Abstract
Introduction
In this review, we compare the spectrum of currently availablemethods for quantifying pulmonary edema in patients.
Review
Imaging and indicator dilution techniques comprise the most commonstrategies for measuring lung water at the bedside. The most accurate (within10% of the gravimetric gold standard) and most reproducible (< 5%between-test variation) are also, unfortunately, the most expensive and mostdifficult to implement for purposes of large-scale clinical trials or forroutine clinical practice.
Conclusion
The standard chest radiograph remains the best screening test forthe detection of pulmonary edema. Indicator-dilution techniques are probablythe best available method at present for quantitation in patient groups.
Similar content being viewed by others
Introduction
Although about 80% of the lung is made up of water, gas-exchanging air spaces are protected by various barriers and drains. In multiple disease states, through injury or pressure (or both), these protective mechanisms fail, resulting in the abnormal accumulation of extravascular lung water (EVLW). The principle paradigm describing fluid flux in the lung is the 'Starling equation', which can be modified to account for the total surface area over which filtration might occur. 'Lymph flow' is a term summarizing those mechanisms responsible for returning extravasated fluid to the vascular compartment:
EVLW=(Lp ×S) [(Pc-Pi)- σ (Πc-Πi)]-lymph flow [1]
where EVLW=extravascular lung water (ml), Lp = the hydraulic conductivity for water (cm/min/mmHg), S = surface area (cm2), Pc and Pi = the hydrostatic pressure within the capillary and interstitial spaces respectively (mmHg), σ = the reflection coefficient for protein (no units), and Πc and Πi = the oncotic pressure within the capillary and interstitial spaces (mmHg).
This equation describes the formation of interstitial edema accommodated by the interstitium. Subsequent movement of fluid into the air spaces develops by a more rapid process, termed alveolar flooding [2,3]. Normally EVLW is < 500 ml [4,5,6,7]. With alveolar flooding, lung water content is usually > 75-100% above normal [8]. It is at this point that physiologic impairment usually occurs. Thus, any method that would be clinically useful must be able to detect changes in EVLW below the threshold of alveolar edema.
Although outcome has never been shown to be linked directly to the amount, or even continued presence, of pulmonary edema per se, the possibility that sufficiently sensitive and accurate techniques could be used to detect pulmonary edema even before it becomes apparent clinically, or could be used to provide information about the natural history of pulmonary edema or its response to therapeutic intervention, is so inherently attractive that the effort to develop and validate such techniques still continues.
The ideal test should be accurate, sensitive, reproducible, non-invasive, practical and inexpensive [9]. There is no single ideal clinical test. Experimentally, EVLW can be evaluated and measured by histologic or gravimetric methods [10]. This comparative review focuses attention specifically on those methods, which can be clinically applied.
Imaging methods
General comments
Common to all imaging methods is spatial information and physical volume. Each picture (pixel) or volume (voxel) element in a cross-sectional image of the lungs represents a specific physical volume. Thus, the units for a variable within that element are those of concentration (e.g. ml EVLW/ml lung). Since the lung is an air containing structure, the amount of lung parenchyma within each voxel can change, depending on the underlying state of lung inflation (lung volume). To quantify changes in images of EVLW in absolute terms, the signal over the entire organ must be integrated.
Most imaging methods (except positron emission tomography; PET) for evaluating pulmonary edema (Table 1) do not estimate EVLW per se, but instead produce estimates of total water content or concentration (i.e. vascular + extravascular water). The data from such methods can be misinterpreted if the blood volume of the lungs is not constant. Although spatially specific to varying degrees, no modality can resolve composition of edema on density alone since the edema, blood and inflammatory white cells are virtually identical, leading in general to an overestimation of EVLW per se. Certainly no modality can differentiate between intra- and extracellular water.
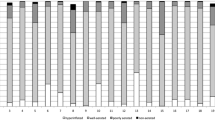
Chest radiography
A chest roentgenogram is commonly used to detect whether or not pulmonary edema is present, to describe its overall distribution within the lung, and to evaluate associated findings to infer a probable etiology. It can also be used, at least semi-quantitatively, to estimate the amount of pulmonary edema that is present as well. Several features of the chest radiograph make such an interpretation possible: (1) certain characteristic 'signs' are associated with only modest increases in EVLW (perhaps as little as 30% above normal values) [11] such as pulmonary 'congestion', vascular 'redistribution', peribronchial cuffing, perihilar 'haze', Kerley's lines, and an 'interstitial' pattern to the radiographic densities; (2) as EVLW increases, the radiographic densities occupy a greater fraction of the total lung airspace (often, mild-to-moderate amounts of edema are present in gravity-dependent lung regions only, while more severe increases in EVLW involve both dependent and non-dependent lung) [12]; and (3) as edema worsens and water displaces air in any given lung region, the 'density' of the 'infiltrate' also worsens, becoming more and more 'white'.
Although relatively quantitative and potentially informative as to etiology, accuracy (the amount of EVLW present) is significantly limited by acquisition techniques and clinical issues that override standardization procedures [13,14] (especially in the critically ill). Under clinically relevant conditions, the correlation of EVLW by chest radiography to other established techniques has been weak [15].
Computed tomography
The principle advantages of using X-ray computed tomography (CT) over conventional radiography are that the density of the infiltrates can be determined quantitatively, the spatial distribution of edema in transverse sections can be defined, and, of course, associated (and at times clinically relevant) findings can be identified. Lung density can be quantified with X-ray CT because the arbitrary Hounsfield units used for CT display can be calibrated against objects or substances of known density. Experimentally, CT-derived estimates of lung density increase by 69% when gravimetric measurements of lung weight increase by about 250% [16] (this difference in the percentage increase does not really indicate anything about accuracy since the units of measurement are not the same). CT densitometry is able to detect rather modest (~50%) increases in EVLW in experimental animals [17]. Obviously, it is not portable and involves exposure to ionizing radiation.
Nuclear magnetic resonance (NMR) imaging
Another emerging approach to estimating lung water content is based on the ability to align hydrogen nuclei (protons) of water in the direction of an externally applied magnetic field [18]. When a subject lays within a magnetic field and is then irradiated with electromagnetic radiation in the form of a correctly applied radiofrequency pulse, 'resonance' (i.e. 'nuclear magnetic resonance') develops from the absorption and subsequent release of energy as the pulse is applied and discontinued. This energy can be detected with appropriately placed amplifiers, producing a signal of varying strength, depending on the strength of the magnetic field and the frequency of the radiofrequency pulse. The spin-echo sequence is the only one to date that has been employed to measure lung water.
Signal intensity, detected after a spin-echo pulse sequence, varies as a function of the time it is sampled once the 90° radiofrequency pulse is stopped (the 'relaxation' time). Generally, proton density images have been obtained with pulse sequences that minimize the effects of both T1 and T2 weighting. Including a negative vascular contrast material(coated magnetite) into the imaging protocol allows the measurement EVLW [19] (studies on rats only).
Repeated measures of lung water by NMR vary by about 5-10% [20]. Numerous studies have reported a good correlation between NMR-determined estimates of lung water and estimates from the gold-standard gravimetric method [21,22,23,24,25,26]. A problem intrinsic to NMR imaging is that normal or mildly edematous lung produces relatively little signal using conventional spin-echo sequences on 1.5 Tesla imagers typically used for clinical purposes [18,25]. As a result, NMR methods can underestimate true lung water in absolute terms by as much as 20-40% [20,27,28] (despite the good correlation with gravimetric methods). This loss of signal is due to artifacts caused by the distinct and separate magnetic susceptibilities of both air and soft-tissue in the normally inflated lung. These artifacts, and therefore the loss of signal, are magnified by the strength of the external magnetic field. Recently, an imager that has only one-tenth the strength of most clinical scanners has been used along with a multi-echo pulse sequence (i.e. a 90° radiofrequency pulse followed by multiple 180° pulses) to minimize the effect of the air-soft-tissue artifact, resulting in an excellent correlation, even in absolute terms, between NMR and gravimetrically determined lung water[29]. This same NMR imaging sequence has also been successfully applied to normal volunteers [29].
T1 and T2 vary according to the type of tissue being examined, raising the theoretical possibility that NMR imaging could be used to identify differences in the composition of pulmonary edema generated by high intravascular pressures (low protein) as opposed to increased vascular permeability (high protein), potentially allowing the edema of heart failure to be distinguished non-invasively from the edema of acute respiratory distress syndrome (ARDS). These distinctions have been made (in rats) with the use of a 40000 Dalton contrast material [30].
Cutillo et al. [31] have actually reported a method of NMR image analysis that takes advantage of the same signal loss artifact (the one caused by the air-soft-tissue interface) that confounds the measurement of proton density in absolute terms (and therefore of lung water) in the normally inflated lung. Since the air-soft-tissue interface is minimized as alveolar edema develops, the expected loss of signal is reduced. This difference in signal loss can be measured, leading to inferences about the location of the developing edema (alveolar edema causing less loss of signal than interstitial edema). To date, however, the method has only been applied to studies in rats [31].
In summary, the technique of NMR imaging continues to be developed as a quantitative tool to measure and monitor the development of pulmonary edema. An important advantage of using NMR to evaluate lung water is that the measurements can be obtained without any need for ionizing radiation. It is expensive, however, and even once the technical hurdles including respiratory and cardiac motion are overcome, considerable difficulty will undoubtedly be encountered when trying to implement such methods in the critically ill patient.
Positron emission tomography
Lung water can be measured by external residue detection techniques, after separately administering radioactively labeled tracers that distribute within the total and intravascular water spaces of the lung. Emissions are then detected with a device such as a gamma camera or a PET scanner. PET is widely held to be the gold standard for measuring EVLW (amongst the nuclear medicine techniques) because a tomographic image can then be created and normalized for the attenuation of the structure being imaged using a transmission (sometimes referred to as an attenuation) scan [32].
Lung water content can be measured either directly, or estimated from tissue density measurements [32,33]. With this approach, the water fraction of lung tissue must be assumed (0.82-0.84 ml/g). A small (~2%) correction for differences in tissue versus blood density can also be incorporated [34].
When lung water (instead of lung density) is measured directly, a sample of sterile water is labeled with a positron-emitting isotope, such as oxygen-15 (H215O) (half-life = 2.06 min), and then administered intravenously. The O-15 labeled water is allowed to equilibrate within tissue water over a 3-4 min period (this makes inaccuracies from areas of hypoperfusion less significant), and the isotope's activity concentration in lung tissue is then determined. If the activity data in the PET image are scaled to simultaneously obtained activity in the blood, the image can be displayed as a quantitative regional map of lung water distribution [35].
An analogous approach is used to measure the blood volume concentration in the images. In this case, O-15 (or, alternatively, C-11) labeled carbon monoxide is used instead of O-15 water. If O-15 carbon monoxide is used, trace amounts of C15O are inhaled as a gas, binding immediately to blood hemoglobin. After a few minutes, to allow equilibration within the body's blood volume, another PET scan is obtained. When again normalized to activity measurements in blood and corrected for attenuation, the image is a regional display of blood volume. An alternative to using peripheral blood samples is to measure the activity within the blood pool of a cardiac chamber. In this case, a further correction is necessary for the so-called 'partial volume averaging effect' (~5-10% in humans), which occurs as a result of the limited spatial resolution of PET relative to the size of the ventricular chamber [34]. With the assumption that 84% of blood is water (a reasonable assumption at normal hematocrits), the blood water content in a lung region can be subtracted from the total lung water concentration, yielding a derived image of extravascular water concentration [36]. The total time required to measure EVLW with PET is about 45min, but repeat measurements can begin in as little as 10-15min from the previous one.
Two previous studies showed that EVLW measurements by PET correlated well with EVLW measurements obtained by gravimetrics (r = 0.86-0.93), even though corrections for potential differences in peripheral versus capillary hematocrit, or for differences in tissue versus blood density were not included [36,37]. Perhaps because such corrections were not incorporated, PET estimates of EVLW systematically underestimated the gravimetric estimates by about 10-15%. PET measurements, however, are highly reproducible (coefficient of variation for repeat measurements < 5%) and linear (r = 0.99 for changes in lung water over a 20-fold concentration range) [37]. The method also shows exquisite sensitivity: as little as 1 ml additional extravascular water can be detected with PET [37].
Despite these impressive performance characteristics, PET imaging is expensive (like NMR) and not widely distributed among medical centers (unlike NMR). Positron-emitting isotopes also produce ionizing radiation (although the amounts used in any one study are quite low). As with X-ray CT or NMR imaging, the patient must be taken to the PET facility for study, an obvious problem in critically ill patients.
Electrical impedance tomography (EIT)
Air and liquid offer different resistances to the flow of electricity through the body. Measuring thoracic bioelectrical impedance in response to a low amplitude alternating electric current passed through the body yields a value for resistivity which can be correlated to gravimetric EVLW after correction for weight [38,39,40]. Recent refinement using 'dynamic' cross-sectional reconstruction of this information 'gated' to the cardiac cycle (a source of electricity) may make this portable test more sensitive and specific [41] and, eventually, clinically attractive.
Indicator dilution methods
EVLW measurements can be obtained by indicator dilution methods using either the so-called 'mean transit time' or 'slope-volume' approaches to analyze the temperature-time or concentration-time data [42,43,44,45].
With the indicator dilution method, a freely diffusible (heat/cold) and a non-diffusible (indocyanine green dye which binds to albumin) indicator each have the same flow but through different volumes of distribution. The difference in the mean transit times of the two indicators is therefore extravascular thermal volume (ETV). In the slope-volume method, a slope for the linear decay of the thermodilution curve is determined by mixing within the largest volume through which the thermal indicator passes (lungs). When multiplied by the cardiac output, pulmonary thermal volume (PTV) can be calculated. Further correction for intrathoracic blood volume yields a value for EVLW. This can be achieved through injection of a single thermal indicator, obviating the need to use indocyanine green dye [46,47].
Since the extravascular water content of myocardium and non-pulmonary blood vessels is small relative to the extravascular water content of the lung, ETV and EVLW are usually considered to be equivalent. Many studies have shown that ETV usually (but not always) closely approximates EVLW [43,44]. The thermal capacitance of the non-aqueous structures may, however, be significant, leading to overestimates of EVLW of 10-15% [48]. Effros [42] and Allison et al. [44] have both pointed out that the measurement of ETV is only equal to EVLW if the relative transit times of the thermal indicator through red cells versus plasma, the relative specific heats of extravascular tissue versus plasma, the density of blood, and the fraction of extravascular mass represented by water are all taken into account. Without such corrections, ETV should consistently overestimate EVLW by as much as 24% in normal lungs. Interestingly, as the lungs become more edematous, a greater fraction of the extravascular mass becomes water, and the error introduced by ignoring these factors (which is the case with commercially available devices) actually goes down.
While the theory underlying these measurements is well understood [42], commercially available equipment may have seriously biased the interpretation of performance in experimental and clinical settings [45,49,50]. In the only systems (COLD Z-03® and PiCCO®, Pulsion Medizintechnik, Munich, Germany) currently available for clinical use, many of the technical problems associated with the earlier equipment have apparently been addressed [44,45,46].
Overall, the correlation coefficient (r) for ETV and gravimetrically determined EVLW is usually at least 0.9 and the slope of the regression relationship is usually between 0.9 and 1.10 [43,44,45]. Using animal data, sensitivity has been estimated to be 88% and specificity 97%, with a coefficient of variation for repeated measurements of 4-8% [44]. This performance record in animals may be somewhat optimistic for the usual intensive care unit clinical setting. Using the 'COLD®' system, Zeravik et al. [51] reported a coefficient of variation of about 8%. Similarly, a strong correlation (r =0.98) with close absolute agreement between ETV and gravimetric measurements obtained from the lungs of organ donors has been reported [48].
The advantages of measuring EVLW by the single or double indicator dilution methods are several; the methods are (superficially) simple to implement, safe, reproducible, and repeatable. On the other hand, they are somewhat invasive (it requires central venous as well as arterial catheterization). In addition, the accumulation of extravascular water in any portion of lung that is downstream from a large vascular obstruction cannot be detected [44]. An analogous problem exists for lung regions that are simply poorly perfused, for instance as a result of using positive end-expiratory pressure (PEEP) [42,44,52].
Conclusion
None of the methods for measuring EVLW, other than chest radiography, have been widely incorporated into clinical practice. One reason is undoubtedly that no one has shown that a measurement of EVLW per se is needed for sound clinical decision making during the treatment of pulmonary edema. Similarly, no one has shown that incorporating such methods into routine clinical practice will affect patient outcome. Although the potential value of having a quantitative measure of pulmonary edema seems obvious (such as a treatment endpoint surrogate for mortality in clinical trials) and various studies have suggested how such measurements might be used in clinical decision making [48], a convincing outcome study demonstrating benefit is still needed.
References
Renkin E: Some consequences of capillary permeability to macromolecules: starling's hypothesis reconsidered. Am J Physiol 1986, 250: H706-H710.
Staub N: The pathogenesis of pulmonary edema. Prog Cardiovasc Dis 1980, 23: 53-80. 10.1016/0033-0620(80)90005-5
Matthay MA: Pathophysiology of pulmonary edema. Clin Chest Med 1985, 6: 301-314.
Lewis FR, Elings VB, Sturm JA: Bedside measurement of lung water. J Surg Res 1979, 27: 250-261. 10.1016/0022-4804(79)90138-0
Sivak ED, Starr NJ, Graves JW, et al.: Extravascular lung water values in patients undergoing coronary artery bypass surgery. Crit Care Med 1982, 10: 593-596.
Sibbald WJ, Warshawski FJ, Short AK, et al.: Clinical studies of measuring extravascular lung water by the thermal dye technique in critically ill patients. Chest 1983, 83: 725-731.
Gallagher JD, Moore RA, Kerns D, et al.: Effects of advanced age on extravascular lung water accumulation during coronary artery bypass surgery. Crit Care Med 1985, 13: 68-71.
Bongard FS, Matthay M, Mackersie RC, Lewis FR: Morphologic and physiologic correlates of increased extravascular lung water. Surgery 1984, 96: 395-403.
Staub NC: Clinical use of lung water measurements. Report of a workshop. Chest 1986, 90: 588-594.
Schuster DP: The evaluation of pulmonary endothelial barrier function: quantifying pulmonary edema and lung injury. In: Pulmonary Edema. Edited by Matthay MA, Ingbar DH. New York: Marcel Dekker, Inc., 1998, 121-161.
Snashall PD, Keyes SJ, Morgan BM, et al.: The radiographic detection of acute pulmonary oedema. A comparison of radiographic appearances, densitometry and lung water in dogs. Br J Radiol 1981, 54: 277-288.
Gattinoni L, Presenti A, Torresin A, et al.: Adult respiratory distress syndrome profiles by computed tomography. J Thorac Imaging 1986, 1: 25-30.
Wheeler A, Carroll F, Bernard G: Radiographic issues in adult respiratory distress syndrome. New Horiz 1993, 1: 471-477.
Halperin B, Feeley T, Mihm F, et al.: Evaluation of the portable chest roentgenogram for quantitating extravascular lung water in critically ill adults. Chest 1985, 88: 649-652.
Eisenberg PR, Hansbrough JR, Anderson D, Schuster DP: A prospective study of lung water measurements during patient management in an intensive care unit. Am Rev Respir Dis 1987, 136: 662-668.
Hedlund LW, Vock P, Effmann EL, Lischko MM, Putman CE: Hydrostatic pulmonary edema. An analysis of lung density changes by computed tomography. Invest Radiol 1984, 19: 254-262.
Forster BB, Muller NL, Mayo JR, et al.: High-resolution computed tomography of experimental hydrostatic pulmonary edema. Chest 1992, 101: 1434-1437.
Mayo JR: Magnetic resonance imaging of the chest. Where we stand. Radiol Clin North Am 1994, 32: 795-809.
Lancaster L, Bogdan AR, Kundel HL, McAffee B: Sodium MRI with coated magnetite: measurement of extravascular lung water in rats. Magn Reson Med 1991, 19: 96-104.
Cutillo AG, Morris AH, Ailion DC, et al.: Assessment of lung water distribution by nuclear magnetic resonance. A new method for quantifying and monitoring experimental lung injury. Am Rev Respir Dis 1988, 137: 1371-1378.
Morris AH, Blatter DD, Case TA, et al.: A new nuclear magnetic resonance property of lung. J Appl Physiol 1985, 58: 759-762.
Cutillo AG, Morris AH, Ailion DC, Durney CH, Case TA: Determination of lung water content and distribution by nuclear magnetic resonance imaging. J Thorac Imag 1986, 1: 39-51.
Mayo JR, Muller NL, Forster BB, Okazawa M, Pare PD: Magnetic resonance imaging of hydrostatic pulmonary edema in isolated dog lungs: comparison with computed tomography. Can Assoc Radiol J 1990, 41: 281-286.
Wexler HR, Nicholson RL, Prato FS, et al.: Quantitation of lung water by nuclear magnetic resonance imaging. A preliminary study. Invest Radiol 1985, 20: 583-590.
Phillips DM, Allen PS, Man SF: Assessment of temporal changes in pulmonary edema with NMR imaging. J Appl Physiol 1989, 66: 1197-1208.
Caruthers SD, Paschal CB, Pou NA, Roselli RJ, Harris TR: Regional measurements of pulmonary edema by using magnetic resonance imaging. J Appl Physiol 1998, 84: 2143-2153.
Rhodes CG: Measurement of lung water using nuclear magnetic resonance imaging [letter]. Br J Radiol 1986, 59: 1135-1136.
Cutillo A, Goodrich K, Krishnamurthy G, et al.: Lung water measurement by nuclear magnetic resonance: correlation with morphometry. J Appl Physiol 1995, 79: 2163-2168.
Mayo JR, MacKay AL, Whittall KP, Baile EM, Pare PD: Measurement of lung water content and pleural pressure gradient with magnetic resonance imaging. J Thorac Imag 1995, 10: 73-81.
Berthezene Y, Vexler V, Jerome H, et al.: Differentiation of capillary leak and hydrostatic pulmonary edema with a macromolecular MR imaging contrast agent. Radiology 1991, 181: 773-777.
Cutillo AG, Goodrich KC, Ganesan K, et al.: Alveolar air/tissue interface and nuclear magnetic resonance behavior of normal and edematous lungs. Am J Respir Crit Care Med 1995, 151: 1018-1026.
Schuster DP: Positron emission tomography: theory and its application to the study of lung disease. Am Rev Respir Dis 1989, 139: 818-840.
Schuster DP, Marklin GF, Mintun MA, Ter-Pogossian MM: PET measurement of regional lung density: 1. J Comput Assist Tomogr 1986, 10: 723-729.
Rhodes C, Hughes JMB: Pulmonary studies using positron emission tomography. Eur Respir J 1995, 8: 1001-1017.
Schuster DP, Mintun MA, Green MA, Ter-Pogossian MM: Regional lung water and hematocrit determined by positron emission tomography. J Appl Physiol 1985, 59: 860-868.
Schuster DP, Marklin GF, Mintun MA: Regional changes in extravascular lung water detected by positron emission tomography. J Appl Physiol 1986, 60: 1170-1178.
Velazquez M, Haller J, Amundsen T, Schuster DP: Regional lung water measurements with PET: accuracy, reproducibility, and linearity. J Nucl Med 1991, 32: 719-725.
Spinale FG, Reines HD, Cook MC, Crawford FA: Noninvasive estimation of extravascular lung water using bioimpedance. J Surg Res 1989, 47: 535-540.
Zellner JL, Spinale FG, Crawford FA: Bioimpedance: a novel method for the determination of extravascular lung water. J Surg Res 1990, 48: 454-459. 10.1016/0022-4804(90)90012-Q
Nierman DM, Eisen DI, Fein ED, et al.: Transthoracic bioimpedance can measure extravascular lung water in acute lung injury. J Surg Res 1996, 65: 101-108. 10.1006/jsre.1996.0350
Adler A, Amyot R, Guardo R, Bates JHT, Berthiaume Y: Monitoring changes in lung air and liquid volumes with electrical impedance tomography. J Appl Physiol 1997, 83: 1762-1767.
Effros RM: Lung water measurements with the mean transit time approach. J Appl Physiol 1985, 59: 673-683.
Sivak ED, Wiedemann HP: Clinical measurement of extravascular lung water. Crit Care Clin 1986, 2: 511-526.
Allison RC, Carlile PV Jr, Gray BA: Thermodilution measurement of lung water. Clin Chest Med 1985, 6: 439-457.
Pfeiffer U, Backus G, Blumel G, et al.: A fiberoptics based system for integrated monitoring of cardiac output, intrathoracic blood volume, extravascular lung water, O2 saturation, and a-v differences. In: Practical Applications of Fiberoptics in Critical Care Monitoring. Edited by Lewis F, Pfeiffer U. Berlin: Springer-Verlag, 1990,:114-125.
Schuster DP, Calandrino FS: Single versus double indicator dilution measurements of extravascular lung water. Crit Care Med 1991, 19: 84-88.
Sibbald WJ, Short AK, Warshawski FJ, Cunningham DG, Cheung H: Thermal dye measurements of extravascular lung water in critically ill patients. Intravascular Starling forces and extravascular lung water in the adult respiratory distress syndrome. Chest 1985, 87: 585-592.
Bock JC, Lewis FR: Clinical relevance of lung water measurement with the thermal-dye dilution technique. J Surg Res 1990, 48: 254-265. 10.1016/0022-4804(90)90222-N
Wickerts CJ, Jakobsson J, Frostell C, Hedenstierna G: Measurement of extravascular lung water by thermal-dye dilution technique: mechanisms of cardiac output dependence. Intensive Care Med 1990, 16: 115-120.
Fallon KD, Drake RE, Laine GA, Gabel JC: Effect of cardiac output on extravascular lung water estimates made with the Edwards lung water computer. Anesthesiol 1985, 62: 505-508.
Zeravik J, Borg U, Pfeiffer U: Efficacy of pressure support ventilation dependent on extravascular lung water. Chest 1990, 97: 1412-1419.
Haider M, Schad H: Effect of positive end-expiratory airway pressure (PEEP) on extravascular thermal lung water estimation in the dog. In: Practical Applications of Fiberoptics in Critical Care Monitoring. Edited by Lewis F, Pfeiffer U. Berlin: Springer-Verlag, 1990, 96-104.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lange, N.R., Schuster, D.P. The measurement of lung water. Crit Care 3, R19 (1999). https://doi.org/10.1186/cc342
Published:
DOI: https://doi.org/10.1186/cc342