Abstract
As in the adult with acute lung injury and acute respiratory distress syndrome, the use of lung-protective ventilation has improved outcomes for neonatal lung diseases. Animal models of neonatal respiratory distress syndrome and congenital diaphragmatic hernia have provided evidence that 'gentle ventilation' with low tidal volumes and 'open-lung' strategies of using positive end-expiratory pressure or high-frequency oscillatory ventilation result in less lung injury than do the traditional modes of mechanical ventilation with high inflating pressures and volumes. Although findings of retrospective studies in infants with respiratory distress syndrome, congenital diaphragmatic hernia, and persistent pulmonary hypertension of the newborn have been similar to those of the animal studies, prospective, randomized, controlled trials have yielded conflicting results. Successful clinical trial design in these infants and in children with acute lung injury/acute respiratory distress syndrome will require an appreciation of the data supporting the modern ventilator management strategies for infants with lung disease.
Similar content being viewed by others
Introduction
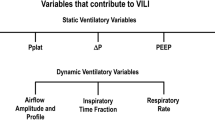
Although the first animal studies demonstrating the phenomenon of ventilator-induced lung injury (VILI) were published in the mid-1970s [1], it took 25 years to translate that information into a practice paradigm for treating adults with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) that is supported by a well designed, randomized, controlled clinical trial [2]. In the pediatric population, the smaller number of absolute cases of ALI/ARDS and lower mortality rate make it unlikely that a similar randomized, controlled clinical trial will be completed in the near future. For the moment, pediatric intensivists must extrapolate clinical trial results and ventilator algorithms from the adult population in their efforts to optimize outcomes in patients requiring mechanical ventilation.
Fortunately, the practice of lung-protective ventilation is not at all revolutionary in neonatal and pediatric intensive care units, where protective modalities such as continuous positive airway pressure (CPAP), high-frequency oscillatory ventilation (HFOV), and extracorporeal membrane oxygenation (ECMO) have been widely utilized over the past 20 years. In the same way that 'children are not just small adults', as the saying goes, they are also not just 'large babies'. Nevertheless, a thoughtful review of the evidence supporting current ventilator strategies used for neonatal respiratory distress syndrome (RDS), persistent pulmonary hypertension of the newborn (PPHN), and congenital diaphragmatic hernia (CDH) will help to guide the use of lung-protective strategies in the pediatric intensive care unit.
Respiratory distress syndrome in the preterm neonate
Nowhere is the potential harm caused by mechanical ventilation more evident than in the premature lung, which at birth is subject to the consequences of supplemental oxygen and mechanical ventilation. Although the ability to replace surfactant has reduced the severity of RDS and has permitted improved survival for even the most premature infants, the percentage of surviving infants who develop neonatal chronic lung disease (CLD) remains high [3, 4]. As in adults with ARDS, the search for interventions that will improve outcomes in RDS has focused on determining the safest and most lung-protective means of providing mechanical ventilation to these infants.
Animal studies
Although preterm lung volumes are small, significant inflation pressures are often necessary during resuscitation because of surfactant deficiency, immature structure, and fetal lung fluid. Animal studies in premature lambs have found that initial resuscitation with high tidal volumes augments abnormalities of lung mechanics [5–7], increases edema formation [8–10], increases inflammatory cytokine production [10], worsens histopathology [5, 6], and leads to decreased surfactant production [11], even when used in combination with surfactant therapy [5–7, 11]. The potential for overdistension is greater in the neonate because of a very compliant chest wall, which permits lung expansion beyond total lung capacity.
Another important mechanism of VILI in the preterm lung is the repetitive opening and closing of atelectatic alveolar units, which is more pronounced in the preterm infant because of surfactant deficiency. A strategy to reduce this effect is the 'open-lung' strategy of maintaining lung volumes with positive end-expiratory pressure (PEEP) or HFOV. McCulloch and coworkers [12] compared HFOV using high and low mean airway pressures in rabbits after saline lavage-induced surfactant deficiency, and found that maintainence of lung volumes significantly improved lung compliance and reduced hyaline membrane formation. In the preterm lamb and newborn piglet surfactant washout models, an open-lung strategy improved histologic evidence of collapse, preserved lung function, improved surfactant function, and reduced inflammation [13–17].
Before the advent of surfactant therapy, many surviving premature infants developed bronchopulmonary dysplasia (BPD) – a disease described by Northway and coworkers [18] in 1967 as one of alveolar and bronchiolar fibrosis. After the advent of surfactant therapy and gentler ventilation techniques, the lung pathology in those infants who continue to require pulmonary support after RDS is characterized by arrested alveolar development with less fibrotic change [19]. This 'new BPD' with deficient alveolarization has been termed 'CLD of infancy', defined clinically as dependence on supplemental oxygen at postconceptual age 36 weeks. Recently, preterm lamb and baboon models that manifest abnormal alveolarization after surfactant and 3–4 weeks of mechanical ventilation have been developed [20, 21]. Studies in these animal models have provided evidence that, in addition to improving other markers of lung injury, lung-protective ventilation improves alveolarization and lung development [20, 22]. This finding has added fuel to the search for the most lung-protective ventilation strategies for extremely premature infants.
If small tidal volumes and lung volume maintenance are able to prevent VILI in the preterm lung, then HFOV should be an ideal mode of ventilation for preterm infants. The most extensive animal data on this subject come from a preterm baboon model that was characterized by Coalson and coworkers in 1982 [23–26]. Using this model, they showed that the pathologic changes of RDS occur more commonly after a high tidal volume and low PEEP strategy than after HFOV using a higher mean airway pressure [25]. Hamilton and coworkers [27] found similar results comparing HFOV with conventional mechanical ventilation (CMV) in the saline-lavaged rabbit model. More recent studies in the premature baboon have demonstrated HFOV to be associated with improvements in lung mechanics and histopathologic outcomes (Fig. 1) when compared with CMV using small tidal volumes and low PEEP [28]. Together, these animal data provide evidence supporting both theoretical advantages of HFOV, namely reduction in VILI associated with high tidal volumes and the repetitive opening and closing of atelectatic units.
Representative lung histopathology in (a) term baboons, (b) preterm baboons treated with a low tidal volume, low positive end-expiratory pressure strategy, and (c) preterm baboons treated with high-frequency oscillatory ventilation. Hematoxylin and eosin; 100×. With permission from Yoder and coworkers [63].
Another strategy to limit VILI is with a combination of permissive hypercapnia and early extubation to CPAP. In the preterm lamb model, 2 hours of CPAP or CMV immediately after birth were compared; animals managed with CPAP exhibited higher lung volumes and reduced inflammatory cell infiltrate [28]. In the baboon CLD model, long-term management with CPAP led to a dramatic improvement in lung development with similar alveolarization to that in an animal killed after normal term delivery [22].
Human studies
Before the surfactant era, Kraybill and coworkers [29] showed that early hypocapnia was associated with a higher incidence of BPD in a retrospective study, and after the advent of surfactant therapy another retrospective study found that hypocapnia before surfactant administration was associated with similar adverse outcomes [30]. These studies formed the basis of the hypothesis that more aggressive ventilation might be causally related to the development of CLD in infants. Two prospective trials of permissive hypercapnia were designed to test this hypothesis; both studies demonstrated decreased ventilator days in the hypercapnic group but neither found a significant difference in CLD development, death, or development of intraventricular hemorrhage [31, 32]. Several authors have evaluated differences in CLD prevalence among neonatal intensive care units [33–35] and concluded that ventilator strategies designed to reduce VILI can explain these discrepancies.
Although the animal studies of HFOV support its use to improve RDS and prevent CLD, studies in preterm infants have not been as convincing. Many early trials did not use prenatal steroids or surfactant, and later studies used HFOV with low mean airway pressures and therefore did not take advantage of the open-lung benefits of HFOV. Two large multicenter, randomized controlled trials of early HFOV versus CMV for the prevention of CLD in preterm infants [36, 37] were recently published simultaneously. Although Courtney and coworkers [36] found no differences in survival among 500 infants with birthweight under 1200 g, survival without CLD was improved from 47% in synchronized intermittent mandatory ventilation-treated infants to 56% in HFOV-treated infants. HFOV-treated infants were successfully extubated a week earlier on average. In contrast, Johnson and coworkers [37] found no significant differences in overall survival or CLD among 787 infants at 23–28 weeks of gestation.
The differences in results for these two studies probably reflect the fact that Courtney and coworkers [36] defined a disease threshold for enrollment (mean airway pressure of at least 6 cmH2O and 0.25 fractional inspired oxygen within the first 4 hours of life), used more closely defined ventilator algorithms and extubation criteria, targeted hypercapnia (partial carbon dioxide tension 40–65 mmHg) and maintained patients on their assigned ventilator until extubation, and the patients had a mean duration of HFOV of more than 6 days. In contrast, Johnson and coworkers [37] did not define a severity of illness threshold for enrollment, did not define algorithms for ventilator management and targeted normocapnia (partial carbon dioxide tension 34–53 mmHg), and the mean duration of HFOV was 3 days. Although Courtney and coworkers studied a more well defined population of infants who were sicker, the study by Johnson and colleagues may more accurately reflect the actual practice of HFOV across neonatal intensive care units [38].
Although the jury remains out concerning how best to practice lung-protective ventilation in order to reduce the incidence of CLD in preterm infants, it is clear that VILI contributes heavily to CLD. Any successful future strategies will undoubtedly employ the concepts of lung-protective ventilation described above.
'Gentle ventilation' for persistent pulmonary hypertension of the newborn
Full-term infants are also susceptible to the injurious effects of mechanical ventilation. PPHN has been well recognized as a clinical syndrome of high pulmonary vascular resistance and right-to-left shunting since the 1950s. The responsiveness of the pulmonary vasculature to acid–base status was elucidated in the 1960s, and led directly to the use of hyperventilation to produce hypocapnia and alkalosis in the management of PPHN [39]. Two case series reported in the early 1980s [40, 41] showed that hyperventilation of infants with PPHN increased arterial oxygen tension over several hours. This approach was associated with reported mortality rates of 40% in all infants and 80–90% in infants with severe PPHN [42, 43].
Given the emerging animal data regarding the significance of VILI [1], Wung and coworkers [44] at Babies' Hospital in New York City began to manage PPHN without hyperventilation in an attempt to protect the lung from high peak inspiratory pressure and tidal volume. This was before the advent of inhaled nitric oxide (iNO) therapy. Those investigators reported 100% survival in 15 infants with severe PPHN ventilated with target partial carbon dioxide tension of 40–60 mmHg. Dworetz and coworkers [43] applied the lessons from the study by Wung and coworkers, and compared 23 infants from the era of hyperventilation versus 17 infants from the era of 'gentle ventilation'. They found that overall survival improved from 65% to 88% as the management changed, and survival in the sickest infants (who met criteria and were eligible for ECMO but did not receive it) improved from 0% to 89%.
Infants with PPHN often present with severe hypoxemic respiratory failure, and as soon as HFOV and ECMO became available in the late 1970s and early 1980s they were put to use in this population of infants with very high mortality rates. Although originally employed as a means to improve arterial oxygen content and systemic oxygen delivery, HFOV and ECMO also provided a means by which the lungs of these infants could be protected from injurious mechanical ventilation. Once iNO became available, HFOV provided a means by which atelectatic lungs could be efficiently recruited and enhance alveolar delivery of this selective pulmonary vasodilator. Kinsella and coworkers [45] found that the response to iNO therapy plus HFOV was better than the response to iNO or HFOV alone in 205 neonates in a randomized, controlled trial. Overall improvement in mortality rates and reduction in need to use ECMO in these infants is probably related to both lung-protective ventilation (regardless of modality) and iNO therapy. Gupta and colleagues [46] used gentle CMV with permissive hypercapnia and iNO and reported an overall mortality rate of 9.8% in infants with meconium aspiration syndrome and PPHN – a figure comparable to that in studies combining HFOV and iNO therapy [45].
Ventilation for congenital diaphragmatic hernia
CDH is another excellent example of the negative impact that aggressive ventilation can have on morbidity and mortality in neonates with lung disease. Despite best efforts to improve survival in the 1980s with delayed surgical repair and other modern technologies such as synchronized intermittent mandatory ventilation, HFOV, surfactant replacement, iNO, and ECMO, mortality rates in infants with CDH remained between 48% and 66% as recently as 1991 [47]. During this time, management strategies included hyperventilation and induced alkalosis in order to reduce pulmonary vascular resistance and limit right-to-left shunting. The application of 'gentle ventilation' principles to the CDH population helped to decrease mortality rates to 31–39% by 1994 (Table 1) [47, 48], 20% in one center by 1998 [49], and 7% in another center by 2002 [50].
'Gentle ventilation' is likely to benefit the infant with CDH because, like the preterm lung, CDH lungs are immature and total lung capacity is small. Even when born full term, infants with CDH have lungs that are immature in structure and biochemistry. Type II pneumocytes have fewer lamellar bodies and surfactant is deficient [51]. An autopsy study found that both alveolarization and surfactant were deficient in CDH lungs, with the affected side being more immature than the unaffected side [52]. An analysis of autopsy specimens from 68 out of 101 infants who died from CDH at one institution from 1981 to 1994 showed that 91% of infants had hyaline membrane formation, which was more prominent in the ipsilateral, severely affected lung [49]. Of the six infants who did not die with prominent hyaline membranes in that study, five were treated with HFOV shortly after birth. The prominent hyaline membranes were postulated to be a result of lung immaturity and VILI [47, 49].
Interestingly, lung disease in those survivors of CDH with pulmonary morbidity closely resembles BPD. In a study of 45 survivors of CDH repair reported in 1993, 15 had clinical and radiologic evidence of BPD [53]. Animal studies indicate that the pathogenesis of VILI is similar in preterm infants and infants with CDH. The lungs of rats with nitrofen-induced CDH who are exposed to mechanical ventilation have abnormally high elastin deposition [54], which is similar to preterm lambs exposed to injurious mechanical ventilation [55]. More abnormal deposition is present in lambs ventilated with a slow rate and large tidal volume as compared with a faster rate and small tidal volume [20]. Abnormal elastin deposition is present in autopsy specimens of lungs of infants with BPD [56, 57], and abnormal layout of elastin deposition has been proposed to play an important role in the impairment of alveolarization seen in BPD [58]. The effects of mechanical ventilation on elastin production and deposition may explain impaired alveolarization in the CLD seen in both premature infants and those with CDH. The improvements in mortality in the era of gentle ventilation of infants with CDH may be in part related to improved alveolar development in these infants, but this has not yet been studied.
Conclusion
The evidence presented above strongly supports the use of lung-protective ventilation in the management of neonatal lung disease. Neonates with RDS, meconium aspiration syndrome, or CDH are thought to have more homogeneous lung pathology than the patchy, heterogeneously aerated pattern seen in ARDS [59], but recent magnetic resonance imaging evidence indicates that RDS has a similar distribution of dependent atelectasis and lung water to ARDS (Fig. 2) [60]. This evidence gives more credence to the concern for alveolar overdistention in the nondependent, aerated regions of the neonatal lung. It is clear that the use of lung-protective ventilator strategies similar to the algorithms developed for adults with ALI/ARDS can have a significant impact on outcomes. The non-neonate with ALI/ARDS and heterogeneous lung mechanics may be particularly susceptible to lung overdistension because of small absolute lung volumes and a highly compliant chest wall. Furthermore, large tidal volumes and elevated airway pressures in these patients may induce regional overdistension and lung stretch that is much more significant than in adults, whose noncompliant chest wall and increased abdominal compartment pressures may limit transpulmonary pressures.
Transverse T1-weighted magnetic resonance images at the level of the left atrium in (a) a 4-day-old, 26-week gestation infant, and (b) a 2-day old, term infant. In the planes of the superimposed vertical white lines, signal intensity is graphed to the left of the images and shows that the preterm infant has a gravity-dependent increase in signal intensity as compared with the homogeneous pattern in the term infant. The arrow in panel a points to an area of dependent thickened pleural margin. With permission from Adams and coworkers [60].
In patients younger than 5 years, the closing capacity of the lung is very close to the functional residual capacity. In the setting of lung disease and mechanical ventilatory support, the young patient is likely to suffer significant alveolar instability and atelectasis. Children with ALI/ARDS may therefore benefit even more than adults from the lessons learned in the animal laboratory and adult clinical trials.
As clinical trial networks in the pediatric population evolve and mature [61], data relevant to the child with ALI/ARDS will emerge. Successful design of these trials will depend on knowledge gained from neonatal animal and human studies. An excellent example is a recent study from Dobyns and coworkers [62], who took lessons from the PPHN population [45] and studied the combined effects of HFOV and iNO on oxygenation in pediatric patients with acute hypoxemic respiratory failure. Although a prospective, randomized, controlled trial with important outcome measures is necessary to draw conclusions about this therapy, data from infants with PPHN have clearly helped to frame the important questions about this novel therapy. In the pursuit of excellent outcomes for children with ALI/ARDS, pediatric investigators and practitioners alike will benefit from a thorough understanding of relevant neonatal and adult animal and clinical data.
Abbreviations
- ALI:
-
acute lung injury
- ARDS:
-
= acute respiratory distress syndrome
- BPD:
-
= bronchopulmonary dysplasia
- CDH:
-
= congenital diaphragmatic hernia
- CLD:
-
= chronic lung disease
- CMV:
-
= conventional mechanical ventilation
- CPAP:
-
= continuous positive airway pressure
- ECMO:
-
= extracorporeal membrane oxygenation
- HFOV:
-
= high-frequency oscillatory ventilation
- INO:
-
= inhaled nitric oxide
- PEEP:
-
= positive end-expiratory pressure
- PPHN:
-
= persistent pulmonary hypertension of the newborn
- RDS:
-
= respiratory distress syndrome
- VILI:
-
= ventilator-induced lung injury.
References
Webb HH, Tierney DF: Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 1974, 110: 556-565.
Anonymous: Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000, 342: 1301-1308. 10.1056/NEJM200005043421801
Yoder BA, Anwar MU, Clark RH: Early prediction of neonatal chronic lung disease: a comparison of three scoring methods. Pediatr Pulmonol 1999, 27: 388-394. 10.1002/(SICI)1099-0496(199906)27:6<388::AID-PPUL5>3.0.CO;2-N
Jobe AH, Ikegami M: Mechanisms initiating lung injury in the preterm. Early Hum Dev 1998, 53: 81-94. 10.1016/S0378-3782(98)00045-0
Bjorklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, Vilstrup CT: Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res 1997, 42: 348-355.
Bjorklund LJ, Ingimarsson J, Curstedt T, Larsson A, Robertson B, Werner O: Lung recruitment at birth does not improve lung function in immature lambs receiving surfactant. Acta Anaesthesiol Scand 2001, 45: 986-993. 10.1034/j.1399-6576.2001.450811.x
Ingimarsson J, Bjorklund LJ, Curstedt T, Gudmundsson S, Larsson A, Robertson B, Werner O: Incomplete protection by prophylactic surfactant against the adverse effects of large lung inflations at birth in immature lambs. Intensive Care Med 2004, 30: 1446-1453. 10.1007/s00134-004-2227-3
Carlton DP, Cummings JJ, Scheerer RG, Poulain FR, Bland RD: Lung overexpansion increases pulmonary microvascular protein permeability in young lambs. J Appl Physiol 1990, 69: 577-583.
Ikegami M, Rebello CM, Jobe AH: Surfactant inhibition by plasma: gestational age and surfactant treatment effects in preterm lambs. J Appl Physiol 1996, 81: 2517-2522.
Ikegami M, Kallapur S, Michna J, Jobe AH: Lung injury and surfactant metabolism after hyperventilation of premature lambs. Pediatr Res 2000, 47: 398-404.
Wada K, Jobe AH, Ikegami M: Tidal volume effects on surfactant treatment responses with the initiation of ventilation in preterm lambs. J Appl Physiol 1997, 83: 1054-1061.
McCulloch PR, Forkert PG, Froese AB: Lung volume maintenance prevents lung injury during high frequency oscillatory ventilation in surfactant-deficient rabbits. Am Rev Respir Dis 1988, 137: 1185-1192.
Michna J, Jobe AH, Ikegami M: Positive end-expiratory pressure preserves surfactant function in preterm lambs. Am J Respir Crit Care Med 1999, 160: 634-639.
Naik AS, Kallapur SG, Bachurski CJ, Jobe AH, Michna J, Kramer BW, Ikegami M: Effects of ventilation with different positive end-expiratory pressures on cytokine expression in the preterm lamb lung. Am J Respir Crit Care Med 2001, 164: 494-498.
van Kaam AH, Dik WA, Haitsma JJ, De Jaegere A, Naber BA, van Aalderen WM, Kok JH, Lachmann B: Application of the open-lung concept during positive-pressure ventilation reduces pulmonary inflammation in newborn piglets. Biol Neonate 2003, 83: 273-280. 10.1159/000069482
van Kaam AH, de Jaegere A, Haitsma JJ, Van Aalderen WM, Kok JH, Lachmann B: Positive pressure ventilation with the open lung concept optimizes gas exchange and reduces ventilator-induced lung injury in newborn piglets. Pediatr Res 2003, 53: 245-253. 10.1203/01.PDR.0000047520.44168.22
van Kaam AH, Haitsma JJ, Dik WA, Naber BA, Alblas EH, De Jaegere A, Kok JH, Lachmann B: Response to exogenous surfactant is different during open lung and conventional ventilation. Crit Care Med 2004, 32: 774-780. 10.1097/01.CCM.0000114578.48244.21
Northway WH Jr, Rosan RC, Porter DY: Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med 1967, 276: 357-368.
Husain AN, Siddiqui NH, Stocker JT: Pathology of arrested acinar development in postsurfactant bronchopulmonary dysplasia. Hum Pathol 1998, 29: 710-717. 10.1016/S0046-8177(98)90280-5
Albertine KH, Jones GP, Starcher BC, Bohnsack JF, Davis PL, Cho SC, Carlton DP, Bland RD: Chronic lung injury in preterm lambs. Disordered respiratory tract development. Am J Respir Crit Care Med 1999, 159: 945-958.
Coalson JJ, Winter VT, Siler-Khodr T, Yoder BA: Neonatal chronic lung disease in extremely immature baboons. Am J Respir Crit Care Med 1999, 160: 1333-1346.
Thomson MA, Yoder BA, Winter VT, Martin H, Catland D, Siler-Khodr TM, Coalson JJ: Treatment of immature baboons for 28 days with early nasal continuous positive airway pressure. Am J Respir Crit Care Med 2004, 169: 1054-1062. 10.1164/rccm.200309-1276OC
Coalson JJ, Kuehl TJ, Escobedo MB, Hilliard JL, Smith F, Meredith K, Null DM Jr, Walsh W, Johnson D, Robotham JL: A baboon model of bronchopulmonary dysplasia. II. Pathologic features. Exp Mol Pathol 1982, 37: 335-350. 10.1016/0014-4800(82)90046-6
Gerstmann DR, deLemos RA, Coalson JJ, Clark RH, Wiswell TE, Winter DC, Kuehl TJ, Meredith KS, Null DM Jr: Influence of ventilatory technique on pulmonary baroinjury in baboons with hyaline membrane disease. Pediatr Pulmonol 1988, 5: 82-91.
Meredith KS, deLemos RA, Coalson JJ, King RJ, Gerstmann DR, Kumar R, Kuehl TJ, Winter DC, Taylor A, Clark RH, et al.: Role of lung injury in the pathogenesis of hyaline membrane disease in premature baboons. J Appl Physiol 1989, 66: 2150-2158.
deLemos RA, Coalson JJ, deLemos JA, King RJ, Clark RH, Gerstmann DR: Rescue ventilation with high frequency oscillation in premature baboons with hyaline membrane disease. Pediatr Pulmonol 1992, 12: 29-36.
Hamilton PP, Onayemi A, Smyth JA, Gillan JE, Cutz E, Froese AB, Bryan AC: Comparison of conventional and high-frequency ventilation: oxygenation and lung pathology. J Appl Physiol 1983, 55: 131-138.
Jobe AH, Kramer BW, Moss TJ, Newnham JP, Ikegami M: Decreased indicators of lung injury with continuous positive expiratory pressure in preterm lambs. Pediatr Res 2002, 52: 387-392. 10.1203/01.PDR.0000025341.25481.42
Kraybill EN, Runyan DK, Bose CL, Khan JH: Risk factors for chronic lung disease in infants with birth weights of 751 to 1000 grams. J Pediatr 1989, 115: 115-120.
Garland JS, Buck RK, Allred EN, Leviton A: Hypocarbia before surfactant therapy appears to increase bronchopulmonary dysplasia risk in infants with respiratory distress syndrome. Arch Pediatr Adolesc Med 1995, 149: 617-622.
Carlo WA, Stark AR, Wright LL, Tyson JE, Papile LA, Shankaran S, Donovan EF, Oh W, Bauer CR, Saha S, et al.: Minimal ventilation to prevent bronchopulmonary dysplasia in extremely-low-birth-weight infants. J Pediatr 2002, 141: 370-374. 10.1067/mpd.2002.127507
Mariani G, Cifuentes J, Carlo WA: Randomized trial of permissive hypercapnia in preterm infants. Pediatrics 1999, 104: 1082-1088. 10.1542/peds.104.5.1082
Van Marter LJ, Pagano M, Allred EN, Leviton A, Kuban KC: Rate of bronchopulmonary dysplasia as a function of neonatal intensive care practices. J Pediatr 1992, 120: 938-946.
Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M, Susser M, Paneth N, Leviton A: Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics 2000, 105: 1194-1201. 10.1542/peds.105.6.1194
Avery ME, Tooley WH, Keller JB, Hurd SS, Bryan MH, Cotton RB, Epstein MF, Fitzhardinge PM, Hansen CB, Hansen TN, et al.: Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics 1987, 79: 26-30.
Courtney SE, Durand DJ, Asselin JM, Hudak ML, Aschner JL, Shoemaker CT: High-frequency oscillatory ventilation versus conventional mechanical ventilation for very-low-birth-weight infants. N Engl J Med 2002, 347: 643-652. 10.1056/NEJMoa012750
Johnson AH, Peacock JL, Greenough A, Marlow N, Limb ES, Marston L, Calvert SA: High-frequency oscillatory ventilation for the prevention of chronic lung disease of prematurity. N Engl J Med 2002, 347: 633-642. 10.1056/NEJMoa020432
Stark AR: High-frequency oscillatory ventilation to prevent bronchopulmonary dysplasia: are we there yet? N Engl J Med 2002, 347: 682-684. 10.1056/NEJMe020080
Sahni R, Wung JT, James LS: Controversies in management of persistent pulmonary hypertension of the newborn. Pediatrics 1994, 94: 307-309.
Peckham GJ, Fox WW: Physiologic factors affecting pulmonary artery pressure in infants with persistent pulmonary hypertension. J Pediatr 1978, 93: 1005-1010.
Drummond WH, Gregory GA, Heymann MA, Phibbs RA: The independent effects of hyperventilation, tolazoline, and dopamine on infants with persistent pulmonary hypertension. J Pediatr 1981, 98: 603-611.
Fox WW, Duara S: Persistent pulmonary hypertension in the neonate: diagnosis and management. J Pediatr 1983, 103: 505-514.
Dworetz AR, Moya FR, Sabo B, Gladstone I, Gross I: Survival of infants with persistent pulmonary hypertension without extracorporeal membrane oxygenation. Pediatrics 1989, 84: 1-6.
Wung JT, James LS, Kilchevsky E, James E: Management of infants with severe respiratory failure and persistence of the fetal circulation, without hyperventilation. Pediatrics 1985, 76: 488-494.
Kinsella JP, Truog WE, Walsh WF, Goldberg RN, Bancalari E, Mayock DE, Redding GJ, deLemos RA, Sardesai S, McCurnin DC, et al.: Randomized, multicenter trial of inhaled nitric oxide and high-frequency oscillatory ventilation in severe, persistent pulmonary hypertension of the newborn. J Pediatr 1997, 131: 55-62.
Gupta A, Rastogi S, Sahni R, Bhutada A, Bateman D, Rastogi D, Smerling A, Wung JT: Inhaled nitric oxide and gentle ventilation in the treatment of pulmonary hypertension of the newborn: a single-center, 5-year experience. J Perinatol 2002, 22: 435-441. 10.1038/sj.jp.7210761
Azarow K, Messineo A, Pearl R, Filler R, Barker G, Bohn D: Congenital diaphragmatic hernia – a tale of two cities: the Toronto experience. J Pediatr Surg 1997, 32: 395-400. 10.1016/S0022-3468(97)90589-3
Wilson JM, Lund DP, Lillehei CW, Vacanti JP: Congenital diaphragmatic hernia – a tale of two cities: the Boston experience. J Pediatr Surg 1997, 32: 401-405. 10.1016/S0022-3468(97)90590-X
Sakurai Y, Azarow K, Cutz E, Messineo A, Pearl R, Bohn D: Pulmonary barotrauma in congenital diaphragmatic hernia: a clinicopathological correlation. J Pediatr Surg 1999, 34: 1813-1817. 10.1016/S0022-3468(99)90319-6
Downard CD, Jaksic T, Garza JJ, Dzakovic A, Nemes L, Jennings RW, Wilson JM: Analysis of an improved survival rate for congenital diaphragmatic hernia. J Pediatr Surg 2003, 38: 729-732. 10.1016/jpsu.2003.50194
Finer NN: Surfactant use for neonatal lung injury: beyond respiratory distress syndrome. Paediatr Respir Rev 2004, Suppl A: S289-S297. 10.1016/S1526-0542(04)90053-X
Asabe K, Tsuji K, Handa N, Kurosaka N, Kajiwara M: Immunohistochemical distribution of surfactant apoprotein-A in congenital diaphragmatic hernia. J Pediatr Surg 1997, 32: 667-672. 10.1016/S0022-3468(97)90001-4
Bos AP, Hussain SM, Hazebroek FW, Tibboel D, Meradji M, Molenaar JC: Radiographic evidence of bronchopulmonary dysplasia in high-risk congenital diaphragmatic hernia survivors. Pediatr Pulmonol 1993, 15: 231-234.
Guarino N, Teramoto H, Shima H, Oue T, Puri P: Effect of mechanical ventilation on the pulmonary expression and production of elastin in nitrofen-induced diaphragmatic hernia in rats. J Pediatr Surg 2002, 37: 1253-1257. 10.1053/jpsu.2002.34974
Pierce RA, Albertine KH, Starcher BC, Bohnsack JF, Carlton DP, Bland RD: Chronic lung injury in preterm lambs: disordered pulmonary elastin deposition. Am J Physiol 1997, 272: L452-L460.
Hislop AA, Wigglesworth JS, Desai R, Aber V: The effects of preterm delivery and mechanical ventilation on human lung growth. Early Hum Dev 1987, 15: 147-164. 10.1016/0378-3782(87)90003-X
Chambers HM, van Velzen D: Ventilator-related pathology in the extremely immature lung. Pathology 1989, 21: 79-83.
Robertson B: The evolution of neonatal respiratory distress syndrome into chronic lung disease. Eur Respir J Suppl 1989, 3: 33s-37s.
Gattinoni L, Pesenti A, Bombino M, Baglioni S, Rivolta M, Rossi F, Rossi G, Fumagalli R, Marcolin R, Mascheroni D, et al.: Relationships between lung computed tomographic density, gas exchange, and PEEP in acute respiratory failure. Anesthesiology 1988, 69: 824-832.
Adams EW, Counsell SJ, Hajnal JV, Cox PN, Kennea NL, Thornton AS, Bryan AC, Edwards AD: Magnetic resonance imaging of lung water content and distribution in term and preterm infants. Am J Respir Crit Care Med 2002, 166: 397-402. 10.1164/rccm.2104116
Randolph AG, Wypij D, Venkataraman ST, Hanson JH, Gedeit RG, Meert KL, Luckett PM, Forbes P, Lilley M, Thompson J, et al.: Effect of mechanical ventilator weaning protocols on respiratory outcomes in infants and children: a randomized controlled trial. JAMA 2002, 288: 2561-2568. 10.1001/jama.288.20.2561
Dobyns EL, Anas NG, Fortenberry JD, Deshpande J, Cornfield DN, Tasker RC, Liu P, Eells PL, Griebel J, Kinsella JP, et al.: Interactive effects of high-frequency oscillatory ventilation and inhaled nitric oxide in acute hypoxemic respiratory failure in pediatrics. Crit Care Med 2002, 30: 2425-2429. 10.1097/00003246-200211000-00004
Yoder BA, Siler-Khodr T, Winter VT, Coalson JJ: High-frequency oscillatory ventilation: effects on lung function, mechanics, and airway cytokines in the immature baboon model for neonatal chronic lung disease. Am J Respir Crit Care Med 2000, 162: 1867-1876.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Vitali, S.H., Arnold, J.H. Bench-to-bedside review: Ventilator strategies to reduce lung injury – lessons from pediatric and neonatal intensive care. Crit Care 9, 177 (2004). https://doi.org/10.1186/cc2987
Published:
DOI: https://doi.org/10.1186/cc2987