become an adjunct to early goal directed therapy in shock states. Our proposed reclassification system may be a basis for identifying different types of microcirculatory abnormalities and possibly provide a guide for therapeutic interventions.
Abbreviations
- CABG:
-
= coronary artery bypass grafting
- ECMO:
-
= extracorporeal membrane oxygenation
- iNOS:
-
= inducible nitric oxide synthase
- MMDS:
-
= microcirculatory and mitochondrial distress syndrome
- OPS:
-
= orthogonal polarization spectral
- PO2:
-
= oxygen pressure
- SDF:
-
= sidestream dark-field.
References
Weil MH, Shubin H: Proposed reclassification of shock states with special reference to distributive defects. Adv Exp Med Biol 1971, 23: 13-23.
Vincent JL: Hemodynamic support in septic shock. Intensive Care Med 2001,27(Suppl 1):S80-92. 10.1007/PL00003799
Pinsky MR, Payen D: Functional hemodynamic monitoring. Crit Care 2005, 9: 566-572. 10.1186/cc3927
Ince C: The microcirculation is the motor of sepsis. Crit Care 2005,9(Suppl 4):S13-19. 10.1186/cc3753
Siegemund M, van Bommel J, Schwarte LA, Studer W, Girard T, Marsch S, Radermacher P, Ince C: Inducible nitric oxide synthase inhibition improves intestinal microcirculatory oxygenation and CO2 balance during endotoxemia in pigs. Intensive Care Med 2005, 31: 985-992. 10.1007/s00134-005-2664-7
Ellis CG, Bateman RM, Sharpe MD, Sibbald WJ, Gill R: Effect of a maldistribution of microvascular blood flow on capillary O(2) extraction in sepsis. Am J Physiol Heart Circ Physiol 2002, 282: H156-164.
Ellis CG, Jagger J, Sharpe M: The microcirculation as a functional system. Crit Care 2005,9(Suppl 4):S3-8. 10.1186/cc3751
De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL: Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med 2002, 166: 98-104. 10.1164/rccm.200109-016OC
Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemansvan Straaten HM, Zandstra DF: Nitroglycerin in septic shock after intravascular volume resuscitation. Lancet 2002, 360: 1395-1396. 10.1016/S0140-6736(02)11393-6
Trzeciak S, Rivers EP: Clinical manifestations of disordered microcirculatory perfusion in severe sepsis. Crit Care 2005,9(Suppl 4):S20-S26. 10.1186/cc3744
Segal SS: Regulation of blood flow in the microcirculation. Microcirculation 2005, 12: 33-45.
Nieuwdorp M, Mooij HL, Kroon J, Atasever B, Spaan JA, Ince C, Holleman F, Diamant M, Heine RJ, Hoekstra JB, et al.: Endothelial glycocalyx damage coincides with microalbuminuria in type 1 diabetes. Diabetes 2006, 55: 1127-1132. 10.2337/diabetes.55.04.06.db05-1619
Lidington D, Tyml K, Ouellette Y: Lipopolysaccharide-induced reductions in cellular coupling correlate with tyrosine phosphorylation of connexin. J Cell Physiol 2002, 193: 373-379. 10.1002/jcp.10179
Cosby K, Partovi KS, Crawford JH, Patel RP, Reiter CD, Martyr S, Yang BK, Waclawiw MA, Zalos G, Xu X, et al.: Nitrite reduction to nitric oxide by deoxyhemoglobin vasodilates the human circulation. Nat Med 2003, 9: 1460-1461. 10.1038/nm954
Shonat RD, Johnson PC: Oxygen tension gradients and heterogeneity in venous microcirculation: a phosphorescence quenching study. Am J Physiol 1997, 272: H2233-H2240.
Ellsworth ML, Pittman RN: Arterioles supply oxygen to capillaries by diffusion as well as by convection. Am J Physiol 1990, 258: H1240-1243.
Golub AS, Pittman RN: Erythrocyte-associated transients in PO2 revealed in capillaries of rat mesentery. Am J Physiol Heart Circ Physiol 2005, 288: H2735-2743. 10.1152/ajpheart.00711.2004
Cabrales P, Tsai AG, Johnson PC, Intaglietta M: Oxygen release from arterioles with normal flow and no-flow conditions. J Appl Physiol 2006, 100: 1569-1576. 10.1152/japplphysiol.00762.2005
Zuurbier CJ, van Iterson M, Ince C: Functional heterogeneity of oxygen supply consumption ratio in the heart. Cardiovasc Res 1999, 44: 488-497. 10.1016/S0008-6363(99)00231-X
Liss P, Nygren A, Revsbech NP, Ulfendahl HR: Intrarenal oxygen tension measured by a modified clark electrode at normal and low blood pressure and after injection of x-ray contrast media. Pflugers Arch 1997, 434: 705-711. 10.1007/s004240050455
Brezis M, Heyman SN, Epstein FH: Determinants of intrarenal oxygenation.II. Hemodynamic effects. Am J Physiol 1994, 267: F1063-F1068.
Johannes T, Mik EG, Nohé B, Raat RJ, Unertl KE, Ince C: Influence of fluid resuscitation on renal microvascular PO2 in a normotensive rat model of endotoxemia. Crit Care 2006, 10: R88. 10.1186/cc4948
Almac E, Siegemund M, Demirci C, Ince C: Microcirculatory recruitment maneuvers improves tissue CO2 abnormalities in sepsis. Minerva Anestesiol 2006, 72: 507-519.
Muller AM, Cronen C, Muller KM, Kirkpatrick CJ: Heterogeneous expression of cell adhesion molecules by endothelial cells in ARDS. J Pathol 2002, 198: 270-275. 10.1002/path.1186
Nakajima Y, Baudry N, Duranteau J, Vicaut E: Microcirculation in intestinal villi: a comparison between hemorrhagic and endotoxin shock. Am J Respir Crit Care Med 2001, 164: 1526-1530.
Humer MF, Phang PT, Friesen BP, Allard MF, Goddard CM, Walley KR: Heterogeneity of gut capillary transit times and impaired gut oxygen extraction in endotoxemic pigs. J Appl Physiol 1996, 81: 895-904.
Ince C, Sinaasappel M: Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med 1999, 27: 1369-1377. 10.1097/00003246-199907000-00031
Schwarte LA, Fournell A, van Bommel J, Ince C: Redistribution of intestinal microcirculatory oxygenation during acute hemodilution in pigs. J Appl Physiol 2005, 98: 1070-1075. 10.1152/japplphysiol.00861.2004
Yamaguchi K, Suzuki K, Naoki K, Nishio K, Sato N, Takeshita K, Kudo H, Aoki T, Suzuki Y, Miyata A, Tsumura H: Response of intra-acinar pulmonary microvessels to hypoxia, hypercapnic. Circ Res 1998, 82: 722-728.
Pennings F, Bouma GJ, Ince C: Direct observation of the human cerebral microcirculation during aneurysm surgery reveals increased arteriolar contractility. Stroke 2004, 35: 1284-1288. 10.1161/01.STR.0000126039.91400.cb
Brealey D, Brand M, Hargreaves I, Heales S, Land J, Smolenski R, Davies NA, Cooper CE, Singer M: Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet 2002, 360: 219-223. 10.1016/S0140-6736(02)09459-X
Fink MP: Bench-to-bedside review: Cytopathic hypoxia. Crit Care 2002, 6: 491-499. 10.1186/cc1824
Groner W, Winkelman JW, Harris AG, Ince C, Bouma GJ, Messmer K, Nadeau RG: Orthogonal polarization spectral imaging: a new method for study of the microcirculation. Nat Med 1999, 5: 1209-1212. 10.1038/13529
Mathura KR, Bouma GJ, Ince C: Abnormal microcirculation in brain tumours during surgery. Lancet 2001, 358: 1698-1699. 10.1016/S0140-6736(01)06722-8
Ince C: Sidestream dark field (SDF) imaging: an improved technique to observe sublingual microcirculation. Crit Care 2005,8(Suppl 1):P72. 10.1186/cc3135
Fries M, Weil MH, Sun S, Huang L, Fang X, Cammarata G, Castillo C, Tang W: Increases in tissue PCO 2 during circulatory shock reflect selective decreases in capillary blood flow. Crit Care Med 2006, 34: 446-452. 10.1097/01.CCM.0000196205.23674.23
Spronk PE, Rommes JH, Schaar C, Ince C: Thrombolysis in fulminant purpura: observations on changes in microcirculatory perfusion during successful treatment. Thromb Haemost 2006, 95: 576-578.
Creteur J, De Backer D, Sakr Y, Koch M, Vincent J: Sublingual capnometry tracks microcirculatory changes in septic patients. Intensive Care Med 2006, 32: 516-523. 10.1007/s00134-006-0070-4
Wan S, LeClerc JL, Vincent JL: Inflammatory response to cardiopulmonary bypass: mechanisms involved and possible therapeutic strategies. Chest 1997, 112: 676-692.
Siegemund M, Stegenga ME, Mathura k, van Bommel J, Ince C: Changes in the porcine microcirculation of the ileum after supra-mesenteric aortic cross-clamping. Intensive Care Med 1999,25(Suppl 1):S10.
Atasever B, Goedhart P, de Mol B, Ince C: Sublingual spectrophotometry: a new method for continuous monitoring of microcirculatory hemoglobin concentration and oxygen saturation during extracorporeal circulation in heart surgery. Nether J Crit Care 2004, 8: 22. 10.1186/cc2489
Boerma EC, Mathura KR, van der Voort PH, Spronk PE, Ince C: Quantifying bedside-derived imaging of microcirculatory abnormalities in septic patients: a prospective validation study. Crit Care 2005, 9: R601-606. 10.1186/cc3809
SDF and OPS Imaging[http://www.sdfimaging.net]
Taylor AE, Moore TM: Capillary fluid exchange. Am J Physiol (Ad Physiol Edu 22) 1999, 277: S203-S210.
Tsai AG, Cabrales P, Winslow RM, Intaglietta M: Microvascular oxygen distribution in awake hamster window chamber model during hyperoxia. Am J Physiol 2003, 285: H1537-1545.
Baskurt OK, Temiz A, Meiselman HJ: Red blood cell aggregation in experimental sepsis. J Lab Clin Med 1997, 130: 183-190. 10.1016/S0022-2143(97)90094-9
Dondorp AM, Angus BJ, Chotivanich K, Silamut K, Ruangveerayuth R, Hardeman MR, Kager PA, Vreeken J, White NJ: Red cell deformability as a predictor of anemia in severe falciparum malaria. Am J Trop Med Hyg 1999, 60: 733-737.
LeDoux D, Astiz ME, Carpati CM, Rackow : Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med 2000, 28: 2729-2732. 10.1097/00003246-200008000-00007
Boerma EC, van der Voort PH, Ince C: Sublingual microcirculatory flow is impaired by the vasopressin-analogue terlipressin in a patient with catecholamine-resistant septic shock. Acta Anaesthesiol Scand 2005, 49: 1387-1390. 10.1111/j.1399-6576.2005.00752.x
Dubois MJ, De Backer D, Creteur J, Anane S, Vincent JL: Effect of vasopressin on sublingual microcirculation in a patient with distributive shock. Intensive Care Med 2003, 29: 1020-1023.
Buwalda M, Ince C: Opening the microcirculation: can vasodilators be useful in sepsis? Intensive Care Med 2002, 28: 1208-1217. 10.1007/s00134-002-1407-2
De Backer D, Creteur J, Preiser J, Dubois M, Sakr Y, Koch M, Verdant C, Vincent J: The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit Care Med 2006, 34: 403-408. 10.1097/01.CCM.0000198107.61493.5A
De Backer D, Verdant C, Chierego M, Koch M, Gullo A, Vincent JL: Effects of drotrecogin alfa activated on microcirculatory alterations in patients with severe sepsis. Crit Care Med 2006, 34: 1918-1924. 10.1097/01.CCM.0000220498.48773.3C
Sakr Y, Dubois MJ, De Backer D, Creteur J, Vincent JL: Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med 2004, 32: 1825-1831. 10.1097/01.CCM.0000138558.16257.3F
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
CI is Chief Scientific Officer of Microvision Medical, an Academic Medical Center based company dedicated to the production of devices for microcirculatory imaging.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Elbers, P.W., Ince, C. Bench-to-bedside review: Mechanisms of critical illness – classifying microcirculatory flow abnormalities in distributive shock. Crit Care 10, 221 (2006). https://doi.org/10.1186/cc4969
Published:
DOI: https://doi.org/10.1186/cc4969